Abstract
Background
Previous studies reported that tuberculosis (TB) is associated with an increased risk of lung cancer or the survival and mortality of lung cancer. However, the impact of coexisting TB on the survival of lung cancer patients was controversial. We aimed to identify risk factors on the survival rate of patients with co-existent active TB and lung cancer.
Methods
One hundred seventy-three patients diagnosed with active TB and lung cancer from January 2016 to August 2021 in Shanghai pulmonary hospital were selected and divided into two groups (≤ 6 months, > 6 months) according to the diagnosis interval between active TB and lung cancer (the order of diagnosis is not considered). The clinical characteristics and survival were analyzed. Univariate and multivariate logistic regression analyses were used to identify the risk factors for overall survival (OS).
Results
One hundred seventy-three patients were diagnosed with lung cancer and active TB. The study population exhibited a median age of 64 years, with a majority of 81.5% being male, 58.0% of patients had a history of smoking. Among those involved, 93.6% had pulmonary TB, 91.9% were diagnosed with non-small cell lung cancer (NSCLC), 76.9% were Eastern Cooperative Oncology Group (ECOG) 0–2 and 12.7% were ECOG 3–4. We observed better survival in the > 6 months group compared with the ≤ 6 months group (hazard ratio [HR] 0.456, 95% confidence interval [CI]:0.234–0.889, P = 0.017). The 1-, 3-, and 5- year OS rates were 94.2%, 80.3%, and 77.6%, respectively, in the > 6 months group and 88.3%, 63.8%, and 58.5%, respectively, in the ≤ 6 months group. Surgery (HR 0.193, [95% CI, 0.038–0.097]; P = 0.046) and ECOG Performance Status (HR 12.866, [95% CI, 2.730–60.638]; P = 0.001) were independent prognostic factors in the > 6 months group.
Conclusions
Patients diagnosed with lung cancer and active TB for more than half a year have a significantly better prognosis than those diagnosed within half a year. ECOG Performance Status and surgery might possibly affect the outcomes of patients with co-existent active TB and lung cancer.
Similar content being viewed by others
Introduction
Globally, TB ranks as the 13th most prevalent cause of mortality and the second most significant infectious agent, resulting in 10 million newly reported cases and a total of 1.5 million fatalities in the year 2020 [1]. China possesses one of the most significant TB burdens, ranking third and accounting for 8.4% of the total global cases [2]. Lung cancer is the second most commonly diagnosed cancer [3] and the leading cause of cancer death, representing approximately 1 in 10 (11.4%) cancers diagnosed and 1 in 5 (18.0%) deaths [4]. In China, it is expected that there will be approximately 870,982 people newly diagnosed with lung cancer, and 766,898 people dying from lung cancer in 2022 [5].
Epidemiological studies have revealed that TB is associated with an increased risk of lung cancer [6, 7], or the survival and mortality of lung cancer [8,9,10], especially adenocarcinoma [11]. Cabrera-Sanchez J et al. have demonstrated that patients diagnosed with TB are at an elevated risk of developing lung cancer [6, 12]. Conversely, patients with cancer exhibit a higher incidence of TB [13]. In a retrospective cohort analysis, the adjusted hazard ratio (aHR) for TB in lung cancer patients was 3.32 [14]. However, the impact of coexisting TB on the survival of lung cancer patients was controversial. TB was independently associated with subsequent mortality due to lung cancer (adjusted HR = 2.01, 95%CI [1.40–2.90], P < 0.001) [15] in a cross-matched cohort. A Korean retrospective study reported that lung cancer with TB was associated with lower mortality (HR = 0.35, 95% CI [0.21–0.60]) [8]. Zhi-Hong Jian et al. reported that coexisting pulmonary diseases are at an elevated risk of mortality among male patients with lung adenocarcinoma [11].
Previous studies have investigated numerous risk factors associated with the co-existence of TB and lung cancer, including smoking [16, 17], age [18], gender [19], inflammatory cytokines [20], C-reactive protein [21]. The objective of this study was to evaluate the impact of these factors on the survival rate of patients with co-existent TB and lung cancer according to the diagnosis interval.
Methods
The present study was performed in Shanghai pulmonary hospital, the standard authority for the diagnosis and treatment of TB and lung cancer in China. The study was approved by the ethics committee of Shanghai pulmonary hospital (Identifier: K18-145).
Study design and population
We conducted a single-center, retrospective analysis of patients with coexisting lung cancer and TB. Patients diagnosed with lung cancer and active TB were enrolled in Shanghai pulmonary hospital from January 2016 to August 2021. Clinical signs, demographic, biological and imaging data were retrieved from the patients’ electronic hospital records. Patient with other tumors or suspected TB or non-tuberculosis mycobacteria (NTM) were excluded from this study. Based on the diagnosis interval, patients were divided into two groups: ≤ 6 months, > 6 months (the order of diagnosis is not considered). Diagnosis of active TB was confirmed by bacteriologic, pathologic, radiographic, and clinical evidence. Baseline patient characteristics were collected, including age, genders, smoking status, stage, comorbidities, cancer type, tumor location, CT image, treatments, the laboratory findings and survival. Clinical staging was performed using the 7th edition of the TNM staging system, which was authorized by the American Joint Committee on Cancer [22].
Outcome
The primary outcome was death from any cause. Follow-up time was calculated from the date of lung cancer diagnosis till date of death or end of the follow-up period on March 31, 2022.
Statistical analysis
Analyses were conducted in SPSS (26.0, SPSS, Chicago, USA) and R (V.3.6.0; The R Project for Statistical Computing).
Baseline characteristics were described with frequencies and percentages for categorical variables and means and standard deviations (SDs) for continuous variables, whereas the median and interquartile range (IQR: 25th–75th) were used for non-normally distributed data. Analysis of the differences between the diagnosis interval ≤ or > 6 months group was performed using the Student’s t-test for continuous variables and the χ2 test or Fisher’s exact test for categorical variables. Kaplan–Meier (KM) analysis and the log rank test were applied to compare OS between two groups. A Cox proportional hazards model was used to test for significant factors on survival when the variables were significantly different at P ≤ 0.05 in the log-rank test with a univariate or multivariate analysis in each group.
Result
Patient characteristics
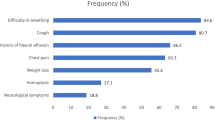
One hundred seventy-three patients diagnosed with lung cancer and active TB from Jan 2016 to August 2021 were divided into two groups based on the diagnosis interval, ≤ 6 months (n = 99), > 6 months (n = 74) (Fig. 1). Population characteristics are outlined in Table 1. The study population exhibited a median age of 64 years, with a majority of 81.5% being male, 58.0% of patients had a history of smoking. Among those involved, 93.6% had pulmonary TB, 91.9% were diagnosed with non-small cell lung cancer (NSCLC), 76.9% were ECOG 0–2 and 12.7% were ECOG 3–4. Patients with early and late stage tumors accounted for the majority (stage I 28.9%; stage IV 33.5%). Patients in the two groups had comparable characteristics, including age, sex, smoking status, stage, comorbidities, tumor location, CT image. The laboratory findings, including C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), inflammatory cytokines, CD4/CD8 T cell ratio were nearly similar in both groups. The two groups of anti-TB treatment accounted for a similar proportion. However, squamous cell carcinoma was found more often in the ≤ 6 months group. Compared with ≤ 6 months group, more patients in the > 6 months group were treated with surgery and chemotherapy. ECOG 0–2, ECOG 3–4 were 49.6%, 15.2%, respectively, in the ≤ 6 months group and 90.5%, 9.5%, respectively, in the > 6 months group (P = 0.000). The mean follow-up period was 14 months (range, 11–19 months) in the ≤ 6 months group and 29 months (range, 8.5–62 months) in the > 6 months group (P = 0.000).
Survival
Patients in the > 6 months group consistently were found to achieve better survival than that in the ≤ 6 months group (HR = 0.456, 95% CI [ 0.234–0.889], P = 0.017). The 1-, 3-, and 5- year OS rates were 94.2%, 80.3%, and 77.6%, respectively, in the > 6 months group and 88.3%, 63.8%, and 58.5%, respectively, in the ≤ 6 months group (Fig. 2). Separate analyses in subsets of patients according to gender, age, tumor location, stage, and type, smoking, treatments, the laboratory findings revealed the same pattern, with few exceptions. We found that patients older than 65 years old (HR 0.253, [95% CI, 0.096–0.669]; P = 0.006), male (HR 0.445, [95% CI, 0.209–0.948]; P = 0.036), stage IV (HR 0.279, [95% CI, 0.102–0.764]; P = 0.013), history of smoking (HR 0.315, [95% CI, 0.136–0.726]; P = 0.007), and those with the level of CRP range from 10 mg/L to 50 mg/L (HR 0.090, [95% CI, 0.010–0.794]; P = 0.03) were all significantly more likely to have worse cumulative OS rate, in the ≤ 6 months group compared with the > 6 months group (Fig. 3).
Univariate and multivariate analysis
Significant predictors were further assessed with a multivariable Cox proportional hazards model after evaluation by the univariate analysis when P < 0.05 in both groups. In the ≤ 6 months group, all the variables, age (HR 0.294, [95% CI, 0.114–0.760]; P = 0.011), left lung cancer (HR 0.271, [95% CI, 0.075–0.973]; P = 0.045), smoking (HR 3.519, [95% CI, 1.267–9.774]; P = 0.016), surgery (HR 0.077, [95% CI, 0.010–0.577]; P = 0.013), ECOG Performance Status (HR 16.329, [95% CI, 6.598–40.415]; P < 0.001), CRP 10–50 mg/L (HR 10.397, [95% CI, 1.288–83.951]; P = 0.028), IL-2R (HR 9.376, [95% CI, 1.122–78.323]; P = 0.028) were significant risk factors affecting OS in the univariate analysis. After multivariate Cox proportional hazards regression analyses, no variable was identified as an independent prognostic factor (Table 2).
In the > 6 months group, stage III (HR 15.192, [95% CI, 1.675–137.826]; P = 0.016), stage IV (HR 12.715, [95% CI, 1.556–103.866]; P = 0.018), surgery (HR 0.079, [95% CI, 0.021–0.296]; P = 0.000), ECOG Performance Status (HR 39.118, [95% CI, 9.852–155.313]; P < 0.001), CRP > 50 mg/L (HR 11.485, [95% CI, 1.165–113.215]; P = 0.037) were significant predictors in the univariate analysis. Multivariate Cox proportional hazards regression analyses showed that surgery (HR 0.193, [95% CI, 0.038–0.097]; P = 0.046), ECOG Performance Status (HR 12.866, [95% CI, 2.730–60.638]; P = 0.001) were independent prognostic factors (Table 3).
Discussion
In this retrospective study, patients in the > 6 months group were consistently found to have a better prognosis than patients in the ≤ 6 months group. This survival advantage was independent of differences in baseline characteristics such as gender, age, stage, and type, smoking, treatments, and the laboratory findings.
Sex-related differences exist in many lung diseases [23] including TB and lung cancer. Previous studies revealed females with active pulmonary TB had a higher risk of dying from lung cancer than males [16, 19]. In China, the mortality ratio was 1.72 for males and 2.79 for females [24]. However, a study from Taiwan, which showed that coexisting pulmonary disease may exert direct effects and increase risk of mortality in men, but not in women [11]. In our study, overall female had a better prognosis than men in overall. Meanwhile, we found that the diagnosis interval can affect prognosis in men, but not in women.
Several studies have investigated the incidence of lung cancer and TB, with a trend towards younger people at the age of high incidence. A South Korean cohort study has revealed that the risks for lung cancer were HR 9.85, 7.1, 3.32, and 2.57 in patients with TB aged 50–59, 60–69, and ≥ 70 years, respectively, compared to patients < 50 years of age [18]. An et al. have found that the mean age of patients with co-existence of TB and lung cancer was 69 years and the risk of lung cancer subsequent to pulmonary TB was significantly higher both for patients younger than 60 years and for those older than 60 years [25], which is consisted with our findings. We found that the diagnosis interval had a greater impact on the prognosis in the elderly, especially those whose diagnosis interval were less than half a year.
Smoking is the most important environmental risk factor for both lung cancer and TB [26]. However, the association between smoking and the development of lung cancer and TB remains uncertain [19, 27]. Liang et al. and Hwang et al. [27] suggested that smoking was not only an influential factor in the development increased risk of of lung cancer in patients with preexisting TB [28]. In a retrospective cohort study conducted in Xuanwei [29], the mortality was similar among men after adjustment for smoking status (HRs 9.7 and 4.3 in the 0–4.9 years and 5 + years after tuberculosis, respectively) and among women after adjustment for smoky coal use (HRs 7.5 and 2.5, respectively). Among ever-users of smoky coal (N = 2430 lung cancer deaths), TB was associated with higher risk of mortality from lung cancer, specifically within the first 0–4.9 years after TB diagnosis (HR 7.5, 95% CI 4.9–11). Additionally in the 5 + years following TB diagnosis, the HR was 2.5 with a 95% CI of 1.2–5.0. In our study, smoking increased the mortality in two groups and the > 6 months group had a better prognosis than the ≤ 6 months group in ever-smokers.
Mycobacterium TB can induce the release of inflammatory mediators, e.g., tumor necrosis factor (TNF)-α and interleukin (IL)-1, IL-2, and IL-12, which can be viewed as cancer promotors [30]. Several studies identified that high CRP levels were risk factors for the development of lung cancer and elevated serum CRP levels will increase the incidence of lung cancer in male TB patients [21]. We found that the number of patients with normal CRP and IL-2 levels were comparable to that of abnormal patients, and that mortality was higher in the < 6 months group among patients with CRP levels of 10 to 50 mg/L.
Lee et al. [8] and Kim et al. [31] reported that much higher proportions of lung cancer coexisting with pulmonary TB were at an advanced stage (T3-4), which was generally consistent with our findings, but we also found that the proportion of phase I and phase IV was comparable and the diagnosis interval can affect the prognosis of advanced patients. TB was found to be significantly associated with adenocarcinoma, but not with squamous or small-cell lung cancer (SCLC) [19]. In our study, adenocarcinoma accounted for the majority, especially in the > 6 months group, however, the type of pathology had no effect on patient prognosis in both groups.
The treatment of patients with lung cancer and TB is still not conclusive. Previous studies reported that lung cancer patients with co-existent granulomatous inflammation who had undergone surgical resection suggest a relatively good clinical outcome even without anti-TB treatment [32]. As for chemotherapy, there was no significant difference in treatment regimen, response rate, median survival time [33] in lung cancer and lung cancer patients with co-existent TB. We found surgery was a positive prognostic indicator in both groups, and an independent factor in the > 6 months group, while chemotherapy had no effect. Short-term tuberculosis lesions and lung cancer lesions are difficult to distinguish, which may result in delayed staging of lung cancer and the inability to perform timely surgery, leading to poor survival and prognosis for patients [34]. Therefore, when diagnosing lung cancer in the presence of active TB, it is imperative to conduct a more precise evaluation of lung cancer staging. This can be achieved through various methods such as Positron Emission Tomography-Computed Tomography, lung puncture, bronchoscopy, etc., rather than solely relying on Chest Computed Tomography..
Few studies analyzed the relationship between ECOG and the prognosis of patients with coexisting lung cancer and active TB. Only a recent study found that lung cancer, presence of metastasis and ECOG ≥ 3 were associated with death from TB [35], which is consisted with our results. In our study, ECOG 0–2 accounted for the majority, especially in the > 6 months group. Meanwhile, we found ECOG 3–4 was an independent risk factor in the > 6 months group. Simultaneous administration of anti-tumor and anti-tuberculosis treatment within a short period of time may exacerbate the patient’s ECOG performance status, preventing them from proceeding to the next step of treatment and resulting in poorer survival and prognosis. Therefore, it is advisable to select treatments with minimal impact on the patient's ECOG score.
Our study have a number of strengths. This study is one of the few retrospective studies that analyses the relationship between the diagnosis interval and the prognosis of patients with coexisting lung cancer and active TB [8, 34]. Previous studies have focused on the effects of pulmonary TB on the development and treatment of lung cancer [6, 20, 33, 34]. Secondly, we assessed various risk factors as possible, along with other potential factors, for better control to measure confounding and report unbiased results. Lastly, this study enrolled a relatively large number of patients with coexisting lung cancer and active TB.
Our study includes several limitations that may influence its generalizability. Firstly, it was performed retrospectively at a single center, and therefore the results may not reflect the general population in China. Secondly, we did not further group the order of diagnosis of lung cancer and pulmonary TB, which can analyze the interaction between TB and lung cancer. The possibility of sampling bias in the diagnosis of active TB could not be excluded. Patients with lung cancer usually received more medical attention. In addition, our study follow-up period was relatively shorter.
Conclusion
Patients diagnosed with lung cancer and active TB for more than half a year have a significantly better prognosis than those diagnosed within half a year. ECOG Performance Status and surgery might possibly affect outcomes of patients with co-existent active TB and lung cancer.
Availability of data and materials
All data generated or analyzed during this study are included in this published article. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- TB:
-
Tuberculosis
- NTM:
-
Non-tuberculosis mycobacteria
- OS:
-
Overall survival
- DM:
-
Diabetes mellitus
- HTN:
-
Hypertension
- COPD:
-
Chronic obstructive pulmonary disease
- CHD:
-
Coronary heart disease
- ECOG:
-
Eastern Cooperative Oncology Group
- SCLC:
-
Small-cell lung cancer
- NSCLC:
-
Non-small cell lung cancer
- CRP:
-
C-reactive protein
- IL:
-
Interleukin
- TNF:
-
Tumor necrosis factor
- IGRA:
-
Interferon gamma release assay
- SAA:
-
Serum amyloid a
- IQR:
-
Inter-quartile range
- SD:
-
Standard deviation
- ESR:
-
Erythrocyte sedimentation rate
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
References
World Health O. Global tuberculosis report 2021. Geneva: World Health Organization; 2021.
Zhu S, Wu Y, Wang Q, Gao L, Chen L, Zeng F, Yang P, Gao Y, Yang J. Long-term exposure to ambient air pollution and greenness in relation to pulmonary tuberculosis in China: a nationwide modelling study. Environ Res. 2022;214(Pt 3):114100.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49.
Xia C, Dong X, Li H, Cao M, Sun D, He S, Yang F, Yan X, Zhang S, Li N, et al. Cancer statistics in China and United States, 2022: profiles, trends, and determinants. Chin Med J (Engl). 2022;135(5):584–90.
Cabrera-Sanchez J, Cuba V, Vega V, Van der Stuyft P, Otero L. Lung cancer occurrence after an episode of tuberculosis: a systematic review and meta-analysis. Eur Respir Rev. 2022;31(165):220025.
Zheng L, Yin J, Wang S, Jiang H, Hu P, Kang Z, Lv P, Li W, Cai C. Associated factors of co-existent pulmonary tuberculosis and lung cancer: a case-control study. Eur J Clin Invest. 2021;51(4):e13432.
Lee HY, Kang HS, Kang JY, Kim JW, Lee SH, Kim SJ, Yeo CD. Clinical characteristics and survival of patients concurrently diagnosed with lung cancer and active pulmonary tuberculosis. Transl Cancer Res. 2022;11(8):2671–80.
Bhowmik S, Mohanto NC, Sarker D, Sorove AA. Incidence and risk of lung cancer in tuberculosis patients, and vice versa: a literature review of the last decade. Biomed Res Int. 2022;2022:1702819.
Huang JY, Jian ZH, Ndi Nfor O, Jhang KM, Ku WY, Ko PC, Jan SR, Ho CC, Lung CC, Pan HH, et al. The impact of coexisting asthma, chronic obstructive pulmonary disease and tuberculosis on survival in patients with lung squamous cell carcinoma. PLoS One. 2015;10(7):e0133367.
Jian ZH, Huang JY, Ko PC, Jan SR, Nfor ON, Lung CC, Ku WY, Ho CC, Pan HH, Liaw YP. Impact of coexisting pulmonary diseases on survival of patients with lung adenocarcinoma: a STROBE-compliant article. Medicine (Baltimore). 2015;94(4):e443.
Oh CM, Roh YH, Lim D, Kong HJ, Cho H, Hwangbo B, Won YJ, Jung KW, Oh K. Pulmonary tuberculosis is associated with elevated risk of lung cancer in Korea: the nationwide cohort study. J Cancer. 2020;11(7):1899–906.
Kumar DS, Ronald LA, Romanowski K, Rose C, Shulha HP, Cook VJ, Johnston JC. Risk of active tuberculosis in migrants diagnosed with cancer: a retrospective cohort study in British Columbia, Canada. BMJ Open. 2021;11(3):e037827.
Wu CY, Hu HY, Pu CY, Huang N, Shen HC, Li CP, Chou YJ. Aerodigestive tract, lung and haematological cancers are risk factors for tuberculosis: an 8-year population-based study. Int J Tuberc Lung Dis. 2011;15(1):125–30.
Leung CC, Hui L, Lee RS, Lam TH, Yew WW, Hui DS, Chan RC, Mok TY, Law WS, Chang KC, et al. Tuberculosis is associated with increased lung cancer mortality. Int J Tuberc Lung Dis. 2013;17(5):687–92.
Hong S, Mok Y, Jeon C, Jee SH, Samet JM. Tuberculosis, smoking and risk for lung cancer incidence and mortality. Int J Cancer. 2016;139(11):2447–55.
Furlow B. Tobacco control, lung cancer, and tuberculosis in Singapore. Lancet Respir Med. 2018;6(10):741–2.
An SJ, Kim YJ, Han SS, Heo J. Effects of age on the association between pulmonary tuberculosis and lung cancer in a South Korean cohort. J Thorac Dis. 2020;12(3):375–82.
Qin Y, Chen Y, Chen J, Xu K, Xu F, Shi J. The relationship between previous pulmonary tuberculosis and risk of lung cancer in the future. Infect Agent Cancer. 2022;17(1):20.
Zhang M, Zhou YY, Zhang YL. High Expression of TLR2 in the serum of patients with tuberculosis and lung cancer, and can promote the progression of lung cancer. Math Biosci Eng. 2019;17(3):1959–72.
Jiang Y, Ni K, Fang M, Li J. The effects of serum hs-CRP on the Incidence of lung cancer in male patients with pulmonary tuberculosis. Iran J Public Health. 2019;48(7):1265–9.
Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471–4.
Silveyra P, Fuentes N, Rodriguez Bauza DE. Sex and gender differences in lung disease. Adv Exp Med Biol. 2021;1304:227–58.
Gao YT, Zheng W, Gao RN, Jin F. Tobacco smoking and its effect on health in China. IARC Sci Publ. 1991;105:62–7.
Wu C-Y, Hu H-Y, Pu C-Y, Huang N, Shen H-C, Li C-P, Chou Y-J. Pulmonary tuberculosis increases the risk of lung cancer. Cancer. 2011;117(3):618–24.
Alavi-Naini R, Sharifi-Mood B, Metanat M. Association between tuberculosis and smoking. Int J High Risk Behav Addict. 2012;1(2):71–4.
Hwang SY, Kim JY, Lee HS, Lee S, Kim D, Kim S, Hyun JH, Shin JI, Lee KH, Han SH, et al. Pulmonary tuberculosis and risk of lung cancer: a systematic review and meta-analysis. J Clin Med. 2022;11(3):765.
Liang HY, Li XL, Yu XS, Guan P, Yin ZH, He QC, Zhou BS. Facts and fiction of the relationship between preexisting tuberculosis and lung cancer risk: a systematic review. Int J Cancer. 2009;125(12):2936–44.
Engels EA, Shen M, Chapman RS, Pfeiffer RM, Yu YY, He X, Lan Q. Tuberculosis and subsequent risk of lung cancer in Xuanwei. China Int J Cancer. 2009;124(5):1183–7.
Fol M, Koziński P, Kulesza J, Białecki P, Druszczyńska M. Dual Nature of Relationship between Mycobacteria and Cancer. Int J Mol Sci. 2021;22(15):8332.
Kim YI, Goo JM, Kim HY, Song JW, Im JG. Coexisting bronchogenic carcinoma and pulmonary tuberculosis in the same lobe: radiologic findings and clinical significance. Korean J Radiol. 2001;2(3):138–44.
Ho JC, Leung CC. Management of co-existent tuberculosis and lung cancer. Lung Cancer. 2018;122:83–7.
Chai M, Shi Q. The effect of anti-cancer and anti-tuberculosis treatments in lung cancer patients with active tuberculosis: a retrospective analysis. BMC Cancer. 2020;20(1):1121.
Uchida Y, Soejima K. Clinical characteristics of patients simultaneously diagnosed with lung cancer and active pulmonary tuberculosis in countries where tuberculosis is moderately endemic. Transl Cancer Res. 2022;11(8):2480–2.
Lira CAG, Peixoto Bittencourt D, Bicalho CDS, Bonazzi Rodrigues P, Freire MP, Abdala E, Pierrotti LC. Clinical profile and mortality predictors for tuberculosis disease among patients with solid tumours. Infect Dis (Lond). 2022;54(11):804–9.
Acknowledgements
We would like to thank all the patients who donate their biological samples.
Funding
This study was supported by Shanghai science and technology commission project (20Y11901500).
Author information
Authors and Affiliations
Contributions
Conception and design: J.N., T.M.X. Acquisition, statistical analysis or interpretation of the data: all authors. Drafting of the manuscript: S.S.X. and Y.H.C. All authors reviewed and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of Shanghai Pulmonary.
Hospital, Tongji University School of Medicine (No. K18-145). Informed consent were waived by the ethics committee of Shanghai Pulmonary Hospital based on the retrospective nature. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xiong, M., Xie, S., Wang, Y. et al. The diagnosis interval influences risk factors of mortality in patients with co-existent active tuberculosis and lung cancer: a retrospective study. BMC Pulm Med 23, 382 (2023). https://doi.org/10.1186/s12890-023-02674-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-023-02674-3