Abstract
Proteomics refers to the study of the entire set of proteins in a given cell or tissue. With the extensive development of protein separation, mass spectrometry, and bioinformatics technologies, clinical proteomics has shown its potential as a powerful approach for biomarker discovery, particularly in the area of oncology. More than 130 exploratory studies have defined candidate markers in serum, gastrointestinal (GI) fluids, or cancer tissue. In this article, we introduce the commonly adopted proteomic technologies and describe results of a comprehensive review of studies that have applied these technologies to GI oncology, with a particular emphasis on developments in the last 3 years. We discuss reasons why the more than 130 studies to date have had little discernible clinical impact, and we outline steps that may allow proteomics to realize its promise for early detection of disease, monitoring of disease recurrence, and identification of targets for individualized therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
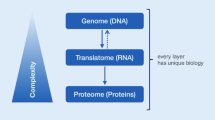
The term “proteome,” coined in 1995, is analogous to “genome,” and was initially used to describe “the entire complement of proteins expressed by a genome, cell, tissue or organism” [1]. The human genome contains about 23,000 protein-coding genes [2], but because of the occurrence of alternative splicing, the proteome is much larger, and probably consists of more than 100,000 distinct polypeptides [3]. The prevalence of post-translational modifications contributes additional diversity. Proteomic analysis is more challenging than genomic analysis, but is also more rewarding, because it captures regulatory effects at all levels of gene expression (i.e., transcriptional, translational, and post-translational). The goal of proteomics, in most cases, is the discovery of protein biomarkers, which are signatures of physiological or disease state. These can be used, alone or in combination, for screening and diagnosis, establishment of individual prognosis, prediction of individual response to therapy, and monitoring of disease progression [4, 5].
This review is in three parts. First, we present an overview of current proteomic technologies. Proteins and peptides are much more chemically diverse than nucleic acids, and the technologies required for proteome analysis are correspondingly more complex. It is helpful to introduce terminology and current technical approaches before considering clinical studies in detail. Second, we describe the use of proteomic technologies in GI oncology. This compilation is based on a MEDLINE search of the literature through August 2008. In addition to summarizing our results in table form, we provide an overview and briefly summarize a few notable findings in the main text. Third, we discuss prospects for application of proteomic findings in GI oncology, including the limitations of current studies and a discussion of steps that are needed to advance the field to the next level.
Proteomic Technologies
Figure 1 provides an overview of currently available analytical strategies, including types of samples and profiling methods.
Strategies for proteomic analysis of clinical samples. Samples may include serum, other body fluids, or tissue. Profiling may be antibody-based or MS-based. A variety of labeling and protein separation techniques may be used prior to the MS. Top-down and bottom-up approaches differ in the order in which steps are performed. In many proteomic studies, key findings are validated by independent means (see text for details and definition of additional terms)
Types of Samples
Samples used for clinical proteomics come from three sources: serum, other accessible body fluids (e.g., saliva, gastric juice, pancreatic juice, or bile), and tissue. Serum is advantageous for screening and early detection of disease because collection is minimally invasive. It presents challenges for analysis, however, because cancer biomarkers are likely to be much more dilute in serum than in the tissue of origin. An additional complication is that a majority of serum peptides likely represent fragments of larger proteins degraded by various proteases [6]. GI fluids are advantageous because they are relatively organ-specific, and proteins of interest may be present at higher concentrations than those in the serum. Because collection is difficult and somewhat invasive, analysis of GI fluids is an option that is primarily applicable in symptomatic patients. Tissue samples are advantageous because tissue is the ultimate source of biomarkers present in serum and other fluids. Although collection is invasive, tissue extraction provides access to a variety of intracellular regulatory proteins, such as regulatory kinases or transcription factors, which would not routinely be present in serum or GI fluids. Tissue studies thus may provide more insight into disease mechanisms than can be obtained by analysis of samples from non-tissue sources.
Tissue proteomics may use material from bulk dissection or laser capture microdissection (LCM). The latter, illustrated in Fig. 2, allows analysis of specific cell types (e.g., cancer cells free of stroma) [7]. Other methods of sample fractionation have also been used to enrich for cancer cells, for example passage through a narrow gauge needle to detach tumor cells from stroma [8]. Tissue proteomics can also be performed using imaging mass spectrometry (IMS), where tissue sections are analyzed directly by mass spectrometry, circumventing the need for microdissection or protein extraction (recently reviewed in [9]).
LCM. a Thermoplastic membrane is placed over a tissue section, b infra-red laser pulse is used to heat a 7.5–30 μm diameter spot, briefly melting the membrane and capturing cells of interest. Heating and cooling of the membrane apparently has no adverse effect [7]. c Cells of interest become attached to the membrane and can be lifted from the slide for downstream analysis. d Application of LCM on colonic epithelium and colon cancer tissue slides
Use of archival tissue is complicated by covalent protein modifications introduced by common methods of fixation and staining. Although several recent reports describe analysis of peptides recovered from formalin-fixed, paraffin-embedded tissues [10–13], the most common method of sample preservation for proteomic analysis is freezing, which necessitates dedicated sample collection. Alternative techniques based on alcohol or other chemical fixatives have also shown promise [14, 15].
Profiling Methods
Mass Spectrometry (MS)-Based Profiling
Many clinical studies are exploratory, that is, broad surveys of the proteome without prior knowledge of the proteins of interest. Profiling of tissue extracts can be performed using either a “top-down” or “bottom-up” approach (Fig. 1). Top-down approaches begin with one or more separation steps to resolve individual proteins, or classes of proteins, in a complex mixture. Because intact proteins are physically and chemically diverse, there is no single universally applicable separation method. Two-dimensional gel electrophoresis (2-DE), which separates proteins based on charge in one dimension and size in the other [16], can separate up to 5,000 distinct proteins simultaneously [17]. Proteins may be reacted with fluorescent CyDyes prior to electrophoresis, or the gel may be stained afterward. Limitations of 2-DE are that it cannot be fully automated, and tends not to resolve proteins that are large, hydrophobic, or strongly basic. Liquid chromatography (LC) provides an alternative to 2D gels; although it can be used for intact proteins, it has found wider application in the “bottom-up” approaches discussed below.
Surface adsorption is a specialized separation and concentration method used in surface enhanced laser desorption ionization (SELDI). A protein solution is incubated with a hydrophobic, charged, or other surface that is fabricated as part of a chip that can be introduced directly into a mass spectrometer, producing a complex mass spectrum that provides a “fingerprint” of a physiological state or disease. SELDI is easily applied to large numbers of clinical samples and is most commonly used for serum studies.
In a bottom-up approach, the order of the analytical steps differs [18, 19]. Proteins in the sample mixture are first digested to completion with a site-specific protease. Peptides (rather than intact proteins) are chromatographically separated by high-resolution ion exchange and reverse-phase LC. Products are again analyzed by MS in the final step [20]. Although throughput is limited, bottom-up approaches can identify very large numbers of proteomic features, and they can be applied to proteins that are difficult to solubilize and resolve when intact [21]. Top-down and bottom-up approaches are thus complementary and potentially provide somewhat different information.
Options for final MS analysis are similar in all approaches. A “soft ionization” procedure creates peptide ions in the gas phase, using mild conditions that maintain peptide bonds intact. In matrix-assisted laser desorption ionization (MALDI) (and its specialized variations, SELDI and IMS) a laser pulse is directed at a mixture of protein sample and an organic matrix (Fig. 3a) [22]. With electrospray ionization (ESI), the other common soft ionization method, a protein or peptide solution passes through a heated capillary, spraying droplets of solution into a vacuum chamber containing a strong electric field, where they then evaporate and ionize (Fig. 3b) [23]. The ions are passed through a mass analyzer, which separates them based on mass-to-charge (m/z) ratio.
MALDI-MS and ESI-MS procedures. a In MALDI-MS, samples are co-crystallized with an organic matrix on a metal target plate. A pulsed laser irradiates the co-crystals, which causes rapid heating and desorption of ions into the gas phase. Ions go through the mass analyzer and the detector registers the numbers of ions at each individual mass-to-charge (m/z) value, then the peptide mass fingerprint is generated. MALDI-MS produces relatively simple spectra composed of ions with unit charge. b In ESI-MS, sample molecules are ionized directly in the analyte solution by passing through a heated capillary device, spraying droplets of solution into a vacuum chamber containing a high-strength electric field. The resulting ions pass through a mass analyzer and detector as in a. ESI-MS produces complex spectra with multiply charged ions
Data is obtained in the form of a mass spectrum—a histogram with ion counts on the vertical axis and m/z on the horizontal axis (Fig. 3). In SELDI, pattern analysis may be applied to detect features of the spectrum that correlate with disease state, even without identification of proteins at the molecular level. In other MS procedures, the goal is molecular identification of proteins present in the sample. This is done by matching a pattern of peptides, or “peptide mass fingerprint,” against a human protein database. Confidence in MS identifications is based on coverage (the fraction of the protein’s total sequence represented among the identified peptides) and statistical criteria particular to the method used.
Tandem mass spectrometers, which have more than one mass analyzer connected in series, can perform MS/MS. This involves selection of an ion of interest based on m/z, partial fragmentation at peptide bonds (by collision with an inert gas), and passage of the products through a second mass analyzer, with the resulting fragmentation pattern providing amino acid sequence information for the precursor ion. Partial sequence data obtained by MS/MS provides a further basis for identification [24].
Imaging MS is performed by first coating a thin (10-μm) tissue section with organic matrix. The section is systematically moved underneath a laser beam and a mass spectrum is collected at each position. Software renders the data as a spatially resolved density map showing relative abundance of peptides or proteins of interest [9, 25].
Quantification of Protein Abundance
Clinical laboratory studies require quantification of molecular species, rather than simple determination of presence or absence. Neither gel staining nor mass spectrometry provides a good indication of absolute quantity. Quantification thus relies on multiplex analysis, where samples from different sources are differentially labeled, mixed, and subjected to electrophoretic or chromatographic separation. The abundance of each protein or peptide is determined relative to the corresponding feature in the other sample. Clinical samples can be compared directly (e.g., diseased versus normal) or indirectly with reference to an invariant internal standard, consisting of a mixture of samples used in the experiment.
Two-dimensional difference gel electrophoresis (2D-DIGE) is the most common multiplex top-down approach [26, 27] (Fig. 4). Proteins are covalently labeled by reaction of cyanine dyes with cysteine or lysine residues. Spectrally distinct dyes are similar in molecular weight and do not change the protein charge. Thus, the same proteins in different samples, labeled in different colors, migrate to the same position in the gel. For each spot, the ratio of emission at different wavelengths provides a measure of relative abundance [28].
Two-dimensional difference gel electrophoresis (2D-DIGE). a Representative gel images of proteins from analysis of a microdissected CRC specimen in our laboratory. Red represents Cy5-labeled sample proteins, and green represents Cy3-labeled pooled internal standard. In the multiplexed image, spots that are more abundant in the sample than in the standard appear red, spots that are less abundant in the sample appear green, and spots that are equal in the sample and the standard appear yellow. b Design of a clinical proteomics experiment. In this example, which is based on analysis of cancer-normal pairs, each patient contributes two samples: cancer and adjacent normal tissue. The number of gels equals the number of samples. For each spot in each gel, the ratio of emission at Cy5 and Cy3 wavelengths is measured. These “internal ratios” are used to compare the relative abundance of a given protein across the different specimens in the experiment
Isotope-coded affinity tag (ICAT) technology is the analogous method for the bottom-up approach. The ICAT reagent combines three moieties: a biotin group, a heavy or light isotope-tagged linker (e.g., containing 2H vs. 1H, or 13C vs. 12C), and a thiol-specific reactive group that reacts with cysteine in the protein sample (Fig. 5a) [29]. Two samples, pre-labeled with heavy- or light-isotope ICAT reagent, are mixed and proteolytically digested (Fig. 5b). Tagged peptides are isolated by avidin affinity chromatography and analyzed by LC-MS [30]. The relative abundance of heavy and light isotope peaks for each peptide provides an accurate measure of the relative abundance of the peptide in different samples. A variation, isotope-coded protein label (ICPL) [31], is based on isotopic labeling of free amino groups in proteins, which are more abundant than thiols. Another variation, isobaric tags for relative and absolute quantification (iTRAQ) allows multiplexing of up to four samples simultaneously [32].
Schematic illustration of ICAT procedure. a ICAT reagent combines three moieties: a biotin tag, a heavy or light isotope-tagged linker, and a thiol-specific reactive group. b Samples, labeled with heavy- or light-isotope ICAT reagent are mixed and digested. Tagged peptides are isolated by avidin affinity chromatography and analyzed by LC-MS. The relative abundance of heavy and light isotope peaks for each peptide is then measured. Peptides of interest can be identified by MS/MS analysis
Antibody-Based Profiling
In contrast to MS-based methods, antibody-based profiling requires prior knowledge of proteins of interest. Tissue microarrays exemplify a broad class of technologies referred to as protein arrays where proteins or tissue samples are spotted on a surface and probed with antibody (Fig. 6a) [33, 34]. Often used for validation of biomarkers identified in MS-based methods, they have the same advantages and disadvantages as other forms of immunohistochemistry (IHC). Interpretation of staining patterns can be subjective, and quantification is less precise than with other proteomic methods [35].
Protein microarray technology. a Tissue microarray. Multiple tissue sections (or protein extracts) are spotted onto an array, which is incubated with a specific antibody against the protein of interest. Samples that contain the protein of interest are then detected. b Antibody microarrays: A series of capture molecules (antibodies) are displayed on a slide or membrane that is exposed to analytes (a tissue lysate). The bound proteins are detected by labeled secondary antibodies
In another variation on array technology, a panel of antibodies is spotted on a surface and incubated with a solubilized mixture of proteins. After washing, the protein bound to each spot is quantified using a labeled secondary antibody or reagent (Fig. 6b) [36]. The technology of antibody arrays is just beginning to be applied in GI oncology [37, 38] and holds promise as a method for simultaneous analysis of multiple biomarkers, or “proteomic signatures” in a clinical laboratory setting.
Use of Proteomic Technologies in GI Oncology
Methods
To identify relevant literature, we searched MEDLINE through August 2008 using entry terms including “proteomics,” “biomarker discovery,” “mass spectrometry,” “gastrointestinal tumor,” “serum,” “human tissue,” “gastric juice,” “pancreatic juice,” “bile,” “GI secretions,” “esophageal cancer,” “gastric cancer,” “small intestine tumor,” “colorectal cancer,” “pancreatic cancer,” “hepatocellular carcinoma,” and “cholangiocarcinoma” in different combinations. English-language abstracts of the retrieved articles were reviewed and categorized. In all but a few cases, full articles were obtained and reviewed. Additional citations were obtained from review articles and from the bibliographies of cited references.
Serum Biomarkers
We identified 57 serum-based studies (Table 1). Of these, 54 used MS-based profiling, while three recent studies applied antibody-based profiling [37–39]. All but one of the MS-based studies used a “top-down” strategy, in the majority of cases SELDI-MS (38/54 studies).
Diseases of the Alimentary Tract
Eight studies analyzed sera from patients with esophageal cancer or related premalignant conditions such as dysplasia or basal cell hyperplasia. In three of these, anonymous SELDI m/z peaks were used in classification algorithms to discriminate between normal or disease states [40–42]. In a fourth SELDI study, m/z peaks were used to distinguish chemoradiation responders from non-responders [43]. Two 2-DE studies identified a small number of serum proteins that differed in pre- and post-surgery patients, with no overlap in the proteins identified in the two reports [44, 45]. Two other studies identified characteristic serum autoantibodies against peroxiredoxin VI and heat-shock protein 70, respectively, as potential diagnostic biomarkers [46, 47].
Five studies of gastric cancer have used the SELDI approach [48–52]. In each case, SELDI identified combinations of m/z peaks that correctly classified most cancer patients versus other subjects. In one study, relevant peaks were identified as stress-related proteins, including heat-shock protein 27, glucose-regulated protein, and protein disulfide isomerase [50]. Levels of these proteins declined following surgery, suggesting that they could be used in surveillance for recurrence [50]. Specificity and sensitivity using SELDI-based biomarkers were higher than those achieved for the same samples using two established markers, carcinoembryonic antigen (CEA) and carbohydrate antigen (CA) 19–9, in combination [52]. A very recent study used antibody microarray technology to explore serum biomarkers of gastric cancer. Serum reactivity with IPO-38 antibody, which is directed against a small nuclear protein (possibly H2B), appeared useful both for diagnosis and for predicting survival in gastric cancer [38].
Ten studies analyzed sera from colorectal cancer (CRC) patients. Nine used SELDI-MS; several showed that SELDI-MS biomarkers compare favorably with established tests, including fecal occult blood or CEA [53], or a triple combination of CEA, CA19–9, and CA 242 [54]. SELDI-MS markers can be used to classify different stages of CRC [55], and to differentiate between good and poor responders to neoadjuvant therapy [56]. As with other diseases, the majority of CRC SELDI-MS studies are based on anonymous peaks, although a few studies report identification of specific proteins associated with classifier peaks, including apolipoproteins A-I and C-I [57], complement C3a des-arg, alpha1-antitrypsin and transferrin [53], and serum amyloid A [58]. A 2-DE serum analysis found 28 spots differentially expressed between cancer and normal, among which clusterin, complement factor I and β-2-glycoprotein I were proposed as a potential panel of CRC biomarkers [59].
Although most studies focus on cancer, three used proteomic methods to identify biomarkers of benign diseases [60–62]. One of these studies showed the ability to distinguish patients with Crohn’s disease or ulcerative colitis from control subjects who were either healthy or suffered from other inflammatory conditions based on four identified classifier proteins [60]. Another showed the ability to identify patients with large colon adenomas based on a set of anonymous m/z peaks [62]. Another used ICAT technology to identify proteins useful for differential diagnosis of familial adenomatous polyposis [61].
Diseases of the Pancreas and Hepatobiliary Tract
Ten studies profiled sera from pancreatic or biliary tract cancer patients. Three SELDI studies identified anonymous m/z peaks that correctly classified most pancreatic cancer [63, 64] or cholangiocarcinoma [65] patients. In one of these studies, SELDI-MS biomarkers, or SELDI-MS biomarkers in combination with CA19-9, were significantly more accurate than CA19-9 alone [63]. Serum CA 19-9 can also be sensitively detected with protein array technology [39]. Other studies, using 2-DE, identified proteins, or in one case autoantibodies, that are differentially present in sera from cancer patients versus control subjects [66–69]. In one of the first applications of antibody microarray to GI oncology, a recent study identified a signature consisting of 21 protein analytes that discriminates between short-surviving (<12 months) and long-surviving pancreatic cancer patients [37].
Twenty studies, primarily using SELDI-MS, characterized changes in the serum proteome of patients with hepatocellular carcinoma (HCC). HCC usually develops following a long history of chronic liver disease, and there is a need for markers of progression to cancer. All SELDI studies identified m/z peaks that accurately classified sera from patients with chronic hepatitis B or C infection, cirrhosis, and HCC (Table 1). Two studies specifically commented on prospects for use of SELDI-MS biomarkers for early detection: Kanmura et al. analyzed sera collected before the diagnosis of HCC by ultrasonography. They demonstrated the ability of SELDI-MS biomarkers to predict the diagnosis of HCC in 6/7 patients before HCC was clinically apparent [70]. Zinkin et al. demonstrated that SELDI-MS biomarkers were more accurate than traditional markers in detecting small HCCs in Hepatitis C patients [71]. A 2-D liquid phase fractionation study, using chromatofocusing (similar to the first dimension of 2-DE but performed in solution) and reverse-phase LC, identified 14 proteins with differential expression in HCC, albeit based on a single patient per group [72]. Another recent study identified a characteristic autoantibody signature in HCC patients [73].
Prospects for Clinical Translation of Serum Biomarkers
When multiple studies of the same disease are compared, a major limitation of serum profiling becomes evident, which is the unsatisfactory reproducibility between studies. The majority of early serum studies used SELDI technology, resulting in identification of anonymous discriminatory m/z peaks. In only a very few cases were the same discriminatory peaks identified. This may well reflect technical differences in sample collection, processing, type of SELDI chip, or other variables. Inconsistency between studies, however, is a major barrier to clinical translation of SELDI biomarkers. In the minority of instances where m/z peaks have been identified at the molecular level, many of them correspond to high abundance, seemingly nonspecific molecules such as stress proteins, clotting factors, and other known serum components. Although tests based on these markers might be clinically useful, it is disappointing that markers have not been identified with a more obvious connection to biological mechanisms of cancer development. One reason for this, suggested by Diamandis [74], is that current SELDI-TOF technology is capable of detecting only those proteins present at a concentration greater than 1 μg/ml, which is approximately 1,000-fold greater than the concentrations of established serum tumor markers (e.g., CEA). Very recently, newer technologies such as ICAT and protein arrays have begun to be applied in serum studies, and it is possible that these may overcome some of the limitations of earlier methodologies.
A potentially difficult issue is that most serum studies relied on patients with advanced disease, where host-tumor (paraneoplastic) interactions are likely to be prominent. Serum biomarkers discovered thus far may not be applicable for early detection of cancer in the general, low-risk population, which is typically a stated goal in serum studies. A more immediate application of serum-based biomarkers may be for differential diagnosis in symptomatic patients or monitoring of disease progression and treatment responses following diagnosis. If issues of standardization and reproducibility can be overcome, accuracy in the various studies cited here (>80% sensitivity and specificity) seems well within the range that would be needed for clinical utility.
Biomarkers from GI Secretions
Biological fluids have a special role in proteomics as applied to GI oncology. The GI tract is unique among organ systems because of the amount and type of secretions. The normal adult produces about 7 l of GI fluids daily, including saliva, gastric juice, pancreatic juice, bile, and enteric secretions [75]. These are secreted and reabsorbed in balance. Fluids produced by the GI tract have less-complex compositions than serum, are relatively organ-specific, and are potentially good sources for biomarker discovery.
There have been two “top-down” 2-D gel-based proteomic profiling studies of gastric juice. These reported simple changes in proteomic pattern that differentiate cancer, precancerous conditions and benign disease, including loss of gastric digestive enzymes and appearance of α1-antitrypsin-related proteins [76, 77] (Table 2).
A SELDI-MS study by Rosty et al. [78] dramatically demonstrated the advantages of using pancreatic juice over serum for detection of pancreatic adenocarcinoma markers. They showed that hepatocarcinoma-intestine-pancreas/pancreatitis-associated-protein-1 (HIP/PAP-1) was present at 1,000-fold higher levels in pancreatic juice of cancer patients than in the serum of the same individuals. The fold difference in cancer patients versus other subjects was also much higher in pancreatic juice than in serum. Studies by Chen et al. [79, 80] used “bottom-up” ICAT and tandem MS-based proteomics to compare protein expression in pancreatic juice from cancer, chronic pancreatitis, and normal tissue. They identified 30 proteins specific to cancer, 27 specific to chronic pancreatitis, with nine in common. Three studies using “top-down” gel-based separations identified numerous potential cancer biomarkers, some of which were known and others of which were novel, including a HIP/PAP-1-related protein designated as PAP-2 [81–83].
Three studies characterized bile from patients with cholangiocarcinoma. Kristiansen et al. [84] used lectin chromatography to enrich for proteins of interest and deplete interfering proteins, facilitating analysis of the glycoproteome. Eighty-seven unique proteins were identified and 33 glycosylation sites were found. Two studies [85, 86] analyzed the proteomes of bile fluid from patients with malignant and benign bile tract obstruction using 2-DE; in one study, the pancreatic elastase/amylase ratio was confirmed to be a much more accurate marker than CEA or CA 19-9 [86].
Prospects for Clinical Translation of GI Secretions Biomarkers
Together, studies confirm the promise of GI secretions as a concentrated source of potentially useful biomarkers. Accessibility of these fluids varies, with collection of gastric juice being considerably easier and less invasive than pancreatic juice or bile. Nevertheless, fluids are routinely collected in symptomatic patients and tests based on these fluids may therefore be practical.
Biomarkers from GI Tissue
Tissue biomarkers are useful when a sample of the diseased tissue is available as a result of biopsy or surgical resection. Biomarkers identified by proteomic profiling of tissue have the potential to be useful directly, for example in staging or prediction of response to therapy. Information gleaned from tissue studies also lays a foundation for development of clinical serum tests; for example, if proteomic profiling reveals that a particular protein is present at high concentration in tumor tissue, one might develop a more-sensitive assay (based, for example, on protein-chip or other approaches) to investigate the presence of the protein in serum from cancer patients.
Diseases of the Alimentary Tract
There have been ten studies of esophageal cancer, all using “top-down” analysis. Eight used 2-DE separation, one used chromatofocusing, and one used capillary high-performance LC (Table 3). One of the most comprehensive of all reported proteomic surveys of GI cancers, conducted by Hatakeyama et al. [87], used 2D-DIGE to analyze 129 microdissected tissue specimens, which identified 217 differentially expressed proteins at the molecular level. Thirty-three of these distinguished tumors with and without nodal metastasis. Extensive bioinformatic analysis identified clusters of similarly regulated proteins, and gene ontology analysis showed that differentially regulated proteins had structural, transporter, chaperone, oxidoreduction, transcription, and signal-transduction activities. Zhao et al. [88] performed an interesting comparison of protein and mRNA expression. Of 38 proteins that differed in cancer-metaplasia pairs, mRNA correlated with protein expression changes in some instances but differed markedly in many others, underscoring the value added by proteomic analysis.
There have been eight gastric cancer tissue studies, all based on “top-down” analyses. Greengauz-Roberts et al. [89] demonstrated the ability to profile very small amounts of tissue (5 μg protein) using LCM and reported 42 proteins with differential expression in gastric adenocarcinoma versus spasmolytic peptide expressing metaplasia. He et al. [90] identified an 18-kDa antrum mucosa protein that was dramatically down-regulated in cancer tissues and proposed a special role for this protein in pathogenesis of gastric cancer. GI stromal tumor is a rare, non-epithelial malignancy of the GI tract, most commonly occurring in the stomach. Many cases are associated with mutation of the KIT protooncogene or platelet-derived growth factor receptor alpha. Two 2-DE studies identified proteins that were differentially expressed in patients in different mutation classes, or that discriminated patients with poor and good prognoses. Pfetin, a potassium channel protein, was identified as a powerful prognostic marker [91].
Eleven reports describe proteomic profiling of CRC or premalignant adenomas (Table 3). Seven studies using top-down 2-DE approaches identified numerous differentially expressed proteins including transcription regulators, signal transduction, and cytoskeletal proteins, molecular chaperones, protein synthesis factors, metabolic enzymes, apoptosis-associated proteins, and a proteoglycan (mimecan). A study of Pei et al. [92] is notable for identifying four proteins that differed specifically between primary tumors derived from node-positive versus node-negative patients. Two studies applied IMS technology on tissue sections without solubilization or protein-separation steps, an approach that is capable of providing spatially resolved images of in situ protein abundance in tumor areas versus normal areas [93, 94]. Another methodologically interesting study by Madoz-Gurpide et al. [95] selected 29 gene products for detailed investigation based on statistically significant up-regulation at the mRNA level and other criteria. They expressed these gene products in E. coli, prepared antibodies, and tested seven by IHC in a tissue microarray. They confirmed that six (ANXA3, BMP4, LCN2, SPARC, MMP7, and MMP11) were up-regulated at the protein level. Their unique, gene- and antibody-based approach avoids bias against interesting classes of proteins (i.e., very large, hydrophobic, or insoluble) that are readily overlooked in top-down proteomic approaches that rely on 2-DE as a first step.
Diseases of the Pancreas and Hepatobiliary Tract
Pancreatic cancer is second only to CRC as a cause of GI cancer deaths in the US. Unlike CRC, it is almost never detected until it has reached an incurable stage. Better detection, together with insights into disease mechanisms that might lead to better preventive or therapeutic options, would bring a large public health benefit. There have been seven “top-down” 2-DE studies (Table 3). The most comprehensive of these, by Lu et al. [96], identified 111 differentially expressed proteins at the molecular level. Proteins in this and other studies have structural, protease, metabolic, immune/inflammatory, transporter, RNA processing, transcription factor, signal transduction, cell adhesion, and other activities; some have been further validated by IHC. Studies by Chen et al. [97, 98] used “bottom-up” ICAT and tandem MS-based proteomics to identify 50 proteins as differentially expressed in cancer and 116 in pancreatitis, with considerable overlap between groups. Finally, A SELDI study [99] identified 33 anonymous m/z peaks that collectively distinguished pancreatic cancer, benign disease, and nonmalignant tissue. The same group applied a similar methodology to cholangiocarcinoma and identified 14 discriminatory, anonymous m/z peaks [65].
HCC is another GI cancer that has been widely studied using tissue profiling. As in the serum studies, progression of HBV or HCV-related disease to HCC has been the main focus. Of 19 studies, 16 used “top-down” 2-DE approaches, two used a “bottom-up” ICAT approach, and one used direct analysis of tissue slices by SELDI-TOF. Two of the most comprehensive studies combined LCM with ICAT and 2D-LC-MS/MS to compare the proteome of HCC with normal liver, identifying 149 differentially expressed proteins in one case, and 261 in another [100, 101]. Blanc et al. [102] identified 155 differentially regulated proteins in a 2-DE study, and Luk et al. [103], identified 90 in another. A 2D-DIGE study identified 127 differentially expressed proteins in cancer, and demonstrated in a validation study that a proteomic signature, based on clathrin heavy chain and formiminotransferase cyclodeaminase, could make substantial contributions to early diagnosis of HCC [104].
A methodologically interesting study by Emadali et al. [105] describes analysis of the hepatic tyrosine phosphoproteome using anti-phosphotyrosine antibodies to enrich for proteins of interest, followed by 1-DE and LC-ESI-MS/MS analysis. Although the study focused on ischemia/reperfusion (I/R) injury, the methodology could be readily extended to HCC. They found that the tyrosine kinase adaptor protein Nck-1 might play a role in I/R-induced actin reorganization.
Identification of Site of Cancer Origin
Pathologists sometimes face the problem of identifying the original site of a metastatic cancer when no primary tumor has been identified. Bloom et al. [106] used 2-DE, MALDI-TOF, and LC-MS/MS to compare the proteomic profiles of 77 histologically similar adenocarcinomas arising from six different sites of origin. Using these data, a neural network could correctly classify a single held-out sample with an average predictive accuracy of 82%. These findings show that proteomic data can be used to construct an accurate classifier for tumors without knowledge of their primary site of origin.
Prospects for Clinical Translation of Tissue Biomarkers
Almost every tissue proteomics study provides quantitative expression values for at least a few hundred “features”—spots on a gel, m/z peaks, or linked sets of peptides identified in bottom-up analysis. Among these features, it is easy to find examples of proteins or other features that show significant differential expression characteristic of physiological or disease states. More than ten independent studies have appeared for some tumor types (i.e., CRC and HCC). However, lists of candidate biomarkers produced in studies of the same tumor type are often significantly different.
Some differences may be attributable to the distinctive patient population seen at individual centers or by the nature of the comparison sample (i.e., patient-matched normal tissue, patients with benign disease, or “healthy” control subjects). There are also sources of variability that are particular to proteomic analysis. Existing proteomic profiling technology samples no more than 1% of the total proteome, and different studies may sample a different 1% depending on details of the methodology. Additionally, in top-down studies, investigators choose only a fraction of the total features as “interesting” enough for molecular identification, and the criteria for selecting these features vary. There are also significant differences in sample preparation. Some studies (14/64) use microdissection or other techniques to enrich for tumor cells, whereas the majority use bulk specimens, where the tumor-cell specific proteomic signature may be partially obscured by intermixed host tissue.
Despite these sources of variability, some common themes are evident, notably quantitative changes in cytoskeletal proteins, stress proteins, and enzymes of intermediary metabolism. In addition to common and abundant proteins, most studies report a few proteins that seem “interesting” because they are potentially involved in processes that drive malignancy, rather than simply reflecting the malignant phenotype. These include transcription factors, signal transduction proteins, and tumor suppressors. Both types of markers are potentially valuable. Quantitative changes in abundant proteins may have value in establishing individual prognosis (e.g., changes in cytoskeletal proteins that are predictive of metastatic potential), whereas transcription factors and signaling proteins may provide novel therapeutic targets.
Application of Proteomic Findings in GI Oncology
The number of exploratory proteomic studies in GI oncology is astonishing: more than 130 to date. Given the multiplicity of studies, have we moved closer to the ultimate objectives of proteomic research? None of the discoveries cited here has yet made a significant impact on clinical care. Many barriers to clinical translation are evident: the disconnect inherent in use of late-stage patients to discover markers of early disease, the lack of overlap in biomarkers identified in different studies of a same disease, and lack of standardization in sample collection and storage, protein-separation procedures, mass spectrometry, and statistical methodology. Rapid evolution of MS technology is a particularly significant contributor to lack of standardization, because studies performed at different times in different institutions almost inevitably involve different instrumentation.
Some progress has been made towards standardization, at least in areas of sample preparation and analysis, as the Early Detection Research Network of the US National Cancer Institute provides the Standard Operating Procedures and Assay Protocols for researchers via its Web site (http://edrn.nci.nih.gov). At present, however, the content of this resource remains limited.
Our review of published proteomic studies in GI oncology has suggested to us several additional steps that would be particularly valuable to the field:
-
It is important that study design and patient selection reflect the intended application of the markers. Markers discovered in tissue-based studies are most likely to be used for establishing individual prognosis or predicting response to therapy when the presence of disease is already known. It is therefore desirable for these studies to focus on classifying disease subsets or establishing molecular correlates of response in existing trials. Markers discovered in serum-based studies are often intended for early diagnosis, in which case it is essential that future studies include subjects who are at risk but have not yet been diagnosed with disease.
-
It would be helpful to incorporate uniformly rigorous statistical criteria in both design and analysis. There is a wide variation in the types and sophistication of statistical analysis employed in proteomic studies. It appears, in many cases, that study size is based on availability of samples or other resources, rather than explicit statistical reasoning. The use of “fold-change” remains prevalent as a criterion for ranking candidate biomarkers, although there is seldom explicit justification.
-
It would be fruitful to maintain an up-to-date and searchable index of the lists of biomarkers obtained in different studies. Proteomic studies generate vast amounts of data; even a small study with 10–20 patients can generate tens of thousands of protein abundance values. In this review, we have relied primarily on the author’s own assessment of their findings, as a comprehensive re-analysis of all of the primary data in the cited studies is beyond our scope.
-
Finally, it is essential that future studies focus not only on identifying the disease-associated alterations in proteins but also on determining the cellular functions of the proteins identified, as well as the mechanistic networks in which they participate. The biomarkers identified experimentally should serve as entry points for investigating the mechanisms of carcinogenesis and tumor progression.
Despite the existing barriers to clinical translation, it is important not to lose sight of the ultimate promise of clinical proteomics in GI medicine. Standard diagnostic procedures for GI diseases are largely based on clinical data in combination with endoscopy, imaging examination, histopathology, and immunohistology. Yet, we often observe that individual patients sharing the same type of disease, with the same histopathologic diagnosis, at an identical stage, end up with different clinical outcomes with respect to survival and treatment response. This indicates that each patient’s disease may have a unique constellation of molecular derangements [107].
In the future, clinical proteomics may provide a rational basis for individualized therapy. Patients with a GI malignancy could be identified early by screening serum or other GI fluids. A tissue biopsy could then be analyzed for a proteomic signature to establish prognosis, to select the best targets for individualized therapy, and to predict therapeutic responses and toxicities [108]. A recurrence could be detected early by serum analysis, providing an opportunity to alter the therapeutic regime. Using these new tools, GI malignancies could become manageable chronic diseases [109].
References
Wasinger VC, Cordwell SJ, Cerpa-Poljak A, et al. Progress with gene-product mapping of the mollicutes: Mycoplasma genitalium. Electrophoresis. 1995;16:1090–1094. doi:10.1002/elps.11501601185.
International Human Genome Sequencing Consortium. Finishing the euchromatic sequence of the human genome. Nature. 2004;431:931–945. doi:10.1038/nature03001.
Harrison PM, Kumar A, Lang N, Snyder M, Gerstein M. A question of size: the eukaryotic proteome and the problems in defining it. Nucleic Acids Res. 2002;30:1083–1090. doi:10.1093/nar/30.5.1083.
Azad NS, Rasool N, Annunziata CM, Minasian L, Whiteley G, Kohn EC. Proteomics in clinical trials and practice: present uses and future promise. Mol Cell Proteomics. 2006;5:1819–1829. doi:10.1074/mcp.R600008-MCP200.
Din S, Lennon AM, Arnott ID, Hupp T, Satsangi J. Technology insight: the application of proteomics in gastrointestinal disease. Nat Clin Pract Gastroenterol Hepatol. 2007;4:372–385. doi:10.1038/ncpgasthep0872.
Zheng X, Baker H, Hancock WS. Analysis of the low molecular weight serum peptidome using ultrafiltration and a hybrid ion-trap Fourier transform mass spectrometer. J Chromatogr A. 2006;1120:173–184. doi:10.1016/j.chroma.2006.01.098.
Murray GI. An overview of laser microdissection technologies. Acta Histochem. 2007;109:171–176. doi:10.1016/j.acthis.2007.02.001.
Roblick UJ, Hirschberg D, Habermann JK, et al. Sequential proteome alterations during genesis and progression of colon cancer. Cell Mol Life Sci. 2004;61:1246–1255. doi:10.1007/s00018-004-4049-4.
Seeley EH, Caprioli RM. Special feature: molecular imaging of proteins in tissues by mass spectrometry. Proc Natl Acad Sci USA. 2008;105:18126–18131.
Guo T, Wang W, Rudnick PA, et al. Proteome analysis of microdissected formalin-fixed and paraffin-embedded tissue specimens. J Histochem Cytochem. 2007;55:763–772. doi:10.1369/jhc.7A7177.2007.
Hwang SI, Thumar J, Lundgren DH, et al. Direct cancer tissue proteomics: a method to identify candidate cancer biomarkers from formalin-fixed paraffin-embedded archival tissues. Oncogene. 2007;26:65–76. doi:10.1038/sj.onc.1209755.
Jiang X, Jiang X, Feng S, Tian R, Ye M, Zou H. Development of efficient protein extraction methods for shotgun proteome analysis of formalin-fixed tissues. J Proteome Res. 2007;6:1038–1047. doi:10.1021/pr0605318.
Lemaire R, Desmons A, Tabet JC, Day R, Salzet M, Fournier I. Direct analysis and MALDI imaging of formalin-fixed, paraffin-embedded tissue sections. J Proteome Res. 2007;6:1295–1305. doi:10.1021/pr060549i.
Lykidis D, Van Noorden S, Armstrong A, et al. Novel zinc-based fixative for high-quality DNA, RNA and protein analysis. Nucleic Acids Res. 2007;35:e85. doi:10.1093/nar/gkm433.
Stanta G, Mucelli SP, Petrera F, Bonin S, Bussolati G. A novel fixative improves opportunities of nucleic acids and proteomic analysis in human archive’s tissues. Diagn Mol Pathol. 2006;15:115–123. doi:10.1097/00019606-200606000-00009.
Kenrick KG, Margolis J. Isoelectric focusing and gradient gel electrophoresis: a two-dimensional technique. Anal Biochem. 1970;33:204–207. doi:10.1016/0003-2697(70)90454-9.
Gorg A, Weiss W, Dunn MJ. Current two-dimensional electrophoresis technology for proteomics. Proteomics. 2004;4:3665–3685. doi:10.1002/pmic.200401031.
MacCoss MJ, McDonald WH, Saraf A, et al. Shotgun identification of protein modifications from protein complexes and lens tissue. Proc Natl Acad Sci USA. 2002;99:7900–7905. doi:10.1073/pnas.122231399.
Washburn MP, Wolters D, Yates JR 3rd. Large-scale analysis of the yeast proteome by multidimensional protein identification technology. Nat Biotechnol. 2001;19:242–247. doi:10.1038/85686.
Wolters DA, Washburn MP, Yates JR 3rd. An automated multidimensional protein identification technology for shotgun proteomics. Anal Chem. 2001;73:5683–5690. doi:10.1021/ac010617e.
Salzano AM, Crescenzi M. Mass spectrometry for protein identification and the study of post translational modifications. Ann Ist Super Sanita. 2005;41:443–450.
Karas M, Hillenkamp F. Laser desorption ionization of proteins with molecular masses exceeding 10,000 daltons. Anal Chem. 1988;60:2299–2301. doi:10.1021/ac00171a028.
Guerrera IC, Kleiner O. Application of mass spectrometry in proteomics. Biosci Rep. 2005;25:71–93. doi:10.1007/s10540-005-2849-x.
Aebersold R, Mann M. Mass spectrometry-based proteomics. Nature. 2003;422:198–207. doi:10.1038/nature01511.
Stoeckli M, Chaurand P, Hallahan DE, Caprioli RM. Imaging mass spectrometry: a new technology for the analysis of protein expression in mammalian tissues. Nat Med. 2001;7:493–496. doi:10.1038/86573.
Shaw J, Rowlinson R, Nickson J, et al. Evaluation of saturation labelling two-dimensional difference gel electrophoresis fluorescent dyes. Proteomics. 2003;3:1181–1195. doi:10.1002/pmic.200300439.
Wilson KE, Marouga R, Prime JE, et al. Comparative proteomic analysis using samples obtained with laser microdissection and saturation dye labelling. Proteomics. 2005;5:3851–3858. doi:10.1002/pmic.200401255.
Marouga R, David S, Hawkins E. The development of the DIGE system: 2D fluorescence difference gel analysis technology. Anal Bioanal Chem. 2005;382:669–678. doi:10.1007/s00216-005-3126-3.
Gygi SP, Rist B, Gerber SA, Turecek F, Gelb MH, Aebersold R. Quantitative analysis of complex protein mixtures using isotope-coded affinity tags. Nat Biotechnol. 1999;17:994–999. doi:10.1038/13690.
Hagenstein MC, Sewald N. Chemical tools for activity-based proteomics. J Biotechnol. 2006;124:56–73. doi:10.1016/j.jbiotec.2005.12.005.
Schmidt A, Kellermann J, Lottspeich F. A novel strategy for quantitative proteomics using isotope-coded protein labels. Proteomics. 2005;5:4–15. doi:10.1002/pmic.200400873.
Ross PL, Huang YN, Marchese JN, et al. Multiplexed protein quantitation in Saccharomyces cerevisiae using amine-reactive isobaric tagging reagents. Mol Cell Proteomics. 2004;3:1154–1169. doi:10.1074/mcp.M400129-MCP200.
Paweletz CP, Charboneau L, Bichsel VE, et al. Reverse-phase protein microarrays which capture disease progression show activation of pro-survival pathways at the cancer invasion front. Oncogene. 2001;20:1981–1989. doi:10.1038/sj.onc.1204265.
Sheehan KM, Calvert VS, Kay EW, et al. Use of reverse-phase protein microarrays and reference standard development for molecular network analysis of metastatic ovarian carcinoma. Mol Cell Proteomics. 2005;4:346–355. doi:10.1074/mcp.T500003-MCP200.
Gulmann C, Sheehan KM, Kay EW, Liotta LA, Petricoin EF 3rd. Array-based proteomics: mapping of protein circuitries for diagnostics, prognostics, and therapy guidance in cancer. J Pathol. 2006;208:595–606. doi:10.1002/path.1958.
Nielsen UB, Geierstanger BH. Multiplexed sandwich assays in microarray format. J Immunol Methods. 2004;290:107–120. doi:10.1016/j.jim.2004.04.012.
Ingvarsson J, Wingren C, Carlsson A, et al. Detection of pancreatic cancer using antibody microarray-based serum protein profiling. Proteomics. 2008;8:2211–2219. doi:10.1002/pmic.200701167.
Hao Y, Yu Y, Wang L, et al. Ipo-38 is identified as a novel serum biomarker of gastric cancer based on clinical proteomics technology. J Proteome Res. 2008;7:3668–3677.
Grote T, Siwak DR, Fritsche HA, et al. Validation of reverse phase protein array for practical screening of potential biomarkers in serum and plasma: accurate detection of ca19-9 levels in pancreatic cancer. Proteomics. 2008;8:3051–3060. doi:10.1002/pmic.200700951.
Hammoud ZT, Dobrolecki L, Kesler KA, et al. Diagnosis of esophageal adenocarcinoma by serum proteomic pattern. Ann Thorac Surg. 2007;84:384–392. doi:10.1016/j.athoracsur.2007.03.088. discussion 392.
Wang LD, Wang DC, Zheng S, et al. Serum proteomic profiles of the subjects with esophageal precancerous and cancerous lesions from , an area with high incidence of esophageal cancer in Henan Province, northern China. Ai Zheng. 2006;25:549–554.
Wang SJ, Zhang LW, Yu WF, et al. Establishment of a diagnostic model of serum protein fingerprint pattern for esophageal cancer screening in high incidence area and its clinical value. Zhonghua Zhong Liu Za Zhi. 2007;29:441–443.
Hayashida Y, Honda K, Osaka Y, et al. Possible prediction of chemoradiosensitivity of esophageal cancer by serum protein profiling. Clin Cancer Res. 2005;11:8042–8047. doi:10.1158/1078-0432.CCR-05-0656.
An JY, Fan ZM, Zhuang ZH, et al. Proteomic analysis of blood level of proteins before and after operation in patients with esophageal squamous cell carcinoma at high-incidence area in henan province. World J Gastroenterol. 2004;10:3365–3368.
Zhang LY, Ying WT, Mao YS, et al. Loss of clusterin both in serum and tissue correlates with the tumorigenesis of esophageal squamous cell carcinoma via proteomics approaches. World J Gastroenterol. 2003;9:650–654.
Fujita Y, Nakanishi T, Hiramatsu M, et al. Proteomics-based approach identifying autoantibody against peroxiredoxin VI as a novel serum marker in esophageal squamous cell carcinoma. Clin Cancer Res. 2006;12:6415–6420. doi:10.1158/1078-0432.CCR-06-1315.
Fujita Y, Nakanishi T, Miyamoto Y, et al. Proteomics-based identification of autoantibody against heat-shock protein 70 as a diagnostic marker in esophageal squamous cell carcinoma. Cancer Lett. 2008;263:280–290. doi:10.1016/j.canlet.2008.01.013.
Ebert MP, Meuer J, Wiemer JC, et al. Identification of gastric cancer patients by serum protein profiling. J Proteome Res. 2004;3:1261–1266. doi:10.1021/pr049865s.
Liang Y, Fang M, Li J, et al. Serum proteomic patterns for gastric lesions as revealed by SELDI mass spectrometry. Exp Mol Pathol. 2006;81:176–180. doi:10.1016/j.yexmp.2006.04.008.
Ren H, Du N, Liu G, et al. Analysis of variabilities of serum proteomic spectra in patients with gastric cancer before and after operation. World J Gastroenterol. 2006;12:2789–2792.
Lim JY, Cho JY, Paik YH, Chang YS, Kim HG. Diagnostic application of serum proteomic patterns in gastric cancer patients by proteinchip surface-enhanced laser desorption/ionization time-of-flight mass spectrometry. Int J Biol Markers. 2007;22:281–286.
Su Y, Shen J, Qian H, et al. Diagnosis of gastric cancer using decision tree classification of mass spectral data. Cancer Sci. 2007;98:37–43. doi:10.1111/j.1349-7006.2006.00339.x.
Ward DG, Suggett N, Cheng Y, et al. Identification of serum biomarkers for colon cancer by proteomic analysis. Br J Cancer. 2006;94:1898–1905. doi:10.1038/sj.bjc.6603188.
Zheng GX, Wang CX, Qu X, Deng XM, Deng BP, Zhang J. Establishment of serum protein pattern for screening colorectal cancer using SELDI-TOF-MS. Exp Oncol. 2006;28:282–287.
Xu WH, Chen YD, Hu Y, et al. Preoperative molecular staging of colorectal cancers by CM10 proteinchip and SELDI-TOF-MS analysis. Zhonghua Zhong Liu Za Zhi Chinese Journal of Oncology. 2006;28:753–757.
Smith FM, Gallagher WM, Fox E, et al. Combination of SELDI-TOF-MS and data mining provides early stage response prediction for rectal tumors undergoing multimodal neoadjuvant therapy. Ann Surg. 2007;245:259–266. doi:10.1097/01.sla.0000245577.68151.bd.
Engwegen JY, Helgason HH, Cats A, et al. Identification of serum proteins discriminating colorectal cancer patients and healthy controls using surface-enhanced laser desorption ionisation-time of flight mass spectrometry. World J Gastroenterol. 2006;12:1536–1544.
Roelofsen H, Alvarez-Llamas G, Dijkstra M, et al. Analyses of intricate kinetics of the serum proteome during and after colon surgery by protein expression time series. Proteomics. 2007;7:3219–3228. doi:10.1002/pmic.200601047.
Rodriguez-Pineiro AM, Rodriguez-Berrocal FJ, Paez de la Cadena M. Improvements in the search for potential biomarkers by proteomics: application of principal component and discriminant analyses for two-dimensional maps evaluation. J Chromatogr A. 2007;849:251–260.
Meuwis MA, Fillet M, Geurts P, et al. Biomarker discovery for inflammatory bowel disease, using proteomic serum profiling. Biochem Pharmacol. 2007;73:1422–1433. doi:10.1016/j.bcp.2006.12.019.
Quaresima B, Crugliano T, Gaspari M, Faniello MC, Cosimo P, Valanzano R, Genuardi M, Cannataro M, Veltri P, Baudi F, Doldo P, Cuda G, Venuta S, Costanzo F. A proteomics approach to identify changes in protein profiles in serum of familial adenomatous polyposis patients. Cancer Lett. 2008;272:40–52.
Ransohoff DF, Martin C, Wiggins WS, et al. Assessment of serum proteomics to detect large colon adenomas. Cancer Epidemiol Biomarkers Prev. 2008;17:2188–2193. doi:10.1158/1055-9965.EPI-07-2767.
Koopmann J, Zhang Z, White N, et al. Serum diagnosis of pancreatic adenocarcinoma using surface-enhanced laser desorption and ionization mass spectrometry. Clin Cancer Res. 2004;10:860–868. doi:10.1158/1078-0432.CCR-1167-3.
Yu Y, Chen S, Wang LS, et al. Prediction of pancreatic cancer by serum biomarkers using surface-enhanced laser desorption/ionization-based decision tree classification. Oncology. 2005;68:79–86. doi:10.1159/000084824.
Scarlett CJ, Saxby AJ, Nielsen A, et al. Proteomic profiling of cholangiocarcinoma: diagnostic potential of SELDI-TOF MS in malignant bile duct stricture. Hepatology. 2006;44:658–666.
Yu KH, Rustgi AK, Blair IA. Characterization of proteins in human pancreatic cancer serum using differential gel electrophoresis and tandem mass spectrometry. J Proteome Res. 2005;4:1742–1751. doi:10.1021/pr050174l.
Bloomston M, Zhou JX, Rosemurgy AS, Frankel W, Muro-Cacho CA, Yeatman TJ. Fibrinogen gamma overexpression in pancreatic cancer identified by large-scale proteomic analysis of serum samples. Cancer Res. 2006;66:2592–2599. doi:10.1158/0008-5472.CAN-05-3659.
Sun ZL, Zhu Y, Wang FQ, et al. Serum proteomic-based analysis of pancreatic carcinoma for the identification of potential cancer biomarkers. Biochim Biophys Acta. 2007;1774:764–771.
Tomaino B, Cappello P, Capello M, et al. Autoantibody signature in human ductal pancreatic adenocarcinoma. J Proteome Res. 2007;6:4025–4031.
Kanmura S, Uto H, Kusumoto K, et al. Early diagnostic potential for hepatocellular carcinoma using the SELDI protein chip system. Hepatology. 2007;45:948–956.
Zinkin NT, Grall F, Bhaskar K, et al. Serum proteomics and biomarkers in hepatocellular carcinoma and chronic liver disease. Clin Cancer Res. 2008;14:470–477. doi:10.1158/1078-0432.CCR-07-0586.
Lee HJ, Kang MJ, Lee EY, Cho SY, Kim H, Paik YK. Application of a peptide-based PF2D platform for quantitative proteomics in disease biomarker discovery. Proteomics. 2008;8:3371–3381. doi:10.1002/pmic.200800111.
Li L, Chen SH, Yu CH, Li YM, Wang SQ. Identification of hepatocellular-carcinoma-associated antigens and autoantibodies by serological proteome analysis combined with protein microarray. J Proteome Res. 2008;7:611–620. doi:10.1021/pr070525r.
Diamandis EP. Analysis of serum proteomic patterns for early cancer diagnosis: drawing attention to potential problems. J Natl Cancer Inst. 2004;96:353–356.
Chang EB, Sitrin MD, Black DD. Gastrointestinal, Hepatobiliary, and Nutritional Physiology. Philadelphia, Pennsylvania: Lippincott-Raven Publisher; 1996.
Hsu PI, Chen CH, Hsieh CS, et al. Alpha1-antitrypsin precursor in gastric juice is a novel biomarker for gastric cancer and ulcer. Clin Cancer Res. 2007;13:876–883. doi:10.1158/1078-0432.CCR-06-1404.
Lee K, Kye M, Jang JS, Lee OJ, Kim T, Lim D. Proteomic analysis revealed a strong association of a high level of alpha1-antitrypsin in gastric juice with gastric cancer. Proteomics. 2004;4:3343–3352. doi:10.1002/pmic.200400960.
Rosty C, Christa L, Kuzdzal S, et al. Identification of hepatocarcinoma-intestine-pancreas/pancreatitis-associated protein I as a biomarker for pancreatic ductal adenocarcinoma by protein biochip technology. Cancer Res. 2002;62:1868–1875.
Chen R, Pan S, Cooke K, et al. Comparison of pancreas juice proteins from cancer versus pancreatitis using quantitative proteomic analysis. Pancreas. 2007;34:70–79. doi:10.1097/01.mpa.0000240615.20474.fd.
Chen R, Pan S, Yi EC, et al. Quantitative proteomic profiling of pancreatic cancer juice. Proteomics. 2006;6:3871–3879. doi:10.1002/pmic.200500702.
Gronborg M, Bunkenborg J, Kristiansen TZ, et al. Comprehensive proteomic analysis of human pancreatic juice. J Proteome Res. 2004;3:1042–1055. doi:10.1021/pr0499085.
Zhou L, Lu Z, Yang A, et al. Comparative proteomic analysis of human pancreatic juice: methodological study. Proteomics. 2007;7:1345–1355. doi:10.1002/pmic.200600086.
Tian M, Cui Y, Song G, et al. Proteomic analysis identifies MMP-9, DJ-1 and A1BG as overexpressed proteins in pancreatic juice from pancreatic ductal adenocarcinoma patients. BMC Cancer. 2008;8:241. doi:10.1186/1471-2407-8-241.
Kristiansen TZ, Bunkenborg J, Gronborg M, et al. A proteomic analysis of human bile. Mol Cell Proteomics. 2004;3:715–728. doi:10.1074/mcp.M400015-MCP200.
Chen B, Dong JQ, Chen YJ, et al. Two-dimensional electrophoresis for comparative proteomic analysis of human bile. Hepatobiliary Pancreat Dis Int. 2007;6:402–406.
Chen CY, Tsai WL, Wu HC, Syu MJ, Wu CC, Shiesh SC. Diagnostic role of biliary pancreatic elastase for cholangiocarcinoma in patients with cholestasis. Clin Chim Acta. 2008;390:82–89.
Hatakeyama H, Kondo T, Fujii K, et al. Protein clusters associated with carcinogenesis, histological differentiation and nodal metastasis in esophageal cancer. Proteomics. 2006;6:6300–6316. doi:10.1002/pmic.200600488.
Zhao J, Chang AC, Li C, et al. Comparative proteomics analysis of Barrett metaplasia and esophageal adenocarcinoma using two-dimensional liquid mass mapping. Mol Cell Proteomics. 2007;6:987–999. doi:10.1074/mcp.M600175-MCP200.
Greengauz-Roberts O, Stoppler H, Nomura S, et al. Saturation labeling with cysteine-reactive cyanine fluorescent dyes provides increased sensitivity for protein expression profiling of laser-microdissected clinical specimens. Proteomics. 2005;5:1746–1757. doi:10.1002/pmic.200401068.
He QY, Cheung YH, Leung SY, Yuen ST, Chu KM, Chiu JF. Diverse proteomic alterations in gastric adenocarcinoma. Proteomics. 2004;4:3276–3287. doi:10.1002/pmic.200300916.
Suehara Y, Kondo T, Seki K, et al. Pfetin as a prognostic biomarker of gastrointestinal stromal tumors revealed by proteomics. Clin Cancer Res. 2008;14:1707–1717. doi:10.1158/1078-0432.CCR-07-1478.
Pei H, Zhu H, Zeng S, et al. Proteome analysis and tissue microarray for profiling protein markers associated with lymph node metastasis in colorectal cancer. J Proteome Res. 2007;6:2495–2501. doi:10.1021/pr060644r.
Li JQ, Xu BJ, Shakhtour B, et al. Variability of in situ proteomic profiling and implications for study design in colorectal tumors. Int J Oncol. 2007;31:103–111.
Shimma S, Sugiura Y, Hayasaka T, Hoshikawa Y, Noda T, Setou M. MALDI-based imaging mass spectrometry revealed abnormal distribution of phospholipids in colon cancer liver metastasis. J Chromatogr A. 2007;855:98–103.
Madoz-Gurpide J, Lopez-Serra P, Martinez-Torrecuadrada JL, Sanchez L, Lombardia L, Casal JI. Proteomics-based validation of genomic data: applications in colorectal cancer diagnosis. Mol Cell Proteomics. 2006;5:1471–1483. doi:10.1074/mcp.M600048-MCP200.
Lu Z, Hu L, Evers S, Chen J, Shen Y. Differential expression profiling of human pancreatic adenocarcinoma and healthy pancreatic tissue. Proteomics. 2004;4:3975–3988. doi:10.1002/pmic.200300863.
Chen R, Brentnall TA, Pan S, et al. Quantitative proteomics analysis reveals that proteins differentially expressed in chronic pancreatitis are also frequently involved in pancreatic cancer. Mol Cell Proteomics. 2007;6:1331–1342. doi:10.1074/mcp.M700072-MCP200.
Chen R, Yi EC, Donohoe S, et al. Pancreatic cancer proteome: the proteins that underlie invasion, metastasis, and immunologic escape. Gastroenterology. 2005;129:1187–1197. doi:10.1053/j.gastro.2005.08.001.
Scarlett CJ, Smith RC, Saxby A, et al. Proteomic classification of pancreatic adenocarcinoma tissue using protein chip technology. Gastroenterology. 2006;130:1670–1678. doi:10.1053/j.gastro.2006.02.036.
Li C, Hong Y, Tan YX, et al. Accurate qualitative and quantitative proteomic analysis of clinical hepatocellular carcinoma using laser capture microdissection coupled with isotope-coded affinity tag and two-dimensional liquid chromatography mass spectrometry. Mol Cell Proteomics. 2004;3:399–409. doi:10.1074/mcp.M300133-MCP200.
Li C, Yi H, Tan YX, et al. Analysis of microdissected cells by two-dimensional LC-MS approaches. Methods Mol Biol. 2007;428:193–208.
Blanc JF, Lalanne C, Plomion C, et al. Proteomic analysis of differentially expressed proteins in hepatocellular carcinoma developed in patients with chronic viral hepatitis c. Proteomics. 2005;5:3778–3789. doi:10.1002/pmic.200401194.
Luk JM, Lam CT, Siu AF, et al. Proteomic profiling of hepatocellular carcinoma in Chinese cohort reveals heat-shock proteins (HSP27, HSP70, GRP78) up-regulation and their associated prognostic values. Proteomics. 2006;6:1049–1057. doi:10.1002/pmic.200500306.
Seimiya M, Tomonaga T, Matsushita K, et al. Identification of novel immunohistochemical tumor markers for primary hepatocellular carcinoma; clathrin heavy chain and formiminotransferase cyclodeaminase. Hepatology. 2008;48:519–530.
Emadali A, Metrakos PP, Kalantari F, Boutros T, Boismenu D, Chevet E. Proteomic analysis of tyrosine phosphorylation during human liver transplantation. Proteome Sci. 2007;5:1. doi:10.1186/1477-5956-5-1.
Bloom GC, Eschrich S, Zhou JX, Coppola D, Yeatman TJ. Elucidation of a protein signature discriminating six common types of adenocarcinoma. Int J Cancer. 2007;120:769–775. doi:10.1002/ijc.22041.
Wulfkuhle JD, Edmiston KH, Liotta LA, Petricoin EF 3rd. Technology insight: pharmacoproteomics for cancer—promises of patient-tailored medicine using protein microarrays. Nat Clin Pract Oncol. 2006;3:256–268. doi:10.1038/ncponc0485.
Calvo KR, Liotta LA, Petricoin EF. Clinical proteomics: from biomarker discovery and cell signaling profiles to individualized personal therapy. Biosci Rep. 2005;25:107–125. doi:10.1007/s10540-005-2851-3.
Feldman AL, Espina V, Petricoin EF 3rd, Liotta LA, Rosenblatt KP. Use of proteomic patterns to screen for gastrointestinal malignancies. Surgery. 2004;135:243–247. doi:10.1016/j.surg.2003.08.019.
Zhao G, Gao CF, Song GY, Li DH, Wang XL. Identification of colorectal cancer using proteomic patterns in serum. Ai Zheng. 2004;23:614–618.
Chen YD, Zheng S, Yu JK, Hu X. Artificial neural networks analysis of surface-enhanced laser desorption/ionization mass spectra of serum protein pattern distinguishes colorectal cancer from healthy population. Clin Cancer Res. 2004;10:8380–8385. doi:10.1158/1078-0432.CCR-1162-03.
Liu XP, Shen J, Li ZF, Yan L, Gu J. A serum proteomic pattern for the detection of colorectal adenocarcinoma using surface-enhanced laser desorption and ionization mass spectrometry. Cancer Invest. 2006;24:747–753. doi:10.1080/07357900601063873.
Lin Y, Goedegebuure PS, Tan MC, et al. Proteins associated with disease and clinical course in pancreas cancer: a proteomic analysis of plasma in surgical patients. J Proteome Res. 2006;5:2169–2176. doi:10.1021/pr0600374.
Zhu XD, Zhang WH, Li CL, Xu Y, Liang WJ, Tien P. New serum biomarkers for detection of HBV-induced liver cirrhosis using SELDI protein chip technology. World J Gastroenterol. 2004;10:2327–2329.
Schwegler EE, Cazares L, Steel LF, et al. SELDI-TOF MS profiling of serum for detection of the progression of chronic hepatitis C to hepatocellular carcinoma. Hepatology. 2005;41:634–642.
Paradis V, Degos F, Dargere D, et al. Identification of a new marker of hepatocellular carcinoma by serum protein profiling of patients with chronic liver diseases. Hepatology. 2005;41:40–47.
Wang JX, Zhang B, Yu JK, Liu J, Yang MQ, Zheng S. Application of serum protein fingerprinting coupled with artificial neural network model in diagnosis of hepatocellular carcinoma. Chin Med J. 2005;118:1278–1284.
Kawakami T, Hoshida Y, Kanai F, et al. Proteomic analysis of sera from hepatocellular carcinoma patients after radiofrequency ablation treatment. Proteomics. 2005;5:4287–4295. doi:10.1002/pmic.200401287.
Ward DG, Cheng Y, N’Kontchou G, et al. Changes in the serum proteome associated with the development of hepatocellular carcinoma in hepatitis C-related cirrhosis. Br J Cancer. 2006;94:287–292. doi:10.1038/sj.bjc.6602923.
Orvisky E, Drake SK, Martin BM, et al. Enrichment of low molecular weight fraction of serum for ms analysis of peptides associated with hepatocellular carcinoma. Proteomics. 2006;6:2895–2902. doi:10.1002/pmic.200500443.
Lee IN, Chen CH, Sheu JC, et al. Identification of complement C3a as a candidate biomarker in human chronic hepatitis C and HCV-related hepatocellular carcinoma using a proteomics approach. Proteomics. 2006;6:2865–2873. doi:10.1002/pmic.200500488.
Huang C, Fan J, Zhou J, Liu YK, Cui JF. The effects of different clinicopathologic variables on serum protein fingerprint in hepatocellular carcinoma patients. Zhonghua Wai Ke Za Zhi. 2006;44:445–449.
Ward DG, Cheng Y, N’Kontchou G, et al. Preclinical and post-treatment changes in the HCC-associated serum proteome. Br J Cancer. 2006;95:1379–1383. doi:10.1038/sj.bjc.6603429.
Gobel T, Vorderwulbecke S, Hauck K, Fey H, Haussinger D, Erhardt A. New multi protein patterns differentiate liver fibrosis stages and hepatocellular carcinoma in chronic hepatitis C serum samples. World J Gastroenterol. 2006;12:7604–7612.
Yang MH, Tyan YC, Jong SB, Huang YF, Liao PC, Wang MC. Identification of human hepatocellular carcinoma-related proteins by proteomic approaches. Anal Bioanal Chem. 2007;388:637–643. doi:10.1007/s00216-007-1263-6.
Cui J, Kang X, Dai Z, et al. Prediction of chronic hepatitis B, liver cirrhosis and hepatocellular carcinoma by SELDI-based serum decision tree classification. J Cancer Res Clin Oncol. 2007;133:825–834. doi:10.1007/s00432-007-0224-y.
Geng X, Wang F, Li YG, Zhu GP, Zhang WM. SELDI-TOF MS proteinchip technology for screening of serum markers of HBV-induced hepatocellular carcinoma. J Exp Clin Cancer Res. 2007;26:505–508.
Cui JF, Liu YK, Zhou HJ, et al. Screening serum hepatocellular carcinoma-associated proteins by SELDI-based protein spectrum analysis. World J Gastroenterol. 2008;14:1257–1262. doi:10.3748/wjg.14.1257.
He QY, Zhu R, Lei T, et al. Toward the proteomic identification of biomarkers for the prediction of HBV-related hepatocellular carcinoma. J Cell Biochem. 2008;103:740–752. doi:10.1002/jcb.21443.
Xia SH, Hu LP, Hu H, et al. Three isoforms of annexin I are preferentially expressed in normal esophageal epithelia but down-regulated in esophageal squamous cell carcinomas. Oncogene. 2002;21:6641–6648. doi:10.1038/sj.onc.1205818.
Qi Y, Chiu JF, Wang L, Kwong DL, He QY. Comparative proteomic analysis of esophageal squamous cell carcinoma. Proteomics. 2005;5:2960–2971. doi:10.1002/pmic.200401175.
Yoo C, Zhao J, Pal M, et al. Automated integration of monolith-based protein separation with on-plate digestion for mass spectrometric analysis of esophageal adenocarcinoma human epithelial samples. Electrophoresis. 2006;27:3643–3651. doi:10.1002/elps.200600117.
Nishimori T, Tomonaga T, Matsushita K, et al. Proteomic analysis of primary esophageal squamous cell carcinoma reveals downregulation of a cell adhesion protein, periplakin. Proteomics. 2006;6:1011–1018. doi:10.1002/pmic.200500262.
Huang ZY, Xiong G, Zhang J, Wang WJ. Screening of differentially expressed proteins from human esophageal cancer and esophageal tissues by two-dimensional difference gel electrophoresis and mass spectrometry. Nan Fang Yi Ke Da Xue Xue Bao. 2007;27:1406–1409.
Hu H, Luo ML, Du XL, et al. Up-regulated manganese superoxide dismutase expression increases apoptosis resistance in human esophageal squamous cell carcinomas. Chin Med J. 2007;120:2092–2098.
Du XL, Hu H, Lin DC, et al. Proteomic profiling of proteins dysregulted in Chinese esophageal squamous cell carcinoma. J Mol Med. 2007;85:863–875. doi:10.1007/s00109-007-0159-4.
Fu L, Qin YR, Xie D, et al. Identification of alpha-actinin 4 and 67-kda laminin receptor as stage-specific markers in esophageal cancer via proteomic approaches. Cancer. 2007;110:2672–2681. doi:10.1002/cncr.23110.
Ryu JW, Kim HJ, Lee YS, et al. The proteomics approach to find biomarkers in gastric cancer. J Korean Med Sci. 2003;18:505–509.
Jang JS, Cho HY, Lee YJ, Ha WS, Kim HW. The differential proteome profile of stomach cancer: identification of the biomarker candidates. Oncol Res. 2004;14:491–499.
Ebert MP, Kruger S, Fogeron ML, et al. Overexpression of cathepsin B in gastric cancer identified by proteome analysis. Proteomics. 2005;5:1693–1704. doi:10.1002/pmic.200401030.
Melle C, Ernst G, Schimmel B, et al. Characterization of pepsinogen C as a potential biomarker for gastric cancer using a histo-proteomic approach. J Proteome Res. 2005;4:1799–1804. doi:10.1021/pr050123o.
Chen CD, Wang CS, Huang YH, et al. Overexpression of CLIC1 in human gastric carcinoma and its clinicopathological significance. Proteomics. 2007;7:155–167. doi:10.1002/pmic.200600663.
Huang Q, Huang Q, Chen W, et al. Identification of transgelin as a potential novel biomarker for gastric adenocarcinoma based on proteomics technology. J Cancer Res Clin Oncol. 2008;134:1219–1227.
Kang HJ, Koh KH, Yang E, et al. Differentially expressed proteins in gastrointestinal stromal tumors with kit and PDGFRA mutations. Proteomics. 2006;6:1151–1157. doi:10.1002/pmic.200500372.
Friedman DB, Hill S, Keller JW, et al. Proteome analysis of human colon cancer by two-dimensional difference gel electrophoresis and mass spectrometry. Proteomics. 2004;4:793–811. doi:10.1002/pmic.200300635.
Alfonso P, Nunez A, Madoz-Gurpide J, Lombardia L, Sanchez L, Casal JI. Proteomic expression analysis of colorectal cancer by two-dimensional differential gel electrophoresis. Proteomics. 2005;5:2602–2611. doi:10.1002/pmic.200401196.
Melle C, Bogumil R, Ernst G, Schimmel B, Bleul A, von Eggeling F. Detection and identification of heat-shock protein 10 as a biomarker in colorectal cancer by protein profiling. Proteomics. 2006;6:2600–2608. doi:10.1002/pmic.200500427.
Mazzanti R, Solazzo M, Fantappie O, et al. Differential expression proteomics of human colon cancer. Am J Physiol. 2006;290:G1329–G1338.
Polley AC, Mulholland F, Pin C, et al. Proteomic analysis reveals field-wide changes in protein expression in the morphologically normal mucosa of patients with colorectal neoplasia. Cancer Res. 2006;66:6553–6562. doi:10.1158/0008-5472.CAN-06-0534.
Wang Y, Ma Y, Lu B, Xu E, Huang Q, Lai M. Differential expression of mimecan and thioredoxin domain-containing protein 5 in colorectal adenoma and cancer: a proteomic study. Exp Biol Med (Maywood). 2007;232:1152–1159.
Shekouh AR, Thompson CC, Prime W, et al. Application of laser capture microdissection combined with two-dimensional electrophoresis for the discovery of differentially regulated proteins in pancreatic ductal adenocarcinoma. Proteomics. 2003;3:1988–2001. doi:10.1002/pmic.200300466.
Shen J, Person MD, Zhu J, Abbruzzese JL, Li D. Protein expression profiles in pancreatic adenocarcinoma compared with normal pancreatic tissue and tissue affected by pancreatitis as detected by two-dimensional gel electrophoresis and mass spectrometry. Cancer Res. 2004;64:9018–9026. doi:10.1158/0008-5472.CAN-04-3262.
Sitek B, Luttges J, Marcus K, et al. Application of fluorescence difference gel electrophoresis saturation labelling for the analysis of microdissected precursor lesions of pancreatic ductal adenocarcinoma. Proteomics. 2005;5:2665–2679. doi:10.1002/pmic.200401298.
Melle C, Ernst G, Escher N, et al. Protein profiling of microdissected pancreas carcinoma and identification of HSP27 as a potential serum marker. Clin Chem. 2007;53:629–635. doi:10.1373/clinchem.2006.079194.
Qi T, Han J, Cui Y, Zong M, Liu X, Zhu B. Comparative proteomic analysis for the detection of biomarkers in pancreatic ductal adenocarcinomas. J Clin Pathol. 2008;61:49–58. doi:10.1136/jcp.2006.044735.
Tian R, Wei LM, Qin RY, et al. Proteome analysis of human pancreatic ductal adenocarcinoma tissue using two-dimensional gel electrophoresis and tandem mass spectrometry for identification of disease-related proteins. Dig Dis Sci. 2008;53:65–72. doi:10.1007/s10620-007-9823-3.
Chung JC, Oh MJ, Choi SH, Bae CD. Proteomic analysis to identify biomarker proteins in pancreatic ductal adenocarcinoma. ANZ J Surg. 2008;78:245–251. doi:10.1111/j.1445-2197.2008.04429.x.
Park KS, Kim H, Kim NG, et al. Proteomic analysis and molecular characterization of tissue ferritin light chain in hepatocellular carcinoma. Hepatology. 2002;35:1459–1466.
Kim J, Kim SH, Lee SU, et al. Proteome analysis of human liver tumor tissue by two-dimensional gel electrophoresis and matrix assisted laser desorption/ionization-mass spectrometry for identification of disease-related proteins. Electrophoresis. 2002;23:4142–4156. doi:10.1002/elps.200290032.
Li C, Tan YX, Zhou H, et al. Proteomic analysis of hepatitis B virus-associated hepatocellular carcinoma: identification of potential tumor markers. Proteomics. 2005;5:1125–1139. doi:10.1002/pmic.200401141.
Song HY, Liu YK, Cui JF, et al. Proteomic analysis on metastasis-associated proteins of hepatocellular carcinoma tissues. Zhonghua Gan Zang Bing Za Zhi. 2005;13:331–334.
Lee IN, Chen CH, Sheu JC, et al. Identification of human hepatocellular carcinoma-related biomarkers by two-dimensional difference gel electrophoresis and mass spectrometry. J Proteome Res. 2005;4:2062–2069. doi:10.1021/pr0502018.
Ai J, Tan Y, Ying W, et al. Proteome analysis of hepatocellular carcinoma by laser capture microdissection. Proteomics. 2006;6:538–546. doi:10.1002/pmic.200500257.
Kuramitsu Y, Harada T, Takashima M, et al. Increased expression and phosphorylation of liver glutamine synthetase in well-differentiated hepatocellular carcinoma tissues from patients infected with hepatitis C virus. Electrophoresis. 2006;27:1651–1658. doi:10.1002/elps.200500718.
Melle C, Ernst G, Scheibner O, et al. Identification of specific protein markers in microdissected hepatocellular carcinoma. J Proteome Res. 2007;6:306–315. doi:10.1021/pr060439b.
Sun W, Xing B, Sun Y, et al. Proteome analysis of hepatocellular carcinoma by two-dimensional difference gel electrophoresis: novel protein markers in hepatocellular carcinoma tissues. Mol Cell Proteomics. 2007;6:1798–1808. doi:10.1074/mcp.M600449-MCP200.
Guo WX, Man XB, Yuan HX, et al. Proteomic analysis on portal vein tumor thrombus-associated proteins for hepatocellular carcinoma. Zhonghua Yi Xue Za Zhi. 2007;87:2094–2097.
Zhang D, Lim SG, Koay ES. Proteomic identification of down-regulation of oncoprotein DJ-1 and proteasome activator subunit 1 in hepatitis B virus-infected well-differentiated hepatocellular carcinoma. Int J Oncol. 2007;31:577–584.
Yi X, Luk JM, Lee NP, et al. Association of mortalin (HSPA9) with liver cancer metastasis and prediction for early tumor recurrence. Mol Cell Proteomics. 2008;7:315–325. doi:10.1074/mcp.M700116-MCP200.
Teramoto R, Minagawa H, Honda M, et al. Protein expression profile characteristic to hepatocellular carcinoma revealed by 2d-DIGE with supervised learning. Biochim Biophys Acta. 2008;1784:764–772.
Ernst G, Melle C, Schimmel B, Bleul A, von Eggeling F. Proteohistography—direct analysis of tissue with high sensitivity and high spatial resolution using protein chip technology. J Histochem Cytochem. 2006;54:13–17. doi:10.1369/jhc.5C6764.2005.
Acknowledgments
We thank Dr. Paul Weinberger and Dr. Rhea-Beth Markowitz, Medical College of Georgia, Augusta, Georgia, USA, for comments during preparation of the manuscript. This work was supported by a US Public Health Service grant, R33 CA95941 (WSD).
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Lin, Y., Dynan, W.S., Lee, J.R. et al. The Current State of Proteomics in GI Oncology. Dig Dis Sci 54, 431–457 (2009). https://doi.org/10.1007/s10620-008-0656-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-008-0656-5