Abstract
Patients with Crohn’s disease (CD) often require surgical resection due to complications, such as strictures and abscesses, or disease refractory to medical therapy. To understand the evolving management of patients with CD after surgery, we outline the risk factors for postoperative recurrence, advances in postoperative endoscopic evaluation and characterization of recurrence, noninvasive methods of assessing postoperative recurrence, use of postoperative prophylactic medical therapy including newer biologics, and novel surgical methods to reduce postoperative recurrence. The Rutgeerts score (RS) was developed to predict progression of disease based on endoscopic appearance postoperatively and to guide medical therapy. However, this scoring system groups ileal and anastomotic lesions into the same category. A modified RS was developed to separate lesions isolated to the anastomosis and those in the neo-terminal ileum to further understand the role of anastomotic lesions in CD progression. Additional scoring systems have also been evaluated to better understand these differences. In addition, noninvasive diagnostic methods, such as small bowel ultrasound, have high sensitivity and specificity for the detection of postoperative recurrence and are being evaluated as independent methods of assessment. Studies have also shown a reduction in endoscopic recurrence with postoperative anti-TNFα therapy. However, preoperative exposure to anti-TNFα therapy may impact postoperative response to these medications, and therefore, determining optimal postoperative prophylaxis strategy for biologic-experienced patients requires further exploration. Lastly, new surgical modalities to reduce postoperative recurrence are currently being investigated with preliminary data suggesting that an antimesenteric functional end-to-end anastomosis (Kono-S) may decrease postoperative recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Crohn’s disease (CD) is a transmural inflammatory process that can involve any part of the digestive tract and affects roughly 1 in 300 people in the Western world with a rising incidence in newly industrialized countries [1, 2]. Patients with CD often require surgical resection due to complications such as strictures, fistulae, abscesses or disease refractory to medical therapy. The risk of surgery after diagnosis is 16.3% at 1 year, 33.3% at 5 years, and 46.6% at 10 years [3, 4]. Clinical or surgical relapse after initial surgery is frequently preceded by endoscopic recurrence at the neo-terminal ileum and is triggered by intestinal luminal contents [5,6,7]. To understand the evolving management of patients with CD after surgery, we reviewed the risk factors for postoperative recurrence, advances in postoperative endoscopic evaluation and characterization of recurrence, noninvasive methods of assessing postoperative recurrence, use of postoperative prophylactic medical therapy including newer biologics, and novel surgical methods to reduce postoperative recurrence.
Methods
For this review, we searched PubMed, EMBASE, Cochrane Central, Clinicaltrials.gov, Web of Science, and Google Scholar from 1990 through 2021, with a focus on studies published after 2015. We identified articles on postoperative recurrence of CD pertaining to: (1) risk factors for recurrence; (2) postoperative endoscopic evaluation; (3) noninvasive methods of postoperative evaluation; (4) drug trials of medical prophylaxis; and (5) surgical methods to reduce postoperative recurrence. We included cohort and randomized controlled studies that involved diagnostics, risk stratification and treatment of patients with CD postoperatively. The search strategy employed a combination of Medical Subject (MeSH) headings and keywords as follows: “Crohn’s disease,” “inflammatory bowel disease,” “CD,” “postoperative care,” “postoperative complications,” “postoperative period,” “surgery,” “operation,” “risk factors,” “disease duration,” “previous resection,” “prior resection,” “disease location,” “anastomosis,” “disease extent,” “risk factor,” “genetic,” “anastomotic configuration,” “laparoscopic,” “open,” “length of resection,” “resection length,” “microscopic disease,” “myenteric plexitis,” “diagnosis,” “microbiome,” “assessment,” “colonoscopy,” “endoscopy,” “ileocolonoscopy,” “noninvasive methods,” “Rutgeerts,” “fecal calprotectin,” “CRP,” “inflammatory markers,” “ultrasound,” “SICUS,” “small intestine contrast enhanced ultrasound,” “CEUS,” “contrast-enhanced ultrasound,” “MRI,” “magnetic resonance imaging,” “small bowel MRI,” “CT,” “computed tomography,” “enterography,” “enteroclysis,” “mucosal healing,” azathioprine,” “thiopurine,” “6-mercaptopurine,” “biologics,” “infliximab,” “adalimumab,” “vedolizumab,” “ustekinumab,” “drug therapy,” “prophylaxis,” “Kono-S,” “mesentery.” Boolean operators (“not,” “and,” “or”) were also used to narrow or widen the search. Studies focusing on pediatric populations, those with less than 6-month follow-up, and those not written in English and unable to be translated to English were excluded. If publications reported duplicate data on a population, only the publication with the longest follow-up period was included.
Risk Factors for Postoperative Recurrence
There are multiple well-known risk factors for postoperative recurrence such as current smoking, younger age at diagnosis, two or more prior surgeries related to CD and penetrating disease [8,9,10,11,12]. Additional clinical risk factors including NOD2/CARD15 genetic variant, continuous ileocolonic disease, and perianal fistulae have also been implicated in postoperative recurrence [13, 14]. Histologic features at the time of resection, such as positive resection margins, myenteric and submucosal plexitis, and granulomas, are also predictive of postoperative CD recurrence in recent studies [15]. In addition, microbial factors, such as bacterial dysbiosis and a low abundance of Faecalibacterium prausnitzii in both resected and postoperative ileal mucosa, have been associated with an increased risk of endoscopic recurrence. However, the utility of using gut microbiota in predicting recurrence may be limited by the use of antibiotics in the pre- and perioperative period [16,17,18,19,20].
Postoperative Endoscopic Evaluation
According to the American Gastroenterological Association (AGA) guidelines published in 2017, postoperative endoscopic monitoring is recommended at 6–12 months after surgery in both patients on and off postoperative medical therapy for CD [3]. The Rutgeerts score (RS) has been traditionally used to grade the severity of endoscopic lesions in the neo-terminal ileum and ileocolonic anastomosis and a score of i1–i4 is considered endoscopic recurrence, with escalation of medical therapy recommended for i2–i4 lesions (Table 1) [21]. However, recent studies have proposed separating aphthous lesions in the neo-terminal ileum from those confined to the anastomosis, as questions remain whether anastomotic lesions are related to post-surgical ischemic changes instead of progression of CD. A modified Rutgeerts score (mRS) was developed with i2 sub-scores (i2a for those isolated to the anastomosis and i2b for > 5 aphthous lesions in the neo-terminal ileum) and performed well as a reliable assessment. However, implementation of this score has yielded contradictory results [22,23,24,25,26]. One retrospective study by Riviere et al. [23] using this modified score found no significant difference in clinical postoperative recurrence and need for surgical intervention between patients with both scores, indicating that anastomotic lesions can also lead to disease recurrence. Similarly, another recent retrospective study by Hirten et al. [26] determined that anastomotic ulcers occur in over half of patients with CD after ileocolic resection and are associated with CD recurrence. In contrast, a retrospective study concluded that endoscopic lesions limited to the ileocolonic anastomosis (i2a) in patients with CD undergoing colonoscopy within 1 year of their resection were not associated with disease progression, whereas those in the neo-terminal ileum (i2b) were [24].
Alternative scoring systems have been developed to better compare disease progression in patients with anastomotic and neo-terminal ileal lesions. A recently published prospective multicenter study developed two separate endoscopic grading systems (REMIND score) for anastomotic and ileal lesions after surgery for ileal or ileocolonic CD [25]. Among 225 included patients, long-term follow-up was available in 193 with a median follow-up of 3.82 years. Clinical recurrence-free survival after surgery, which was defined as CD-related clinical manifestations confirmed either by endoscopy, imaging or therapeutic intensification, CD-related complications, or CD-related subsequent surgery, was significantly shorter in patients with ileal lesions compared to those without, and patients with exclusively ileal lesions had poorer clinical long-term outcomes than patients with exclusively anastomotic lesions. However, patients with anastomotic lesions had poorer clinical long-term outcomes than those without any lesions at the anastomosis or neo-terminal ileum. These data suggest that patients with ileal lesions, including mild ones (RS i1), could benefit from escalation of treatment. In addition, separately characterizing anastomotic and ileal lesions using the REMIND score may provide further data to help predict postoperative long-term outcomes and identify which patients need escalation of medical therapy.
Noninvasive Methods of Evaluating Postoperative Recurrence
Although endoscopy is considered the gold standard for assessing postoperative recurrence in CD, it is costly, more invasive, and bears risks, such as bleeding and perforation [27]. Given these limitations, there is growing literature on the utility of noninvasive methods of identifying disease recurrence [27,28,29]. Systemic inflammatory markers, such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), can be helpful in monitoring response to therapy in acute flares. However, they are less correlated with postoperative endoscopic recurrence [30]. Calprotectin is a Ca-binding antimicrobial protein that is present in proportion to inflammation in body fluids and can be easily quantified in feces [31, 32]. In preoperative CD, fecal calprotectin (FC) levels have been shown to correlate with endoscopic disease activity and are useful surrogate markers for mucosal healing [33, 34].
Given these promising data, several studies have evaluated the role of FC in postoperative CD. In a meta-analysis of 613 patients with postoperative CD, the pooled sensitivity and specificity values of FC for detecting endoscopic recurrence were high at 0.82 (95% confidence interval (CI) 0.73–0.89, 8 studies, n = 391) and 0.61 (95% CI 0.51–0.71), respectively [35]. In an analysis of 135 participants from the randomized, multicenter Postoperative Crohn’s Endoscopic Recurrence (POCER) trial that evaluated the ability of endoscopic evaluations and step-up treatment to prevent CD recurrence after surgery, FC levels were measured before surgery and at 6, 12, and 18 months after resection [27]. The median FC level was higher in patients with disease recurrence (RS ≥ i2) than in patients with remission at 6 months after surgery (275 vs. 72 μg/g, respectively; P < 0.001) and levels of FC > 100 μg/g indicated endoscopic recurrence with 89% sensitivity and 58% specificity. In patients with endoscopic recurrence at 6 months who stepped-up treatment, FC levels decreased over the 18-month period. This study elucidated the value of monitoring FC after surgery, especially with regard to predicting relapse and performing early endoscopic evaluation with step-up treatment, if indicated. Similarly, in a prospective cohort study of 99 patients with CD who underwent ileocolonic resection, FC levels were higher in patients with endoscopic recurrence compared to those in remission (median FC 196.5 μg/g vs. 42.1 μg/g; P < 0.001) [36]. Interestingly, the median FC for recurrent disease using RS ≥ i2 was lower than recurrence when using mRS ≥ i2b (excludes anastomotic lesions), suggesting that FC has increased sensitivity and accuracy when endoscopic recurrence based only on anastomotic lesions is excluded.
In a more recent study of 61 patients who had undergone ileocolonic resection for CD, FC, acute phase reactants [CRP, fibrinogen, white blood cell count (WBC), and platelet count], and plasma cytokines [interleukin (IL)-1β, IL-2, IL-6, IL-10, IL-12p70, IL-13, tumor necrosis factor (TNF)-α, interferon (IFN)-γ] were measured before surgery and at various time points during the postoperative follow-up [37]. Higher FC values were significantly associated with risk of postoperative endoscopic recurrence (mRS ≥ i2b) over time. Endoscopic recurrence was best predicted by FC ≥ 160 μg/g at 6 months after surgery (85% sensitivity, 70% specificity, 26% predictive positive value, 98% negative predictive value) and combined values of FC, IL-6, and IFN-γ levels at 6 months postoperatively had a high predictive capacity to assess the risk of early recurrence [area under the curve (AUC) 0.90]. Therefore, FC in combination with other serologic markers can be beneficial in predicting and monitoring postoperative recurrence and may better assist in identifying which patients need further endoscopic evaluation and escalation of medical therapy; however, further studies are necessary to assess whether these markers can replace endoscopy as primary evaluation [29].
Other minimally invasive diagnostic methods, such as transabdominal ultrasound (TUS), small intestine contrast ultrasound (SICUS), contrast-enhanced ultrasound (CEUS), and CT or MR enterography (CTE/MRE), may be helpful in predicting and assessing postoperative recurrence. SICUS is performed after oral ingestion of contrast solution and can visualize both established CD lesions as well as minor changes in the small bowel wall [38]. CEUS uses intravenous contrast which allows for evaluation of intestinal wall vasculature and can estimate inflammatory activity in CD [39]. In a recent systematic review with meta-analysis of 10 studies with 536 patients with postoperative recurrence, accuracy of TUS, SICUS, and CEUS was evaluated [40]. US had high sensitivity (94%; 95% CI 86%–97%) and specificity (84%; 95% CI 62%–94%) in the diagnosis of postoperative recurrence in comparison with endoscopy as the reference standard, and sensitivity of SICUS was higher and specificity was lower than that of TUS, possibly due to the pressure/distension of the bowel wall produced by luminal contrast. Only one study of CEUS was included in the analysis and in combination with B-mode US (assessment of parietal thickness and presence of transmural complications), it had high sensitivity, specificity, and accuracy in the diagnosis of endoscopic recurrence at 98%, 100%, and 98.3%, respectively [41]. An additional study evaluating this method found that the presence of wall thickness (WT) ≥ 6 mm or WT between 5 and 6 mm with bowel wall contrast enhancement ≥ 70% or extra-intestinal perforating complications had the best results for grading recurrence (sensitivity, specificity, and accuracy of 90.3%, 87%, and 88.9%, respectively) [42]. These findings suggest that US has a high sensitivity and specificity for the diagnosis of postoperative recurrence. The European Crohn’s and Colitis Organization guidelines have defined it as an emerging assessment tool for identifying postoperative recurrence with strong inter-operator reliability [43]. However, small bowel ultrasound has yet to be established in the USA and specialized training will be required with validated activity scores [44, 45].
Cross-sectional imaging, such as CTE and MRE, has also been shown to predict postoperative recurrence in CD. In a prospective study of 30 patients with suspected CD recurrence after surgical resection, MR enteroclysis (similar to MRE, however, oral contrast is administered via nasojejunal tube) and endoscopy were performed and compared [46]. An MR score was developed characterizing severity of findings related to CD and was shown to have high agreement with the RS. Similarly, in a meta-analysis of 76 patients from 3 studies assessing postoperative recurrence in CD, the pooled sensitivity and specificity for MRE were high at 97% and 84%, respectively with excellent accuracy (AUC 0.98), suggesting that MRE may provide an accurate assessment of postoperative endoscopic recurrence in CD [47]. Similar findings have been shown with CTE. In a prospective analysis of 32 patients with CD with ileocolic resection, ileocolonoscopy and CTE were performed within 1 week of each other and there was a good correlation between endoscopic and CTE recurrence (r = 0.782, P < 0.0001) [48]. A more recent study analyzed a subgroup of 31 patients who underwent both ileocolonoscopy and CTE within 1 month of each other for surveillance of CD recurrence postoperatively and the sensitivity and specificity of CTE were 92.3% and 83.3%, respectively [49]. CT enteroclysis has also been shown to help differentiate between disease recurrence and fibrostenosis at the anastomotic site after ileocolic resection for CD. The two most discriminating variables they discovered in the differentiation between anastomotic recurrence and fibrostenosis was the comb sign (P = 0.026) and stratification (P < 0.001) [50]. These noninvasive methods can both predict postoperative recurrence and provide additional information alongside endoscopy, especially with regard to stricturing behavior and evaluation of areas that are not visualized on endoscopy. However, the utility of these methods needs to be further evaluated in larger studies.
Postoperative Prophylactic Medical Therapy
In addition to postoperative evaluation, initiation of medical therapy is crucial in preventing recurrence. The decision to start medical treatment post-surgery is based off of the strongest risk factors for recurrence, which include age < 30 years, active smoking, and at least 2 prior surgeries for penetrating and/or perianal disease and treatment is usually initiated around 2–4 weeks after surgery [2,3,4]. Nitroimidazole antibiotics have been shown to prevent early endoscopic recurrence and delay clinical recurrence. However, their long-term use is limited by drug effects and toxicity and therefore only recommended for 3 months [51,52,53]. In three randomized controlled trials, thiopurines reduced the risk of clinical relapse at 12–36 months [pooled relative risk (RR) 0.79; 95% CI 0.67–0.92; I2 = 0%; GRADE moderate certainty evidence], but did not prevent endoscopic relapse in two of these studies (pooled RR 0.85; 95% CI 0.64–1.13; I2 = 62%; GRADE low certainty evidence) [54,55,56,57]. Interestingly, in the Mercaptopurine versus Placebo to Prevent Recurrence of Crohn's Disease after Surgical Resection (TOPPIC) trial, thiopurines were effective in preventing postoperative clinical recurrence in smokers only [55].
In terms of biologic therapy, the Prospective, Multicenter, Randomized, Double-Blind, Placebo-Controlled Trial Comparing Remicade (infliximab) and Placebo in the Prevention of Recurrence in Crohn's Disease Patients Undergoing Surgical Resection Who Are at an Increased Risk of Recurrence (PREVENT) study was the first randomized controlled trial to assess postoperative clinical and endoscopic recurrence after anti-TNFα therapy compared to placebo [58]. Patients were randomly assigned (1:1) to infliximab (5 mg/kg) or placebo every 8 weeks within 45 days of surgical resection. The primary endpoint was a composite of clinical recurrence defined as CD Activity Index (CDAI) score > 200 and a ≥ 70-point increase above baseline AND endoscopic recurrence with RS of ≥ i2 or fistula/abscess development before or at week 76. The major secondary endpoint was endoscopic recurrence of CD before or at week 76. Although treatment was planned for a maximum of 208 weeks, the study was terminated after week 104 because the composite outcome was not met. Infliximab reduced endoscopic recurrence at 76 weeks (absolute risk reduction, 29.4%; P < 0.001). However, it was not significantly superior to placebo in preventing clinical recurrence. These results further confirm the well-established concept that clinical and endoscopic disease activity in patients with CD do not correlate.
Although the PREVENT study showed the benefit of infliximab in reducing postoperative endoscopic recurrence, the differing results with regard to clinical and endoscopic recurrence resulted in a failure to achieve the primary composite endpoint, which in turn resulted in premature termination of the study and may not have provided enough time for clinical complications to develop [59]. In addition, this composite endpoint has not been validated in previous studies, and therefore, interpretation of these data is unclear. Lastly, this study used every 8-week dosing for infliximab without induction and did not evaluate the use of infliximab continuously through surgery or check drug levels, which may have compromised optimal dosing.
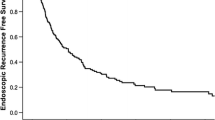
The POCER trial aimed to identify the optimal strategy to prevent disease recurrence and compared active management based on risk of postoperative recurrence and adjustment of therapy according to endoscopic findings to standard care [60]. In this trial, all patients with CD who underwent surgery were treated with 3 months of metronidazole therapy and those at high risk of recurrence (smoking, fistulizing disease, or prior resection) also received a thiopurine or adalimumab if they were intolerant to thiopurines. They were then randomized (2:1) to colonoscopy at 6 months (active care) or no colonoscopy (standard care). In the active care group, if patients were found to have endoscopic recurrence with RS ≥ i2 at 6 months, therapy was stepped-up to thiopurine, adalimumab every 2 weeks with thiopurine, or weekly adalimumab (after induction). The primary endpoint was endoscopic recurrence at 18 months. At 18 months, endoscopic recurrence occurred in 49% of patients in the colonoscopy (active care) arm and 67% in the no colonoscopy (standard of care) arm (modified intention-to-treat, P = 0.03). Smokers had a significantly higher risk of endoscopic recurrence than nonsmokers. As expected, there was no correlation between clinical recurrence defined by CDAI score > 200 or CDAI score > 150 and endoscopic recurrence.
The POCER trial showed that treating according to risk of recurrence, with assessment with 6-month colonoscopy and treatment step-up for endoscopic recurrence, is significantly better than optimum drug therapy alone for prevention of postoperative recurrence of Crohn’s disease. In addition, this strategy of detecting and treating based on endoscopic recurrence is more effective than waiting for clinical recurrence [61]. Interestingly, more than 80% of patients across both the active and standard care groups were considered high risk. Further studies are needed to validate risk stratification, especially as there are additional important risk factors for postoperative recurrence as mentioned above. The PREVENT and POCER trials both show that proactive monitoring for endoscopic recurrence and active management is crucial in preventing postoperative recurrence. However, optimal medical treatment after surgery is still unclear, especially with regard to combination therapy, need for re-induction, and timing of when to start treatment postoperatively.
In order to determine whether preoperative treatment with anti-TNFα therapy influenced postoperative response, Shinagawa et al. [62] performed a sub-analysis within their large multicenter retrospective analysis of 1871 patients with CD who underwent intestinal resection before and after anti-TNFα therapy was introduced in Japan in 2002. In the overall multivariable analysis, the postoperative use of immunomodulators (IM) (hazard ratio (HR) 0.60; 95% CI 0.44–0.81) and anti-TNFα therapy (HR, 0.71; 95% CI, 0.57–0.88) was associated with a lower reoperation rate. In addition, the reoperation rate was lowest in patients on combination therapy with IM and anti-TNFα therapy and highest in those who did not receive either of the drugs [(anti-TNFα + and IM +): 12.4% vs. (anti-TNFα + and IM −): 19.0% vs. (anti-TNFα − and IM −): 26.3%; P = 0.002)]. After stratifying patients by anti-TNFα exposure prior to surgery, the postoperative administration of anti-TNFα was found to be effective in the biologic-naive group with lower reoperation rates, but not in the group that failed biologic therapy before operation. Therefore, determining optimal postoperative prophylaxis strategy for biologic-experienced patients requires further exploration.
Lastly, the role of other biologics such as ustekinumab and vedolizumab in postoperative maintenance remains unclear and these are generally reserved for patients who have failed anti-TNFα therapy or are restricted by specific contraindications to anti-TNFα agents that do not impact use of other biologic agents [29]. A single retrospective study of patients with CD who underwent surgery sought to investigate the use of vedolizumab in the postoperative setting [63]. Of the patients who received vedolizumab postoperatively, 91% had previous use of anti-TNFα agents. At 6–12 months of follow-up, rates of clinical (Harvey–Bradshaw index ≤ 4) and serological (CRP < 3 mg/L) remission were similar among patients receiving vedolizumab or anti-TNFα agents (52% vs. 63%, P = 0.50; 50% vs. 62%, P = 0.43, respectively). However, the rate of endoscopic remission as defined by simple endoscopic score for CD (SES-CD) of 0 was significantly lower in the vedolizumab group compared to the anti-TNFα group (25% vs. 66%, P = 0.01). In a small clinical practice cohort of patients with CD from the ENEIDA registry who were prescribed vedolizumab or ustekinumab within the first 3 months after surgery, postoperative endoscopic recurrence (RS > i1) occurred in 40% of patients on vedolizumab and 58% of those on ustekinumab, similar to that reported with anti-TNFα agents [64, 65]. Interestingly, 17% of patients on each of these medications were on concomitant immunosuppressants and no data were provided on preoperative anti-TNFα use. Further investigation with randomized controlled trials is required before determining the utility of other biologics in preventing postoperative recurrence of CD.
Surgical Methods and Postoperative Recurrence
As most of the disease activity after surgery occurs near the original surgical anastomosis, the type of anastomotic configuration and luminal diameter has also been implicated in the development of postoperative recurrence. Currently, a wide lumen configuration with a stapled side-to-side anastomosis is favored as it may prevent early stenosis, colonic reflux, fecal stasis, and secondary ischemia and has been associated with reduced overall postoperative complications, especially anastomotic leaks [66,67,68,69]. However, the American Society of Colon and Rectal Surgeons (ASCRS) guidelines published in 2020 suggest that reconstruction following ileocecal resection using side-to-side, side-to-end, or end-to-end handsewn or stapled anastomosis should be based on surgeon preference and experience, as the data regarding anastomotic technique, leak, and recurrence are conflicting (strong recommendations based on low-quality evidence) [70].
The Kono-S anastomosis is a newer antimesenteric functional end-to-end configuration that has been proposed to reduce postoperative recurrence [71]. This technique involves transecting the bowel with a linear cutter so that the mesentery side is located in the center (mesenteric preservation) and both stumps are then sutured to create a supporting column to maintain the diameter and dimension of the anastomosis (Fig. 1). Longitudinal enterotomies are then made to the antimesenteric sides of the two segments, and the side-to-side antimesenteric anastomosis is performed in a transverse fashion. Creating a supporting column immediately behind the posterior wall of the anastomosis prevents distortion of the lumen of the anastomosis and alterations of the fecal stream, especially on the mesenteric side which is often the initial site of macroscopic recurrence [66, 72, 73].
Surgical Technique of Kono-S Anastomosis. a Bowel resection is accomplished using a linear staple cutter such that the mesentery side is located in the center of the stump. b Each bowel stump is reinforced with sutures. c Both stumps are sutured together to create a supporting column to maintain the diameter and dimension of the anastomosis. Longitudinal enterotomies are made at the antimesenteric sides of the two segments of intestine, which is indicated by the dotted lines. d The side-to-side antimesenteric anastomosis is then performed in transverse fashion. e The supporting column is located between the anastomosis and the mesentery when the anastomosis is completed.
In the first study evaluating this method, Kono et al. [71] performed a retrospective analysis of 69 patients who underwent Kono-S anastomosis between 2003 and 2009 and compared this cohort to 72 patients who underwent a conventional side-to-side anastomosis. The median endoscopic recurrence score in the Kono-S group was significantly lower than that in the conventional group (RS i2.6 vs. i3.4; P = 0.008), and surgical recurrence at 5 years was also lower in Kono-S group (0% compared to 15%; P = 0.0013). Another retrospective study of 215 patients by the same authors compared the Kono-S anastomosis to end-to-end anastomosis over a 10 year period [74]. The 5-year surgery-free survival rate at the anastomosis site with Kono-S anastomosis was significantly higher than that with end-to-end anastomosis (95% vs. 81%; P < 0.001).
The surgical prevention of anastomotic recurrence by excluding mesentery in Crohn’s disease (SuPREMe-CD) study was the first to randomize 79 patients with ileocolic CD to Kono-S group anastomosis compared to a conventional stapled side-to-side anastomosis [75]. After 6 months postoperatively, endoscopic recurrence (RS ≥ i2) and severe (RS ≥ i3) were significantly lower in the Kono-S compared to the conventional group. After 24 months, clinical recurrence was lower in the Kono-S group compared to the conventional group (18% vs. 30%, P = 0.04, OR 3.47). Surgical recurrence was not significantly different between the two groups (0% in Kono-S group vs. 4.6% in conventional group, P = 0.3). Although these results are promising, further studies should look at long-term follow-up and there is currently one ongoing multicenter trial comparing the Kono-S anastomosis and side-to-side functional end anastomosis with up to 60 months evaluation [76].
Another surgical method currently being explored is a radical resection of the mesentery given the concern that the mesentery may play a pathologic role in CD [77]. Coffey et al. investigated this theory by comparing 30 patients who underwent conventional ileocolic resection where mesentery was divided flush with the intestine (Cohort A) to 34 patients who underwent resection which included excision of the mesentery (Cohort B) [78]. Cumulative reoperation rates were significantly lower in Cohort B compared to A (2.9% vs. 40%, P = 0.003). Based on these results, an international, multicenter, randomized controlled trial was developed to compare extensive mesenteric excision to limited mesenteric excision and currently undergoing recruitment [79, 80].
Conclusion
In patients with CD who have undergone intestinal surgery, early evaluation for endoscopic recurrence has been shown to improve outcomes. There is still controversy on how to best characterize these lesions in the neo-terminal ileum and anastomosis and the risk of progression. In addition, the recommendation for postoperative medical therapy continues to evolve with the addition of new biologic therapies. Lastly, new surgical modalities to reduce postoperative recurrence are currently being explored with preliminary data suggesting that an antimesenteric functional end-to-end anastomosis (Kono-S) can decrease postoperative recurrence.
References
Cosnes J, Gowerrousseau C, Seksik P, Cortot A. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011;140:1785-1794.e4.
Ng SC, Shi HY, Hamidi N et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390:2769–2778.
Nguyen GC, Loftus EV, Hirano I et al. American gastroenterological association institute guideline on the management of Crohn’s disease after surgical resection. Gastroenterology. 2017;152:271–275.
Frolkis AD, Dykeman J, Negrón ME et al. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology. 2013;145:996–1006.
Rutgeerts P, Peeters M, Hiele M et al. Effect of faecal stream diversion on recurrence of Crohn’s disease in the neoterminal ileum. Lancet. 1991;338:771–774.
Rutgeerts P, Geboes K, Vantrappen G, Kerremans R, Coenegrachts JL, Coremans G. Natural history of recurrent Crohns disease at the ileocolonic anastomosis after curative surgery. Gut. 1984;25:665–672.
D’Haens GR, Geboes K, Peeters M, Baert F, Penninckx F, Rutgeerts P. Early lesions of recurrent Crohn’s disease caused by infusion of intestinal contents in excluded ileum. Gastroenterology. 1998;114:262–267.
Ryan WR, Allan RN, Yamamoto T, Keighley MRB. Crohn’s disease patients who quit smoking have a reduced risk of reoperation for recurrence. Am J Surg. 2004;187:219–225.
Reese GE, Nanidis T, Borysiewicz C, Yamamoto T, Orchard T, Tekkis PP. The effect of smoking after surgery for Crohn’s disease: a meta-analysis of observational studies. Int J Colorectal Dis. 2008;23:1213–1221.
Beaugerie L, Seksik P, Nion-Larmurier I, Gendre JP, Cosnes J. Predictors of Crohn’s disease. Gastroenterology. 2006;130:650–656.
Simillis C, Yamamoto T, Reese GE et al. A meta-analysis comparing incidence of recurrence and indication for reoperation after surgery for perforating versus nonperforating Crohn’s disease. Am J Gastroenterol. 2008;103:196–205.
Sachar DB, Lemmer E, Ibrahim C et al. Recurrence patterns after first resection for stricturing or penetrating Crohn’s disease. Inflamm Bowel Dis. 2009;15:1071–1075.
Bernell O, Lapidus A, Hellers G. Risk factors for surgery and postoperative recurrence in Crohn’s disease. Ann Surg. 2000;231:38–45.
Alvarez-Lobos M, Arostegui JI, Sans M et al. Crohn’s disease patients carrying Nod2/CARD15 gene variants have an increased and early need for first surgery due to stricturing disease and higher rate of surgical recurrence. Ann Surg. 2005;242:693–700.
Tandon P, Malhi G, Abdali D et al. Active margins, plexitis, and granulomas increase postoperative Crohn’s recurrence: systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2021;19:451–462.
Sokol H, Pigneur B, Watterlot L et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc Natl Acad Sci U S A. 2008;105:16731–16736.
Dey N, Soergel DAW, Repo S, Brenner SE. Association of gut microbiota with post-operative clinical course in Crohn’s disease. BMC Gastroenterol. 2013. https://doi.org/10.1186/1471-230X-13-131.
De Cruz P, Kang S, Wagner J et al. Association between specific mucosa-associated microbiota in Crohn’s disease at the time of resection and subsequent disease recurrence: a pilot study. J Gastroenterol Hepatol. 2015;30:268–278.
Wright EK, Kamm MA, Wagner J et al. Microbial factors associated with postoperative Crohn’s disease recurrence. J Crohns Colitis. 2017;11:191–203.
Sokol H, Brot L, Stefanescu C et al. Prominence of ileal mucosa-associated microbiota to predict postoperative endoscopic recurrence in Crohn’s disease. Gut. 2019. https://doi.org/10.1136/gutjnl-2019-318719.
Rutgeerts P, Geboes K, Vantrappen G, Beyls J, Kerremans R, Hiele M. Predictability of the postoperative course of Crohn’s disease. Gastroenterology. 1990;99:956–963.
Ma C, Gecse KB, Duijvestein M et al. Reliability of endoscopic evaluation of postoperative recurrent Crohn’s disease. Clin Gastroenterol Hepatol. 2020;18:2139–2141.
Rivière P, Vermeire S, Irles-Depe M et al. No change in determining Crohn’s disease recurrence or need for endoscopic or surgical intervention with modification of the Rutgeerts’ scoring system. Clin Gastroenterol Hepatol. 2019;17:1643–1645.
Ollech JE, Aharoni-Golan M, Weisshof R et al. Differential risk of disease progression between isolated anastomotic ulcers and mild ileal recurrence after ileocolonic resection in patients with Crohn’s disease. Gastrointest Endosc. 2019;90:269–275.
Hammoudi N, Auzolle C, Tran Minh ML et al. Postoperative endoscopic recurrence on the neoterminal ileum but not on the anastomosis is mainly driving long-term outcomes in Crohn’s disease. Am J Gastroenterol. 2020;115:1084–1093.
Hirten RP, Ungaro RC, Castaneda D et al. Anastomotic ulcers after ileocolic resection for Crohn’s disease are common and predict recurrence. Inflamm Bowel Dis. 2020;26:1050–1058.
Wright EK, Kamm MA, De Cruz P et al. Measurement of fecal calprotectin improves monitoring and detection of recurrence of Crohn’s disease after surgery. Gastroenterology. 2015;148:938-947.e1.
Biancone L, Onali S, Calabrese E et al. Non-invasive techniques for assessing postoperative recurrence in Crohn’s disease. Dig Liver Dis. 2008;40:S265–S270.
Barnes EL, Lightner AL, Regueiro M. Perioperative and postoperative management of patients with Crohn’s disease and ulcerative colitis. Clin Gastroenterol Hepatol. 2020;18:1356–1366.
Yamamoto T, Shimoyama T. Monitoring and detection of disease recurrence after resection for Crohn’s disease: The role of non-invasive fecal biomarkers. Expert Rev Gastroenterol Hepatol. 2017;11:899–909.
Steinbakk M, Naess-Andresen CF, Fagerhol MK, Lingaas E, Dale I, Brandtzaeg P. Antimicrobial actions of calcium binding leucocyte L1 protein, calprotectin. Lancet. 1990;336:763–765.
Røseth AG, Fagerhol MK, Aadland E, Schjønsby H. Assessment of the neutrophil dominating protein calprotectin in feces: a methodologic study. Scand J Gastroenterol. 1992;27:793–798.
D’Haens G, Ferrante M, Vermeire S et al. Fecal calprotectin is a surrogate marker for endoscopic lesions in inflammatory bowel disease. Inflamm Bowel Dis. 2012;18:2218–2224.
Sipponen T, Savilahti E, Kärkkäinen P et al. Fecal calprotectin, lactoferrin, and endoscopic disease activity in monitoring anti-TNF-alpha therapy for Crohn’s disease. Inflamm Bowel Dis. 2008;14:1392–1398.
Qiu Y, Mao R, Chen BL et al. Fecal calprotectin for evaluating postoperative recurrence of Crohn’s disease: a meta-analysis of prospective studies. Inflamm Bowel Dis. 2015;21:315–322.
Lopes S, Andrade P, Afonso J et al. Correlation between calprotectin and modified rutgeerts score. Inflamm Bowel Dis. 2016;22:2173–2181.
Cerrillo E, Moret I, Iborra M et al. A nomogram combining fecal calprotectin levels and plasma cytokine profiles for individual prediction of postoperative Crohn’s disease recurrence. Inflamm Bowel Dis. 2019;25:1681–1691.
Calabrese E, Maaser C, Zorzi F et al. Bowel ultrasonography in the management of Crohn’s disease. A review with recommendations of an international panel of experts. Inflamm Bowel Dis. 2016;22:1168–1183.
Migaleddu V, Quaia E, Scano D, Virgilio G. Inflammatory activity in Crohn disease: ultrasound findings. Abdom Imaging. 2008;33:589–597.
Rispo A, Imperatore N, Testa A et al. Diagnostic accuracy of ultrasonography in the detection of postsurgical recurrence in Crohn’s disease: a systematic review with meta-analysis. Inflamm Bowel Dis. 2018;24:977–988.
Paredes JM, Ripollés T, Cortés X et al. Contrast-enhanced ultrasonography: usefulness in the assessment of postoperative recurrence of Crohn’s disease. J Crohn’s Colitis. 2013;7:192–201.
Martínez MJ, Ripollés T, Paredes JM, Moreno-Osset E, Pazos JM, Blanc E. Intravenous contrast-enhanced ultrasound for assessing and grading postoperative recurrence of Crohn’s disease. Dig Dis Sci. 2019;64:1640–1650 https://doi.org/10.1007/s10620-018-5432-6.
Gionchetti P, Dignass A, Danese S et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: part 2: surgical management and special situations. J Crohn’s Colitis. 2017;11:135–149.
Maaser C, Kucharzik T, Gecse K. Is intestinal ultrasound ready to be used as standard monitoring tool in daily practice and as endpoint in clinical trials? J Crohn’s Colitis. 2021;15:1–2.
Goodsall TM, Jairath V, Feagan BG et al. Standardisation of intestinal ultrasound scoring in clinical trials for luminal Crohn’s disease. Aliment Pharmacol Ther. 2021;53:873–886.
Sailer J, Peloschek P, Reinisch W, Vogelsang H, Turetschek K, Schima W. Anastomotic recurrence of Crohn’s disease after ileocolic resection: comparison of MR enteroclysis with endoscopy. Eur Radiol. 2008;18:2512–2521.
Yung DE, Har-Noy O, Tham YS et al. Capsule endoscopy, magnetic resonance enterography, and small bowel ultrasound for evaluation of postoperative recurrence in Crohn’s disease: systematic review and meta-analysis. Inflamm Bowel Dis. 2018;24:93–100.
Mao R, Gao X, Zhu ZH et al. CT Enterography in evaluating postoperative recurrence of crohn’s disease after ileocolic resection: complementary role to endoscopy. Inflamm Bowel Dis. 2013;19:977–982.
Choi IY, Park SH, Park SH et al. CT enterography for surveillance of anastomotic recurrence within 12 months of bowel resection in patients with crohn’s disease: an observational study using an 8-year registry. Korean J Radiol. 2017;18:906–914.
Soyer P, Boudiaf M, Sirol M et al. Suspected anastomotic recurrence of Crohn disease after ileocolic resection: evaluation with CT enteroclysis. Radiology. 2010;254:755–764.
Rutgeerts P, Hiele M, Geboes K et al. Controlled trial of metronidazole treatment for prevention of Crohn’s recurrence after ileal resection. Gastroenterology. 1995;108:1617–1621.
Rutgeerts P, Van Assche G, Vermeire S et al. Ornidazole for prophylaxis of postoperative Crohn’s disease recurrence: a randomized, double-blind, placebo-controlled trial. Gastroenterology. 2005;128:856–861.
Doherty GA, Bennett GC, Cheifetz AS, Moss AC. Meta-analysis: targeting the intestinal microbiota in prophylaxis for post-operative Crohn’s disease. Aliment Pharmacol Ther. 2010;31:802–809.
Gjuladin-Hellon T, Iheozor-Ejiofor Z, Gordon M, Akobeng AK. Azathioprine and 6-mercaptopurine for maintenance of surgically-induced remission in crohn’s disease. Cochrane Database Syst Rev. 2019. https://doi.org/10.1002/14651858.CD010233.pub3.
Mowat C, Arnott I, Cahill A et al. Mercaptopurine versus placebo to prevent recurrence of Crohn’s disease after surgical resection (TOPPIC): a multicentre, double-blind, randomised controlled trial. Lancet Gastroenterol Hepatol. 2016;1:273–282.
D’Haens GR, Vermeire S, Van Assche G et al. Therapy of metronidazole with azathioprine to prevent postoperative recurrence of Crohn’s disease: a controlled randomized trial. Gastroenterology. 2008;135:1123–1129.
Hanauer SB, Korelitz BI, Rutgeerts P et al. Postoperative maintenance of Crohn’s disease remission with 6-mercaptopurine, mesalamine, or placebo: a 2-year trial. Gastroenterology. 2004;127:723–729.
Regueiro M, Feagan BG, Zou B et al. Infliximab reduces endoscopic, but not clinical, recurrence of Crohn’s disease after ileocolonic resection. Gastroenterology. 2016;150:1568–1578.
Ghosh S, D’Haens G. Is an ounce of prevention worth a pound of cure: postoperative recurrence of Crohn’s disease? Gastroenterology. 2016;150:1521–1524.
De Cruz P, Kamm MA, Hamilton AL et al. Crohn’s disease management after intestinal resection: a randomised trial. Lancet. 2015;385:1406–1417.
Vuitton L, Peyrin-Biroulet L. The POCER trial: bet on active care. Gastroenterology. 2015;148:1474–1475.
Shinagawa T, Hata K, Ikeuchi H et al. Rate of reoperation decreased significantly after year 2002 in patients with Crohn’s disease. Clin Gastroenterol Hepatol. 2020;18:898-907.e5.
Yamada A, Komaki Y, Patel N et al. The use of vedolizumab in preventing postoperative recurrence of Crohn’s disease. Inflamm Bowel Dis. 2018;24:502–509.
Mañosa Ciria M, Hinojosa E, Carbajo A et al. P681 Efficacy of vedolizumab for the prevention of postoperative recurrence in Crohn’s disease: Data from clinical practice from the ENEIDA registry. J Crohn’s Colitis. 2020;14:S554–S555.
Mañosa Ciria M, Fernandez-Clotet A, Hernández-Camba A et al. P462 Efficacy of ustekinumab for the prevention of postoperative recurrence in crohn’s disease. Data from clinical practice from the eneida registry. J Crohn’s Colitis. 2020;14:S410–S410.
Alshantti A, Hind D, Hancock L, Brown SR. The role of Kono-S anastomosis and mesenteric resection in reducing recurrence after surgery for Crohn’s disease: a systematic review. Color Dis. 2021;23:7–17.
Brown SR, Fearnhead NS, Faiz OD et al. The Association of Coloproctology of Great Britain and Ireland consensus guidelines in surgery for inflammatory bowel disease. Color Dis. 2018;20:3–117.
Simillis C, Purkayastha S, Yamamoto T, Strong SA, Darzi AW, Tekkis PP. A meta-analysis comparing conventional end-to-end anastomosis vs. other anastomotic configurations after resection in Crohn’s disease. Dis Colon Rectum. 2007;50:1674–1687.
He X, Chen Z, Huang J, Lian L et al. Stapled side-to-side anastomosis might be better than handsewn end-to-end anastomosis in ileocolic resection for Crohn’s disease: a meta-analysis. Dig Dis Sci. 2014;59:1544–1551 https://doi.org/10.1007/s10620-014-3039-0.
Lightner AL, Vogel JD, Carmichael JC et al. The American Society of colon and rectal surgeons clinical practice guidelines for the surgical management of Crohn’s disease. Dis Colon Rectum. 2020;63:1028–1052.
Kono T, Ashida T, Ebisawa Y et al. A new antimesenteric functional end-to-end handsewn anastomosis: surgical prevention of anastomotic Recurrence in Crohn’s disease. Dis Colon Rectum. 2011;54:586–592.
Anthony A, Dhillon AP, Pounder RE, Wakefield AJ. Ulceration of the ileum in Crohn’s disease: correlation with vascular anatomy. J Clin Pathol. 1997;50:1013–1017.
Kono T, Fichera A. Surgical treatment for Crohn’s disease: a role of Kono-S anastomosis in the west. Clin Colon Rectal Surg. 2020;33:335–343.
Shimada N, Ohge H, Kono T et al. Surgical recurrence at anastomotic site after bowel resection in Crohn’s disease: comparison of Kono-S and end-to-end anastomosis. J Gastrointest Surg. 2019;23:312–319.
Luglio G, Rispo A, Imperatore N et al. Surgical prevention of anastomotic recurrence by excluding mesentery in Crohn’s disease: the SuPREMe-CD study—a randomized clinical trial. Ann Surg. 2020;272:210–217.
Study of the Kono-S anastomosis versus the side-to-side functional end anastomosis [Internet]. Available from: https://clinicaltrials.gov/ct2/show/NCT03256240
Coffey JC, O’Leary DP, Kiernan MG, Faul P. The mesentery in Crohn’s disease: friend or foe? Curr Opin Gastroenterol. 2016;32:267–273.
Coffey CJ, Kiernan MG, Sahebally SM et al. Inclusion of the mesentery in ileocolic resection for Crohn’s disease is associated with reduced surgical recurrence. J Crohn’s Colitis. 2018;12:1139–1150.
Li Y, Mohan H, Lan N et al. Mesenteric excision surgery or conservative limited resection in Crohn’s disease: study protocol for an international, multicenter, randomized controlled trial. Trials. 2020;21:210.
Postoperative Progression of the Disease Following Extensive Versus Limited Mesenteric Excision for Crohn’s Disease [Internet]. Available from: https://clinicaltrials.gov/ct2/show/NCT03769922
Fleshner P. Operative management of Crohn disease of the small bowel, colon, and rectum. In: Post T, editor. UpToDate. Waltham, MA: UpToDate Inc.Available from: https://www.uptodate.com
Funding
Corrona LLC: Consulting; Abbvie: Speaker’s Bureau; Pfizer: Speaker’s Bureau; Prometheus: Advisory Board.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this review article, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Dasharathy, S.S., Limketkai, B.N. & Sauk, J.S. What’s New in the Postoperative Management of Crohn’s Disease?. Dig Dis Sci 67, 3508–3517 (2022). https://doi.org/10.1007/s10620-021-07205-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-021-07205-w