Abstract
It has been demonstrated that scar tissue and fibrosis may increase the likelihood of developing malignancies. Specifically, scar tissue has been linked to the occurrence and progression of lung cancer (LC), though the precise mechanisms necessitate further research for explanation. Lung scarring can stem from various causes, with carcinogenesis on scarring lesions in pulmonary tuberculosis (PTB) being the most frequent (accounting for approximately 75% of cases). Notably, having previously cured, PTB is the second most common risk factor for LC after smoking, with approximately 3% of PTB patients experiencing LC as a secondary condition. This essay will delve into the mechanisms, treatment, and prognosis of tuberculosis scar carcinoma (TSC).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Tuberculosis (TB) is a highly infectious disease caused by Mycobacterium tuberculosis (MTB) and primarily affects the lungs, resulting in high morbidity and mortality rates. According to the World Health Organization (WHO) statistics for 2020, the global proportion of people with TB is 56 per 100,000 population, with 10 million new cases and approximately 1.5 million deaths attributed to the disease each year [1]. Lung cancer (LC) is a significant health concern with low survival rates, and several factors like smoking, air pollution, diet, inflammation, and prior respiratory illnesses can trigger its development [2]. Research has indicated that TB may be a contributing risk factor in the development and progression of LC, with a coexistence rate of approximately 2% [3]. Due to the complex interactions between these diseases, the precise mechanisms underlying the relationship between TB and LC remain incompletely understood. Nevertheless, prevailing theories suggest the involvement of inflammatory stimulation, immune function, DNA damage, and scar calcification [4]. Given the diverse disease manifestations and complex interactions, research remains ongoing to fully understand the relationship between TB and LC. Additionally, the scarring of pulmonary tuberculosis (PTB) lesions is a crucial risk factor for LC development [5].
The concept of scar carcinoma (SC) was first introduced by Friedrich Scholar in 1939, defining it as a group of malignancies that arise from scars around the lungs [6]. Since then, numerous studies have been conducted to investigate the mechanisms by which lung scarring can trigger the development of LC. However, these studies have mainly consisted of single or small patient case reports, and more large-scale population-based epidemiological and data analyses are required. SC is a relatively rare condition that mostly affects males and typically involves the upper lobe of the lung. The histopathological type of this condition is usually adenocarcinoma [7].
2 Historical studies
The diagnostic criteria for scar included lesions that did not involve the main bronchi, continuous hyalinized scars on pathological examination, and initial scar tissue that did not contain cancer cells [6]. In 1972, Freant et al. conducted a retrospective study of 119 SC patients from 1961 to 1972 to investigate the relationship between scar tissue and cancer. A large number of histopathological examinations revealed the presence of elastic fibers and anthrax pigments in the lesion, while tumor masses could be found in some dense hyaline connective tissue or adjacent areas. In some cases, cancer tissues of varying degrees of differentiation were seen around scars, from epithelial hyperplasia to metaplasia to overt carcinoma [8]. Auerbach et al. conducted a comprehensive retrospective study, analyzing 1186 cases of LC patients from over 7000 autopsy cases between 1955 and 1975, revealing a total of 82 cases of SC. The outcomes showed that peripheral LCs accounted for 15% of SCs, and 45% of these cases were caused by scar tissue. Among the SC cases, 72% were adenocarcinomas, with 75% of cancers located in the upper lobe, and more than half of the cases were related to infarcts caused by scar tissue [9]. The study conducted by Luders and Themel investigated the etiology of pulmonary scars, in which they stated that pulmonary scars were mostly due to PTB, and TB scars played a crucial role in SC formation [10]. Another research work by Brett et al. reviewed 917 patients diagnosed with LC from 2013 to 2017 through imaging at a South African hospital, of which 268 had lung scars or diffuse fibrosis, suggesting a strong association between lung scar and primary LC [11].
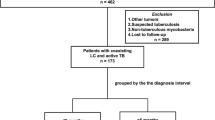
Based on the survey, it was observed that individuals with a history of PTB had twice the risk of developing LC as compared to the general population [12]. PTB patients often experience inflammation due to recurrent tissue damage and repair, with some underlying infections causing inflammation that results in the production of inflammatory factors, such as interleukin (IL) and tumor necrosis factor (TNF), during their long-term treatment. As a result of this inflammation, acute phase proteins are produced, leading to tissue fibrosis and ultimately formation of scar tissue [13]. Several large-scale studies have been conducted to investigate the relationship between TB and LC. A study conducted by Engles et al. on 42,422 farmers in Xuanwei, China, from 1976 to 1996 involved a series of standardized questionnaires and follow-up visits. It was found that the mortality rate of LC in patients with PTB was significantly greater than in those without PTB (25 vs. 3.1 per 1000 person-years) [14]. Zheng et al. have suggested that LC may develop as a consequence of PTB on the same side of the lung [15]. The PLCO trial followed 66,863 cancer-free individuals aged 55 to 74 years for 12 years, and those with lung scars on chest radiography had 1.8 times higher risk of developing LC than controls (HR = 1.8; CI 1.4–2.4) [16]. Additionally, Everatt et al. observed a 3.5-fold increase in LC incidence in 21,986 PTB patients from Lithuania compared to the non-PTB population, with 477 of the PTB patients developing LC during the final follow-up [17]. Su et al. conducted a retrospective analysis of 11,522 subjects with latent tuberculosis infection (LTBI) along with 46,088 matched subjects, revealing that PTB contacts had a 2.7 times higher risk of LC, indicating a higher incidence of LC in the LTBI group [18]. Furthermore, TB has also been associated with the occurrence of secondary LC. Ho et al. conducted a large national cohort study that followed 1,936,512 individuals with or without TB and observed a 1.67-fold increase in secondary LC risk in TB patients compared to the non-TB population of primary cancer [19]. Related studies are presented in Table 1.
3 Inflammatory mechanisms of lung cancer caused by tuberculosis scar
The process of fibrotic scarring in PTB results from repeated tissue damage and repair. This process is associated with mechanisms of long-term pulmonary inflammation that increase the risk of LC [20]. Initially, reactive oxygen species (ROS) produced at the lesion promote inflammation and stimulate the production of cytokines such as TNF, IL-1, and IL-6. These cytokines, in turn, stimulate the expression of cyclooxygenase (COX) -2, IL-2, C-reactive protein (CRP), and nuclear factor kappa B (NF-κB), thus further intensifying the inflammatory response. Inflammatory factors can also induce the synthesis of P-selectin and E-selectin, which in turn activate endothelial cells to produce vascular cell adhesion molecule (VCAM) and intercellular adhesion molecule (ICAM). These processes activate leukocytes and allow them to accumulate in the lesion, while free radicals produced by activated leukocytes can cause DNA damage in the lesion cell [21]. In the presence of inflammatory cytokines, nitric oxide (NO) is produced and can oxidize DNA and even damage some DNA repair proteins [22]. Inflammatory factors can also affect genome integrity by inhibiting cytochrome P-450 or glutathione S-transferase isoenzymes [22]. Therefore, ROS-induced inflammatory responses can promote DNA damage, thereby increasing the endogenous carcinogenic risk.
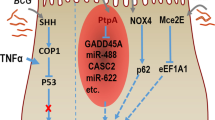
TNF, IL-1, and IL-6 can stimulate the production of angiogenic factors, such as vascular endothelial growth factor (VEGF), and transforming growth factor (TGF) -β1, produced by inflammatory macrophages [22]. TGF-β, TNF-α, and IL-related factors can induce lung remodeling, promote residual fibrosis of the lesion, and trigger the production of cancer-associated fibroblasts (CAF). As depicted in Fig. 1, CAF activation is linked with the activation of ROS, inflammatory cascade processes, and genetic damage. CAF and angiogenic factors are both dense and indispensable components of the tumor microenvironment [23]. TGF-β and IL-related factors, which are produced by inflammation-stimulated macrophages, can induce the production of heat shock protein (HSP47), promote collagen synthesis by lung fibroblasts, and eventually form scar tissue. During a chronic inflammatory response, persistent cascades lead to enlarged inflammation, causing persistent DNA damage, apoptosis, and residual fibrosis, which may eventually lead to gene mutations activating oncogenes and slowly evolving into cancer cells. An increase in fibrosis obstructs the flow of blood and lymphoid tissue through the scar tissue, further promoting the growth of cancer cells [24], as shown in Fig. 2. This mechanism can result in the inability of normal cells to adapt, leading to their death and their replacement by variant cells that can adapt to this abnormal growth environment, which are likely to be malignant cells.
The presence of inflammatory monocytes (IMs) is a known cause of scar tissue formation and can also be found in pathological tissue specimens. This is particularly true for squamous cell carcinoma, which is often characterized by a massive infiltration of IMs. Inhibition of the accumulation of IMs can be an effective drug target, potentially leading to inhibited tumor metastasis. It is worth noting that IMs express factor XIIIA at high levels, which in turn promotes fibrin cross-linking and creates scaffolds to aid in the invasion and metastasis of squamous cell carcinoma cells [25]. Chemokine ligand 2 (CCL-2) is responsible for the recruitment of IMs, and elevated levels of CCL-2 have also been found in patients with PTB [26]. Furthermore, IMs have the ability to differentiate into dendritic cells or tumor-associated macrophages (TAMs), both of which can play an important role in promoting tumor growth [27].
4 Treatment and prognosis of tuberculosis scar carcinoma
Early detection is the key to treating TSC. Clinical studies suggest that a comprehensive approach using multiple treatment methods, such as surgery, radiotherapy, anti-tumor drug chemotherapy, immunotherapy, targeted therapy, traditional Chinese medicine treatment, and intervention, should be selected based on the specific pathological type, TNM stage, lesion location, size, extent, and overall patient health to maximize efficacy. The ultimate goal is to alleviate patient pain, improve quality of life, and prolong overall survival (OS) [28].
4.1 Surgical treatment of tuberculosis scar carcinoma
In cases of severe fibrosis, radiotherapy is not recommended. Additionally, there are no systematic studies of chemotherapy regimens for SC. As a result, radical surgery is the preferred method for treating localized lesions with no serious complications. During surgery, it is important to thoroughly dissect intrapulmonary and mediastinal lymph nodes and perform radical surgery. However, due to its high malignancy, lymphatic or hematogenous metastasis and the prognosis are generally poor [28].
4.2 Chemotherapy for tuberculosis scar carcinoma
When it comes to treating SC, there are a variety of drug options available. In addition to traditional anti-tumor drugs, there have been large-scale studies exploring the effectiveness of drugs such as steroids, ulinastatin, sivelestat sodium, and macrolides in the treatment process, although they have not yet been clinically confirmed [29]. Hypoxia-inducible factor (HIF) plays a role in promoting LC metastasis and is associated with inflammation-related signaling pathways. As a result, HIF inhibitors are being widely studied as novel anticancer agents [30, 31]. Other drugs, such as pirfenidone, inhibit the expression of fibroblast growth factor (bFGF), TGF-β, CTGF, and TIMP-1, reducing the production of type I and type III collagen fibers. Pirfenidone also inhibits inflammatory mediators to varying degrees, exerting its anti-inflammatory effects [32, 33]. However, pirfenidone alone is not effective at inhibiting cancer cells. Combining it with cisplatin has been shown to achieve better efficacy because pirfenidone can enhance the efficacy of cisplatin by inhibiting the production of scars to change the tumor microenvironment and increase drug permeability [32]. Paclitaxel has also been demonstrated to be effective in inhibiting the growth of SC cells by inducing apoptosis and hindering the cell cycle [34]. Additionally, oral LY2109761, proposed by Wei et al., has been shown to reduce TGF-β1-induced collagen production, which inhibits scar fibrosis progression. This provides new ideas for the treatment of patients with early TSC. However, it is important to note that while these drugs show promise, further clinical testing may still be required [35].
4.3 Immunotherapy for tuberculosis scar carcinoma
Immunotherapy is a novel treatment modality that has been actively researched in recent years. Of particular interest are immune checkpoint inhibitors (ICI) that have shown promise for cancer therapy such as programmed cell death protein-1 (PD-1) and its ligand (PD-L1) inhibitors. Clinically, their use is based on the level of PD-L1 expression. For example, advanced non-small cell lung cancer (NSCLC) with PD-L1 expression greater than 50% can be treated with the PD-1 antibody, Keytruda (pembrolizumab), as a monotherapy with a response rate of approximately 40% [36]. According to a first-line monotherapy trial based on relevant research, the survival rate of NSCLC patients was compared between PD-(L)1 antibody therapy and platinum-based first-line chemotherapy. The final results showed that pembrolizumab significantly extended patients’ survival time, especially for those with higher PD-L1 expression [37]. PD-1 and cytotoxic T-lymphocyte–associated protein 4 (CTLA-4) are complementary co-inhibitory receptors; so, according to the latest relevant clinical trials, the combination of PD-1 and CTLA-4 inhibitors is expected to improve patient efficacy compared to monotherapy [38]. In addition to PD-(L)1 antibody therapy, different checkpoint inhibitor combinations, with or without chemotherapy, may also improve patients’ survival rates. Therefore, it is particularly important to select appropriate targets for individualized treatment according to patients’ conditions. The efficacy of immunotherapy for SC is influenced by several factors, such as cancer type, stage, and timing of diagnosis [39].
4.4 Prognosis of tuberculosis scar carcinoma
The prognosis of TSC is still debated, with some scholars suggesting that the prognosis seems favorable in the LC population (with a 5-year survival rate between 5/6 and 3/7) [40]. However, Freant et al. reported a 5-year survival rate of only 5% after SC surgery [8]. Studies have indicated that that the prognosis of pulmonary scar carcinoma (PSC) is primarily linked to the cancer cell type and lesion stage, and not necessarily to the scar itself. SC adenocarcinomas typically invade blood vessels and lymph nodes, leading to distant metastasis and a poor prognosis. Carroll proposed that scar tissue proliferation may hinder lymphatic and blood drainage, while carcinogens accumulate at the scar, promoting the spread of its blood vessels and lymph nodes [41]. Freant et al. also found that SC lymph nodes are often heavily involved, and the presence or absence of lymph node metastasis is an important prognostic indicator [8]. Early lymph node metastasis may be a unique feature of SC. Therefore, clinicians should remain vigilant for the possibility of SC, monitor lesions closely, and pay extra attention to patients with a history of pulmonary PTB to achieve early diagnosis and treatment. In conclusion, patients with PTB scars are at an increased risk of LC and require close monitoring and follow-up.
5 Conclusion
Studies in history have confirmed the relationship between TB and LC, but the mechanisms that govern the interaction between these two diseases are not yet fully understood. TB infection can cause chronic inflammation and plays an integral role in scarring. While most current research on TSC comes from published case reports or series, additional TSC samples and data studies are necessary to better comprehend their biological behavior and to develop potential new treatments. A potentially difficult issue with SC diagnosis is that histological examination is performed long after a precipitating event, which may lead to scar formation. Since determining the timing of the initial injury is challenging, evidence of scarring prior to SC has been a point of debate for decades. To better understand how scar problems lead to cancer development, it is essential to track the scar’s development over time and observe its eventual transition into cancer through imaging. The diagnosis and treatment of TSC remain a challenge in various clinical settings.
Data Availability
The data used in this study were obtained from publicly accessible academic databases such as PubMed and Web of Science. These data were obtained through legitimate channels and comply with the terms and conditions of these databases. In this paper, we have cited relevant data obtained from PubMed and Web of Science to support our research findings and perspectives. We have taken appropriate measures to ensure the accuracy and reliability of the data. It is important to emphasize that the use of these data is in accordance with the regulations of the respective databases and adheres to applicable laws and ethical guidelines. We commit to citing these data appropriately and providing correct citation information in the references. Please note that this study may also include third-party materials from other sources, such as figures, images, and quotations. We have made reasonable efforts to ensure that the use of these third-party materials complies with copyright laws and fair use principles. Unless otherwise stated, these materials are also subject to the data availability statement of this paper. If you have any questions or need further information regarding the availability of specific data, please contact the data providers such as PubMed and Web of Science directly.
References
(2020). World Health Organization 2020.
de Groot, P., & Munden, R. F. (2012). Lung cancer epidemiology, risk factors, and prevention. Radiologic Clinics of North America, 50(5), 863–876.
Ayman, R., Glen, H., Ahmad, A., et al. (2016). A case of tuberculosis and adenocarcinoma coexisting in the same lung lobe. International Journal of Mycobacteriology, 5, 80–82.
Xiong, K., Sun, W., He, Y., & Fan, L. (2021). Advances in molecular mechanisms of interaction between Mycobacterium tuberculosis and lung cancer: A narrative review. Translational Lung Cancer Research, 10(10), 4012–4026.
Cicenas, S., & Vencevicius, V. (2007). Lung cancer in patients with tuberculosis. World Journal of Surgical Oncology, 5, 22.
Friedrich, G. (1939). Peripheral lung cancers on the floor near pleural scars. Virchows Archiv für Pathologische Anatomie und Physiologie und für Klinische Medizin, 304(1), 230–247.
Brett S, Irusen EM, Koegelenberg CFN. (2020). Pulmonary scarring and its relation to primary lung cancer. African Journal of Thoracic and Critical Care Medicine 26(1), https://doi.org/10.7196/AJTCCM.2020.v26i1.050
Freant, L. J., Joseph, W. L., & Adkins, P. C. (1974). Scar carcinoma of the lung. Fact or fantasy? The Annals of Thoracic Surgery, 17(6), 531–7.
Auerbach, O., Garfinkel, L., & Parks, V. R. (1979). Scar cancer of the lung: Increase over a 21 year period. Cancer, 43(2), 636–642.
Luders, C. J., & Themel, K. G. (1954). Die Narbenkrebse der Lungen als Beitrag zur Pathogenese des peripheren Lungencarcinoms [Cicatricial cancers of the lungs as a contribution to the pathogenesis of the peripheral carcinoma of the lungs]. Virchows Archiv for Pathologische Anatomie und Physiologie und for Klinische Medizin, 325(5), 499–551.
Brett S, Irusen EM, Koegelenberg CFN. (2020). Pulmonary scarring and its relation to primary lung cancer. Afr J Thorac Crit Care Med., 26(1) https://doi.org/10.7196/AJTCCM.2020.v26i1.050.
Bodegom, P. C., Wagenaar, S. S., Corrin, B., Baak, J. P., Berkel, J., & Vanderschueren, R. G. (1989). Second primary lung cancer: Importance of long term follow up. Thorax, 44(10), 788–793.
Engels, E. A. (2008). Inflammation in the development of lung cancer: Epidemiological evidence. Expert Review of Anticancer Therapy, 8(4), 605–615.
Engels, E. A. S. M., Chapman, R. S., Pfeiffer, R. M., et al. (2009). Tuberculosis and subsequent risk of lung cancer in Xuanwei, China. International Journal of Cancer, 124, 1183–1187.
Zheng, W., Blot, W. J., Liao, M. L., et al. (1987). Lung cancer and prior tuberculosis infection in Shanghai. British Journal of Cancer, 56, 501–504.
Yu, Y. Y., Pinsky, P. F., Caporaso, N. E., Chatterjee, N., Baumgarten, M., Langenberg, P., Furuno, J. P., Lan, Q., & Engels, E. A. (2008). Lung cancer risk following detection of pulmonary scarring by chest radiography in the prostate, lung, colorectal, and ovarian cancer screening trial. Archives of Internal Medicine, 168(21), 2326–2332.
Everatt, R., Kuzmickiene, I., Davidaviciene, E., et al. (2016). Incidence of lung cancer among patients with tuberculosis: A nationwide cohort study in Lithuania. The International Journal of Tuberculosis and Lung Disease, 20, 757–763.
Su, V. Y., Yen, Y. F., Pan, S. W., et al. (2016). Latent tuberculosis infection and the risk of subsequent cancer. Medicine (Baltimore), 95, e2352.
Ho, L. J., Yang, H. Y., Chung, C. H., Chang, W. C., Yang, S. S., Sun, C. A., Chien, W. C., & Su, R. Y. (2021). Increased risk of secondary lung cancer in patients with tuberculosis: A nationwide, population-based cohort study. PLoS ONE, 16(5), e0250531.
Shiels, M. S., Albanes, D., Virtamo, J., et al. (2011). Increased risk of lung cancer in men with tuberculosis in the alpha-tocopherol, beta-carotene cancer prevention study. Cancer Epidemiology, Biomarkers & Prevention, 20, 672–678.
Manning, A. M., Bell, F. P., Rosenbloom, C. L., et al. (1995). NF-kappa B is activated during acute inflammation in vivo in association with elevated endothelial cell adhesion molecule gene expression and leukocyte recruitment. Journal of Inflammation, 45, 283–296.
Balkwill, F. M. A. (2001). Inflammation and cancer: back to Virchow? Lancet, 357, 539–545.
Dheda, K. B. H., Huggett, J. F., Johnson, M. A., et al. (2005). Lung remodeling in pulmonary tuberculosis. The Journal of Infectious Diseases, 192, 1201–1209.
Ardies, C. (2003). Inflammation as cause for scar cancers of the lung. Integrative Cancer Therapies, 2, 238–246.
Porrello, A., Leslie, P. L., Harrison, E. B., Gorentla, B. K., Kattula, S., Ghosh, S. K., et al. (2018). Factor XIIIA-expressing inflammatory monocytes promote lung squamous cancer through fibrin cross-linking. Nature Communications, 9, 1988.
Hasan, Z., Cliff, J. M., Dockrell, H. M., et al. (2009). CCL2 responses to Mycobacterium tuberculosis are associated with disease severity in tuberculosis. PLoS One, 4, e8459.
Porrello, A., Leslie, P. L., Harrison, E. B., et al. (2018). Factor XIIIA-expressing inflammatory monocytes promote lung squamous cancer through fibrin cross-linking. Nature Communications, 9, 1988.
Shetty, N., Noronha, V., Joshi, A., et al. (2014). Diagnostic and treatment dilemma of dual pathology of lung cancer and disseminated tuberculosis. Journal of Clinical Oncology, 32(6), e7-9.
Saito, Y., Kawai, Y., Takahashi, N., Ikeya, T., Murai, K., Kawabata, Y., et al. (2011). Survival after surgery for pathologic stage IA non-small cell lung cancer associated with idiopathic pulmonary fibrosis. The Annals of Thoracic Surgery, 92, 1812–1817.
Ren, W., Mi, D., Yang, K., Cao, N., Tian, J., Li, Z., et al. (2013). The expression of hypoxia-inducible factor-1alpha and its clinical significance in lung cancer: A systematic review and meta-analysis. Swiss Medical Weekly, 143, w13855.
Eltzschig, H. K., & Carmeliet, P. (2011). Hypoxia and inflammation. The New England Journal of Medicine, 364, 656–665.
Li, C., Rezov, V., Joensuu, E., Vartiainen, V., Ronty, M., Yin, M., et al. (2018). Pirfenidone decreases mesothelioma cell proliferation and migration via inhibition of ERK and AKT and regulates mesothelioma tumor microenvironment in vivo. Scientific Reports, 8, 10070.
Tanino, Y. (2018). Does pirfenidone have anticancer effects in patients with idiopathic pulmonary fibrosis? Respiratory Investigation, 56, 95–96.
Zhou, W., & Guo, Z. L. M. W. D. C. L. Z. L. (2019). Taxifolin inhibits the scar cell carcinoma growth by inducing apoptosis, cell cycle arrest and suppression of PI3K/AKT/mTOR pathway. Journal of B.U.ON., 24(2), 853–858.
Wei, G., Xu, Q., Liu, L., Zhang, H., Tan, X., Zhang, C., Han, C., Guo, Y., Han, G., & Zhang, C. (2018). LY2109761 reduces TGF-β1-induced collagen production and contraction in hypertrophic scar fibroblasts. Archives of Dermatological Research, 310(8), 615–623.
Jones, M. G., Andriotis, O. G., Roberts, J. J., Lunn, K., Tear, V. J., Cao, L., et al. (2018). Nanoscale dysregulation of collagen structure-function disrupts mechano-homeostasis and mediates pulmonary fibrosis. eLife, 7, e36354.
Reck, M., Remon, J., & Hellmann, M. D. (2022). First-line immunotherapy for non-small-cell lung cancer. Journal of Clinical Oncology, 40(6), 586–597.
Kato, K., Doki, Y., Ogata, T., Motoyama, S., Kawakami, H., Ueno, M., Kojima, T., Shirakawa, Y., Okada, M., Ishihara, R., Kubota, Y., Amaya-Chanaga, C., Chen, T., Matsumura, Y., & Kitagawa, Y. (2023). First-line nivolumab plus ipilimumab or chemotherapy versus chemotherapy alone in advanced esophageal squamous cell carcinoma: A Japanese subgroup analysis of open-label, phase 3 trial (CheckMate 648/ONO-4538–50). Esophagus, 20(2), 291–301.
Goto T.(2018). Measuring surgery outcomes of lung cancer patients with concomitant pulmonary fibrosis: A review of the literature. Cancers :10
Hukill, P. B., & Stern, H. (1962). Adenocarcinoma of the lung-histological factors affecting prognosis. A study of 38 patients with resection and 5-year follow-up. Cancer, 15, 504–514.
Carroll, R. (1962). The influence of lung scars on primary lung cancer. The Journal of Pathology and Bacteriology, 83, 293–7.
Funding
This work was supported by the Shanghai Municipal Science and Technology Major Project (2021SHZDZX0100) and the Fundamental Research Funds for the Central Universities, 2021 Science and Technology Think Tank Youth Talent Plan of China Association for Science and Technology, “Dream Tutor” Outstanding Young Talents Program (fkyq1901), and the National Key Research and Development Program of China (2021YFF1201200 and 2021YFF1200900). Figure was created using BioRender.com. The work was supported by the Shanghai Science and Technology Development Foundation, China (21Y11901000, 20ZR1446700); National Natural Science Foundation of China (82170006); and the Clinical Research Foundation of Shanghai Pulmonary Hospital (SKPY2021003).
Author information
Authors and Affiliations
Contributions
Wenwen Sun and Yujin Liu: conceptualization, writing—original draft. Lishu Zhao and Hao Wang: investigation, resources. Li Ye and Xinyue Liu: figure, visualisation. Kandi Xu: supervision. Yu Chen and Lin Fan: funding acquisition, resources, supervision, writing—review and editing.
Corresponding authors
Ethics declarations
Informed consent
This work comprehensively complies with the principles of informed consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Wenwen Sun and Yujin Liu are first authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sun, W., Liu, Y., Zhao, L. et al. New progress of tuberculosis scar carcinoma. Cancer Metastasis Rev 42, 653–659 (2023). https://doi.org/10.1007/s10555-023-10128-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-023-10128-9