Abstract
Pseudomyxoma peritonei (PMP) is a rare, progressive, slowly growing neoplastic condition which is poorly understood, with a 5-year progression-free survival rate as low as 48%. PMP is most commonly caused by appendiceal mucinous neoplasms (AMN), and understanding their genetic biology and pathogenicity may allow for the development of better novel systemic treatments to target key deleterious mutations and the implicated pathways. The primary aim of this systematic review was to identify the genetic profile of histologically confirmed human PMP or AMN samples. The secondary aim was to identify whether genetic marks could be used to predict patient survival. Ovid EMBASE, Ovid MEDLINE, PubMed, and Web of Science were searched to identify studies investigating the genetic profile of histologically-confirmed human PMP or AMN samples. We review findings of 46 studies totalling 2181 tumour samples. The most frequently identified somatic gene mutations in patients with PMP included KRAS (38–100%), GNAS (17–100%), and TP53 (5–23%); however, there were conflicting results of their effect on survival. Three studies identified molecular subtypes based on gene expression profiles classifying patients into oncogene-enriched, immune-enriched, and mixed molecular subtypes with prognostic value. This review summarises the current literature surrounding genetic aberrations in PMP and AMNs and their potential utility for targeted therapy. Given the recent advances in clinical trials to directly target KRAS and GNAS mutations in other cancers, we propose a rationale to explore these mutations in future pre-clinical studies in PMP with a view for a future clinical trial.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
1.1 The prevalence and development of pseudomyxoma peritonei
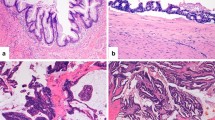
Pseudomyxoma peritonei (PMP) is a rare malignant clinical syndrome with an estimated incidence of 1–2 per 1,000,000 [1]. Appendiceal mucinous neoplasms (AMN) are a common type of appendiceal tumour where the tumour cells and extracellular mucin may accumulate causing the appendix to rupture. This results in the dissemination and metastasis of the AMN and mucin into the peritoneal cavity and specific anatomical sites (including the greater omentum, under-surface of the right hemidiaphragm, right subhepatic space, and paracolic gutters) [2, 3] following the redistribution phenomenon, which leads to the development of PMP (Fig. 1) [4]. The redistribution phenomenon is a character-defining feature of PMP and occurs when extracellular mucin follows the normal flow of peritoneal fluid, redistributing the neoplastic cells [3, 5] (Fig. 1). PMP is most commonly caused by mucinous neoplasms of appendiceal origin; however, there are reported cases of ovarian, colonic, and pancreatic origin in the literature [2, 6,7,8]. PMP may be caused by both low-grade mucinous appendiceal neoplasms (LAMN) and high-grade mucinous appendiceal neoplasms (HAMN) [3]. Figure 1 depicts the physiological transformations that occur in PMP.
The physiological sequelae of PMP. AMN and extracellular mucin accumulate in the appendix causing it to rupture. These neoplasms will metastasise throughout (and are confined to) the abdominopelvic cavity following the redistribution phenomenon. Consequently, the patient will develop mucinous ascites, peritoneal implants, and abdominal pain; and there may be metastasis to the ovaries in female patients. (Created with BioRender.com, accessed on 4 September 2022)
1.2 Nomenclature of PMP and appendiceal mucinous neoplasms
Previous literature has noted various classification systems used to grade PMP and AMN, which has proven to be confusing [7, 9, 10]. To address these discrepancies, Carr et al. [3] and the Peritoneal Surface Oncology Group International (PSOGI) reached a consensus on the terminology (refer to Supplementary Table 1 for detailed classifications), and PMP is now classified according to the peritoneal histology instead of the primary tumour [2].
1.3 Current treatment options for PMP
Cytoreductive surgery (CRS), where the tumour and extracellular mucin are removed, combined with hyperthermic intraperitoneal chemotherapy (HIPEC) with mitomycin-C and cisplatin is the gold standard treatment for patients with PMP [11,12,13,14,15,16,17,18]. CRS-HIPEC is currently the only treatment available with potential chances of long-term disease control and cure for these patients, as supported by a recent retrospective analysis of nearly 2000 patients [19]. Although some studies have noted a 5-year overall survival (OS) of more than 50% [14, 19, 20], another study concluded that patients have a much lower progression-free survival (PFS) rate of 48% with 31% of the sample had disease progression despite this treatment [21]. PMP patients with good prognostic factors, including low-grade histology, low peritoneal load, and no residual macroscopic disease have high chances of being cured by CRS-HIPEC [17]. Contrarily, for PMP patients with poor prognostic factors such as high grade or signet ring histology and unresectable or recurrent disease, the therapeutic options are limited, and the currently available systemic treatment options are inefficient to change the natural progression of the disease [17]. There is an unmet need for better and rational treatment options with reduced adverse side effects for these patients.
Genomics have been used to successfully guide treatment in other cancers. They are useful in understanding disease progression and identifying actionable targets for novel treatments as accomplished in colorectal [22, 23], lung [24], and breast cancers [25]. Although the genetic profile of PMP and AMN has been previously studied, currently they have not identified unique genetic targets to allow for treatments with reduced adverse side effects. This review aims to identify genetic alterations in PMP of appendiceal origin and look at survival outcomes. Collating evidence on the genetic aberrations present in PMP and AMN to date will not only identify recurrent and well-known driver genes, as well as rare gene events, but also help characterise the molecular mechanisms that define this disease [26]. Consequently, such a comprehensive characterisation can be utilised to identify established mutations with a druggable target and guide areas for future research focussing on translational drug discovery that target these genetic aberrations and mechanisms. The hope would be that this will ultimately lead to improved treatments with less adverse side effects, that are linked to the genetic profiles of PMP aiding clinicians during their decisions on treatment plans. Here, we review evidence of 46 studies that investigated genetic aberrations in PMP and AMNs samples, and we provide a comprehensive compendium of what is currently known about the genetic profile and molecular subtypes of PMP and AMN.
2 Methods
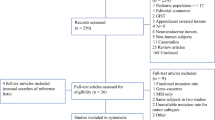
A systematic literature search (registered on PROSPERO under the registration number CRD42021228193) was performed on four electronic databases; Ovid EMBASE, Ovid MEDLINE, PubMed, and Web of Science, to identify genetic aberrations in PMP and AMN (Table 1, Fig. 2). The search was limited to studies written in English language published between 1995 and 2021. Titles, abstracts, and full texts were screened by two independent researchers (NWM and NMA) and any disagreements resolved by a third researcher (SPB). Studies were included according to the following criteria: original research; human adults diagnosed with PMP or AMN; and studies of oncogenic marks. Studies were excluded using the following criteria: PMP of other origin other than AMN; participants under 18 years old; data from animal or cell models; and any other study not related to PMP or AMN. The reference list of a systematic review which identified somatic alterations in AMN by Stein et al. 2020 [27] was searched; however, no additional studies matching the inclusion criteria were identified. The search strategy has been outlined in Table 1 and the screening process is shown in an adapted version of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart in Fig. 2 [28].
The following data items were extracted: sample size and classification of tumours; age; gender; tissue processing; experimental method used; genetic markers of human resected tissue of patients diagnosed with PMP or mucinous appendiceal neoplasms; implicated gene pathways; and survival analyses. To provide an accurate assessment of the quality of the included studies the risk of bias in non-randomised studies of interventions (ROBINS-I) tool was used which included four main domains: confounding bias, selection bias, information bias, and reporting bias (Supplementary Table 2) [29]. Studies were scored as low, moderate, or high, risk of bias.
3 Results
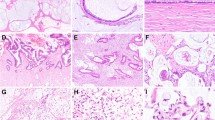
This review included 46 studies, a total of 2181 tumour samples (sample size range across studies 1–374) of various histological subtypes of PMP and AMN: LAMN, HAMN, mucinous adenocarcinomas (MAC), mucinous cystadenocarcinomas, mucinous cystadenomas, and PMP due to low-grade neoplasms (low-grade mucinous carcinoma peritonei LGMCP) and high-grade neoplasms (high-grade mucinous carcinoma peritonei HGMCP) (Table 2). The mean and median age ranged from 50.9 to 68.0 and from 51 to 61, respectively. However, there was a wide age range of 20 to 94 across all 46 studies. Both males and females were affected; however most studies (n=26) had a range of 51–100% of females in their samples.
3.1 Prevalence of mutations
The most frequently identified somatic gene mutations were in KRAS and GNAS with 70% of studies (n=32) identifying KRAS gene mutations (a proto-oncogene) and 57% of studies (n=26) identifying GNAS gene mutations (a complex locus) (Table 2). Across the reviewed studies, the most common variants noted in KRAS mutations were found on codon 12 (G12D, G12C, and G12V) and in codon 13 (G13D) in PMP and AMN [30, 44, 74]. The most commonly identified GNAS mutation variants were R201H and R201C [30]. Additional oncogenes were identified: 24% of studies (n=11) identified PIK3CA mutations, 11% (n=5) identified CTNNB1 mutations, and 13% (n=6) identified AKT1 mutations. The following tumour suppressor genes were identified: 37% of studies (n=17) identified TP53 mutations, 30% (n=14) identified SMAD4 mutations, 24% (n=11) identified APC mutations, 9% (n=4) identified ATM mutations, 9% identified RNF43 mutations, and 7% (n=3) identified RB1 mutations. A summary of all genetic alterations identified are recorded in the Supplementary Table 2.
All papers stated the experimental method used to analyse their samples (Table 2), and the two most frequently used methods were next-generation sequencing (NGS) and polymerase chain reaction (PCR) across studies. A third of studies (n=15) used NGS as their main experimental method [32,33,34,35, 38, 41, 42, 44, 46, 48, 50,51,52, 57, 59]. A third of studies (n=15) used PCR: 13 studies used it as their main experimental method [4, 26, 47 57] and 2 studies used it to validate their findings [49, 54]. Some studies (13%; n=6) used Sanger sequencing [34, 36, 44, 50, 63, 64] and 7% of studies (n=3) used whole-exome sequencing [4, 40, 45]. All methods have been recorded in Table 2.
A third of studies (n=14) noted co-existing KRAS and GNAS mutations in their samples with co-occurrence rates ranging from 13 to 100% [4, 30, 32, 34, 35, 38, 42, 44,45,46, 48, 51, 52, 59] (Table 2). Some studies discovered co-occurrences of KRAS and GNAS mutations in both low-grade and high-grade lesions of PMP and AMN by NGS in formalin-fixed paraffin-embedded (FFPE) samples [4, 30, 32, 34, 44, 51, 52]. For example, Yanai et al. [34] used NGS on FFPE samples to identify a co-occurrence rate of 15% in LAMN, 13% in PMP cases caused by HAMN, and 22% in MAC. Pietrantonio et al. [51] supports this as they found that GNAS mutations were significantly associated with KRAS mutations (P=0.002) and noted a co-occurrence rate of 52% in their PMP samples. Flatmark et al. [30] used NGS on FFPE samples and noted co-occurrences in 87% of their low-grade PMP and 100% of their high-grade PMP samples. Two studies did not specify the rates according to histological subtype in their samples of PMP; however, Gleeson et al. [44] found a co-occurrence rate of 87% and Pietrantonio et al. [51] found a co-occurrence rate of 64%.
Other studies comprised of only low-grade samples also documented the co-occurrence of KRAS and GNAS mutations using the same experimental methods [35, 38, 42, 45, 48, 59]. Using NGS, Foster et al. [35] noted a co-occurrence rate of 100% in their sample of LGMCP, Tsai et al. [38] identified a co-occurrence rate of 35% in LAMN and 83% in PMP cases caused by LAMN, and Liu et al. [59] identified a co-occurrence rate of 40% in their sample of LAMN. Pengelly et al. [45] identified a co-occurrence rate of 100% in their sample of LAMN using whole-exome sequencing, and Alakus et al. [4] noted a co-occurrence rate of 69% in their sample of LAMN and PMP using PCR. There were two case reports that used NGS: Matson et al. [48] found that both KRAS and GNAS were present in their patient with LAMN (n=1), and Wen et al. [46] found the same in their patient with MAC (n=1).
The low co-occurrence rate in MAC has also been established by Liao et al. [32] who noted the co-occurrence to be 63% in LAMN, 56% in HAMN, and 10% in MAC. Zhu et al. [42] supports this as they noted the co-occurrence to be 57% in LAMN, 57% in moderately differentiated MAC, and 23% in poorly differentiated MAC. The co-occurrences of these mutations in multiple studies indicate that they are a common characteristic of PMP. This suggests that whilst there may be a relationship between LAMN and HAMN on a molecular level, there are other gene mutations that are responsible for the progression from LAMN to HAMN such as TP53, and this distinguishes these neoplasms from MAC which have markedly lower expression of KRAS and GNAS mutations.
Studies (n=17) noted the presence of TP53 mutations in PMP and AMN samples [4, 26, 32, 34, 35, 38,39,40,41,42,43,44, 51, 52, 55, 57, 59]. Nine papers noted TP53 expression in only high-grade neoplasms and PMP [4, 26, 32, 38,39,40, 44, 57, 59], whereas four papers noted TP53 expression in both low-grade and high-grade neoplasms [34, 35, 42, 55] (Table 2). Specifically, Nummela et al. [57] noted that P53 protein expression was significantly associated with HAMN (P=0.012). In studies where TP53 was expressed exclusively in PMP caused by high-grade neoplasms, this indicated that this mutation led to more malignant phenotypes [26, 44]. This was expected as high-grade neoplasms harboured more gene mutations [42, 44] and exhibited more malignant cytology compared to low-grade neoplasms [2]. Some studies did not stratify their findings into histological subtype, and therefore it was not possible to report whether TP53 mutations were exclusive to a specific tumour grade [41, 43, 51, 52].
3.2 Prognostic value of mutations and molecular subtypes
Two studies identified molecular subtypes according to gene expression patterns and stratified patient samples into immune-enriched, oncogene-enriched, or mixed subtypes [31, 37] (Table 2). The oncogene-enriched subtype was characterised by overexpression of genes associated with cancer progression including ERBB2, SLC44A4, and EPCAM, whereas the immune-enriched subtype was marked by overexpression of genes with roles in immune pathways including IL23A, TRA, and CD37. The mixed subtype was characterised by overexpression of genes from both categories. The oncogene-enriched subtype had a significantly lower OS of 1.4 years than the immune-enriched (7.7 years) and mixed subtypes (3.6 years) (P=0.005), and the molecular subtypes were independent predictors for survival [31, 37]. This was expected as oncogene-enriched subtype tumours exhibited more aggressive tumour growth and had an increased expression of gene mutations involved in cell proliferation (ERBB2, SLC44A4, EPCAM, CLDN3, and CLDN4), cell differentiation (ELF3 and GPX2), and mucin production (KRT20).
Levine et al. [53] developed a 2-tier prognostic molecular subtype classification based on the gene expression profile of 139 genes in LGMCP. Unsupervised hierarchical clustering analysis identified two molecular subtypes based on gene expression patterns and their association with survival outcomes. These were denoted ‘favourable-prognosis subtype’ marked by increased expression of pathway signatures reflecting allograft rejection and antigen processing and presentation, and ‘poor-prognosis subtype’ marked by overexpression of proto-oncogenes including EPCAM, CEACAM5, FGFR3, HER-2, and MET. They noted that a subset of LGMCP predominantly associated with the poor-prognosis subtype group did not respond to CRS/HIPEC. The higher failure rate indicated there was a potential role for adjuvant, systemic therapies in this subset of patients which may be determined according to the gene mutation profiles.
Out of the 46 studies, 16 studies (35%) undertook survival analyses (Table 3). Pietrantonio et al. [51] noted that KRAS mutation status was an independent predictor of PFS in a multivariate analysis. However, other studies found no significant difference in the OS in KRAS-mutated neoplasms compared to KRAS wild-type, and KRAS mutations were not an independent prognostic factor for OS [60, 61]. Although two studies noted that samples with GNAS mutations had significantly shorter median PFS [51, 52], one study found no significant difference in OS in tumours with GNAS mutations compared to those without [60]. Additionally, samples with loss of SMAD4 expression had a significantly lower OS than those with preserved expression but it was not an independent factor of the same [58]. Three studies agreed that TP53 mutations and p53 expression were associated with poorer PFS and OS in log-rank tests [42, 57, 61]. However, they did not reach a consensus on their effect as independent predictors in multivariate analyses [42, 57]. One study noted that patients with relapsed PMP receiving palliative treatment of combined metronomic capecitabine and bevacizumab achieved a median PFS of 8.2 months with a 1-year OS of 91% [52]. Whilst this suggests that the drugs were effective, it would be beneficial to compare the effect of this combination treatment with a cohort that did not receive the drugs or with other drug treatments to make accurate comparisons on the true efficacy of the treatment and compare survival endpoints. Lastly, five studies concluded that tumour grade was an independent prognostic factor for survival [37, 42, 53, 58, 60]. However, Nummela et al. [57] did not find this to be statistically significant in their multivariate analysis. Tumours should be graded with the same classification system, and survival analyses should be undertaken for each histological subtype separately to allow for accurate comparisons on the role of individual gene mutations on survival to be made. The survival analysis findings have been summarised in Table 3.
3.3 Risk of bias
Overall, across all four domains, 41% (n=19) papers had a low risk of bias, and 59% (n=27) had a moderate risk of bias due to conflicts with the confounding domains (Supplementary Table S2). Two studies did not specify the origin of their tumours as their samples consisted of synchronous mucinous tumours of appendiceal and ovarian origin [72, 73]. Other studies (n=25) had issues with tumour grading: 12 did not specify what classification system was used [4, 35, 36, 41, 47, 50,51,52, 54, 59, 62, 66], five used older versions of the World Health Organization (WHO) classification system [49, 57, 67, 68, 70], four used the Bradley classification [31, 37, 53, 61], two used older versions of the American Joint Committee on Cancer Staging Manual [58, 60], one used the Misdraji classification [63], and one used the TNM classification of malignant tumours [40]. Due to the variations in nomenclature, 18 out of these 25 studies had a moderate reporting bias as they stratified their results according to tumour grades, which may have influenced the subsequent analyses. All studies in the systematic review had a low risk of selection and information bias.
4 Discussion
This systematic review included 46 studies and found KRAS, GNAS, and TP53 were the most frequently identified somatic gene mutations with other genetic alterations recorded in lower frequencies. Moreover, three papers identified molecular subtypes based on gene signatures that had prognostic value [31, 37, 53]. The mean age recorded in these papers ranged from 51 to 68 years, and there was an overall female predominance (≥51%) in their samples. Although the WHO does not have global statistics on PMP or AMN, Orphanet (the portal for rare diseases and orphan drugs) states that PMP has a female predominance with an age of onset after 40 years which shows that these studies represent global data [75]. There is an unmet need to establish rational treatment options for PMP patients for which the current gold standard CRS-HIPEC does not offer a cure of the natural disease progression.
4.1 KRAS, GNAS, and TP53 mutations in PMP and AMN
KRAS is a proto-oncogene that codes for the RAS involved in the RAS/Raf/MAP-kinase pathway regulating cell differentiation, proliferation, and apoptosis (Supplementary Figure S1) [76, 77]. RAS has also been noted to activate other pathways such as the PI3K-AKT-mTOR pathway which is involved in promoting cell growth and suppressing apoptosis [78] (Supplementary Figure S1A). Most common mutations in KRAS associated with cancer result in aberrant RAS activation, leading to uncontrolled cell growth, contributing to tumourigenesis [76, 79] (Supplementary Figure S1B) [80]. The high prevalence of KRAS mutations across histological subtypes, particularly in PMP (64–100%), confirms that it is a hallmark feature in these neoplasms.
Small molecule inhibitors have been developed to specifically target KRAS mutations and have been tested in solid tumour models including colorectal, pancreatic, ovarian, and lung cancer. For example, MRTX849 (adagrasib) is an irreversible covalent inhibitor, selectively binding to KRAS G12C (G>T) in its GDP-bound state, keeping the mutated protein locked in its inactive form. As a result, the Raf/MAPK pathway is not activated, preventing tumour growth and proliferation [78]. These were ground-breaking findings as they provided a foundation for targeting this mutation in cancer. This compound has shown promising results in a phase I/II clinical trial for colorectal cancer [81], non-small cell lung cancer [82], and pancreatic adenocarcinoma namely KRYSTAL-1 (ClinicalTrials.gov; ID: NCT03785249) [79]. Other clinical trials have identified sotorasib (ClinicalTrials.gov; ID: NCT03600883) [83, 84], JAB-21822 (ClinicalTrials.gov; ID: NCT05009329), and D-1553 (ClinicalTrials.gov; ID: NCT04585035) as targeted treatments for KRAS G12C mutations in solid tumours, non-small cell lung cancer, and colorectal cancer with sotorasib already approved as a treatment for small cell lung cancer. Both variants, KRAS G12D and G12C, are missense mutations affecting a commonly mutated codon in PMP. We performed functional annotation of the KRAS G12D variant using the Ensembl variant effect predictor (VEP) (https://www.ensembl.org/Tools/VEP, date accessed: 13 October 2022). G12D is predicted to be functionally deleterious (SIFT) and likely to be clinically pathogenic (ClinVar) (Supplementary Table 4). Notably, very recent clinical trials are utilising HRS-4642 (ClinicalTrials.gov; ID: NCT05533463) and ASP3082 (ClinicalTrials.gov; ID: NCT05382559) to specifically target KRAS G12D mutations in solid tumours. This supports a rationale to also explore targeting KRAS G12D in pre-clinical studies in PMP to produce preliminary results supporting a clinical trial.
In PMP, the character-defining redistribution phenomenon occurs when extracellular mucin follows the normal flow of peritoneal fluid, redistributing the mucin and neoplastic cells [3, 5]. Therefore, targeting mucin production would help prevent metastatic spread. Dilly et al. [85] investigated the use of dual MEK-PI3K drug therapy against KRAS-mutated mucinous appendiceal and colonic cancers as well as a mucin 2-secreting LS174T cell line. Using co-treatment with trametinib, a MEK inhibitor, and pictilisib, a PI3K inhibitor, they noted that there were reduced phosphorylated-ERK and phosphorylated-AKT protein levels which supported the notion that MAPK/PI3K signalling was inhibited. There was a significant decrease in MUC2 expression suggesting an effective mucinous tumour growth suppression which may be an effective therapy in these patients.
GNAS is a complex locus that codes for the stimulatory alpha subunit of the guanine nucleotide-binding protein complex (G-protein) (Gsα) involved in the protein kinase A (PKA) pathway-regulating metabolism, cell growth, and differentiation (Supplementary Figure S2A) [86, 87]. In PMP and AMN, the variants of GNAS mutations are most commonly located on codons R201C and R201H [30]. These variants code for a mutated form of Gsα which will lead to aberrant activation of adenylate cyclase resulting in the constant activation of downstream signalling leading to uncontrolled cell proliferation (Supplementary Figure 2B).
In the reviewed studies, GNAS mutations were identified in both low-grade and high-grade neoplasms at high frequencies (ranging 31–100%), and the most common variants were R201C and R201H (Table 2). Studies have indicated that GNAS mutations may have a role in mucin production, a key morbidity of PMP [26, 63]. Nishikawa et al. [63] noted that GNAS mutations were significantly associated with the protein expression of MUC5AC (P=0.037) in LAMN and MAC. When introduced into the colorectal cell line HT29, GNAS mutations led to a significant increase of MUC2 and MUC5AC expression which are well known for their role in mucin production in PMP. This implicates the PKA pathway as a potential therapeutic target for managing mucinous ascites, a hypothesis that requires further investigation.
A recent study using blood and tumour samples from PMP patients (samples used from Clinical Trials.gov; ID: NCT02073500) [30], identified GNAS mutations (R201H and R201C) and suggested the resulting Gsα to be a potential neoantigen. In vitro stimulation of PBMCs using peptides containing aforementioned point mutations resulted in strong immune responses as measured by proliferation and IFN-γ production. Additionally, CyTOF analysis of tumour samples revealed expression of immune checkpoint (IC) molecules, particularly TIGIT and PD-1 in infiltrating T cells, suggesting a pre-existing immune response, providing the rationale for combination therapy with IC inhibitors and Gsα peptide vaccine in PMP.
Developing successful treatments that target point mutations per se, has been challenging due to the intrinsic characteristics of the proteins they encode, and targeting strategies have been nonspecific and inefficient [88]. Small molecule inhibitors have shown controversial efficacy, due to lack of activity or selectivity, and significant off target effects [88]. This has become apparent with the unsuccessful efforts to target TP53 mutations in the past decades [89, 90]. Nevertheless, the recent clinical trials focussing efforts on directly targeting GNAS and KRAS mutations have shown promising advances with considerable clinical efficacy.
4.2 Molecular subtypes
CRS/HIPEC is the current standard of care treatment for PMP, albeit with high failure rates. Sinukumar et al. [91] noted that only 44% achieved complete cytoreduction with no residual tumour, and Chua et al. [92] found that 49% of their sample had recurrence of disease in less than 12 months after surgery. Surgeons make the decision to proceed with incomplete CRS/HIPEC based on their own experience and discretion, but there is no rational consensus or tool to guide this decision in the clinical setting. Three studies identified molecular subtypes in samples with failed or incomplete CRS/HIPEC based on gene expression profiles and found favourable-prognosis, poor-prognosis, oncogene-enriched, immune-enriched, and mixed subtypes with prognostic value [31, 37, 53].
Two studies developed molecular subtypes according to gene expression patterns and stratified their patient samples into immune-enriched, oncogene-enriched, or mixed subtypes [31, 37]. The oncogene-enriched subtype had no long-term survivors as they had a mean OS of 1.4 years [31], which implied that incomplete CRS should be avoided in this subtype as it did not yield a prolonged benefit. By contrast, the immune-enriched subtype had a longer survival with a mean OS of 7.7 years [31] which supported the use of CRS/HIPEC even in the event of incomplete cytoreduction. A future hypothesis may explore the efficacy of preoperative chemotherapy treatment in patients with oncogene-enriched subtypes and preoperative immunotherapy treatment in those with immune-enriched subtypes as adjuvant treatments to CRS/HIPEC to further improve the OS.
Levine et al. [53] developed two different molecular subtypes in LGMCP known as poor-prognosis and favourable-prognosis subtypes. The differences in the molecular subtypes implied that there was heterogeneity within low-grade neoplasms, and some were more aggressive in nature despite their low-grade histology. Consequently, there is potential for personalised and targeted treatment plans. For example, the poor-prognosis subtype had an overexpression of genes such as the MET proto-oncogene, known to activate multiple oncogenic pathways such as MAPK/ERK and P13K/AKT [93]. Consequently, there is an opportunity to use agents that target MET in this subset of patients. Rilotumumab, an inhibitor of hepatocyte growth factor/MET pathway was found to significantly increase OS in patients with overexpressed MET in gastric and oesophagogastric junction adenocarcinomas (ClinicalTrials.gov; ID: NCT00719550) [94]. If these molecular subtypes are to be used in a clinical setting to predict the outcomes of CRS/HIPEC and improve treatment efficacy, this warrants validation through a randomised-controlled clinical trial.
4.3 Survival analysis in PMP and AMN
Prognosis has an important role in oncology for patients and clinicians to make informed decisions about the most appropriate treatment option and its outcome [95, 96]. Survival analyses are effective methods of testing prognosis, yet there is a paucity of data on the effect of gene mutations on the survival in PMP or AMN patients. Studies in this systematic review attempt to address this; however, there were conflicting conclusions on the effects of individual gene mutations on survival. We highlight the lack of consensus on the effect of individual genotypes on survival and suggest that molecular subtyping may be more effective in predicting survival as they have been proven to have prognostic value [31, 37, 53]. Within this remit, it may be useful to retrospectively map these molecular subtypes onto PMP datasets where transcriptomic data is readily available, to validate the prognostic value of the molecular subtypes.
4.4 Strengths and limitations
The robustness of the methodology in this systematic review is a key strength. The abstract screening process was done in duplicate, and the two reviewers had a relatively high agreement rate of 99.91%. This is reflective of clear inclusion and exclusion criteria which were wide enough to capture the diversity of studies on this topic and precise enough to ensure that substantial conclusions may be drawn from the findings [97]. The search strategy was well-developed and included papers from 1995 to 2021 as the oldest study exploring the gene profile of AMN was published in 1996 [98]. Furthermore, there was a manual search of the reference list of Stein et al. [27] to account for any paper that may have been missed. Although the aims of the reviews were similar, there were notable differences in their study design compared to the current review. They only searched two databases and included studies up to 2016 whereas the current systematic review searched four databases and included studies up until 2020. This is important as there was an increase in publications on papers in this field between 2017 and 2021 (n=19), and studies published in 2020 introduced molecular subtypes and their role in prognosis [31, 37]. The risk of bias analysis identified that all studies in the review had a low risk of selection bias which indicated that their samples are accurate representations of the general population. The risk of bias analysis also provided an accurate assessment of the overall effect of the results which strengthened the conclusions drawn in this review.
Although this review yields valuable evidence about the genetic aberrations of PMP and AMN, there are some notable limitations. The sample sizes of older studies included in this review from 1996 to 2015 are relatively small (n=1) which may be due to the rarity and low incidence of PMP [1]. As a result, a small sample size may hinder the accuracy of statistical analyses due to low power [65]. Furthermore, NGS is more sensitive than Sanger sequencing and PCR and can identify more variants that may not be detectable by other techniques [99,100,101]. PMP has a low cellularity high mucin content, and therefore it is more challenging to perform NGS and Sanger sequencing since larger volumes of tumour cells are required [21]. Nonetheless, there is a risk that older studies (1996–2015) that used PCR may have failed to record key variations of the somatic mutations that were identified by NGS in more recent studies (2014–2020). Extreme heterogeneity in PMP histologies, for example the co-existence of high-grade with low-grade features in the same patient and the differences in histology between the primary (appendix) and metastatic (PMP) disease, may explain the differential prevalence rate of mutations seen. Moreover, the results cannot be averaged across studies due to the heterogeneity in study design, including sample size, tumour classification systems, tissue processing, and experimental methods used to investigate genetic aberrations. This highlights the need for greater standardisation of methods during validation so that the findings may be easily comparable, and conclusions may be more accurately translated into the clinical setting.
5 Conclusions
In summary, this review identified the genetic aberrations in PMP and AMN. KRAS, GNAS, and TP53 were the most frequently identified somatic mutations. Given the recent advances in clinical trials to directly target KRAS and GNAS mutations in other cancers, we propose a rationale to explore targeting KRAS G12C and G12D, and GNAS R201H and R201C in pre-clinical studies in PMP to produce preliminary results supporting a future clinical trial. Finally, given that molecular subtyping may be more effective in predicting survival, we encourage future clinical trials to complement the genotyping of PMP with transcriptomic analysis to validate and improve current molecular signatures and potentially develop more efficient clinical tools to predict survival and response to therapy.
References
Smeenk, R., Van Velthuysen, M., Verwaal, V., et al. (2008). Appendiceal neoplasms and pseudomyxoma peritonei: A population based study. European Journal of Surgical Oncology (EJSO), 34(2), 196–201.
Carr, N. J., Bibeau, F., Bradley, R. F., et al. (2017). The histopathological classification, diagnosis and differential diagnosis of mucinous appendiceal neoplasms, appendiceal adenocarcinomas and pseudomyxoma peritonei. Histopathology, 71(6), 847–858.
Carr, N. J., Cecil, T. D., Mohamed, F., et al. (2016). A consensus for classification and pathologic reporting of pseudomyxoma peritonei and associated appendiceal neoplasia: The results of the Peritoneal Surface Oncology Group International (PSOGI) modified Delphi Process. The American journal of surgical pathology, 40(1), 14–26.
Alakus, H., Babicky, M., Ghosh, P., et al. (2014). Genome-wide mutational analysis reveals core signaling pathways in mucinous neoplasms of the appendix. Cancer Research, 74(19), 1.
Sugarbaker, P. H. (1994). Pseudomyxoma peritonei: A cancer whose biology is characterized by a redistribution phenomenon. Annals of Surgery, 219(2), 109–111.
Bree, E. D., Witkamp, A., Van De Vijver, M., et al. (2000). Unusual origins of pseudomyxoma peritonei. Journal of surgical oncology, 75(4), 270–274.
Ronnett, B. M., Kurman, R. J., Zahn, C. M., et al. (1995). Pseudomyxoma peritonei in women: A clinicopathologic analysis of 30 cases with emphasis on site of origin, prognosis, and relationship to ovarian mucinous tumors of low malignant potential. Human Pathology, 26(5), 509–524.
Young, R. H., Gilks, C. B., & Scully, R. E. (1991). Mucinous tumors of the appendix associated with mucinous tumors of the ovary and pseudomyxoma peritonei. A clinicopathological analysis of 22 cases supporting an origin in the appendix. The American journal of surgical pathology, 15(5), 415–429.
Misdraji, J., Yantiss, R. K., Graeme-Cook, F. M., et al. (2003). Appendiceal mucinous neoplasms: A clinicopathologic analysis of 107 cases. Am J Surg Pathol, 27(8), 1089–1103.
Bradley, R. F., Stewart IV, J. H., Russell, G. B., et al. (2006). Pseudomyxoma peritonei of appendiceal origin: A clinicopathologic analysis of 101 patients uniformly treated at a single institution, with literature review. The American journal of surgical pathology, 30(5), 551–559.
Sugarbaker, P. H. (2006). New standard of care for appendiceal epithelial neoplasms and pseudomyxoma peritonei syndrome? The lancet oncology, 7(1), 69–76.
Sugarbaker, P. H. (2001). Cytoreductive surgery and perioperative intraperitoneal chemotherapy as a curative approach to pseudomyxoma peritonei syndrome. Tumori Journal, 87(4), 3–5.
Kusamura, S., O’Dwyer, S. T., Baratti, D., et al. (2008). Technical aspects of cytoreductive surgery. Journal of surgical oncology, 98(4), 232–236.
Chua, T. C., Moran, B. J., Sugarbaker, P. H., et al. (2012). Early-and long-term outcome data of patients with pseudomyxoma peritonei from appendiceal origin treated by a strategy of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Journal of Clinical Oncology, 30(20), 2449–2456.
Gusani, N. J., Cho, S. W., Colovos, C., et al. (2008). Aggressive surgical management of peritoneal carcinomatosis with low mortality in a high-volume tertiary cancer center. Annals of Surgical Oncology, 15(3), 754–763.
Miner, T. J., Shia, J., Jaques, D. P., et al. (2005). Long-term survival following treatment of pseudomyxoma peritonei: An analysis of surgical therapy. Annals of Surgery, 241(2), 300.
Sommariva, A., Tonello, M., Rigotto, G., et al. (2021). Novel perspectives in pseudomyxoma peritonei treatment. Cancers (Basel), 13(23), 5965.
Govaerts, K., Lurvink, R. J., De Hingh, I. H. J. T., et al. (2021). Appendiceal tumours and pseudomyxoma peritonei: Literature review with PSOGI/EURACAN clinical practice guidelines for diagnosis and treatment. European Journal of Surgical Oncology, 47(1), 11–35.
Kusamura, S., Barretta, F., Yonemura, Y., et al. (2021). The role of hyperthermic intraperitoneal chemotherapy in pseudomyxoma peritonei after cytoreductive surgery. JAMA Surg, 156(3), e206363.
Järvinen, P., Ristimäki, A., Kantonen, J., et al. (2013). Feasibility of radical cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for pseudomyxoma peritonei of appendiceal origin. Scandinavian Journal of Surgery, 102(3), 145–151.
Baratti, D., Kusamura, S., Nonaka, D., et al. (2009). Pseudomyxoma peritonei biological features are the dominant prognostic determinants after complete cytoreduction and hyperthermic intraperitoneal chemotherapy. Annals of Surgery, 249(2), 243–249.
Muzny, D. M., Bainbridge, M. N., Chang, K., et al. (2012). Comprehensive molecular characterization of human colon and rectal cancer. Nature, 487(7407), 330–337.
Shukla, H. D. (2017). Comprehensive analysis of cancer-proteogenome to identify biomarkers for the early diagnosis and prognosis of cancer. Proteomes, 5(4), 28.
Tan, A. C., & Tan, D. S. W. (2022). Targeted therapies for lung cancer patients with oncogenic driver molecular alterations. J Clin Oncol, 40(6), 611–625.
Lau, K. H., Tan, A. M., & Shi, Y. (2022). New and emerging targeted therapies for advanced breast cancer. International Journal of Molecular Sciences, 23(4), 2288.
Noguchi, R., Yano, H., Gohda, Y., et al. (2015). Molecular profiles of high-grade and low-grade pseudomyxoma peritonei. Cancer Med, 4(12), 1809–1816.
Stein, A., Strong, E., Clark Gamblin, T., et al. (2020). Molecular and genetic markers in appendiceal mucinous tumors: A systematic review. Annals of Surgical Oncology, 27(1), 85–97.
Moher, D., Liberati, A., Tetzlaff, J., et al. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine, 6(7), e1000097.
Sterne, J. A., Hernán, M. A., Reeves, B. C., et al. (2016). ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ, 355, i4919.
Flatmark, K., Torgunrud, A., Fleten, K. G., et al. (2021). Peptide vaccine targeting mutated GNAS: a potential novel treatment for pseudomyxoma peritonei. Journal for immunotherapy of cancer, 9(10), e003109.
Moaven, O., Su, J., Jin, G., et al. (2020). Clinical implications of genetic signatures in appendiceal cancer patients with incomplete cytoreduction/HIPEC. Annals of Surgical Oncology, 27(13), 5016–5023.
Liao, X., Vavinskaya, V., Sun, K., et al. (2020). Mutation profile of high-grade appendiceal mucinous neoplasm. Histopathology, 76(3), 461–469.
King, M. C., Munoz-Zuluaga, C., Ledakis, P., et al. (2020). Germline and somatic genetic alterations in two first-degree relatives with appendiceal low-grade mucinous carcinoma peritonei. Clin Case Rep, 8(12), 3168–3177.
Yanai, Y., Saito, T., Hayashi, T., et al. (2020). Molecular and clinicopathological features of appendiceal mucinous neoplasms. Virchows Archiv, 478(3), 413–426.
Foster, J. M., Patel, A., Zhang, C., et al. (2020). Investigating the utility of extended mutation analysis in gastrointestinal peritoneal metastasis. Journal of Surgical Oncology, 122(6), 1106–1113.
Lung, M. S., Mitchell, C. A., Doyle, M. A., et al. (2020). Germline whole exome sequencing of a family with appendiceal mucinous tumours presenting with pseudomyxoma peritonei. BMC Cancer, 20(1), 369.
Su, J., Jin, G. X., Votanopoulos, K. I., et al. (2020). Prognostic molecular classification of appendiceal mucinous neoplasms treated with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Annals of Surgical Oncology, 27(5), 1439–1447.
Tsai, J. H., Yang, C. Y., Yuan, R. H., et al. (2019). Correlation of molecular and morphological features of appendiceal epithelial neoplasms. Histopathology, 75(4), 468–477.
LaFramboise, W. A., Pai, R. K., Petrosko, P., et al. (2019). Discrimination of low- and high-grade appendiceal mucinous neoplasms by targeted sequencing of cancer-related variants. Mod Pathol, 32(8), 1197–1209.
Liu, W., Liu, L., Wang, R., et al. (2019). Bevacizumab combined with oxaliplatin/capecitabine in patient with refractory and recurrent mucinous adenocarcinoma of the appendix: A case report. Front Oncol, 9, 55.
Tokunaga, R., Xiu, J., Johnston, C., et al. (2019). Molecular profiling of appendiceal adenocarcinoma and comparison with right-sided and left-sided colorectal cancer. Clinical Cancer Research, 25(10), 3096–3103.
Zhu, X., Salhab, M., Tomaszewicz, K., et al. (2019). Heterogeneous mutational profile and prognosis conferred by TP53 mutations in appendiceal mucinous neoplasms. Human Pathology, 85, 260–269.
Ang, C. S., Shen, J. P., Hardy-Abeloos, C. J., et al. (2018). Genomic landscape of appendiceal neoplasms. JCO Precision Oncology, 8(2), 1–18.
Gleeson, E. M., Feldman, R., Mapow, B. L., et al. (2018). Appendix-derived pseudomyxoma peritonei (PMP): Molecular profiling toward treatment of a rare malignancy. American Journal of Clinical Oncology, 41(8), 777–783.
Pengelly, R. J., Rowaiye, B., Pickard, K., et al. (2018). Analysis of mutation and loss of heterozygosity by whole-exome sequencing yields insights into pseudomyxoma peritonei. Journal of Molecular Diagnostics, 20(5), 635–642.
Wen, K. W., Grenert, J. P., Joseph, N. M., et al. (2018). Genomic profile of appendiceal goblet cell carcinoid is distinct compared to appendiceal neuroendocrine tumor and conventional adenocarcinoma. Human Pathology, 77, 166–174.
Ang, C., Stollman, A., Zhu, H., et al. (2017). Clinical benefit from trametinib in a patient with appendiceal adenocarcinoma with a gnas r201h mutation. case rep oncol, 10(2), 548–552.
Matson, D. R., Xu, J., Huffman, L., et al. (2017). KRAS and GNAS Co-mutation in metastatic low-grade appendiceal mucinous neoplasm (LAMN) to the ovaries: A practical role for next-generation sequencing. Am J Case Rep, 18, 558–562.
Saarinen, L., Nummela, P., Thiel, A., et al. (2017). Multiple components of PKA and TGF-β pathways are mutated in pseudomyxoma peritonei. PLoS One, 12(4), e0174898.
Borazanci, E., Millis, S. Z., Kimbrough, J., et al. (2017). Potential actionable targets in appendiceal cancer detected by immunohistochemistry, fluorescent in situ hybridization, and mutational analysis. J Gastrointest Oncol, 8(1), 164–172.
Pietrantonio, F., Perrone, F., Mennitto, A., et al. (2016). Toward the molecular dissection of peritoneal pseudomyxoma. Ann Oncol, 27(11), 2097–2103.
Pietrantonio, F., Berenato, R., Maggi, C., et al. (2016). GNAS mutations as prognostic biomarker in patients with relapsed peritoneal pseudomyxoma receiving metronomic capecitabine and bevacizumab: A clinical and translational study. Journal of Translational Medicine, 14(1), 125.
Levine, E. A., Votanopoulos, K. I., Qasem, S. A., et al. (2016). Prognostic molecular subtypes of low-grade cancer of the appendix. Journal of the American College of Surgeons, 222(4), 493–503.
Wu, R. L., Ali, S., Sarkar, F. H., et al. (2015). Identification of differentially expressed miRNAs in appendiceal mucinous cystadenocarcinoma from mucinous cystadenoma. J Cancer Sci Ther, 7(11), 328–335.
Hara, K., Saito, T., Hayashi, T., et al. (2015). A mutation spectrum that includes GNAS, KRAS and TP53 may be shared by mucinous neoplasms of the appendix. Pathol Res Pract, 211(9), 657–664.
Roberts, D. L., O'Dwyer, S. T., Stern, P. L., et al. (2015). Global gene expression in pseudomyxoma peritonei, with parallel development of two immortalized cell lines. Oncotarget, 6(13), 10786–10800.
Nummela, P., Saarinen, L., Thiel, A., et al. (2015). Genomic profile of pseudomyxoma peritonei analyzed using next-generation sequencing and immunohistochemistry. International Journal of Cancer, 136(5), E282–E289.
Davison, J. M., Hartman, D. A., Singhi, A. D., et al. (2014). Loss of SMAD4 protein expression is associated with high tumor grade and poor prognosis in disseminated appendiceal mucinous neoplasms. Am J Surg Pathol, 38(5), 583–592.
Liu, X., Mody, K., De Abreu, F. B., et al. (2014). Molecular profiling of appendiceal epithelial tumors using massively parallel sequencing to identify somatic mutations. Clinical Chemistry, 60(7), 1004–1011.
Singhi, A. D., Davison, J. M., Choudry, H. A., et al. (2014). GNAS is frequently mutated in both low-grade and high-grade disseminated appendiceal mucinous neoplasms but does not affect survival. Human Pathology, 45(8), 1737–1743.
Shetty, S., Thomas, P., Ramanan, B., et al. (2013). Kras mutations and p53 overexpression in pseudomyxoma peritonei: association with phenotype and prognosis. Journal of Surgical Research, 180(1), 97–103.
Pulighe, F., Paliogiannis, P., Cossu, A., et al. (2013). Molecular analysis of appendiceal mucinous cystadenoma and rectal adenocarcinoma in a patient with urothelial carcinoma: A case report. J Med Case Rep, 7, 170.
Nishikawa, G., Sekine, S., Ogawa, R., et al. (2013). Frequent GNAS mutations in low-grade appendiceal mucinous neoplasms. Br J Cancer, 108(4), 951–958.
Zauber, P., Berman, E., Marotta, S., et al. (2011). Ki-ras gene mutations are invariably present in low-grade mucinous tumors of the vermiform appendix. Scand J Gastroenterol, 46(7-8), 869–874.
Maheshwari, V., Tsung, A., Lin, Y., et al. (2006). Analysis of loss of heterozygosity for tumor-suppressor genes can accurately classify and predict the clinical behavior of mucinous tumors arising from the appendix. Annals of Surgical Oncology, 13(12), 1610–1616.
Sebastian, A. R., Fernandez Morejon, F. J., Boix, P. B., et al. (2006). Controversial origin of pseudomyxoma peritonei. Clinical and Translational Oncology, 8(10), 767–769.
Feltmate, C. M., Lee, K. R., Johnson, M., et al. (2005). Whole-genome allelotyping identified distinct loss-of-heterozygosity patterns in mucinous ovarian and appendiceal carcinomas. Clin Cancer Res, 11(21), 7651–7657.
Maru, D., Wu, T. T., Canada, A., et al. (2004). Loss of chromosome 18q and DPC4 (Smad4) mutations in appendiceal adenocarcinomas. Oncogene, 23(3), 859–864.
O'Connell, J. T., Hacker, C. M., & Barsky, S. H. (2002). MUC2 is a molecular marker for pseudomyxoma peritonei. Modern Pathology, 15(9), 958–972.
Kabbani, W., Houlihan, P. S., Luthra, R., et al. (2002). Mucinous and nonmucinous appendiceal adenocarcinomas: Different clinicopathological features but similar genetic alterations. Mod Pathol, 15(6), 599–605.
Shih, I. M., Yan, H., Speyrer, D., et al. (2001). Molecular genetic analysis of appendiceal mucinous adenomas in identical twins, including one with pseudomyxoma peritonei. American Journal of Surgical Pathology, 25(8), 1095–1099.
Szych, C., Staebler, A., Connolly, D. C., et al. (1999). Molecular genetic evidence supporting the clonality and appendiceal origin of Pseudomyxoma peritonei in women. American Journal of Pathology, 154(6), 1849–1855.
Chuaqui, R. F., Zhuang, Z., Emmert-Buck, M. R., et al. (1996). Genetic analysis of synchronous mucinous tumors of the ovary and appendix. Human Pathology, 27(2), 165–171.
Munari, G., Businello, G., Mattiolo, P., et al. (2021). Molecular profiling of appendiceal serrated lesions, polyps and mucinous neoplasms: A single-centre experience. Journal of Cancer Research and Clinical Oncology, 147(7), 1897–1904.
Orphanet. Pseudomyxoma peritonei summary. https://www.orpha.net/consor/cgi-bin/OC_Exp.php?Expert=26790&lng=EN (accessed 29 June 2021).
Molina, J. R., & Adjei, A. A. (2006). The Ras/Raf/MAPK pathway. Journal of Thoracic Oncology, 1(1), 7–9.
Seger, R., & Krebs, E. G. (1995). The MAPK signaling cascade. The FASEB Journal, 9(9), 726–735.
Lambert, J. M., Lambert, Q. T., Reuther, G. W., et al. (2002). Tiam1 mediates Ras activation of Rac by a PI(3)K-independent mechanism. Nature Cell Biology, 4(8), 621–625.
Simanshu, D. K., Nissley, D. V., & McCormick, F. (2017). RAS proteins and their regulators in human disease. Cell, 170(1), 17–33.
Mukhopadhyay, S., Vander Heiden, M. G., & McCormick, F. (2021). The metabolic landscape of RAS-driven cancers from biology to therapy. Nature Cancer, 2(3), 271–283.
Johnson, M. L., Ou, S. H. I., Barve, M., et al. (2020). 4LBA Late breaking - KRYSTAL-1: Activity and safety of adagrasib (MRTX849) in patients with colorectal cancer (CRC) and other solid tumors harboring a KRAS G12C mutation. European Journal of Cancer, 138, S2.
Jänne, P. A., Riely, G. J., Gadgeel, S. M., et al. (2022). Adagrasib in non-small-cell lung cancer harboring a KRAS(G12C) mutation. N Engl J Med, 387(2), 120–131.
Skoulidis, F., Li, B. T., Dy, G. K., et al. (2021). Sotorasib for lung cancers with KRAS p.G12C mutation. N Engl J Med, 384(25), 2371–2381.
Canon, J., Rex, K., Saiki, A. Y., et al. (2019). The clinical KRAS(G12C) inhibitor AMG 510 drives anti-tumour immunity. Nature, 575(7781), 217–223.
Dilly, A., Honick, B. D., Lee, Y. J., et al. (2020). Rational application of targeted therapeutics in mucinous colon/appendix cancers with positive predictive factors. Cancer Medicine, 9(5), 1753–1767.
Skalhegg, B., & Tasken, K. (2000). Specificity in the cAMP/PKA signaling pathway. Differential expression, regulation, and subcellular localization of subunits of PKA. Front Biosci, 5(5), D678–DD93.
Hannah-Shmouni, F. (2016). Alterations of phosphodiesterases in adrenocortical tumors. Frontiers in Endocrinology, 30(7), 111.
Dang, C. V., Reddy, E. P., Shokat, K. M., et al. (2017). Drugging the ‘undruggable’ cancer targets. Nat Rev Cancer, 17(8), 502–508.
Sanz, G., Singh, M., Peuget, S., et al. (2019). Inhibition of p53 inhibitors: Progress, challenges and perspectives. J Mol Cell Biol, 11(7), 586–599.
Hu, J., Cao, J., Topatana, W., et al. (2021). Targeting mutant p53 for cancer therapy: Direct and indirect strategies. Journal of Hematology & Oncology, 14(1), 157.
Sinukumar, S., Mehta, S., As, R., et al. (2019). Analysis of clinical outcomes of pseudomyxoma peritonei from appendicular origin following cytoreductive surgery and hyperthermic intraperitoneal chemotherapy-A retrospective study from INDEPSO. Indian journal of surgical oncology, 10(Suppl 1), 65–70.
Chua, T. C., Liauw, W., & Morris, D. L. (2012). Early recurrence of pseudomyxoma peritonei following treatment failure of cytoreductive surgery and perioperative intraperitoneal chemotherapy is indicative of a poor survival outcome. Int J Colorectal Dis, 27(3), 381–389.
Gherardi, E., Birchmeier, W., Birchmeier, C., et al. (2012). Targeting MET in cancer: Rationale and progress. Nat Rev Cancer, 12(2), 89–103.
Iveson, T., Donehower, R. C., Davidenko, I., et al. (2014). Rilotumumab in combination with epirubicin, cisplatin, and capecitabine as first-line treatment for gastric or oesophagogastric junction adenocarcinoma: An open-label, dose de-escalation phase 1b study and a double-blind, randomised phase 2 study. Lancet Oncol, 15(9), 1007–1018.
Mackillop, W. J. (2006). The importance of prognosis in cancer medicine TNM Online. (eds. L. H. Sobin, M. K. Gospodarowicz, B. O'Sullivan, L. H. Sobin, D. E. Henson, & R. V. P. Hutter).
Halabi, S., & Owzar, K. (2010). The importance of identifying and validating prognostic factors in oncology. Seminars in oncology, 37(2), e9–e18.
McKenzie JE, Brennan SE, Ryan RE, et al. Chapter 3: Defining the criteria for including studies and how they will be grouped for the synthesis. In: Cochrane Handbook for Systematic Reviews of Interventions. 6.2 ed; 2021.
Cuatrecasas, M., Matias-Guiu, X., & Prat, J. (1996). Synchronous mucinous tumors of the appendix and the ovary associated with pseudomyxoma peritonei. A clinicopathologic study of six cases with comparative analysis of c-Ki-ras mutations. American Journal of Surgical Pathology, 20(6), 739–746.
Tuononen, K., Mäki-Nevala, S., Sarhadi, V. K., et al. (2013). Comparison of targeted next-generation sequencing (NGS) and real-time PCR in the detection of EGFR, KRAS, and BRAF mutations on formalin-fixed, paraffin-embedded tumor material of non-small cell lung carcinoma-superiority of NGS. Genes Chromosomes Cancer, 52(5), 503–511.
de Biase, D., Visani, M., Baccarini, P., et al. (2014). Next generation sequencing improves the accuracy of KRAS mutation analysis in endoscopic ultrasound fine needle aspiration pancreatic lesions. PLoS One, 9(2), e87651.
Vigliar, E., Malapelle, U., de Luca, C., et al. (2015). Challenges and opportunities of next-generation sequencing: A cytopathologist’s perspective. Cytopathology, 26(5), 271–283.
Author information
Authors and Affiliations
Contributions
Conceptualization, N.W.M. and S.P.B.; methodology, N.W.M., N.M.A, and S.P.B.; investigation, N.W.M., N.M.A, and S.P.B.; resources, N.W.M., N.M.A, T.J.U., and S.P.B.; writing—original draft preparation, N.W.M. and S.P.B.; writing—review and editing, N.W.M., N.M.A, T.J.U., Z.S.W., and S.P.B.; visualisation, N.W.M. and S.P.B.; supervision, S.P.B.; project administration, N.W.M. and S.P.B.. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
: Table S1: Classification of mucinous epithelial neoplasia of the appendix, intra-abdominal mucin, and pseudomyxoma peritonei. (DOCX 19 kb)
ESM 2
: Table S2: Assessment of the quality and risk of bias of included studies. (DOCX 89 kb)
ESM 3
: Table S3: All gene mutations identified in this systematic review. (DOCX 105 kb)
ESM 4
: Table S4: Somatic mutations in KRAS G12D and predicted influence on protein function. (XLSX 11 kb)
ESM 5
: Figure S1: The RAS/Raf/MAP-Kinase Pathway. (DOCX 564 kb)
ESM 6
: Figure S2: GNAS in the cAMP-PKA pathway. (DOCX 662 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Murage, N.W., Ahmed, N.M., Underwood, T.J. et al. The genetic profile and molecular subtypes of human pseudomyxoma peritonei and appendiceal mucinous neoplasms: a systematic review. Cancer Metastasis Rev 42, 335–359 (2023). https://doi.org/10.1007/s10555-023-10088-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-023-10088-0