Abstract
This study sought to evaluate the impact of severe obesity on image quality and ventricular function assessment in cardiovascular magnetic resonance (MRI) and trans-thoracic echocardiography (TTE). We studied 100 consecutive patients who underwent clinically indicated cardiac MRI and TTE studies within 12 months between July 2017 and December 2020; 50 (28 females and 22 males; 54.5 ± 18.7 years) with normal body mass index (BMI) (18.5–25 kg/m2) and 50 (21 females and 29 males; 47.2 ± 13.3 years) with severe obesity (BMI ≥ 40 kg/m2). MRI and TTE image quality scores were compared within and across cohorts using a linear mixed model. Categorical left (LVF) and right (RVF) ventricular function were compared using Cohens Kappa statistic. Mean BMI for normal weight and obese cohorts were 22.2 ± 1.7 kg/m2 and 50.3 ± 5.9 kg/m2, respectively. Out of a possible 93 points, mean MRI image quality score was 91.5 ± 2.5 for patients with normal BMI, and 88.4 ± 5.5 for patients with severe obesity; least square (LS) mean difference 3.1, p = 0.460. TTE scores were 64.2 ± 13.6 for patients with normal BMI and 46.0 ± 12.9 for patients with severe obesity, LS mean difference 18.2, p < 0.001. Ventricular function agreement between modalities was worse in the obese cohort for both LVF (72% vs 80% agreement; kappa 0.53 vs 0.70, obese vs. normal BMI), and RVF (58% vs 72% agreement, kappa 0.18 vs 0.34, obese vs. normal BMI). Severe obesity had limited impact on cardiac MRI image quality, while obesity significantly degraded TTE image quality and ventricular function agreement with MRI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity affects over 40% of adults in the United States with rising prevalence and worsening severity; nearly 10% of adults now have a body mass index (BMI) ≥ 40 kg/m2 (severe or Class III obesity) [1, 2]. Obesity has long been recognized as a strong independent predictor of cardiovascular disease (CVD) [3,4,5], and non-invasive imaging modalities including transthoracic echocardiography (TTE), computed tomography (CT), single photon emission tomography (SPECT), and cardiovascular magnetic resonance imaging (MRI) are commonly used to evaluate CVD. However, imaging of patients with severe obesity poses technical challenges for all modalities, including table weight and bore diameter limitations, higher radiation dosing, and signal attenuation that reduces signal–noise ratio (SNR) and causes artifacts [6,7,8,9].
The accuracy of left (LVF) and right (RVF) ventricular function assessment is critical for contemporary management of numerous cardiovascular diseases [10]. MRI has high spatial and temporal resolution, measures chamber volumes without geometric assumptions, and is the reference standard for quantitative LVF and RVF [11]. Though inter-observer variability is improved with three-dimensional contrast-enhanced TTE, the limits of TTE agreement with cardiac MRI remains wide for both LVF [12] and RVF [13, 14]. The potential for patient misclassification based on inaccurate ventricular function assessment can subsequently lead to additional downstream testing or unnecessary procedures.
While TTE is often used to evaluate for a cardiac etiology of symptoms such as dyspnea or extremity edema, image quality can be severely hampered in patients with obesity, leading to diagnostic uncertainty [7, 15]. CT and SPECT are used to evaluate coronary artery disease but do not provide the hemodynamic information necessary for a complete evaluation of CVD. Furthermore, in patients with high BMI, CT and SPECT require higher contrast loads and radiation doses, and attenuation artifacts can be problematic [8, 9]. Given these limitations, the optimal cardiac imaging strategy in patients with severe obesity remains unclear.
Though the negative impact of severe obesity on TTE image quality is well recognized, this is less well understood for cardiac MRI, and the effect on ventricular function assessment has not been previously studied. Emerging data has demonstrated the diagnostic utility of cardiac MRI in severe obesity [16, 17]. However, there has been no direct comparison of image quality or ventricular function between severely obese and normal weight cohorts across cardiac MRI and TTE. In this study, we hypothesize that severe obesity adversely affects MRI image quality to a lesser degree than TTE. Additionally, we hypothesize that LVF and RVF agreement between TTE and MRI is worse in patients with severe obesity compared with patients with normal BMI.
Materials and methods
Study cohort and design
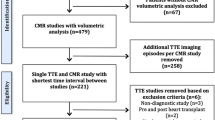
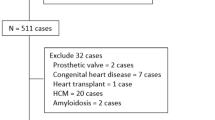
A total of 134 patients with normal BMI and 143 patients with severe obesity were consecutively screened from patients who had clinical cardiac MRI and TTE studies between July 2017 and December 2020. Exclusion criteria included: greater than 12 months between index MRI and TTE and limited TTE or MRI studies. General MRI exclusion criteria were known hypersensitivity to gadolinium-based contrast agents, glomerular filtration rate < 30 mL/min/1.73 m2, pregnancy, and hemodynamic instability. Image quality was scored and ventricular volumes were compared. Of the final cohort, no patients had a clinically reported non-diagnostic TTE or cardiac MRI. Additionally, no patients were referred for cardiac MRI with a stated indication of non-diagnostic TTE. This retrospective HIPAA-compliant study was approved by the local Institutional Review Board with waiver of informed consent (IRB #2020H062).
Image quality scoring
To compare the quality of MRI and TTE images, we developed a 31-part list of imaging categories (Figs. 1, 2) that could be applied equally to both modalities. Readers scored each parameter according to their level of confidence: parameter cannot be visualized/evaluated (Score 0); parameter can be visualized/evaluated with low (Score 1), average (Score 2), and high (Score 3) confidence, for a maximum total possible score of 93 points. Each part was designated into three commonly evaluated anatomical sections: chambers (left and right ventricles and atria), vessels (aortic segments), and valves (aortic, mitral, and tricuspid). Each section scored reader confidence in visual interpretation and quantitative measurements.
Cardiac MRI image quality assessment list. Image quality scoresheet used for cardiac MRI outlining the 31-part list of routine imaging categories. Higher scores indicate higher level of quality for a maximum total possible score of 93 points. Note the additional, separately-scored tissue characterization for MRI
Image quality assessment for TTE was performed independently by two ACC/COCATS level-III TTE (TH, BL) readers with 16 and 8 years of experience, respectively, while image quality assessment for MRI was performed independently by two different ACC/COCATS level-III cardiac MRI (MT, SR) readers each with 10 years of experience. All readers were blinded to BMI and the other modality images. The pairs of readers for each modality first reviewed and scored 20 cases (not included in the study cohort) together to develop a consensus on image quality scoring definitions.
The image quality scores for MRI and TTE were tabulated independently by each reviewer. Every raw score for each structure (e.g., aortic valve, left atrium) was averaged between the two readers for both MRI and TTE, then summed to obtain a sub-total for each category (chambers, vessels, and valves), and summed again to obtain a total image quality score. A separate image quality score was assigned to MRI tissue characterization scans (T1 and T2 mapping, LGE) that have no TTE equivalent.
To quantify the proportion of patients with a potential clinical status change between MRI and TTE, we reviewed patients with LVF < 50% by either modality for discrepancies using LVF < 50% or < 35% as these are common cutoffs for changes in clinical management. A clinical status change was defined as any cardiovascular interventions performed between each imaging modality (e.g. revascularization, arrhythmia management, cardiac arrest, initiation of guideline directed therapy) that could affect ventricular function.
Cardiovascular magnetic resonance imaging protocol
Cardiac MRI studies were performed using 1.5 T scanners with either 60 cm or 70 cm bore diameter: (MAGNETOM Avanto, Espree, Aera or Sola, Siemens Healthineers AG, Erlangen, Germany). Cardiac MRI images were acquired specific to the clinical indication following Society for Cardiovascular Magnetic Resonance recommendations [18]. All cardiac MRI studies were required to include 2-, 3-, and 4-chamber long-axis cine images, a complete short-axis cine stack, and at least one aortic or main pulmonary artery phase contrast scan without aliasing. Late gadolinium enhancement (LGE) and T1 and T2 maps were optional. No specific protocols were implemented for patients with obesity beyond standard sequence parameter modifications (i.e., larger field of view if wrap artifact present) to accommodate larger body habitus. Free-breathing real-time cine [19] was used in patients unable to breath hold. Oral benzodiazepines were administered as needed for claustrophobia. Quantitative LVF and RVF were measured by the clinical reader from contiguous short-axis cine images using validated software. LVF and RVF categorical groups were defined as follows: ejection fraction ≥ 50% = normal, 40–49% = mild, 30–39% = moderate, and ≤ 29% = severe dysfunction.
Two-dimensional transthoracic echocardiography protocol
TTE studies were acquired by experienced sonographers using any of six clinical scanners: Vivid E95 and Vivid IQ (GE Vingmed Ultrasound, Horten, Norway), Acuson Bonsai and Acuson SC2000 (Siemens Healthineers AG, Erlangen, Germany), iE33 and Epiq (Philips Medical Systems, Andover, MA). Echocardiographic studies were required to meet the criteria for a complete TTE with Doppler per current American Society of Echocardiography (ASE) recommendations [20]. LV volumes were measured by biplane Simpson method from the apical 4- and 2-chamber views following ASE recommendations [21]. Microbubble contrast agent was administered (Definity®; Lantheus, North Billerica, MA, USA) if endocardial border definition was inadequate. LVF was assessed quantitatively and categorized using the same definitions as cardiac MRI. RVF was assessed categorically by visual assessment, tricuspid annulus excursion, S' tissue Doppler, and fractional area change. The final determination of LVF and RVF was at the discretion of the clinical readers, considering available visual and quantitative metrics.
Statistical analyses
An unpaired t-test was used to compare continuous variables, while chi-square or Fisher exact test was used for proportions. Linear mixed model followed by either paired or unpaired t-tests were used to test primary and secondary hypotheses. Cohen’s kappa statistic was applied to test the agreement in LVF and RVF, defined as a patient having the same LVF or RVF categorical group for both MRI and TTE, using the following interpretation rubric: 0–0.20 = no agreement, 0.21–0.40 = fair agreement, 0.41–0.60 = moderate agreement, 0.61–0.80 = substantial agreement, and 0.81–1.00 = almost perfect agreement [22]. Wilcoxon sign rank test was used to compare MRI tissue characterization image quality between the cohorts. Polyserial correlations were used to determine the effect of time on categorical LVF and RVF differences.
Results
Clinical characteristics
Characteristics of the patients studied are shown in Table 1. After screening, the study cohort included 100 patients; 50 patients (age 54.5 ± 18.7 years; range: 22–92 years, 28 female) with normal BMI (22.2 ± 1.7 kg/m2) and 50 patients (age 47.2 ± 13.3 years; range: 20–73 years, 21 female) with severe (Class III) obesity (BMI 50.3 ± 5.9 kg/m2). Mean absolute time between MRI and TTE studies was 83.2 ± 87.8 days and was not statistically different between the cohorts (p = 0.845); 66% of the MRI and TTE pairs were within 90 days of each other. The most common indication for imaging was heart failure. The use of microbubble contrast for TTE was more frequent in the severely obese than the normal BMI cohort (64% vs 20%, p < 0.001). Mean LV ejection fraction was similar between the normal BMI and severely obese cohorts by MRI (45.5% ± 14.5% and 47.4% ± 17.6%, respectively, p = 0.558) and by TTE (46.0% ± 15.3% and 49.4% ± 16.3%, respectively, p = 0.283). The mean RV ejection fraction by cardiac MRI showed no significant difference between the normal BMI and severely obese cohorts (52% ± 11.5% and 47.8% ± 12.5%, respectively, p = 0.127). TTE similarly demonstrated no significant differences between normal BMI and severely obese cohorts in categorical RVF (p = 0.561), with 76% of patients having normal RVF.
MRI and TTE image quality score comparison between cohorts
Out of a possible 93 points, mean overall image quality score for MRI was similar between the normal BMI (91.5 ± 2.5) and severely obese (88.4 ± 5.5) cohorts; least square (LS) mean difference 3.1, p = 0.460 (Table 2, Fig. 3). Subsection MRI scores including chambers, valves, vessels, and LV and RV demonstrated similarly high and preserved image quality scores between normal BMI and severely obese cohorts (Table 2, Figs. 3, 4).
Mean overall total image quality score for TTE was significantly higher in the normal BMI cohort (64.2 ± 13.6) compared with the severely obese cohort (46.0 ± 12.9); LS mean difference 18.2, p < 0.001 (Table 2, Fig. 3). Subsection TTE scores including chambers, valves, and vessels in addition to LV and RV focused image quality subsets were all significantly lower in the severely obese cohort (Table 2, Figs. 3, 4). Differences in TTE image quality scores between the cohorts were not explained by chronic obstructive pulmonary disease status (p = 0.424).
Overall image quality was higher in MRI than TTE in the normal BMI cohort (91.5 ± 2.5 vs 64.2 ± 13.6; LS mean difference 27.4, p < 0.001), and this discrepancy was even greater in the severely obese cohort (88.4 ± 5.5 vs 46.0 ± 12.9; LS mean difference 42.4, p < 0.001). Similar findings were noted in the scoresheet subsections, and LV and RV subsets (Figs. 3, 4). The decrease in overall image quality scores observed from the normal BMI to the severely obese cohort was greater in TTE (39.6% drop) compared to MRI (3.5% drop).
Additional analysis was performed on the subset of patients who received microbubble contrast for TTE. In the normal BMI cohort, the mean overall TTE image quality score for patients not receiving contrast was not significantly different from those receiving contrast (65.7 ± 2.0 vs 58.0 ± 4.1, respectively; LS mean difference 7.8 ± 4.6, p = 0.184). In the severely obese cohort, the mean overall TTE image quality score for patients not receiving contrast was also not significantly different from those receiving contrast (50.9 ± 3.0 vs 43.2 ± 2.3, respectively; LS mean difference 7.7 ± 3.8, p = 0.093). Representative example MRI and TTE images with and without contrast demonstrating cases with both low TTE image quality scores and low MRI image quality scores can be seen in Fig. 5A and B.
A Example of low overall echocardiography image quality score. Top (left to right) – 4 chamber TTE views without, with microbubble contrast, MRI steady state free precession cine. Bottom: 2 chamber TTE views without, with microbubble contrast, MRI steady state free precession cine. Overall image quality score: TTE – 21; MRI – 91. TTE transthoracic echocardiography, MRI magnetic resonance imaging. BMI 49.2. B Example of low overall cardiac magnetic resonance image quality score. Top (left to right) – 4 chamber MRI steady state free precession cine, TTE view without, with microbubble contrast. Bottom: 2 chamber MRI steady state free precession cine, TTE view without, with microbubble contrast. Overall image quality score: MRI – 71; TTE – 43.5. TTE transthoracic echocardiography, MRI magnetic resonance imaging. BMI = 56.5
Agreement between cardiac MRI and TTE ventricular function assessment
Comparing categorical LVF assessment, there was substantial agreement between cardiac MRI and TTE for the normal BMI cohort (kappa = 0.70, p < 0.001), but only moderate agreement in the severely obese cohort (kappa = 0.53, p < 0.001). There was a higher percentage of patients in the normal BMI cohort in whom MRI and TTE LVF category matched, compared with the obese BMI cohort (80% vs 72% of MRI-TTE pairs with agreement, p < 0.001) (Table 3A, Fig. 6A). There was fair agreement between MRI and TTE in the categorical assessment of RVF for the normal BMI cohort (kappa = 0.34, p < 0.001), but there was no agreement in the severely obese cohort (kappa = 0.18, p = 0.004). There was a higher percentage of patients in whom MRI and TTE RVF category matched in the normal BMI cohort compared with the severely obese BMI cohort (72% vs 58% of MRI-TTE pairs with agreement, p < 0.001) (Table 3B, Fig. 6B). Among 53 patients with LVF < 50% determined by either or both modalities, there were 16 patients with discrepant MRI and TTE LVF around the specified < 50% or < 35% cutoffs, of which only five (9%) could possibly be explained by a clinical status change occurring between the two imaging study dates. Scatter plots of differences in LVF and RVF categories across time did not demonstrate an identifiable pattern (Supplemental Data).
MRI tissue characterization
MRI-derived myocardial T1 and T2 mapping, and LGE were performed in 70%, 66%, and 95% of patients, respectively. Median T1, T2, and LGE image quality scores were high. T1 and LGE image quality was similar between the cohorts (p = 0.289 and p = 0.090, respectively), while T2 mapping image quality scored higher in the normal BMI cohort, p = 0.030 (Table 4).
Discussion
Our objectives were to determine the effect of severe obesity on image quality for cardiac MRI and TTE, and to assess ventricular function agreement between modalities. When compared with patients with normal BMI, image quality for patients with severe obesity remained high and preserved for cardiac MRI but was negatively impacted for TTE. Furthermore, categorical agreement in LV and RV function between cardiac MRI and TTE was worse in the severely obese cohort compared with the normal weight cohort, which may lead to misdiagnosis or inappropriate treatment. These findings highlight the significance of choosing the appropriate imaging modality for clinical assessment and underscore the link between image quality, diagnostic assessment, and subsequent treatment decisions.
This study introduced a novel scoring system to evaluate and compared MRI and TTE image quality in a semi-quantitative manner. The scoring focused on criteria assessable by both modalities, such as ventricular morphology and function, excluding modality-specific criteria like myocardial fibrosis. While prior studies have examined image quality within populations [22] or modalities [23], our approach compared image quality between populations (normal BMI vs. severely obese) and across modalities (MRI vs. TTE). Image quality across all modalities can be compromised in patients with severe obesity [8, 24, 25], and while MRI and TTE are routinely used to evaluate these patients, a head-to-head comparison of the impact of severe obesity on both MRI and TTE had not been previously investigated.
Our finding that TTE image quality significantly degrades in patients with severe obesity is in agreement with previous studies [26, 27]. Increased fat mass causes signal attenuation, reducing the capacity of TTE to assess cardiac morphology, function, and flow [28, 29]. The use of microbubble contrast agent can help to maintain TTE image quality in patients with obesity, although adding to the complexity and cost of the exam [7, 15]. Ellenberger et al. recently reported echo contrast use of 23% of patients with normal BMI and 71% of patients with severe obesity, comparable to the 20% and 64% rates of contrast usage, respectively in our cohorts [30]. We found that patients receiving microbubble contrast in either normal BMI or severely obese cohorts had similar image quality scores as those not receiving contrast. Although contrast may enhance the LV endocardial border, it does not typically improve assessment of valves, vessels, or atria. As supported by Ellenberger et al. and our findings of similar TTE image quality scores with and without contrast, we speculate that microbubble contrast is often used when pre-contrast image quality is severely compromised and does not necessarily improve image quality substantially when pre-contrast quality is poor.
Consistent with the assumption that MRI is the modality least sensitive to image quality degradation caused by obesity [31], we observed no significant difference in cardiac MRI image quality between normal BMI and obese cohorts. Beyond the function and flow measurements afforded by TTE, MRI provides myocardial tissue characterization and the ability to evaluate scar, fibrosis, and edema. In our study, T1 mapping and LGE demonstrated consistent image quality between BMI cohorts, indicating feasibility regardless of body habitus. However, severe obesity poses challenges for MRI as well, including bore size and patient table weight limitations, increased burn risk caused by skin folds, and increased rates of claustrophobia [8]. Lower field, open MRI scanners have been available for some time, offering an alternative that can accommodate patients with severe obesity and/or claustrophobia. While cardiac MRI has been demonstrated on these systems [32, 33], an open magnet configuration can require compromises in overall system performance. The recent introduction of low-field MRI scanners with conventional magnet design but larger bore diameter and higher table weight limits may help expand MRI access to patients with severe obesity [34]. Additionally, low-field systems are significantly less costly to acquire, install, and operate than standard 1.5 T or 3 T scanners, and recent reports are demonstrating good cardiac image quality [35].
When examining differences between cardiac MRI and TTE imaging quality, we found that MRI image quality was superior to TTE in both normal BMI and severely obese cohorts, and this difference was more pronounced in the severely obese cohort. This observed overall image quality effect was also seen in each pre-specified subcategory (chambers, valves, and vessels), suggesting that the overall score difference was not skewed by the effect of a single subcategory. A study conducted by Kanagala et al. also found image quality differences between MRI and TTE in patients with heart failure [22]; the authors attributed this in part to the effect on TTE image quality of common comorbidities including obesity [22, 35].
Cardiac MRI is widely accepted as the reference standard for cardiac morphology and function, and we found discrepancies in MRI and TTE measures of left and right ventricular function with poorer agreement between TTE and MRI in patients with severe obesity compared with those with normal BMI. LVF was misclassified by TTE in approximately one-third of patients with severe obesity, and RVF misclassified in nearly one-half. Notably, RVF by TTE has previously demonstrated varying correlation with MRI [13, 36], and our findings also reflect this real-world variability with no agreement in RVF in patients with severe obesity. Review of the 53 patients with LVF < 50%, only 9% of these had clinical status changes (one arrest, three restoration of sinus rhythm, and one due to medical treatment of heart failure). The remaining LVF discrepancies could not be explained by interval clinical events suggesting the differences in ventricular function may be better attributable to image quality. Despite a majority of patients in both cohorts having normal cardiac function, we demonstrated a significant effect of severe obesity on categorical ventricular function assessment. We speculate that a larger cohort with abnormal cardiac function would have more dramatic observations.
Our study has several limitations. The retrospective design introduces potential referral biases, although no MRI studies were included with an indication of non-diagnostic TTE. We were unable to account for patients not referred to MRI due to claustrophobia or an inability to fit into the scanner bore, and MRI studies that were not completed due to patient discomfort or claustrophobia. Additionally, the retrospective nature of the study and non-contemporaneous scans introduce the possibility of circumstantial events between scans that could impact cardiac function and image quality. Two-thirds of patients had their MRI and TTE performed within 90 days apart, and given that the time differences between TTE and MRI were not statistically different between the normal BMI and severely obese cohorts, we expect that any potential time-related biases would have been equivalent (Supplemental Data). While our novel image quality scoring system was not previously validated, the scores confirmed the quality degradation due to severe obesity by TTE but preserved in cardiac MRI. Future prospective studies employing simultaneous MRI and TTE assessments with standardized LVF and RVF quantification methods would help mitigate any biases introduced by the time between exams.
Our cohorts comprised only normal weight and severely obese patients and did not include those falling into overweight to moderately obese categories (25 < BMI < 40). Therefore, we cannot draw any conclusions regarding MRI or TTE image quality in these intermediate groups. Finally, all MRI scans were done at 1.5 T. Cardiac MRI is also commonly performed at 3 T, which offers higher signal-to-noise ratio that can be used to increase spatial resolution or shorten scan time. However, artifacts caused by field inhomogeneity are worse at higher field, thus it is unclear how our results would translate to 3 T MRI.
In conclusion, cardiac MRI may provide more reliable diagnostic information than TTE in patients with severe obesity, suggesting cardiac MRI could be used as the first-line modality choice for CVD evaluation in this population. Cardiac MRI image quality was preserved in patients with severe obesity, whereas TTE showed a significant quality degradation in this group. Contrast-enhanced TTE did not demonstrate superior image quality compared to non-contrast exams in either patient cohort. Furthermore, there was worse agreement between MRI and TTE in the categorical assessment of LVF and RVF in patients with severe obesity. With a high and increasing prevalence of severe obesity [2], high quality and accurate imaging techniques are necessary to support best clinical practice.
Abbreviations
- ACC:
-
American College of Cardiology
- COCATS:
-
Core Cardiology Training Symposium
- CVD:
-
Cardiovascular disease
- LVF:
-
Left ventricular function
- RVF:
-
Right ventricular function
- LV:
-
Left ventricle
- RV:
-
Right ventricle
- SNR:
-
Signal–noise ratio
- OSUWMC:
-
The Ohio State University Wexner Medical Center
- LGE:
-
Late gadolinium enhancement
References
Hales CM (2020) Prevalence of obesity and severe obesity among adults: United States. 2017–2018. NCHS Data Brief. 360:1–8
Sturm R, Hattori A (2013) Morbid obesity rates continue to rise rapidly in the United States. Int J Obes (Lond) 37:889–891. https://doi.org/10.1038/ijo.2012.159
Gelber RP, Gaziano JM, Orav EJ et al (2008) Measures of obesity and cardiovascular risk among men and women. J Am Coll Cardiol 52:605–615. https://doi.org/10.1016/j.jacc.2008.03.066
Tsao CW, Aday AW, Almarzooq ZI et al (2023) Heart Disease and Stroke Statistics-2023 Update: A Report From the American Heart Association. Circulation 147:e93–e621. https://doi.org/10.1161/CIR.0000000000001123
Dong X, Strudwick M, Wang WY et al (2023) Impact of body mass index and diabetes on myocardial fat content, interstitial fibrosis and function. Int J Cardiovasc Imaging 39:379–390. https://doi.org/10.1007/s10554-022-02723-8
Carucci LR (2013) Imaging obese patients: problems and solutions. Abdom Imaging 38:630–646. https://doi.org/10.1007/s00261-012-9959-2
Finkelhor RS, Moallem M, Bahler RC (2006) Characteristics and impact of obesity on the outpatient echocardiography laboratory. Am J Cardiol 97:1082–1084. https://doi.org/10.1016/j.amjcard.2005.10.052
Uppot RN (2007) Impact of obesity on radiology. Radiol Clin North Am 45:231–246. https://doi.org/10.1016/j.rcl.2007.03.001
Wang AJ, Goldsmith ZG, Chu W et al (2013) Obesity triples the radiation dose of stone protocol computerized tomography. J Urol 189:2142–2146. https://doi.org/10.1016/j.juro.2012.12.029
Paul AH, Biykem B, David A et al (2022) AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. https://www.ahajournals.org/doi/epdf/. https://doi.org/10.1161/CIR.0000000000001063. Accessed 15 Dec 2022
Petersen SE, Aung N, Sanghvi MM et al (2017) Reference ranges for cardiac structure and function using cardiovascular magnetic resonance (CMR) in Caucasians from the UK Biobank population cohort. J Cardiovasc Magn Reson 19:18. https://doi.org/10.1186/s12968-017-0327-9
Hoffmann R, Barletta G, Von Bardeleben S et al (2014) Analysis of left ventricular volumes and function: a multicenter comparison of cardiac magnetic resonance imaging, cine ventriculography, and unenhanced and contrast-enhanced two-dimensional and three-dimensional echocardiography. J Am Soc Echocardiogr 27:292–301. https://doi.org/10.1016/j.echo.2013.12.005
Agasthi P, Chao C-J, Siegel RJ et al (2020) Comparison of echocardiographic parameters with cardiac magnetic resonance imaging in the assessment of right ventricular function. Echocardiography 37:1792–1802. https://doi.org/10.1111/echo.14877
Philip Cynthia, Rebecca Seifrie P, Peterso Gabriel et al (2021) Cardiac MRI for patients with increased cardiometabolic risk. Radiol Cardiothorac Imaging. 3(2):e200575. https://doi.org/10.1148/ryct.2021200575
Hu S-J, Liu S-X, Katus H, Luedde M (2007) The value of contrast dobutamine stress echocardiography in detecting coronary artery disease in overweight and obese patients. Can J Cardiol 23:885–889
Doeblin P, Kelle S (2021) Cardiac magnetic resonance imaging: the echo of the obese? Eur Heart J - Cardiovasc Imaging 22:528–529. https://doi.org/10.1093/ehjci/jeaa327
Ge Y, Steel K, Antiochos P et al (2021) Stress CMR in patients with obesity: insights from the Stress CMR perfusion imaging in the United States (SPINS) registry. Eur Heart J Cardiovasc Imaging 22:518–527. https://doi.org/10.1093/ehjci/jeaa281
Kramer CM, Barkhausen J, Bucciarelli-Ducci C et al (2020) Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. J Cardiovasc Magn Reson 22:17. https://doi.org/10.1186/s12968-020-00607-1
Breuer FA, Kellman P, Griswold MA, Jakob PM (2005) Dynamic autocalibrated parallel imaging using temporal GRAPPA (TGRAPPA). Magn Reson Med 53:981–985. https://doi.org/10.1002/mrm.20430
Mitchell C, Rahko PS, Blauwet LA et al (2019) Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: recommendations from the American society of echocardiography. J Am Soc Echocardiogr 32:1–64. https://doi.org/10.1016/j.echo.2018.06.004
McHugh ML (2012) Interrater reliability: the kappa statistic. Biochem Med 22(3):276–282. https://doi.org/10.11613/BM.2012.031
Kanagala P, Cheng ASH, Singh A et al (2018) Diagnostic and prognostic utility of cardiovascular magnetic resonance imaging in heart failure with preserved ejection fraction – implications for clinical trials. J Cardiovasc Magn Reson 20:4. https://doi.org/10.1186/s12968-017-0424-9
Klinke V, Muzzarelli S, Lauriers N et al (2013) Quality assessment of cardiovascular magnetic resonance in the setting of the European CMR registry: description and validation of standardized criteria. J Cardiovasc Magn Reson 15:55. https://doi.org/10.1186/1532-429X-15-55
Lim SP, Arasaratnam P, Chow BJ et al (2015) Obesity and the challenges of noninvasive imaging for the detection of coronary artery disease. Can J Cardiol 31:223–226. https://doi.org/10.1016/j.cjca.2014.12.003
Uppot RN (2018) Technical challenges of imaging & image-guided interventions in obese patients. Br J Radiol 91:20170931. https://doi.org/10.1259/bjr.20170931
Mathew B, Francis L, Kayalar A, Cone J (2008) Obesity: effects on cardiovascular disease and its diagnosis. J Am Board Fam Med 21:562–568. https://doi.org/10.3122/jabfm.2008.06.080080
Kosmala W, Wong C, Kuliczkowska J et al (2008) Use of body weight and insulin resistance to select obese patients for echocardiographic assessment of subclinical left ventricular dysfunction. Am J Cardiol 101:1334–1340. https://doi.org/10.1016/j.amjcard.2007.12.034
Gaudieri V, Nappi C, Acampa W et al (2017) Assessment of cardiovascular impairment in obese patients: limitations and troubleshooting of available imaging tools. Revista Española de Medicina Nuclear e Imagen Molecular 36:247–253. https://doi.org/10.1016/j.remn.2017.01.010
Cortez RM, Okoshi MP, Okoshi K (2022) A review of the roles and limitations of noninvasive imaging methods for investigating cardiovascular disease in individuals with obesity. Med Sci Monit 30(28):e937362. https://doi.org/10.12659/MSM.937362
Ellenberger K, Jeyaprakash P, Sivapathan S et al (2022) The effect of obesity on echocardiographic image quality. Heart Lung Circ 31:207–215. https://doi.org/10.1016/j.hlc.2021.06.525
Alì M, Monti CB, Gold B et al (2020) Open 1.0-T versus closed 1.5-T cardiac MR: image quality assessment. Clin Imaging 68:102–107. https://doi.org/10.1016/j.clinimag.2020.06.019
Klein H-M, Meyners W, Neeb B et al (2007) Cardiac magnetic resonance imaging using an open 0.35 T system. J Comput Assist Tomogr 31(3):430–434. https://doi.org/10.1097/01.rct.0000238010.64931.c6
Campbell-Washburn AE, Varghese J, Nayak KS et al (2024) Cardiac MRI at low field strengths. J Magn Reson Imaging 59:412–430. https://doi.org/10.1002/jmri.28890
Varghese J, Jin N, Giese D et al (2023) Building a comprehensive cardiovascular magnetic resonance exam on a commercial 0.55 T system: a pictorial essay on potential applications. Front Cardiovasc Med 1(10):e1120982
Alpert MA, Lavie CJ, Agrawal H et al (2014) Obesity and heart failure: epidemiology, pathophysiology, clinical manifestations, and management. Transl Res 164:345–356. https://doi.org/10.1016/j.trsl.2014.04.010
Anavekar NS, Gerson D, Skali H et al (2007) Two-dimensional assessment of right ventricular function: an echocardiographic-MRI correlative study. Echocardiography 24:452–456. https://doi.org/10.1111/j.1540-8175.2007.00424.x
Acknowledgements
HN for his statistical assistance with study design and manuscript review. DS for her assistance with regulatory approvals and retrospective enrollment of patients.
Funding
This work is funded by National Heart, Lung, and Blood Institute (R01HL161618).
Author information
Authors and Affiliations
Contributions
AGl, CC, OS, and MT contributed to study conception and design. Data collection was performed by AG, MT, BL, TH, and SR. Data analysis and statistics were completed by AG, CC, and VY. Manuscript and figure preparation was completed by AG, CC, VY, OS, and MT. All manuscript drafts and versions, including this draft, were read and approved by all authors.
Corresponding author
Ethics declarations
Conflict of interest
None of the co-authors have any financial associations that might pose a conflict of interest in connection with the submitted article. Dr. Orlando Simonetti receives institutional research support Siemens Medical Solutions; Siemens was not involved in the collection of data or preparation of this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Goyal, A., Crabtree, C.D., Lee, B.C. et al. The impact of severe obesity on image quality and ventricular function assessment in echocardiography and cardiac MRI. Int J Cardiovasc Imaging 40, 1081–1094 (2024). https://doi.org/10.1007/s10554-024-03078-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-024-03078-y