Abstract
Background
Physical and mechanical restraints used in treatment, care, education, and corrections programs for children are high-risk interventions primarily due to their adverse physical, emotional, and fatal consequences.
Objective
This study explores the conditions and circumstances of restraint-related fatalities in the United States by asking (1) Who are the children that died due to physical restraint? and (2) How did they die?
Method
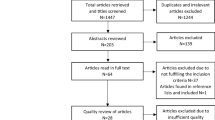
The study employs internet search systems to discover and compile information about restraint-related fatalities of children and youth up to 18 years of age from reputable journalism sources, advocacy groups, activists, and governmental and non-governmental agencies. The child cohort from a published study of restraint fatalities in the United States from 1993 to 2003 is combined with restraint fatalities from 2004 to 2018. This study’s scope has expanded to include restraint deaths in community schools, as well as undiscovered restraint deaths from 1993 to 2003 not in the 2006 study.
Results
Seventy-nine restraint-related fatalities occurred over the 26-year period from across a spectrum of children’s out-of-home child welfare, corrections, mental health and disability services. The research provides a data snapshot and examples of how fatalities unfold and their consequences for staff and agencies. Practice recommendations are offered to increase safety and transparency.
Conclusions
The study postulates that restraint fatalities result from a confluence of medical, psychological, and organizational causes; such as cultures prioritizing control, ignoring risk, using dangerous techniques, as well as agencies that lack structures, processes, procedures, and resources to promote learning and to ensure physical and psychological safety.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Restraints are “any manual method, physical or mechanical device, material, or equipment that immobilizes or reduces the ability of a person to move his or her arms, legs, body, or head freely” (Substance Abuse and Mental Health Services Administration (SAMHSA), 2010, p. 10). Physical or mechanical restraints (hereafter referred to as restraints) within children’s out-of-home care settings are used to contain a child’s acute physical behavior that is likely to cause injury to themselves or those around them. As safety interventions, restraints are never to be used as coercion, discipline, convenience, or retaliation (American Academy of Child & Adolescent Psychiatry, 2002; Centers for Medicare & Medicaid Services, 2008); but when restraints are employed, agency personnel, either alone or in a team, are asked to make a rapid series of consequential choices, under pressure, and within situations that are charged with anger, panic, aggression, counter-aggression, and violence (see Bystrynski et al., 2021; Geoffrion et al., 2021; Smith et al., 2017). Depending on the conditions that surround these events, the outcomes could range from a constructive engagement with learning and growth (Steckley & Kendrick, 2008) to emotional harm and resentment (Mohr et al., 2003), including the potential for serious injury or death (Aiken et al., 2011; Nunno et al., 2006, 2008; Weiss et al., 1998). Regardless of whether a physical injury occurs, restraints can be traumatic to children (Steckley, 2010), many of whom are already physically, developmentally (Norwood et al., 2011), or psychologically vulnerable due to a history of maltreatment and loss (Zelechoski et al., 2013). Restraints can jeopardize fragile therapeutic adult–child relationships, reinforce maladaptive interaction patterns and belief systems at all levels of an organization, and expose other vulnerable youth, as well as staff to ambient stress (Evans et al., 2002; Gorman–Smith & Tolan, 1998; Hollenstein et al., 2004; Steckley, 2010; Steckley & Kendrick, 2008). Restraint incidents may also be traumatizing for staff and children who witness the events (Bonner et al., 2002). Acknowledging these iatrogenic conditions, together with the documentation of fatalities (Weiss et al., 1998) and other severe and debilitating injuries (United States Government Accountability Office, 2008), some states have outlawed certain restraints such as the basket hold, single person, supine and prone restraints, and have limited restraint use as a protection against immediate danger to self or others (Butler, 2017; Masters, 2017).
Despite these efforts to limit and control restraints, fatalities remain a rare but grim consequence of their use. In the United States, there is no systematic documentation or examination of these incidents on the state or national level to prevent future events. Current reporting systems, such as the annual reports from U.S. Department of Health & Human Services Children’s Bureau on child maltreatment (United States Department of Health & Human Services & Administration for Children and Families, 2018) are dependent on reports provided by state child welfare systems which primarily involve familial child abuse or neglect fatalities. Only limited data are collected on fatalities that occur in foster, group, or residential care. Fatalities that occur outside of the child welfare system (e.g., within juvenile justice, mental health, community schools, or agencies for the developmentally delayed) are not reported through this avenue. The National Child Death Review case reporting system, a state-based system with national coordination (Palusci & Covington, 2014), is voluntary and primarily covers deaths due to drownings, sudden unexplained infant deaths, and automobile accidents. We see no systematic data collection, reviews, or analyses within this system regarding children’s restraint-related fatalities.
The United States Government Accountability Office (2009) and the United States Department of Justice (2009) have published reports on children’s injuries and deaths caused by restraints in schools and juvenile justice centers. These reports have led to substantial regulatory and legislative reforms, such as banning supine, prone, or all floor restraints or restraints on young children and requiring care agencies to implement effective restraint reduction strategies. However, they provide few clues about the frequency of restraint fatalities or an analysis of the root causes for the bulk of these tragedies.
Purpose
The current study is an extension of an initial examination of eleven years (1993–2003) of restraint fatalities published in 2006 (Nunno et al., 2006). This study maintains the original article’s purpose of exploring the conditions and circumstances of restraint-related fatalities to inform restraint and injury reduction initiatives. The data in this paper included and followed up on the 44 fatalities from 1993 to 2003 and expanded the study’s scope to include restraint deaths in community schools, hospitals, and other centers that treated children were medically fragile or who had physical and emotional difficulties. This expansion of the study’s scope and the increased sophistication of the search methodology and internet resources led to the discovery of an overcount of one fatality that was counted twice reported in 1993 and 10 additional restraint deaths that occurred from 1993 to 2003 not discovered in the original study. This study also reports 26 additional fatalities from 2004 to 2018.
This study adheres to the original questions asked in Nunno et al. (2006), “Who are the children and adolescents that die in physical and mechanical restraints?” and “How did they die?” However, the current study expands the inquiry further to explore the latter question, not only from a medical perspective, but from ecological and systems-level perspectives to address the multiple failures contributing to these fatalities. In the 14 years since the publication of the original study, a professional consensus has emerged that restraints are safety interventions that do not effectively teach self-control and that have little or no therapeutic benefit (American Academy of Child & Adolescent Psychiatry, 2016; American Psychiatric Nurses Association, 2018; British Institute for Learning Disabilities, 2014). We hold that a death resulting from a safety intervention requires a thorough examination involving critical scrutiny and the steps taken to minimize risks to children’s safety. Such scrutiny should determine whether a safety intervention creates more risk than the behavior it seeks to contain or control.
Methodology
Because there is no reliable central data source for restraint fatalities in the United States, the current study, as in the 2006 study, employed available internet search systems to discover and compile records of each of these fatalities. The U.S. Department of Justice has found that methodologies such as print and television media coverage, reports from advocacy groups, activists, and researchers can provide reliable data (Edwards et al., 2018) on these low-frequency, high-consequence events. The use of media reports from reputable journalism sources has also been used successfully to examine restraint fatalities in social care settings within the United Kingdom (Aiken et al., 2011; Paterson et al., 2003) and child fatalities in intercountry adoption of Russian children in the United States (Hegar et al., 2015).
Our search was limited to information that is part of the public record. We conducted systematic searches using Google™, LexisNexis™, Access World News™, and Factiva™ for reports of restraint-related deaths from 1993 to 2018 employing keywords such as restraint of patients, physical and mechanical restraints, fatalities in restraints, fatal child restraints, child restraint deaths, child deaths in residential care, restraint deaths in schools, restraint deaths in juvenile justice, restraint deaths in developmental disabilities, and restraint deaths in mental health centers. Our selection criteria included fatalities of any child or young person 18 years or younger who resided in or was in the care of any public or private setting serving children in the child welfare, mental health, developmental disability, or juvenile justice systems. Differing from the 2006 study, we added restraint fatalities that occurred in schools and foster homes. Schools represented in this research are public, private, or charter schools not affiliated with an agency within the child welfare, juvenile justice, mental health, or developmental disability service systems. We classified a fatality that occurred in a residential school as a residential fatality. We recorded each fatality’s details in a spreadsheet and checked our information against existing reports (Norwood et al., 2011) and websites (Zehder, 2017) that compile information on child fatalities. To the extent available, we recorded child, staff, and agency characteristics associated with each fatality, along with type and position of the restraint, circumstances surrounding the event, and type of fatality review or investigations performed by law enforcement, a governmental body, or an advocacy group. We conducted follow-up searches on fatalities initially reported in Nunno et al. (2006) through internet searches using specific child, staff, and agency names to find additional regulatory, civil, and criminal outcomes. If new information contradicted previously gathered information, both sources were noted in the database. Although we utilized only public information, we chose to de-identify any child, staff, or agency information in this article. The methodology used for this effort was reviewed and approved by the authors’ Institutional Review Board.
Findings
Fatalities by State and Agency Type
Overall, this study discovered 79 restraint-related fatalities between 1993 and 2018. These are summarized in two 13-year increments, from 1993 to 2005 (two years beyond the original study period in Nunno et al. (2006) and between 2006 to 2018. Comparing the frequency of restraints between these two periods provides evidence of whether the frequency of restraint deaths has remained stable, increased, or decreased. Fifty-nine fatalities occurred from 1993 to 2005, and 20 from 2006 to 2018, a decline of over 65% (Table 1). Of the 79 total fatalities, 27 occurred in agencies serving children within a State child welfare system (e.g., residential treatment centers, group homes, or foster homes), 22 occurred in psychiatric agencies, 13 in juvenile corrections, 14 in programs for physically disabled or developmentally-delayed children, two in community school programs for physically disabled or developmentally delayed children, and one in a private unlicensed wilderness camp.
The fatalities reported here occurred within 30 states. The total number of fatalities per state during the 26-years ranged from 1 to 17 (Table 2). Although most states had only one or two fatalities, two had far more: Texas (n = 17) and Pennsylvania (n = 7). Over the study period, six individual agencies experienced multiple fatalities that ranged from 2 to 4 fatalities per agency.
Age, Gender, Race/Ethnicity
Of the fatalities, 56 were boys with a mean age of 14.4 years, and 23 were girls with a mean age of 15.0 years. We were able to verify the race/ethnicity of 51 child fatalities, while information on race/ethnicity was not available for the remaining 28. Table 3 provides a breakdown of the gender, age, and racial characteristics.
Immediate Cause of Death
The leading cause of death among the fatalities discovered from 1993 to 2018 was asphyxia (Table 4). Asphyxia is the lack of oxygen or excess carbon dioxide in the body due to irregular or disturbed respirations (asphyxia, 2003) The body's position during restraint or compression from the adults’ weight on the victim's face, neck, chest, or back may contribute to asphyxiation (Chmieliauskas et al., 2018; Paterson et al., 2003). The next most common cause of death was cardiac arrhythmia (heart rhythm difficulties). Other causes included exertion (physical agitation or stress during a restraint),Footnote 1 internal bleeding, blunt trauma, strangulation, cardiac hypertrophy (enlarged or thickening of the heart walls), aspiration, strangulation, sudden death, hyperthermia, and natural causes.
In a limited number of fatalities, the details included in reports revealed clues to the context surrounding the restraint event. For example, one report listed the cause of death as cardiac arrhythmia precipitated by stress and acute asphyxia. In another fatality, the report indicated that the child died in a prolonged prone physical restraint associated with extreme distress and physical agitation. Asphyxiation, acute respiratory distress, and a blood infection were reported as the cause of death in a third case, while another described a fatality due to dehydration while in mechanical restraints. In these last two fatalities, the conditions were cited in the plaintiff’s civil suit as evidence of poor medical care, inadequate supervision, and neglect by the agency.
Type and Position of the Restraint
The type and position of a restraint can significantly affect its potential to cause injury or death (Sethi et al., 2018). In our study, fatalities occurred while children were placed in physical and mechanical restraints and in positions described as seated, prone (face down), side, or supine (face up) positions. Of the 63 fatalities related to physical restraint, 38 happened in a prone position, three in a basket hold, two in a seated position, and one in a side position. In the remainder of the physical restraints, the child's position was unknown or could not be accurately determined. Thirteen fatalities involved mechanical apparatus, such as straps, boards, other rigid devices, handcuffs, or children were wrapped inside of a carpet, blanket, or mattress. Of these 13 deaths, three occurred in a supine position, five in a prone position, one while the child was seated, and in four fatalities the position was unknown. In three of the deaths, a determination could not be made if the restraint was physical or mechanical or in what position the children perished.
Rationale for the Restraint
From the media reports, we documented one or more rationales for the use of restraints in about half of all deaths. The events leading up to these fatal physical restraint incidents were often triggered by relatively benign child behaviors that do not appear to have been threatening or dangerous. These events involved non-compliance with staff demands or program requirements, such as remaining quiet or sitting properly without wiggling. In other examples, the precipitating event involved children refusing to give up a ball, accept exercise willingly as a punishment, put on shoes, take off a hoodie, or leave or return to a cottage, a classroom, or a gym. Non-compliance rarely constituted a behavior likely to result in injury to the child or others, and when it entailed refusal to release an object, that object was not likely to have been seen as a weapon. For example, after reviewing a fatal restraint initiated for non-compliance, a judge described that restraint “as an inappropriate disciplinary tactic, using excessive, unnecessary force out of proportion to the minimal risk posed by the child’s action” (United States Government Accountability Office, 2009, p. 17). Another report cited “a dangerous combination of high rates of prone restraints and a low standard of initiating a restraint” as contributing to the disproportionate application of restraint to the behavior exhibited by the young person (United States Department of Justice, 2009, p. 10).
Other Critical Factors in the Fatality
We discovered other factors that were proximal to the deaths and may have contributed to the fatality. Signs of breathing restrictions or distress were indicated in 14 fatalities based on the children saying “I can't breathe” or “I give [up]” before the loss of consciousness or death. Reports indicated that in 10 fatalities, children vomited or urinated and that five children turned blue during the restraint. Ten fatalities occurred within the confines of a seclusion, time-out, or cool-down room.
Some deaths were related to the use of dangerous techniques such as a chokehold, headlock, or staff placing weight or positional pressure on the child’s upper torso, neck, chest, or back. Of the 38 prone-related deaths involving physical restraint, eight involved between two and eight staff lying on the child, six involved staff crossing children’s arms across their chest while prone, and four involved a staff member sitting on children. Two prone fatalities were the result of a neck or chokehold. Four prone fatalities occurred in conjunction with an escort in which a staff member held the children’s arms behind their back, forced them forward, and dropped them to the ground facedown.
Legal or Regulatory Actions
Twenty-five of the fatalities resulted in civil suits against the organization and its employees. The majority of the civil cases resulted in settlement agreements between the plaintiffs and the defendants, with the settlement terms often held confidential. In many instances, fatalities were reviewed or investigated by local or state police officials. Twenty-four fatalities resulted in some criminal action ranging from criminal investigations to grand jury hearings or criminal trials. We could only document three convictions of individuals among the 79 fatalities over the study period. In the remaining cases, charges were not pursued, were dropped, or grand juries refused to indict them. In many cases, civil and criminal actions were concurrent.
In 38 fatalities, federal or state authorities, or appropriate licensing bodies, investigated whether staff’s handling of the incident could be abuse, neglect, regulatory, or licensing violations. Child placing agencies, after learning of a fatality, often terminated all other placements within those entities. Four agencies with fatalities, especially those with multiple fatalities, were closed by their boards, lost their license temporarily, or went bankrupt. One organization with multiple care locations changed its name and resumed business as a newly formed entity.
Discussion
Fatal restraints found by our methodology suggest that fatalities were not due to one apparent factor but to a confluence of medical, psychological, and organizational factors and dynamics (Roy et al., 2019). Confluence refers to the convergence of several factors or elements that interact to place the child at greater or lesser risk of injury or death (Sethi et al., 2018). Figures 1 and 2-Confluence of Factors Contributing to the Fatality-portray de-identified composite narratives (Willis, 2019), based on events present in the 79 fatalities reviewed, that illustrate how multiple factors interact and result in fatal restraints.
Ollie was removed from his parent’s custody when he was 9 years old due to severe malnutrition and neglect. He often was found foraging the neighborhood for food and ate out of dumpsters. His parents’ parental rights were terminated two years later. Ollie was diagnosed as having post-traumatic stress syndrome and had a difficult time concentrating on tasks. There was some evidence that he had received a brain injury, although there was never a diagnosis. His placements in multiple foster homes failed because of his severe outbursts when he did not have access to food when hungry, but he never attacked or became violent towards others. He had been in his latest therapeutic foster home placement for eighteen months and was doing well. His outbursts were diminishing in frequency and intensity. His foster parents used time out as a behavior support, and he was learning to self-isolate when he was frustrated. He was beginning to relate to other children and was able to participate in neighborhood games. Ollie was placed in a new special education classroom in a mental health day treatment program to prepare him for a community school program. The classroom housed both children who resided in residential and foster homes and specialized in behavior management. His foster parents worried that the new classroom would set Ollie back and feared that his food anxiety would increase and be misunderstood. In class one day Ollie became agitated because he was hungry. He failed to respond to his teacher’s repeated, vocal commands to calm himself and sit down. He paced the classroom and when he did not follow the teacher’s orders, the teacher placed him in a chair and held him via a seated basket hold with his arms around his torso. When Ollie, who was 5′1″ and 130 pounds, continued to struggle, she placed him face-down on the floor with his crossed arms still under him. His teacher, who weighed 225 pounds and was 6″1’, lay on top of him while the aide held his legs. During the restraint Ollie said, “I can’t breathe” and “I give”. The assistant principal asked the teacher to end the restraint after 15 min according to school policy. The aide and the teacher sat Ollie, who was limp, in a chair and wiped drool from his mouth. The assistant principal reported that he thought he was playing possum. The procedure was witnessed by a teacher aide, a school assistant principal, and other students. While the state protective authorities determined that the teacher’s response was abusive and an administrative judge upheld the ruling saying that he thought the teacher was “reckless”, the school and the restraint trainers continued to support the teacher’s restraint methods
Plymouth was upset that the shirt she loved was missing from her closet. She walked angrily to her friend’s room to accuse her of taking the shirt but was escorted back to her room by a staff. She was agitated and went immediately to her closet to show the staff that it was gone. When she was at the closet, she retrieved a small object in her hand. Staff asked to see what it was, but she refused to comply. A supervisor, hearing the Plymouth disturbance, told the staff person to take care of business in there because it was time for dinner. The situation escalated and the staff person immediately initiated a single person restraint, but lost her balance and fell on Plymouth who landed face up on her back. The staff person remained laying on Plymouth’s torso to maintain control. Plymouth was upset that the shirt she loved was missing from her closet. She walked angrily to her friend’s room to accuse her of taking the shirt but was escorted back to her room by a staff. She was agitated and went immediately to her closet to show the staff that it was gone. When she was at the closet, she retrieved a small object in her hand. Staff asked to see what it was, but she refused to comply. A supervisor, hearing the Plymouth disturbance, told the staff person to take care of business in there because it was time for dinner. The situation escalated and the staff person immediately initiated a single person restraint, but lost her balance and fell on Plymouth who landed face up on her back. The staff person remained laying on Plymouth’s torso to maintain control. Plymouth died from mechanical asphyxiation while staff lay on her in a supine position on the floor. Her death was the fourth restraint-related fatality to occur within the umbrella organization over the past eight years. Just days prior to Plymouth’s death, the state’s regulatory agency placed the treatment center on probation because of persistent concerns cited, such as multiple restraints, the frequent use of PRNs (as the need arises) to control behavior, and the lack of treatment and crisis plans for individual children. In the previous two years, the administration and care staff were cited for abuse when they “encouraged” competitions where the girls wrestled with one another for food and snack prizes
Medical Factors
Generally, staff members who employ restraints have limited or no medical training or access to on-site emergency medical resources or even knowledge about the child’s medical profile and risk. Although this is especially relevant within child welfare and juvenile justice agencies, medical resources and information can be scarce, unreliable, or unavailable even in organizations serving young people with mental health disorders or developmental delays. These dynamics concur with the findings examining restraint deaths in the United Kingdom (Aiken et al., 2011). Further, our research found that staff members with little or no medical background made medical decisions during a restraint which contributed to multiple child deaths. For example, one staff member refused a known asthmatic child on medication his prescribed inhaler during a restraint. After repeatedly requesting his inhaler, staff involved in the restraint denied his request because they believed that he had no difficulty breathing and that his calls for help were not genuine. His plea “I can’t breathe” became the child’s last words.
Psychological Factors
Youth in therapeutic residential settings, group care, foster care, psychiatric hospitals, and juvenile justice settings have often experienced a chronic history of complex trauma, including neglect, physical or sexual abuse, and exposure to household and community violence (Briggs et al., 2014; Zelechoski et al., 2013). Their trauma histories contribute to high clinical need levels, and their often severe behavioral dysregulation can present profound challenges for the adults charged with ensuring their safety and healthy development (Gonzalez, 2014). Trauma-affected children are highly reactive to perceptions of threat and are particularly vulnerable to the traumatic effects of being physically restrained while in these environments. Under even the best circumstances, these experiences can undermine children’s sense of safety (Porges, 2020) and trigger "shame, humiliation, rage, and fear" (Sethi et al., 2018, p. 140). Although staff’s intention may be to ensure safety, for many children, restraints create a sense of terror, causing extreme physiological reactivity (e.g., hyperventilation, racing heart rate) that overwhelms their capacity to regulate their emotions and behavior (Porges, 2017, 2020), placing them at increased medical risk. Potentially fatal elements can be introduced to this mix. Staff members may consider the restraint as routine and naively respond to the child’s “fight or flight” behavior by applying more pressure to subdue the child. Staff might also misattribute youth behaviors to bad choices or character in need of “consequences” or retribution (O’Toole & Sahar, 2014). In these cases, staff may apply hazardous and misguided tactics that compromise children’s breathing and cardiac capacity or inflict severe injury to the head, neck, or torso, increasing the child’s extreme emotional reactivity and stress. As a pathologist who oversaw a restraint fatality explains: “Emotional stress, physical stress, just any kind of alteration in the physiology where the ability of our body to function as it does (is compromised) can certainly increase the risk of sudden death in any of us” (Savali, 2017, p. 8).
Organizational Factors
We recognize that few, if any, fatal restraints could be attributed to individual malice, nor were they due solely to the mistakes of the individual staff involved. Rather than focusing on assigning blame to individual staff, we advocate viewing each incident as a failure of the entire organization and identifying organizational deficiencies that contributed to them. Fatal restraints often were supervised or observed by others, sometimes even by medical personnel, and involved the participation of multiple staff. These fatal restraints were often a team event where no team member effectively monitored the child’s safety. As was previously stated, signs of breathing restrictions or distress were indicated in 14 fatalities based on the children saying, “I can't breathe” or “I give [up]” before a loss of consciousness or death. In 15 fatalities, children vomited, urinated, or turned blue during the restraint. These signals should have been detected by an adult monitoring these events and immediately triggered a change in tactics or discontinuation of the restraint. As one judge who reviewed the details of a death of a seven-year old girl commented, “there were a lot of other people who made decisions that led up to her death” (Disability Rights/Wisconsin, 2008). In another fatality, the district attorney was unable to hold an individual or individuals responsible because he could not “narrow it down to the actions of one.” (Bernhard & Kohler, 2010, p. 19). Ultimately, the use of seriously flawed intervention techniques, where compliance, control, and punishment were the goal and where multiple people were involved, appeared to trigger a form of bystander apathy (Grissinger, 2012), leading to safety deafness among the adults employing the restraints. This safety deafness was even allowed as a defense in one case where a Grand Jury indicted six defendants as responsible for a child’s death during a restraint. The judge reviewing the indictment decided that the state’s attorney could not show that the defendants, who had no medical background, were aware of, or should have been aware of any risk created by refusing an asthmatic child’s request for his medication during a highly stressful event.
Investigations of these agencies by regulatory, law enforcement, or child protective authorities revealed that fatalities were often associated with violations of law and regulations. One agency even convinced the state licensing agency to assign an investigator who would be more lenient towards the organization in its application of regulatory enforcement. When thorough investigations were completed, they found that agencies lacked the essential organizational structures, processes, procedures, and resources needed to minimize safety risks to children during restraints. Organizational factors that contributed to the fatal events were especially evident in, but not limited to, agencies that experienced multiple fatalities. These agencies often were cited for sub-standard treatment planning and assessments and for the punitive use of restraints as a consequence for rule-breaking and disruption rather than limiting their use to protecting children from harm. In one startling example, an agency was placed on probation by the state four days before their latest fatality because of persistent safety-related concerns about the facility’s irresponsible and high-risk practices with the children in its care. The state licensing monitor conducting the review before the fatality incident noted the agency’s frequent use of emergency restraints and medications to subdue children. The monitor also noted no individualized client plans and that the written treatment, safety, or crisis management plans were essentially the same for all clients. Two years prior, the center was cited for abuse when staff members encouraged girls to fight one another for snacks.
Utilizing restraints without robust organizational protections in place poses serious, persistent safety breaches with immediate, foreseeable, and severe physical and emotional consequences for any vulnerable child's safety, security, and health. These organizational structures and processes are critical to preventing the misuse of physical restraint and ameliorating the harmful consequences of these high-risk interventions when they do occur.
Limitations
There are limitations with the methodology we used to assess restraint-related fatalities. The absence of a central repository for data such as the U.S. National Child Death Fatality Review Case Reporting System (Palusci & Covington, 2014) on these low frequency, high consequence events makes them difficult to study. Therefore, examining established and respected media publications, public advocacy documents, and other governmental and non-government reports is one of the few methodologies available to ascertain the prevalence and conditions contributing to these fatalities. This methodology is dependent on secondary source materials or reports given through the lens of media informants. Our experience with informant reports is that they come initially from law enforcement or agency spokesperson information; later, investigation results may come from district attorneys, grand juries, or spokespersons for families and state officials. Public advocacy groups or legislative personnel trigger reports published months after an event when the fatality's public memory has faded. Rarely are autopsies or depositions made public. Access to information about these fatalities appears dependent on the public's long-term interest in these fatalities, their perceptions of the child victims, and whether these children have robust and tenacious advocacy.
Cutbacks and closings at local and regional newspaper outlets may have hindered our ability to discover child fatalities through media reports. Nevertheless, few alternatives remain to investigate and report on local events such as child fatalities (Abernathy, 2018). Given that many juvenile justice and child welfare agencies reside in rural areas with scarce local media, especially newspapers, findings presented here likely undercount child fatalities.
Future Research
This study has highlighted the need for more complete data since basic and essential information regarding these fatalities were not available. For example, knowing the racial and ethnic composition of the youth fatalities is critical. Restraints are applied at a disproportionate rate to children and adolescents of color, especially children with physical and emotional disabilities (Donovan et al., 2003; National Disability Rights Network, 2012; Toriello et al., 2003; United States Commission of Civil Rights, 2019). Unfortunately, this methodology’s missing data limits our ability to determine whether any such disproportionality translates to fatalities among this vulnerable population. Another critical area to examine in future research is what factors such as legislation and regulatory reforms in restraint use, the decrease in residential care placements, and length of stay contributed to the 65% decline in fatalities from 1993 to 2005 to 2007–2018.
Additionally, reports typically lacked information such as the duration of the fatal restraint, the frequency of prior restraints with the victim child or for the agency overall, the frequency of prior restraints with the staff involved, details about the child's treatment, including their medication usage prior to and during the restraint, safety and individual crisis management plans, agency policy, training, and supervision records. Without these evidentiary elements, it is not easy to assess how these events occurred or what remediation strategies might reduce their risk of recurrence.
In most cases, we were unable to review autopsy reports to verify the initial cause of death attributed to the incident by the agency representatives and reported by the media to determine how the restraint and other injuries contributed to a death or whether the injuries happened before, during, or after the restraint. Reviewing a complete autopsy report (including toxicology reports) with medical experts would be essential to a more robust review of the circumstances of the restraint, as the composite narrative below reveals:
A single staff restrained a 250 pound 17-year-old adolescent on the floor, and after a few minutes, the adolescent became limp and unresponsive. An autopsy showed evidence of a traumatic head injury, evidence of chest compression (which may have occurred during resuscitation), and internal bleeding. The autopsy reported that the adolescent suffocated. The initial report made by the agency to the young person’s parents stated that death was due to congestive heart failure.
Analyzing fatal events with multiple and complex causes would ideally include direct access to participants, autopsies, the location of the fatality, the events that triggered the restraint, and the culture and climate of the organization, including the levels of physical and verbal aggression (see Bystrynski et al., 2021; Geoffrion et al., 2021; Smith et al., 2017). In addition, variation and shifts in state-level regulations and oversight policies would also help explain fatality rates over time. Including such elements was beyond the scope and resources of our project but should be incorporated into future investigations.
Practice recommendations
This paper focuses on the use of physical and mechanical restraints on children that resulted in a fatality. We examined available information about each incident, including the circumstances that increased the potential for adverse and fatal consequences. Some of the circumstances surrounding these fatalities may have been unavoidable, while some were clearly due to errors in judgment, inadequate training, lack of knowledge, or social and organizational pressure for staff to use coercion to maintain control and compliance. Some, however rare, may be due to personal or professional malfeasance.
We offer the following considerations for systems and organizations that use restraints as safety interventions with children to lessen the risk of harm associated with restraints; and to increase the transparency of their use for families, children, staff, and the general public. We consider the introduction, implementation, and adherence to these recommendations to be the responsibility of all leadership levels in child-serving systems that permit restraints.
-
1. Restraints are high-risk safety procedures that can result in severe injury or death. They are safety interventions for acute physical behavior that places the child or another person in immediate danger and produces emotional trauma for both children and adults.
-
2. A restraint is likely abusive if it harms or places the child at higher risk than the acute behavior it aims to contain or control, or if the restraint technique is unapproved or misused, such as coercion, discipline, convenience, or retaliation.
-
3. Restraints have little to no therapeutic benefit. They can be counter-productive to treatment, disrupt essential adult-child relationships, and impede children’s social and emotional learning, especially among vulnerable children with severe trauma histories.
-
4. Any organization and any individual using restraints must recognize and accept responsibility for their potential to cause serious injury, emotional trauma, or death; these untoward outcomes can lead to allegations of child maltreatment, criminal and civil actions, penalties, liability, and financial judgments.
-
5. Significant reductions in restraints are possible through attention to high-quality care, programming that matches children's developmental and relationship needs, high quality and competency-based staff training, family involvement, staff accountability, supervision, and monitoring. Employing a program model that includes educating staff about the effects of trauma and trains staff to rely less on coercive tactics and more on building appropriate developmental relationships may provide a milieu that inherently de-escalates agitation and prevents interpersonal violence (Bloom & Farragher, 2013; Farragher, 2002; Hodgdon et al., 2013; Izzo et al., 2016; Nunno et al., 2017; Zegers et al., 2008; Zelechoski et al., 2013).
-
6. By allowing the use of restraints, leaders ask staff to make high-consequence choices rapidly and under pressure. To mitigate the risks associated with this practice, organizational structures and processes are required to ensure:
-
• Training to competence for behavior support and non-aggressive crisis management strategies and tactics
-
• Organizational cultures and climates where the paramount concern is child safety
-
• Knowledge of the child's medical history and condition, as well as their abuse, neglect, and trauma history
-
• Informed parental consent
-
• Informed child assent
-
• The development of safety plans or individual crisis support plans that make critical safety information available to staff before any restraint is initiated
-
• Monitoring by supervisors or medical personnel during a restraint
-
• Staff and team debriefing and supervision after restraint
-
• Debriefing sessions to help both staff and children process and learn from each restraint incident
-
• Individual and organizational self-assessment and learning regarding restraint reduction
-
• Monitoring of restraint incidents by external regulatory bodies
-
These considerations should guide restraint use to ensure immediate safety and promote positive adult–child relationships, learning, and well-being.
Conclusion
Adverse incidents tend to result not from one definite cause but instead from a confluence of several causes and events (Roy et al., 2019). The events surrounding the restraint fatalities in this study reflect this phenomenon. This research offers clues suggesting that restraint fatalities occur in organizations with cultures and climates that prioritize compliance and control, ignore restraint risk potential and well-established risk reduction strategies, and fail to ensure individual and organizational learning from adverse events. There appears to be a lack of essential organizational structures, processes, procedures, resources, and determination to reduce risk through training staff to competency, monitoring, and supervision within many of these agencies, especially among agencies that experienced multiple prior fatalities, that had histories of abuse and neglect reports, regulatory complaints and violations. The lack of training and a retrospective safety and risk assessment process may have perpetuated these agencies’ unsafe practice norms, thus compromising children's treatment and safety.
In many of these reports, there was little evidence that staff either had the resources or the competence to administer a restraint under highly volatile circumstances without reliance on strategies that increased the risk for an adverse outcome. The staff demonstrated poor judgment by utilizing dangerous techniques like chokeholds or applying weight on the child's torso, neck, chest, or back, which produce significant medical risk regardless of whether the child is supine, prone, seated, or standing. These fatality incidents illustrate that children’s deaths resulted not from the restraints position alone but from a combination of staff’s lack of competency in behavior management and support, their use of dangerous techniques, and the lack of organizational procedures to reduce safety risks. The evidence points to the conclusion that any restraint in any position can cause death when carried out using methods that compromise breathing, exceeds cardiac capacity, or has the potential to inflict severe injury to the head, neck, or torso.
Any agency that provides care, custody, and treatment to children assumes a position of trust that they will ensure their protection and supervision. Embedded in this trust is the expectation that any intervention will be carefully assessed as to whether it serves the children’s best interests and ensures their physical and emotional safety. Expressly, the duty of care demands cognizance and foreseeability of any physical, emotional, and developmental risk associated with the use of high-risk interventions and that the agency incorporate robust risk-reduction strategies into their procedures and practices. The public's trust in these safety interventions and their continued use demands that any high-risk intervention creates less risk than the behavior it contains.
Change history
18 September 2021
A Correction to this paper has been published: https://doi.org/10.1007/s10566-021-09650-0
Notes
Associated with a controversial syndrome excited delirium characterized as extreme agitation during a restraint (Council on Psychiatry and Law, 2020).
References
Abernathy, P. M. (2018). The expanding news desert. UNC Press: Chapel Hill. https://www.newsdesert.com
Aiken, F., Duxbury, J., Dale, C., & Harbinson, I. (2011). Review of the medical theories and research relating to restraint related deaths. Caring Solutions.
American Academy of Child and Adolescent Psychiatry. (2002). Practice parameter for the prevention and management of aggressive behavior in child and adolescent psychiatric institutions, with special reference to seclusion and restraint. Journal of the American Academy of Child and Adolescent Psychiatry, 41(2), 4–24.
American Academy of Child and Adolescent Psychiatry. (2016). Policy statement: Coercive interventions for reactive attachment disorder. Author. https://www.aacap.org/aacap/Policy_Statements/2003/Coercive_Interventions_for_Reactive_Attachment_Disorder.aspx
asphyxia. (2003). Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health. In Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health. Retrieved August 4 2021, from https://medical-dictionary.thefreedictionary.com/asphyxia
American Psychiatric Nurses Association. (2018). Position statement on the use of seclusion and restraint. Author. https://www.apna.org
Bernhard, B., & Kohler, J. (2010). Girl, 16, dies during a restraint at an already-troubled hospital. St. Louis Post-Dispatch - St Louis Today, 1–21. http://stltoday.com/news/local/metro//girl-dies-during-restraint--at-an-already-troubled-hospital/article_4a10ccdd-5d08-52bd-bfc5-c435014aa09b.html
Bloom, S., & Farragher, B. (2013). Restoring Sanctuary: A New Operating System for Trauma-Informed Systems of Care. Oxford University Press.
Bonner, G., Lowe, T., Rawcliffe, D., & Wellman, N. (2002). Trauma for all: A pilot study of the subjective experience of physical restraint for mental health inpatients and staff in the UK. Journal of Psychiatric and Mental Health Nursing, 9, 465–473.
Briggs, E. C., Greeson, J. K. P., Layne, C. M., Fairbank, J. A., Knoverek, A. M., & Pynoos, R. S. (2014). Trauma exposure, psychosocial functioning, and treatment needs of youth in residential care: preliminary findings from the NCTSN core data set. Journal of Child & Adolescent Trauma, 5, 1–15.
British Institute for Learning Disabilities. (2014). BILD Code of Practice for minimising the use of restrictive physical interventions, planning, developing and delivering training: A guide for purchasers of training, training organisations and trainers (4th ed.). Author.
Butler, J. (2017). How safe is the schoolhouse? An analysis of state seclusion and restraint laws and policies. Autism National Committee. http://www.autcom.org/pdf/HowSafeSchoolhouse.pdf
Bystrynski, J., Braun, M. T., Corr, C., Miller, D., & O’Grady, C. (2021). Predictors of injury to youth associated with physical restraint in residential mental health treatment centers. Child and Youth Care Forum, 50(3), 511–526. https://doi.org/10.1007/s10566-020-09585-y
Centers for Medicare & Medicaid Services. (2008). Hospitals – Restraint/Seclusion Interpretive Guidelines & Updated State Operations Manual (SOM) Appendix A. In Centers for Medicare & Medicaid Services (Ed.), S&C-08–18 (pp. 1–348). Baltimore, MD: Department of Health & Human Services.
Chmieliauskas, S., Mundinas, E., Fomin, D., Andriuskeviciute, G., Laima, S., Jurolaic, E., Stasiuniene, J., & Jasulaitis, A. (2018). Sudden deaths from positional asphyxia. Medicine, 97(24), 1–5. https://doi.org/10.1097/MD.0000000000011041
Council on Psychiatry and Law. (2020). Position statement on concerns about use of the Term “Excited Delirium” and appropriate medical management in out-of-hospital Contexts. In APA Official Actions. Washington, DC: American Psychiatric Association.
Disability Rights/Wisconsin. (2008). A tragic result of failure to act: The death of Angelika Arndt. Disability Rights/Wisconsin. http://www.charlydmiller.com/LIB13/2008Nov26AngellikaArndt.pdf
Donovan, A., Plant, R., Peller, A., Siegel, L., & Martin, A. (2003). Two-year trends in the use of seclusion and restraint among psychiatrically hospitalized youths. Psychiatric Services, 54(7), 987–993.
Edwards, F., Esposito, M. H., & Lee, H. (2018). Risk of police-involved death by race/ethnicity and place, United States, 2012–2018. American Journal of Public Health, 108(9), 1241–1248. https://doi.org/10.2105/AJPH.2018.304559
Evans, D., Wood, J., & Lambert, L. (2002). Physical restraint - Part 2: Minimization in acute and residential care facilities. Best Practice, 6(4), 1–6.
Farragher, B. (2002). A system-wide approach to reducing incidents of therapeutic restraint. Residential Treatment for Children and Youth, 20, 1–14.
Geoffrion, S., Lamothe, J., Frasera, S., Lafortune, D., & Dumais, A. (2021). Worker and perceived team climate factors influence the use of restraint and seclusion in youth residential treatment centers: Results from a mixed-method longitudinal study. Child Abuse and Neglect: An International Journal, 111, 104825. https://doi.org/10.1016/j.chiabu.2020.104825
Gonzalez, M. J. (2014). Mental health care of families affected by the child welfare system. Child Welfare, 93(1), 7–58.
Gorman-Smith, D., & Tolan, P. (1998). The role of exposure to community violence and developmental problems among inner-city youth. Development and Psychopathology, 10(1), 101–116.
Grissinger, M. (2012). Actively caring for the safety of patients: overcoming bystander apathy. Pharmacy and Therapeutics, 37(6), 317–319.
Hegar, R. L., Verbovaya, O., & Watson, L. D. (2015). Child fatality in Intercountry adoption: What media reports suggest about deaths of Russian children in the U.S. Children and Youth Services Review, 55, 182–192. https://doi.org/10.1016/j.childyouth.2015.06.002
Hodgdon, H. B., Kinniburgh, K., Gabowitz, D., Blaustein, M. E., & Spinazzola, J. (2013). Development and implementation of trauma-informed programming in Youth residenial treatment centers using the ARC framework. Journal of Family Violence, 28(7), 679–692. https://doi.org/10.1007/s10896-013-9531-z
Hollenstein, T., Granic, I., Stoolmiller, M., & Snyder, J. (2004). Rigidity in parent-child interactions and the development of externalizing and internalizing behavior in early childhood. Journal of Abnormal Child Psychology, 32, 595–607.
Izzo, C. V., Smith, E. G., Holden, M. J., Norton, C. I., Nunno, M. A., & Sellers, D. E. (2016). Intervening at the setting-level to prevent behavioral incidents in residential child care: Efficacy of the CARE program model. Prevention Science, 17, 554–564. https://doi.org/10.1007/s11121-016-0649-0
Masters, K. J. (2017). Physical restraint: A historical review and current practice. Psychiatric Annals, 47(1), 52–55. https://doi.org/10.3928/00485713-20161129-01
Mohr, W. K., Petti, T. A., & Mohr, B. D. (2003). Adverse effects associated with physical restraint. Canadian Journal of Psychiatry, 48(5), 330–337.
National Disability Rights Network. (2012). School is not supposed to hurt. Author. www.ndrn.org
Norwood, L., Ciccone, J. R., Kennedy, D. M., Moy, D. L. F., Allrich, M. K., & Naiditch, Z. (2011). National review of restraint related deaths of children and adults with disabilities: The lethal consequences of restraint. Equip for Equality.
Nunno, M. A., Day, D. M., & Bullard, L. B. (Eds.). (2008). For our own safety: Examining the safety of high-risk interventions for children and young people. Child Welfare League of America.
Nunno, M. A., Holden, M. J., & Tollar, A. (2006). Learning from tragedy: A survey of child and adolescent restraint fatalities. Child Abuse and Neglect: The International Journal, 30(12), 1333–1342.
Nunno, M. A., Smith, E. G., Martin, W. R., & Butcher, S. (2017). Benefits of embedding research into practice: An agency-university collaboration. Child Welfare, 94(3), 113–133.
O’Toole, M. J., & Sahar, G. (2014). The effects of attributions for crIme on attitudes toward prison reform. Applied Psychology in Criminal Justice, 10(1), 46–65.
Palusci, V. J., & Covington, T. M. (2014). Child maltreatment deaths in the U.S. national child death review case reporting system. Child Abuse and Neglect: The International Journal, 38(1), 25–36. https://doi.org/10.1016/j.chiabu.2013.08.014
Paterson, B., Bradley, P., Stark, C., Saddler, D., Leadbetter, D., & Allen, D. (2003). Deaths associated with restraint use in health and social care in the UK. The results of a preliminary survey. Journal of Psychiatric and Mental Health Nursing, 10, 3–15.
Porges, S. W. (2017). The pocket guide to the polyvagal theory: the transformative power of feeling safe. W.W. Norton & Co
Porges, S. W. (2020). Foreword: Feeling Safe is the Treatment. In J. Mitchell, J. Tucci, & E. Tronick (Eds.), The handbook of therapeutic care for children (pp. 11–17). Jessica Kingsley.
Roy, C., Castonguay, A., Fortin, M., Drolet, C., Franche-Choquette, G., Dumais, A., Lafortune, D., Bernard, P., & Geoffrion, S. (2019). The use of restraint and seclusion in residential treatment care for Youth: A systematic review of related factors and interventions. Trauma, Violence, & Abuse, 22(2), 318–338. https://doi.org/10.1177/1524838019843196
Savali, K. W. (2017, May 26). Ky. to close juvenile detention center where 16 year-old Gynna Mc Millen was found dead. The Root, 13. https://www.the root.com/ky-to-close-juvenile-detention-center-where-16-year-old-1795599201
Sethi, F., Parkes, J., Baskind, E., Paterson, B., & O’Brien, A. (2018). Restraint in mental health settings: Is it time to declare a position? British Journal of Psychiatry, 212, 137–141. https://doi.org/10.1192/bjp.2017.31
Smith, Y., Colletta, L., & Bender, A. E. (2017). Client violence against youth care workers: Findings of an exploratory study of workforce issues in residential treatment. Journal of Interpersonal Violence. https://doi.org/10.1177/0886260517743551
Steckley, L. (2010). Containment and holding environments: Understanding and reducing physical restraint in residential child care. Children and Youth Services Review, 32(1), 120–128. https://doi.org/10.1016/j.childyouth.2009.08.007
Steckley, L., & Kendrick, A. (2008). Young People’s experiences of physical restraint in residential care: Subtlety and complexity in policy and practice. In M. A. Nunno, D. M. Day, & L. B. Bullard (Eds.), For Our Own Safety: Examining the Safety of High-risk Interventions for Children and Young People (pp. 3–24). Child Welfare League of America.
Substance Abuse and Mental Health Services Administration (SAMHSA). (2010). Promoting Alternatives to the Use of Seclusion and Restraint—Issue brief #1: A National strategy to prevent seclusion and restraint in behavioral health services. rockville, MD: U.S. Department of Health and Human Services Retrieved from https://www.samhsa.gov/sites/default/files/topics/trauma_and_violence/seclusion-restraints-1.pdf
Toriello, P. J., Leierer, S. J., & Keferl, J. E. (2003). The impact of race on the use of physical restraint with adolescent males with behavioral disabilities: An initial study. Journal of Applied Rehabilitation Counseling, 34(4), 38–43.
United States Department of Justice. (2009). Investigation of the lansing residential center, Louis Gosset, Jr. Residential Center, Tryon Residential Center, and Tryon Girls Center (JI-NY-0009). U.S. Department of Justice. https://www.clearinghouse.net/detail.php?id=14180
United States Government Accountability Office. (2008). Residential programs: Selected cases of death, abuse, and deceptive marketing (GAO-08–713T).
United States Government Accountability Office. (2009). Seclusion and restraints: Selected cases of death and abuse at public and private schools and treatment centers: (GAO-09–719T). United States Government Accountability Office. http:// www.gao.gov/assets/130/122526.pdf.
United States Department of Health & Human Services, & Administration for Children and Families. (2018). Child maltreatment 2016. Author. https://www.acf.hhs.gov/cb/research-data-technology/statistics-research/child-maltreatment
United States Commission of Civil Rights. (2019). Beyond suspensions: Examining school discipline policies and connections to the school-to-prison pipeline for students of color with disabilities. Author. www.usccr.gov
Weiss, E. M., Altimari, D., Blint, D. F., & Megan, K. (1998 11&14, 1998). Deadly restraint: A hartford courant investigative report. Hartford Courant. http://www.courant.com/news/connecticut/hc-xpm-1998-10-11-9810090779-story.html#share=email~storyhttp://www.courant.com/news/connecticut/hc-xpm-2006-10-14-0610140661-story.html#share=email~story
Willis, R. (2019). The use of composite narratives to present interview findings. Qualitative Research, 19(4), 471–480. https://doi.org/10.1177/1468794118787711
Zegers, M., Schuengel, C., & Van IJzendoorn, M., & Janssens, J. . (2008). Attachment and problem behavior of adolescents during residential treatment. Attachment and Human Development, 10(1), 91–103.
Zehder, I. (2017). Memory-Of.com. Coalition against institutionalized child abuse (CAICA). http://children-in-treatment.memory-of.com
Zelechoski, A. D., Sharma, R., Beserra, K., Miguel, J. L., DeMarco, M., & Spinazzola, J. (2013). Traumatized youth in residential treatment settings: prevalence, clinical presentation, treatment, and policy implications. Journal of Family Violence, 28(7), 639–652. https://doi.org/10.1007/s10896-013-9534-9
Author information
Authors and Affiliations
Contributions
MAN conceptualized the study and the methodology; responsible data integrity and the accuracy of the analysis; wrote and edited the original and multiple drafts including the abstract, introduction; purpose; methodology; findings; discussion; limitations; practice recommendations; and conclusion. LAM wrote, reviewed, and edited multiple drafts from early inception to final article submission; designed, wrote, edited composite narratives for figures 1 & 2 to illustrate the confluence dynamics; assisted in data analysis and assessment and inclusion of narratives for illustration of concepts and dynamics. CVI reviewed, wrote, and edited multiple drafts; contributed concepts and wrote sections of the medical, psychological, and organizational components of the discussion section. EGS designed and developed the Excel program that tracked the fatalities and the data that was the basis for this study’s findings. Designed the tables that reported the findings. Assited in editing and writing. DES supervised the writing and editing of the article; provided demographic analysis for the tables, as well as, final editorial approval for publication submission. MJH initiated and supervised the entire publication process including funding, assistance in conceptualization, writing and editing.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nunno, M.A., McCabe, L.A., Izzo, C.V. et al. A 26-Year Study of Restraint Fatalities Among Children and Adolescents in the United States: A Failure of Organizational Structures and Processes. Child Youth Care Forum 51, 661–680 (2022). https://doi.org/10.1007/s10566-021-09646-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10566-021-09646-w