Abstract
Background
Bacteremic cholangitis carries a high mortality rate of up to 10 % in relation to organ failure (OF), including septic shock.
Aim
The purpose of this study was to elucidate predictive factors for OF in bacteremic cholangitis.
Methods
A retrospective review of all patients diagnosed with acute cholangitis and proven bacteremia from 2003 to 2011 was performed. Comprehensive clinical and laboratory data of 211 patients were analyzed.
Results
There were 42 cases (19.9 %) of OF and 5 deaths (2.4 %). In the multivariate logistic regression analysis, significant predictive factors for OF were successful biliary decompression, presence of extended-spectrum beta-lactamase organism (ESBL), higher total bilirubin, and higher blood urea nitrogen (BUN) level at admission with odds ratios (ORs) of 0.129, 6.793, 1.148, and 1.089, respectively. Subgroup analysis of 165 patients who underwent biliary decompression before an event (with OF: 20, without OF: 145) was performed to elucidate the risk factors for organ failure even after successful biliary drainage. Variables significantly associated with OF included ESBL and BUN (OR = 4.123 and 1.177, respectively). We developed a scoring system with regression coefficient of each significant variable. The organ failure score was calculated using the following equation: (1.4 × ESBL) + (0.2 × BUN). This scoring system for predicting OF was highly sensitive (85.0 %) and specific (83.4 %).
Conclusions
Biliary decompression, ESBL, total bilirubin, and BUN are prognostic determinants in patients with bacteremic cholangitis. An organ failure scoring system may allow clinicians to identify groups with poor prognosis even after successful biliary decompression.
Similar content being viewed by others
Introduction
Acute cholangitis is mainly caused by secondary bacterial infection after gallstone or tumor causes biliary obstruction. It is most often diagnosed from clinical, laboratory, and image findings [1]. The appropriate use of biliary drainage and antibiotics is essential for the treatment of acute cholangitis. If appropriate treatment is not provided, mortality from infection could reach 88–100 % [2, 3]. Due to the recent development of endoscopic retrograde cholangiopancreatography (ERCP) and the appropriate administration of antibiotics, the mortality rate from infection has been decreasing. However, the mortality rate among patients with acute cholangitis is still 5–10 % [4]; and particularly, the mortality rate among patients with bacteremic cholangitis 30 days after their hospitalization is 10 % [5].
Organ failure, including septic shock, is a main prognostic factor related to the mortality of bacteremia [6–10], and previous studies have investigated several factors associated with organ failure in bacteremia. Among demographic and clinical factors, old age, underlying renal disease, and multiple sources of bacteremia have been reported to be the risk factors of organ failure in patients with bacteremia [6, 11].
Cholangitis is distinct from other infectious diseases in some aspects, such as disease course, treatment strategy, etc. According to previous studies on bacteremic cholangitis, organ failure was also reported to be an important prognostic factor of mortality [5, 12]. However, the risk factors of organ failure have not yet been identified in patients with bacteremic cholangitis. Furthermore, it is difficult to predict the development of organ failure in spite of successful biliary drainage as the main treatment.
This study aimed to identify the risk factors of the development of organ failure in patients with bacteremic cholangitis and to develop a prognostic scoring system that can be used to predict organ failure using the risk factors.
Materials and Methods
Study Population
The study initially included all patients with a discharge diagnosis of acute cholangitis from May 2003 through March 2011 using information contained in medical charts and computerized records. If multiple episodes of cholangitis occurred in the same patient, only the first episode of cholangitis was included to ensure statistical independence in the analyses. Of these, patients were excluded for the following reasons: no definite or suspected diagnosis of cholangitis using Tokyo guidelines [13], no proven bacteremia, no initiation or completion of treatment in our hospital, and organ failure that occurred before admission. Individuals were also excluded from this study if they had coagulase-negative Staphylococcus spp., which is the most common skin flora. A chart showing patient selection and study flow is provided in Fig. 1. Finally, 211 patients with bacteremic cholangitis were included for the analysis. The study protocol was approved by the Institutional Review Board (IRB) of Seoul National University Bundang Hospital.
Definitions of Events
The definite or suspected diagnosis of acute cholangitis was made based on the diagnostic criteria for acute cholangitis in the Tokyo guidelines. Bacteremia was defined as the presence of organisms in the blood, documented by at least one positive blood culture. Sepsis was defined as bacteremia with systemic inflammatory response syndrome (SIRS) [14]. Septic shock was defined as sepsis associated with evidence of organ hypoperfusion and arterial systolic blood pressure <90 mmHg refractory to fluid resuscitation or a requirement for the use of vasopressors to maintain blood pressure [14]. All the cases of shock caused by drugs, heart failure, and bleeding were excluded in this definition.
Cases of organ failure [5, 15] that occurred after emergency department (ED) admission manifested as: (1) acute renal failure (ARF)—serum creatinine level >265 μmol/L or, in the case of preexisting renal dysfunction, a doubling of previous serum creatinine values [16, 17]; (2) altered consciousness level—Glasgow coma scale (GCS) score of <12 or a decrease in the GCS score of at least 3 if primary central nervous system injury is present; (3) acute respiratory distress—pulse oxygen saturation <90 % or ventilator care; and (4) septic shock. All patients who already had organ failure on admission were excluded from this study (Fig. 1).
All technically successful endoscopic drainages or percutaneous drainages were considered as “successful biliary decompression”. In patients having multiple procedures, data from only the first procedure were included in the analysis.
Data Collection
The following data were collected for analysis. Clinical and demographic variables included age, sex, body mass index, alcohol, smoking, body temperature, respiratory rate, Charcot’s triad, symptom to door time (time from symptom onset until arrival at the hospital), and Charlson comorbidity index score [18, 19]. Etiologic variables were malignant biliary obstruction, benign biliary stricture, and choledocholithiasis. Microbiological and laboratory variables included causative microorganism, organism resistant to initial antibiotics, white blood cell count, platelet count, prothrombin time, hemoglobin, blood urea nitrogen (BUN), creatinine, aspartate aminotransferase, alanine aminotransferase, total bilirubin, albumin, glucose, C-reactive protein, and total CO2 level at admission. Treatment and outcome variables were successful biliary decompression, visit to decompression time (time from arrival at the hospital until intervention for biliary decompression), and length of hospital stay.
Statistical Analysis
In the univariate analyses, the Mann–Whitney U test and the Pearson χ2 with Fisher exact test were used to compare continuous or discrete variables, respectively. To identify the independent risk factors for the development of organ failure in bacteremic cholangitis patients, stepwise logistic regression analyses were performed. All significant variables at the univariate analysis were entered in the multivariate analysis. In the subgroup analysis, only patients who underwent successful biliary decompression before events were included to adjust for the potential confounding effect. Univariate and multivariate logistic regression analyses were also performed to identify the independent predictor for organ failure. Then, logistic regression coefficients of the factors were ascertained to develop equations (organ failure score) to predict organ failure. Finally, receiver operating curves (ROC) were constructed for the organ failure score to determine a specific threshold value that would optimize its sensitivity and specificity. P < 0.05 for two-sided tests was considered statistically significant. All statistical analyses were performed with SPSS 18.0 (SPSS Inc., Chicago, IL, USA).
Results
The Risk Factors for Organ Failure in Overall Patients with Bacteremic Cholangitis
A total of 211 patients, 31.3 % of whom were female and with a mean age of 67.4 ± 13.7 years, were enrolled. The most common microorganism was Escherichia coli (55.5 %), followed by Klebsiella pneumoniae (18 %), Pseudomonas aeruginosa (8.5 %), Enterobacter species (6.6 %), Enterococcus species (2.8 %), Micrococcus species (2.8 %), Bacillus species (1.9 %), Staphylococcus (1.4 %), Streptococcus (0.5 %), and others (2 %). The overall hospital mortality rate was 2.37 % (n = 5). Within the mortality group, four patients expired due to septic shock, and one patient expired due to respiratory failure.
There were 42 cases (19.9 %) of organ failure, including septic shock (n = 18), respiratory failure (n = 17), ARF (n = 4), and mental change (n = 3). The median time taken to organ failure from the patient’s initial arrival at the hospital was 11.5 h (range 3–498 h). All patients received intravenous antibiotics within the initial 2 h. Biliary decompression was attempted in 192 (91 %) patients and successfully performed in 181 (94.3 %) individuals, of whom 127 (70.2 %) initially received endoscopic drainage, and 54 (29.8 %) received percutaneous drainage. Among the 42 patients who had organ failure, 20 individuals received successful biliary decompression before the event. Among the 169 event-free patients, 145 underwent successful biliary decompression. The mean length of the hospital stay was 20.0 ± 16.4 and 11.8 ± 10.1 days in patients with and without organ failure, respectively (P < 0.001).
Univariate analysis identified 13 variables that were significantly (P < 0.05) associated with organ failure in bacteremic cholangitis (Table 1). Multivariate analysis showed that organ failure was significantly associated with the presence of extended-spectrum beta-lactamase (ESBL) organism, higher total bilirubin, and higher BUN level and was inversely associated with successful biliary decompression (odds ratio = 6.793, 1.148, 1.089, and 0.129, respectively) (Table 1).
The Risk Factors for Organ Failure in Patients Who Underwent Successful Biliary Decompression Due to Bacteremic Cholangitis
Some patients experienced organ failure even after successful biliary decompression. Therefore, to find the risk factors for organ failure in patients who underwent successful biliary decompression, 167 patients who underwent biliary decompression before organ failure were included in this subgroup analysis. Organ failure developed in 20 patients and not in 145 patients. Univariate analysis identified six variables significantly (P < 0.05) associated with organ failure (Table 2). Of these six factors, the presence of ESBL organism and higher BUN level were found to be significantly associated with organ failure in bacteremic cholangitis after multivariate analysis (Table 2).
Proposal of Organ Failure Scoring System in Patients Who Underwent Successful Biliary Decompression Due to Bacteremic Cholangitis
The regression coefficients (standard error) for ESBL and BUN in the multiple logistic regression model to predict the risk of organ failure were 1.416 (0.714) and 0.163 (0.036), respectively. Therefore, the regression equation for predicting organ failure was proposed as the following:
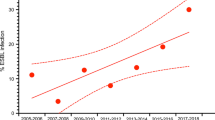
This equation can be used to provide a numerical score that gives prognostic information for bacteremic cholangitis. When dichotomizing the organ failure score to a value ≥4.5 with receiver operating characteristic (ROC) curves, the sensitivity, specificity, accuracy, positive predictive value, and negative predictive value for organ failure in bacteremic cholangitis patients who underwent biliary decompression were 81.8, 83.4, 83.2, 43, and 96.8 %, respectively (Fig. 2). When all 211 bacteremic cholangitis patients were included into the analysis, the score ≥4.5 for predicting organ failure was still highly sensitive and specific (76.2, 81.7 %, respectively).
Receiver operating characteristic (ROC) curves of organ failure score to predict organ failure in bacteremic cholangitis patients who had undergone previously successful biliary decompression. The area under the ROC curves was 0.888 [95 % confidence interval (CI) 0.798–0.978], and the best cut-off point of the organ failure score was 4.5 (sensitivity 85.0 %, specificity 83.4 %)
Discussion
There has been no study to investigate “bacteremia-organ failure sequence” or prognostic factors in bacteremic cholangitis. In this study, multivariate analysis identified four independent factors for organ failure in bacteremic cholangitis: the presence of ESBL organism, higher total bilirubin, and higher BUN level as risk factors, and successful biliary decompression as a protective factor. For patients who experienced organ failure even after successful biliary decompression, we proposed an organ failure scoring system to predict organ failure due to bacteremic cholangitis. The scoring system for predicting organ failure was highly sensitive and specific.
Biliary decompression is a central part in the treatment of acute cholangitis. It was shown that serum and bile endotoxin levels decrease after successful biliary drainage [20]. Moreover, the level of IL-6, which is another inflammatory mediator reported to be associated with the development of multiple organ failure and subsequent poor prognosis [21], in bile was found to be correlated directly with the rate of bilirubin decrease following biliary drainage [22].
The impact of higher bilirubin and subsequent jaundice on the prognosis in bacteremic cholangitis is poorly understood, although it is a sensitive indicator of biliary obstruction. Elevated bilirubin can stimulate oxidative stress and decrease cell survival [23, 24]. Moreover, bilirubin promotes apoptosis in cultured cells [25] and can also induce the inflammatory response, which is further increased when cells are simultaneously exposed to lipopolysaccharide [26]. Recently, it was reported that serum bilirubin levels are associated with the development of acute respiratory distress syndrome (ARDS) and mortality in sepsis [27], which is consistent with our finding.
BUN has been reported to be a prognostic factor in various conditions, including cholangitis [28–30]. BUN levels are known to be strongly influenced by many non-renal factors such as protein intake, dehydration, gastrointestinal bleeding, infection, or steroid use. Therefore, BUN itself is not a valid marker of ARF in humans [31], which supports that it is not a confounding factor in our study. Meanwhile, BUN is an integral marker of tissue necrosis, protein catabolism, and renal function. Those are closely related to organ failure [32, 33]; therefore, our results regarding BUN are explainable.
Previous studies have also investigated the worse prognosis of ESBL organism in relation to severe sepsis or organ failure [34]. Most of the cases were due to inappropriate initial antibiotics use [35, 36]; those findings are compatible with our results. Among the ESBL patients in our study, inappropriate use of initial antibiotics was more frequent in patients with organ failure than in those without organ failure (12/16; 75 % and 5/13; 38.5 %, respectively, P = 0.047). In addition, 10/12 patients who developed organ failure due to ESBL received inappropriate antibiotics, despite previous ESBL history.
Biliary decompression is a main treatment of acute cholangitis. The subgroup analysis involving only patients who underwent biliary decompression before events aimed to identify cases of high risk bacteremic cholangitis that could progress to the development of organ failure even after successful biliary decompression; it was also used to develop a scoring system to predict organ failure. In the subgroup analysis, ESBL organism and baseline BUN level were independent risk factors. Recently, a prompt gram stain has become feasible soon after admission [37]. Although the detection of ESBL organism usually takes a few days in the current clinical practice, new methods have also recently emerged for rapid detection of extended β-lactamase-producing gram-negative bacilli in blood cultures [38–42]. These facts support the clinical relevance of our work, because it has been possible using newly emerging methods to detect “bacteremia” or “ESBL” patients during the early period of hospitalization. In the analysis, the organ failure score developed with two significant factors was highly sensitive and specific for predicting organ failure when dichotomizing the score to a value ≥4.5. This scoring system and cut-off value ≥4.5 would allow clinicians to identify the group with poor prognosis even after biliary decompression. Clinicians could then monitor those patients closely in an intensive care setting with specific treatment strategy. However, the results from subgroup analysis do not support a lower effectiveness of biliary decompression in patients with higher organ failure score. To ascertain that fact, it seems that further studies are needed to identify the outcome of biliary decompression in the population with a higher organ failure score. Unlike biliary drainage, decompression time, itself, was not a significant variable in subgroup analysis. Furthermore, the mean time taken to decompression from the patient’s arrival was longer in patients without organ failure, even though early decompression is crucial for prognosis in cholangitis [43]. That may be due to differences between the two groups (patients with organ failure and without organ failure) in basal characteristics, underlying comorbidities, laboratory findings, etc.
In this study, some patients developed organ failure despite previous biliary decompression. This finding is compatible with those of previous studies [5, 44]. One possible explanation is that rapidly progressed severe endotoxemia results in irreversible tissue hypoxia and necrosis. Some factors, such as volume status, may enhance this process, which could be expressed as a high BUN level. Another explanation is, as we mentioned earlier, inappropriate initial antibiotics therapy. Further large prospective study is needed to reveal the role of the factors we identified in our study in the progression of the “bacteremia-to-organ failure process” despite biliary intervention.
The limitations of this study include the retrospective design without a systemized management protocol and single center experience. However, to the best of our knowledge, our work is the very first study to report prognostic factors in bacteremic cholangitis. A further well designed prospective study is needed to validate the organ failure score.
In conclusion, biliary decompression is a significant protective factor for organ failure in bacteremic cholangitis. ESBL, baseline total bilirubin and BUN are the risk factors for organ failure. In addition, an organ failure scoring system may help clinicians to recognize high-risk cholangitis patients with bacteremia.
References
Yusoff IF, Barkun JS, Barkun AN. Diagnosis and management of cholecystitis and cholangitis. Gastroenterol Clin N Am. 2003;32:1145–1168.
Saik RP, Greenburg AG, Farris JM, Peskin GW. Spectrum of cholangitis. Am J Surg. 1975;130:143–150.
Rogers L. Biliary abscess of the liver with operation. Br Med J. 1903;2:706–707.
Bornman PC, van Beljon JI, Krige JE. Management of cholangitis. J Hepatobiliary Pancreat Surg. 2003;10:406–414.
Lee CC, Chang IJ, Lai YC, Chen SY, Chen SC. Epidemiology and prognostic determinants of patients with bacteremic cholecystitis or cholangitis. Am J Gastroenterol. 2007;102:563–569.
Kang CI, Song JH, Chung DR, et al. Risk factors and pathogenic significance of severe sepsis and septic shock in 2286 patients with gram-negative bacteremia. J Infect. 2011;62:26–33.
Rello J, Ricart M, Mirelis B, et al. Nosocomial bacteremia in a medical-surgical intensive care unit: epidemiologic characteristics and factors influencing mortality in 111 episodes. Intensive Care Med. 1994;20:94–98.
Pittet D, Thievent B, Wenzel RP, Li N, Gurman G, Suter PM. Importance of pre-existing co-morbidities for prognosis of septicemia in critically ill patients. Intensive Care Med. 1993;19:265–272.
Vincent JL, de Mendonca A, Cantraine F, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26:1793–1800.
Ziegler EJ, Fisher CJ Jr, Sprung CL, et al. Treatment of gram-negative bacteremia and septic shock with HA-1A human monoclonal antibody against endotoxin. A randomized, double-blind, placebo-controlled trial. The HA-1A Sepsis Study Group. N Engl J Med. 1991;324:429–436.
Brun-Buisson C, Doyon F, Carlet J. Bacteremia and severe sepsis in adults: a multicenter prospective survey in ICUs and wards of 24 hospitals. French Bacteremia–Sepsis Study Group. Am J Respir Crit Care Med. 1996;154:617–624.
Melzer M, Toner R, Lacey S, Bettany E, Rait G. Biliary tract infection and bacteraemia: presentation, structural abnormalities, causative organisms and clinical outcomes. Postgrad Med J. 2007;83:773–776.
Yokoe M, Takada T, Mayumi T, et al. Accuracy of the Tokyo guidelines for the diagnosis of acute cholangitis and cholecystitis taking into consideration the clinical practice pattern in Japan. J Hepatobiliary Pancreat Sci. 2011;18:250–257.
Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101:1644–1655.
Bone RC, Fisher CJ Jr, Clemmer TP, Slotman GJ, Metz CA, Balk RA. A controlled clinical trial of high-dose methylprednisolone in the treatment of severe sepsis and septic shock. N Engl J Med. 1987;317:653–658.
Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency. Am J Kidney Dis. 2002;39:930–936.
Hou SH, Bushinsky DA, Wish JB, Cohen JJ, Harrington JT. Hospital-acquired renal insufficiency: a prospective study. Am J Med. 1983;74:243–248.
Murray SB, Bates DW, Ngo L, Ufberg JW, Shapiro NI. Charlson Index is associated with one-year mortality in emergency department patients with suspected infection. Acad Emerg Med. 2006;13:530–536.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383.
Lau JY, Chung SC, Leung JW, Ling TK, Yung MY, Li AK. Endoscopic drainage aborts endotoxaemia in acute cholangitis. Br J Surg. 1996;83:181–184.
Pinsky MR, Vincent JL, Deviere J, Alegre M, Kahn RJ, Dupont E. Serum cytokine levels in human septic shock. Relation to multiple-system organ failure and mortality. Chest. 1993;103:565–575.
Akiyama T, Hasegawa T, Sejima T, et al. Serum and bile interleukin 6 after percutaneous transhepatic cholangio-drainage. Hepatogastroenterology. 1998;45:665–671.
Cesaratto L, Calligaris SD, Vascotto C, et al. Bilirubin-induced cell toxicity involves PTEN activation through an APE1/Ref-1-dependent pathway. J Mol Med (Berl). 2007;85:1099–1112.
Ostrow JD, Pascolo L, Brites D, Tiribelli C. Molecular basis of bilirubin-induced neurotoxicity. Trends Mol Med. 2004;10:65–70.
Fernandes A, Falcao AS, Silva RF, et al. Inflammatory signalling pathways involved in astroglial activation by unconjugated bilirubin. J Neurochem. 2006;96:1667–1679.
Fernandes A, Silva RF, Falcao AS, Brito MA, Brites D. Cytokine production, glutamate release and cell death in rat cultured astrocytes treated with unconjugated bilirubin and LPS. J Neuroimmunol. 2004;153:64–75.
Zhai R, Sheu CC, Su L, et al. Serum bilirubin levels on ICU admission are associated with ARDS development and mortality in sepsis. Thorax. 2009;64:784–790.
Leese T, Neoptolemos JP, Baker AR, Carr-Locke DL. Management of acute cholangitis and the impact of endoscopic sphincterotomy. Br J Surg. 1986;73:988–992.
Aronson D, Mittleman MA, Burger AJ. Elevated blood urea nitrogen level as a predictor of mortality in patients admitted for decompensated heart failure. Am J Med. 2004;116:466–473.
Faisst M, Wellner UF, Utzolino S, Hopt UT, Keck T. Elevated blood urea nitrogen is an independent risk factor of prolonged intensive care unit stay due to acute necrotizing pancreatitis. J Crit Care. 2010;25:105–111.
Thomas L. Labor und Diagnose. Germany: TH-Books-Verlagsgesellschaft, Frankfurt/Main; 2005:544–547.
Moore FA. Effects of immune-enhancing diets on infectious morbidity and multiple organ failure. J Parenter Enteral Nutr (JPEN). 2001;25:S36–S42; discussion S-3.
Doi K, Leelahavanichkul A, Hu X, et al. Pre-existing renal disease promotes sepsis-induced acute kidney injury and worsens outcome. Kidney Int. 2008;74:1017–1025.
Kang CI, Song JH, Chung DR, et al. Risk factors and treatment outcomes of community-onset bacteraemia caused by extended-spectrum beta-lactamase-producing Escherichia coli. Int J Antimicrob Agents. 2010;36:284–287.
Du B, Long Y, Liu H, et al. Extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae bloodstream infection: risk factors and clinical outcome. Intensive Care Med. 2002;28:1718–1723.
Lautenbach E, Metlay JP, Bilker WB, Edelstein PH, Fishman NO. Association between fluoroquinolone resistance and mortality in Escherichia coli and Klebsiella pneumoniae infections: the role of inadequate empirical antimicrobial therapy. Clin Infect Dis. 2005;41:923–929.
Barenfanger J, Graham DR, Kolluri L, et al. Decreased mortality associated with prompt gram staining of blood cultures. Am J Clin Pathol. 2008;130:870–876.
Jain S, Andrews J, Fraise A, Brenwald N. Rapid detection of extended-spectrum beta-lactamase-producing gram-negative bacilli in blood cultures. J Antimicrob Chemother. 2007;60:652–654.
Ercis S, Sancak B, Kocagoz T, Kocagoz S, Hascelik G, Bolmstrom A. Rapid 4 to 6 hour detection of extended-spectrum beta-lactamases in a routine laboratory. Scand J Infect Dis. 2007;39:781–785.
Nordmann P, Dortet L, Poirel L. Rapid detection of extended-spectrum-beta-lactamase-producing enterobacteriaceae. J Clin Microbiol. 2012;50:3016–3022.
Cagatay AA, Kocagoz T, Eraksoy H. Dio-sensimedia: a novel culture medium for rapid detection of extended spectrum beta-lactamases. BMC Infect Dis. 2003;3:22.
Colodner R, Reznik B, Gal V, Yamazaki H, Hanaki H, Kubo R. Evaluation of a novel kit for the rapid detection of extended-spectrum beta-lactamases. Eur J Clin Microbiol Infect Dis. 2006;25:49–51.
Boey JH, Way LW. Acute cholangitis. Ann Surg. 1980;191:264–270.
Hui CK, Lai KC, Yuen MF, Ng M, Lai CL, Lam SK. Acute cholangitis—predictive factors for emergency ERCP. Aliment Pharmacol Ther. 2001;15:1633–1637.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Ban Seok Lee and Jin-Hyeok Hwang contributed equally to this work as first author.
Rights and permissions
About this article
Cite this article
Lee, B.S., Hwang, JH., Lee, S.H. et al. Risk Factors of Organ Failure in Patients with Bacteremic Cholangitis. Dig Dis Sci 58, 1091–1099 (2013). https://doi.org/10.1007/s10620-012-2478-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2478-8