Abstract
The presence of left main coronary artery disease (LMCAD) is associated with an unfavorable clinical outcome. The clinical utility of FFRCT testing for non-invasive physiological assessment in LMCAD remains largely unknown. In this single center observational study LMCAD patients were retrospectively identified between November 2015 and December 2017. We evaluated the relationship between LMCAD diameter stenosis and downstream FFRCT values, and the clinical consequences following FFRCT testing in patients with LMCAD. The composite endpoint (all-cause death, myocardial infarction, unplanned revascularization) was determined over a median follow-up of 1.1 years. LMCAD was registered in 432 of 3202 (13%) patients having coronary CTA. FFRCT was prescribed in 213 (49%), while 59 (14%) patients were referred directly to invasive angiography or myocardial perfusion imaging. FFRCT was performed in 195 (45%) patients. LM stenosis severity was inversely related to downstream FFRCT values. In patients with simple LMCAD with stenosis ≥ 50%, > 80% had FFRCT > 0.80 in non-diseased proximal and downstream segments (n = 7). No patients with simple LMCAD and FFRCT > 0.80 (n = 20) suffered an adverse clinical outcome. FFRCT testing in patients with LMCAD is feasible. LM stenosis severity is inversely related to FFRCT value. Patients with LMCAD and FFRCT > 0.80 have favorable clinical outcomes at short-term follow-up. Large-scale studies assessing the clinical utility and safety of deferring invasive catheterization following FFRCT testing in patients with LMCAD are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
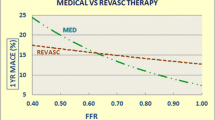
Left main coronary artery disease (LMCAD) is present in 4–7% of patients undergoing invasive coronary angiography (ICA) [1,2,3]. Since the presence of LMCAD with stenosis > 50% is associated with unfavorable clinical outcomes, characterization of the left main (LM) anatomy is crucial [4]. Several studies support the use of fractional flow reserve (FFR) to assess the hemodynamic consequences of LMCAD [5,6,7,8]. Coronary computed tomography angiography (CTA) is increasingly used as the first line test in patients with suspected coronary artery disease (CAD) [9, 10]. However, as for ICA, CTA findings are often discordant with lesion-specific ischemia as determined by FFR, which currently remains the gold standard for decision-making during ICA [11]. CT-derived FFR (FFRCT) has emerged as a test with high diagnostic performance and correlation when compared with measured FFR [11, 12] and as a valuable gatekeeper to the catherization laboratory in patients with stable CAD [13, 14]. Recently, it has been demonstrated that FFRCT is effective in differentiating patients with stenosis who do not require further downstream testing or intervention (FFRCT > 0.80) from higher risk patients in whom further testing and intervention should be considered (FFRCT ≤ 0.80) [15,16,17]. However, the association between LMCAD and a normal FFRCT result has not previously been explored. Thus, the purpose of this study of patients with stable chest pain was two-fold: 1. to describe the relationship between LMCAD and FFRCT and 2. to evaluate the clinical utility of FFRCT in patients with LMCAD.
Materials and methods
This single-center, observational all-comer study included patients with LMCAD determined by CTA between November 2015 and December 2017 at Aarhus University Hospital, Denmark. The strategy of CTA as first line testing in symptomatic patients with suspected coronary artery disease (CAD) in this institution has previously been described [14, 15, 18, 19]. In brief, CTA testing is the preferred diagnostic test strategy in patients with non-emergent chest pain and no known CAD such as previous revascularization. FFRCT testing is recommended in patients with one or more lesions of moderate stenosis severity (30 to 70%) before decision-making on downstream management. Direct referral to ICA is generally recommended in patients with high risk anatomy including significant LMCAD, high grade proximal left anterior descending coronary artery (LAD) stenosis, and/or 3-vessel disease in this institution. However, other factors than test results (e.g. clinical presentation, patient preferences, and lesion characteristics) are also considered, when deciding the post-CTA patient management strategy [15]. Therefore, ICA may be deferred in some patients with “high-risk” anatomic features.
Data sources
Data were retrieved from 3 regional or national registries: 1. the Western Denmark Cardiac Computed Tomography Registry, containing information on the testing indication, patient demographics, CT acquisition characteristics, and CT test results [9], 2. the Danish National Patient Registry providing information on diagnoses, test utilization, and procedures from every hospitalization and outpatient clinical visits [9], and 3. the Civil Registration System, which contains complete data on mortality [9]. The study was approved by the Danish Data Protection Agency (1-16-02-110-17) with a waiver for individual informed consent by the regional ethical committee.
Coronary CTA
Coronary CTA was performed using dual source scanners (Siemens Definition Flash or Siemens Definition Force, Siemens, Forchheim, Germany) as previously described [14, 15, 18, 19]. In brief, scans were performed according to best CTA acquisition practice guidelines [20]. Oral and/or intravenous beta-blockers or oral ivabradine were administered if necessary, targeting a heart rate < 60 beats/minute. Sublingual spray nitroglycerin 0.8 mg 3 to 5 min before the scan was administered in all patients. An initial non-enhanced high-pitch spiral acquisition scan was performed for assessment of the Agatston score. Coronary CTA acquisition was performed using prospective electrocardiographic triggering. In case of a heart rate of < 65 beats/min a RR scan interval of 65 to 75% was applied and in case of a heart rate of ≥ 65 beats/min the RR acquisition window was widened to 40 to 70%. Vessels with a diameter ≥ 1.8 mm were evaluated for lumen narrowing. Coronary stenosis severity was categorized into four groups: 1–24%, 25–49%, 50–69%, and 70–99%. Stenosis severity ≥ 50% was definded as significant. Stenosis location was defined as proximal or distal as previously described [21]. Patients without a LM (separate ostia), and those with LM or proximal vessel occlusion were not included in this study. Cardiologists with a mean CTA interpretation experience of 7 years performed the readings.
CTA-derived fractional flow reserve
The science behind FFRCT has previously been described in detail [22]. Standard CTA datasets were transferred for off-site analysis as previously described (HeartFlow, Redwood City, California, US) [11]. A 3D FFRCT model provides computed FFR values in all segments with a lumen diameter > 1.8 mm. A lesion with an FFRCT value ≤ 0.80 was categorized as hemodynamically significant. From November 2015, a 3D interactive FFRCT model was available providing FFRCT values at all points of the coronary tree.
LMCAD assessment
In patients with simple LMCAD (isolated LM lumen diameter reduction between 1 and 99% with no ≥ 50% stenosis in the left major arteries), absolute FFRCT values were registered, 1. distally in the LM just proximal to the bifurcation when the distal border of the lesion was located ≥ 5 mm from the bifurcation, 2. in the proximal LAD and left circumflex artery (LCx) 1–2 cm distal from the bifurcation, and 3. in the distal LAD and distal LCx segments (Fig. 1). The first diagonal branch, and first obtuse marginal branch were used as delineators between proximal and non-proximal LAD and LCx segments, respectively. Distal FFRCT values were assessed in the most distal LAD and LCx segments (with lumen diameter > 1.8 mm). In patients with complex LMCAD (LMCAD with one or more significant ≥ 50% stenosis in non-LM coronary arteries), downstream FFRCT was registered only in segments without stenosis ≥ 50%. In patients with stenosis ≥ 50% in the proximal part of LAD or LCx, FFRCT was only registered in the non-diseased vessel. An increase of the FFRCT value ≥ 0.03 in mid-proximal relative to more the value in the LM was defined as pressure recovery. Patients with at least one severe lesion with FFRCT < 0.65 in either the proximal LAD or proximal LCx were excluded from the analysis, because FFR < 0.65 in lesions located in proximal segments may influence the reliability of the FFR assessment of the LM [6, 7].
FFRCT reading strategy. Examples of patients with simple (A) or complex (B) left main coronary artery disease (LMCAD). FFRCT was registered 1. distally in the LM 2. in the proximal left anterior descending (LAD) and left circumflex artery (LCX) segments, and 3. distal segments. The first diagonal branch and first obtuse branch delineated proximal and non-proximal segments. Distal values were assessed in the most distal segments with lumen diameter > 1.8 mm. In patients with simple LMCAD (A) FFRCT was registered in all segments 1–3. In patients with complex LMCAD (B) downstream FFRCT were registered only in non-stenotic arteries. Thus, FFRCT values in example B were registered only in the distal LM, and proximal and mid LCX segments. Left: Coronary CT angiography curved multiplanar reconstructions. Right: Three-dimensional FFRCT model. The red arrows indicate the location of LMCAD. The yellow arrow denotes a proximal 60% diameter stenosis in the LAD
Clinical endpoint and follow-up
We used a composite endpoint comprising all-cause death, myocardial infarction, and unplanned revascularization. Unplanned revascularization was defined as a procedure performed during an ICA which was not scheduled in the immediate post-CTA FFRCT testing management plan. Follow-up began at the time of the CT scan and continued until the clinical event or end of the study period, June 18, 2018. There was no loss to follow-up during the study period.
Statistics
Categorical variables were described by counts and percentages. Groups were compared using Fisher´s exact test. Continuous variables were described using mean ± standard deviation (SD) or median (interquartile range, range) as appropriate. Means were compared between the groups using the Student’s t-test with unequal variance and medians were compared using Mann–Whitney U test. Means and medians between more than two groups were compared using the Kruskal–Wallis test. A p value ≤ 0.05 was considered statistically significant. The endpoint analysis was estimated using the Kaplan Meier method. All analysis were performed using SPSS version 25 (SPSS Inc; Chicago, IL, US).
Results
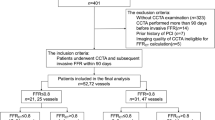
During the study period, coronary CTA was performed in 3202 patients. LMCAD was registered in 432 (13%) patients (Fig. 2). Post-coronary CTA direct referral to ICA or myocardial perfusion imaging (MPI) was planned in 59 (14%) patients. Of the remaining patients, FFRCT was prescribed in 213 (49%) patients, while in 160 (37%) patients no additional downstream testing was planned. A conclusive FFRCT result was available in 201 (94%) patients. Coronary CTA image quality was inadequate for FFRCT analysis in 9 (4%) patients, LM was absent in 3 patients, while in 6 patients the FFRCT value of the proximal LAD or LCx was < 0.65 (Fig. 2). Therefore, 195 (45%) patients with available FFRCT results comprised the basis of this report. Baseline patient characteristics are presented in Table 1. Mean (SD) age was 64 (± 10) years, and 62% were men. Patients in the FFRCT group had a higher clinical risk score (Updated Diamond-Forrester, 51% vs. 39%, p < 0.001), and more frequently had typical angina (58% vs. 15%, p < 0.001) than patients in whom FFRCT was not prescribed. Baseline anatomical characteristics of study patients are presented in Table 2. Patients in the FFRCT group had higher median Agatston scores than those in the no FFRCT group (351 vs. 47, p < 0.001), but lower than the group of patients who were referred directly to ICA or myocardial perfusion imaging (351 vs 535, p = 0.009). Coronary CTA acquisition characteristics are presented in Table S1.
Flow chart of study patients. CTA computed tomography angiography, LMCAD left main coronary artery disease, ICA invasive coronary angiography, MPI myocardial perfusion imaging, FFRCT coronary CTA-derived fractional flow reserve, LM left main coronary artery, prox. Proximal, LAD left anterior descending artery, LCx left circumflex artery. *Patients with 3-vessel disease. In patients with LMCAD stenosis ≥ 50%, 9 had 3-vessel disease
Relationship between left main anatomy and downstream physiology
In patients undergoing FFRCT testing, maximum LM stenosis ranged between 1–24%, 25–49%, 50–69% and 70–99% in 53%, 37%, 9% and 1%, respectively. FFRCT values in the distal LM, proximal LAD, proximal LCx, distal LAD and distal LCx decreased with increasing LM stenosis severity (Table 3).
In patients with simple LMCAD (n = 21) and complex LMCAD (n = 174) FFRCT values were significantly lower in the group with LM stenosis ≥ 50% versus those without stenosis (Table S2). Yet FFRCT in the LM was > 0.80 in 95% (18/19) of the patients with maximum LM stenosis ≥ 50%, including 7 (39%) with simple LMCAD and 11 (61%) with complex LMCAD, respectively. The proportion of patients with maximum LM stenosis ≥ 50%, and FFRCT > 0.80 decreased to 82% (9/11) when FFRCT was assessed in non-diseased proximal LAD and LCx segments. The number of patients with a significant FFRCT value was highest in the distal segments (Table S3).
In 3 (2%) patients pressure recovery was identified; downstream FFRCT values > 0.80 in all. One such case is presented in Fig. 3.
Pressure recovery phenomenon. Typically, pressure will reach a minimum in the throat of stenosis with slight pressure recovery 0.5–1 cm distal to the stenosis because of the increase in the cross-sectional area of the vessel and then decrease further downstream the vessel due to the continuous decrease in the cross-sectional area of the vessel and possibly the presence of flow limiting artery disease in more distal segments. However, FFRCT values may transiently rise also in segments located more distal to stenosis. In this case, the step-up in FFRCT from 0.92 distally in the left main (LM) to 0.95 in the mid left anterior descending artery (LAD) is caused by the presence of post-stenotic vessel dilatation resulting in reduced flow velocity and pressure recovery. We defined significant pressure recovery as an increase in FFRCT ≥ 0.03 when moving from the lesion-specific FFRCT "reading point" (typically 1–2 cm distal to the lower border of the stenosis) to more distal located segments. Coronary CT angiography curved multiplanar reconstructions. Right: Three-dimensional FFRCT model. Red arrow indicates the location of LMCAD. LCX left circumflex artery
Clinical outcomes
The risk of the composite endpoint during follow-up was 5% (Table 4). There was a numerically but not statistically significant difference in the risk of the composite endpoint when comparing the FFRCT and no FFRCT groups (5% versus 1%, p = 0.15) as shown in Table S4.
The risk of the composite endpoint, the number of ICA and of revascularization procedures in patients with simple or complex LMCAD based on the LM FFRCT values are presented in Table 4. There were no events in patients with simple LMCAD, of whom 7 of 8 with LM stenosis ≥ 50% had FFRCT > 0.80. The number of ICAs and revascularizations according to the anatomical findings and FFRCT results in patients with simple LMCAD are shown in Fig. S1. Patients with simple LMCAD with stenosis ≥ 50% having ICAs or revascularizations performed were more likely to have numerically lower FFRCT values than those without ICA or revascularization.
In a subanalysis including the total FFRCT cohort and distal FFRCT values the risk of composite endpoint was 6% (7/126) vs. 3% (2/69) in patients with distal FFRCT value ≤ 0.80 and FFRCT value > 0.80, respectively (p = 0.09) (Table S5 and Fig. S2).
Discussion
In this study of consecutive symptomatic patients undergoing first line coronary CTA, LM stenosis severity was inversely related to FFRCT values irrespective of the reading point i.e. in the distal LM, or the proximal or distal LAD or LCx segments. In patients with simple LMCAD and stenosis ≥ 50%, more than 80% had FFRCT > 0.80 in non-diseased proximal and distal LAD and/or LCx segments. FFRCT > 0.80 in patients with LMCAD was associated with favorable clinical outcomes.
Left main artery stenosis is associated with unfavorable outcomes. Therefore, societal guidelines emphasize the importance of revascularization of LM stenosis [23]. Although, FFR represents the gold standard for decision-making in the catherization laboratory, guidelines recommend that in the event of significant LM disease that treatment decision-making is guided by intravascular ultrasound (IVUS) or optical coherence tomography (OCT) (IIa recommendation level) [23].
Patients with significant LMCAD were excluded from the FAME trials [24, 25], however preliminary data indicate that long-term outcome is more favorable in patients undergoing FFR than pure angiographically guided LM revascularization [8]. Assessing LM disease based on angiography or physiology is challenging due to the short length, catheter damping [26] and overlap of downstream vessels [27]. Moreover, downstream disease in the proximal LAD or LCx may influence the FFR values over LM stenosis potentially leading to false negative results [7, 28]. Accordingly, it has been demonstrated that FFR < 0.65 in lesions located in the proximal segments may influence the reliability of FFR assessment of LMCAD [6, 7].
Coronary CTA is increasingly used as the first line test in patients suspected of stable CAD, a strategy which is supported by guidelines [10]. Recently, the evidence for FFRCT has expanded beyond diagnostic validation [11, 12] by facilitating less referrals to ICA and less findings of non-obstructive disease in patients with moderate CAD [13,14,15]. Moreover, it has recently been demonstrated that patients with intermediate stenosis and FFRCT > 0.80 have favorable clinical outcomes without the need of further testing [15,16,17]. However, no previous study has investigated the potential clinical utility of FFRCT in patients with LMCAD. In this institution, patients with significant LM stenosis by coronary CTA are categorized as high risk and therefore per institutional practice it is recommended that such patients are referred directly to ICA, while in patients with non-obstructive LMCAD FFRCT may be used for non-invasive hemodynamically adjudication. However, other circumstances than LM stenosis severity may have influenced downstream clinical decision-making in these patients, such as symptoms, other lesion anatomical characteristics, and patient preferences. Therefore, in this study FFRCT was used as an adjunctive test before decision-making on downstream management even in some patients with simple LM stenosis. In some of these patients, ICA was deferred based on a normal FFRCT result.
While FFR interrogation for assessment of LMCAD is performed in the proximal LAD and LCx segments [5] in this study, we also registered, FFRCT values in the distal LM. In accordance with previous findings we found that FFRCT values were inversely associated with LM stenosis severity [15]. Moreover, FFRCT values were lower in distal than in proximal segments reflecting the fact that FFRCT is the sum of multiple downstream resistances from discrete lesions or diffuse disease. One striking finding was the low proportion of FFRCT positivity in significant LM stenosis, even among those with simple LMCAD with stenosis ≥ 50%. In patients with simple LMCAD and stenosis ≥ 50% only 13% and 13% demonstrated FFRCT ≤ 0.80 when assessed distally in the LM or in proximal LAD and LCx segments. In comparison, in another real-world report from this institution, the proportion of stable patients with stenosis ≥ 50% in proximal segments and FFRCT ≤ 0.80 was 48% [15]. In a previous study assessing LMCAD physiology, it was demonstrated that significant stenosis or lesions in the downstream vessels may result in overestimation of FFR values [28]. However, since the low proportion of FFRCT positivity was present even in the event of minimal or absent downstream disease other mechanisms most likely play a role. The short length of the LM may potentially influence the atherosclerotic plaque formation and reliability of diameter stenosis assessment [29]. Rheological factors in very proximal LM stenosis may also play a role. At the entry of the left coronary system the blood flow is turbulent and pressure losses reduced compared to segments with laminar flow [29]. These findings need further delineation in future studies.
In contrast to FFR, which measures pressure at the location of the pressure wire, FFRCT values are available everywhere in the coronary tree. Thus, unlike invasive FFR, FFRCT may potentially be assessed in the LM stem. However, due to the short length of the LM it may be difficult in the majority of patients to obtain the value 10–20 mm distal to the lower border of stenosis, which is the location recommended for management actions [30]. A shorter distance between the lesion and the FFRCT reading point may potentially lead to more cases with pressure recovery which typically occurs just distal to a stenosis due to the increase in the cross-sectional area and corresponding loss in flow velocity (Bernoulli’s principle) and then decreases again due to the continuous decrease in vessel area and/or downstream disease. The phenomenon was infrequently seen in this dataset, and thus could not explain the high number of FFRCT > 0.80 in patients with LM stenosis ≥ 50%.
Importantly, outcomes were favorable in patients with simple LMCAD and FFRCT ≥ 0.80. However, these findings are exploratory only and thus need confirmation in future studies. Overall, the proportion of patients with an adverse cardiac event during short-term follow-up was low. Notably, all adverse events occurred in patients with complex LMCAD. More studies are needed to assess the clinical utility of FFRCT in patients with LMCAD including exploration of the safety of deferring ICA in those with FFRCT > 0.80 as well as assessing the value of FFRCT ≤ 0.80 for decision-making on ICA and revascularization.
LM disease has traditionally required invasive angiography with or without FFR for determination of revascularization. CTA has up till now been deemed unable to adequately assess patients with LM disease. Potentially, the inherent risk of periinterventional complications in LMCAD patients may be reduced if safety of CTA-FFRCT assessment for deferral of ICA in this setting can be confirmed in larger studies. This is a first description of the feasibility and clinical outcomes of FFRCT use in patients with LM disease. The present data are in accordance with recent data demonstrating the promise of extension of CTA use in more complex lesion subsets, and in those which had been previously deemed inappropriate or impossible for CTA testing [31, 32].
Study limitations
This is a single-center study with inherent limitations such as selection bias and possibly lack of generalizability of results. The number of patients with LM stenosis ≥ 50% was limited. However, the present study included an all-comer consecutive cohort of symptomatic patients, and thus is representative of patients encountered in clinical practice. In this study individual CT cardiologists prescribed FFRCT or ICA according to a varying degree of integrating test preferences and thresholds. We have no further information about reasons for sending some patients directly to ICA and not to FFRCT testing and vice versa. The proportion of patients with significant LMCAD or adverse clinical outcomes was low. Information of angina would have been valuable. Studies with more patients and longer follow-up are needed to confirm the present findings.
Conclusions
FFRCT testing in patients with LMCAD is feasible. LM stenosis severity is inversely related to downstream FFRCT values. Patients with LMCAD and FFRCT > 0.80 have favorable clinical outcomes at short-term follow-up. More studies assessing the clinical utility and safety of FFRCT testing in patients with LMCAD are warranted.
Data availability
The study data supporting the manuscript are available from the corresponding author upon approval of a reasonable request.
Code availability
Not applicable.
References
Cohen MV, Gorlin R (1975) Main left coronary artery disease. Clinical experience from 1964–1974. Circulation 52(2):275–85
Noto TJ Jr, Johnson LW, Krone R, Weaver WF, Clark DA, Kramer JR Jr, Vetrovec GW (1991) Cardiac catheterization 1990: a report of the Registry of the Society for Cardiac Angiography and Interventions (SCA&I). Cathet Cardiovasc Diagn 24(2):75–83
Fajadet J, Chieffo A (2012) Current management of left main coronary artery disease. Eur Heart J 33(1):36–50b
Yusuf S, Zucker D, Peduzzi P, Fisher LD, Takaro T, Kennedy JW, Davis K, Killip T, Passamani E, Norris R et al (1994) Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the Coronary Artery Bypass Graft Surgery Trialists Collaboration. Lancet 344(8922):563–570
Hamilos M, Muller O, Cuisset T, Ntalianis A, Chlouverakis G, Sarno G, Nelis O, Bartunek J, Vanderheyden M, Wyffels E, Barbato E, Heyndrickx GR, Wijns W, De Bruyne B (2009) Long-term clinical outcome after fractional flow reserve-guided treatment in patients with angiographically equivocal left main coronary artery stenosis. Circulation 120(15):1505–1512
Daniels DV, van’t Veer M, Pijls NH, van der Horst A, Yong AS, De Bruyne B, Fearon WF (2012) The impact of downstream coronary stenoses on fractional flow reserve assessment of intermediate left main disease. JACC Cardiovasc Interv 5(10):1021–1025
Fearon WF, Yong AS, Lenders G, Toth GG, Dao C, Daniels DV, Pijls NHJ, De Bruyne B (2015) The impact of downstream coronary stenosis on fractional flow reserve assessment of intermediate left main coronary artery disease: human validation. JACC Cardiovasc Interv 8(3):398–403
Mallidi J, Atreya AR, Cook J, Garb J, Jeremias A, Klein LW, Lotfi A (2015) Long-term outcomes following fractional flow reserve-guided treatment of angiographically ambiguous left main coronary artery disease: a meta-analysis of prospective cohort studies. Catheter Cardiovasc Interv 86(1):12–18
Nielsen LH, Botker HE, Sorensen HT, Schmidt M, Pedersen L, Sand NP, Jensen JM, Steffensen FH, Tilsted HH, Bottcher M, Diederichsen A, Lambrechtsen J, Kristensen LD, Ovrehus KA, Mickley H, Munkholm H, Gotzsche O, Husain M, Knudsen LL, Norgaard BL (2017) Prognostic assessment of stable coronary artery disease as determined by coronary computed tomography angiography: a Danish multicentre cohort study. Eur Heart J 38(6):413–421
Moss AJ, Williams MC, Newby DE, Nicol ED (2017) The updated NICE guidelines: cardiac CT as the first-line test for coronary artery disease. Curr Cardiovasc Imaging Rep 10(5):15
Norgaard BL, Leipsic J, Gaur S, Seneviratne S, Ko BS, Ito H, Jensen JM, Mauri L, De Bruyne B, Bezerra H, Osawa K, Marwan M, Naber C, Erglis A, Park SJ, Christiansen EH, Kaltoft A, Lassen JF, Botker HE, Achenbach S (2014) Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (analysis of coronary blood flow using CT angiography: next steps). J Am Coll Cardiol 63(12):1145–1155
Driessen RS, Danad I, Stuijfzand WJ, Raijmakers PG, Schumacher SP, van Diemen PA, Leipsic JA, Knuuti J, Underwood SR, van de Ven PM, van Rossum AC, Taylor CA, Knaapen P (2019) Comparison of coronary computed tomography angiography, fractional flow reserve, and perfusion imaging for ischemia diagnosis. J Am Coll Cardiol 73(2):161–173
Douglas PS, Pontone G, Hlatky MA, Patel MR, Norgaard BL, Byrne RA, Curzen N, Purcell I, Gutberlet M, Rioufol G, Hink U, Schuchlenz HW, Feuchtner G, Gilard M, Andreini D, Jensen JM, Hadamitzky M, Chiswell K, Cyr D, Wilk A, Wang F, Rogers C, De Bruyne B (2015) Clinical outcomes of fractional flow reserve by computed tomographic angiography-guided diagnostic strategies vs. usual care in patients with suspected coronary artery disease: the prospective longitudinal trial of FFR(CT): outcome and resource impacts study. Eur Heart J 36(47): 3359–3367.
Jensen JM, Botker HE, Mathiassen ON, Grove EL, Ovrehus KA, Pedersen KB, Terkelsen CJ, Christiansen EH, Maeng M, Leipsic J, Kaltoft A, Jakobsen L, Sorensen JT, Thim T, Kristensen SD, Krusell LR, Norgaard BL (2018) Computed tomography derived fractional flow reserve testing in stable patients with typical angina pectoris: influence on downstream rate of invasive coronary angiography. Eur Heart J Cardiovasc Imaging 19(4):405–414
Norgaard BL, Terkelsen CJ, Mathiassen ON, Grove EL, Botker HE, Parner E, Leipsic J, Steffensen FH, Riis AH, Pedersen K, Christiansen EH, Maeng M, Krusell LR, Kristensen SD, Eftekhari A, Jakobsen L, Jensen JM (2018) Coronary CT angiographic and flow reserve-guided management of patients with stable ischemic heart disease. J Am Coll Cardiol 72(18):2123–2134
Patel MR, Nørgaard BL, Fairbairn TA, Nieman K, Akasaka T, Berman DS, Raff GL, Hurwitz Koweek LM, Pontone G, Kawasaki T, Sand NPR, Jensen JM, Amano T, Poon M, Øvrehus KA, Sonck J, Rabbat MG, Mullen S, De Bruyne B, Rogers C, Matsuo H, Bax JJ, Leipsic J (2020) 1-year impact on medical practice and clinical outcomes of FFR(CT): the ADVANCE registry. JACC Cardiovasc Imaging 13(1 Pt 1):97–105
Ihdayhid AR, Norgaard BL, Gaur S, Leipsic J, Nerlekar N, Osawa K, Miyoshi T, Jensen JM, Kimura T, Shiomi H, Erglis A, Jegere S, Oldroyd KG, Botker HE, Seneviratne SK, Achenbach S, Ko BS (2019) Prognostic value and risk continuum of noninvasive fractional flow reserve derived from coronary CT angiography. Radiology 292(2):343–351
Norgaard BL, Gormsen LC, Botker HE, Parner E, Nielsen LH, Mathiassen ON, Grove EL, Ovrehus KA, Gaur S, Leipsic J, Pedersen K, Terkelsen CJ, Christiansen EH, Kaltoft A, Maeng M, Kristensen SD, Krusell LR, Lassen JF, Jensen JM (2017) Myocardial perfusion imaging versus computed tomography angiography-derived fractional flow reserve testing in stable patients with intermediate-range coronary lesions: influence on downstream diagnostic workflows and invasive angiography findings. J Am Heart Assoc. https://doi.org/10.1161/jaha.117.005587
Norgaard BL, Hjort J, Gaur S, Hansson N, Botker HE, Leipsic J, Mathiassen ON, Grove EL, Pedersen K, Christiansen EH, Kaltoft A, Gormsen LC, Maeng M, Terkelsen CJ, Kristensen SD, Krusell LR, Jensen JM (2017) Clinical use of coronary CTA-derived FFR for decision-making in stable CAD. JACC Cardiovasc Imaging 10(5):541–550
Abbara S, Blanke P, Maroules CD, Cheezum M, Choi AD, Han BK, Marwan M, Naoum C, Norgaard BL, Rubinshtein R, Schoenhagen P, Villines T, Leipsic J (2016) SCCT guidelines for the performance and acquisition of coronary computed tomographic angiography: a report of the society of Cardiovascular Computed Tomography Guidelines Committee: Endorsed by the North American Society for Cardiovascular Imaging (NASCI). J Cardiovasc Comput Tomogr 10(6):435–449
Adjedj J, De Bruyne B, Flore V, Di Gioia G, Ferrara A, Pellicano M, Toth GG, Bartunek J, Vanderheyden M, Heyndrickx GR, Wijns W, Barbato E (2016) Significance of intermediate values of fractional flow reserve in patients with coronary artery disease. Circulation 133(5):502–508
Taylor CA, Fonte TA, Min JK (2013) Computational fluid dynamics applied to cardiac computed tomography for noninvasive quantification of fractional flow reserve: scientific basis. J Am Coll Cardiol 61(22):2233–2241
Neumann F-J, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet J-P, Falk V, Head SJ, Jüni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO, Group ESCSD (2019) 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J 40(2):87–165
Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van’ t Veer M, Klauss V, Manoharan G, Engstrom T, Oldroyd KG, Ver Lee PN, MacCarthy PA, Fearon WF (2009) Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 360(3):213–224
De Bruyne B, Pijls NH, Kalesan B, Barbato E, Tonino PA, Piroth Z, Jagic N, Mobius-Winkler S, Rioufol G, Witt N, Kala P, MacCarthy P, Engstrom T, Oldroyd KG, Mavromatis K, Manoharan G, Verlee P, Frobert O, Curzen N, Johnson JB, Juni P, Fearon WF (2012) Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 367(11):991–1001
Pellicano M, Ciccarelli G, Xaplanteris P, Gioia GD, Milkas A, Colaiori I, Heyse A, Durme FV, Vanderheyden M, Bartunek J, Bruyne BD, Barbato E (2020) DISENGAGE registry. Circulation 13(11):8640. https://doi.org/10.1161/CIRCINTERVENTIONS.119.008640
Puri R, Kapadia SR, Nicholls SJ, Harvey JE, Kataoka Y, Tuzcu EM (2012) Optimizing outcomes during left main percutaneous coronary intervention with intravascular ultrasound and fractional flow reserve: the current state of evidence. JACC Cardiovasc Interven 5(7):697–707
Yong AS, Daniels D, De Bruyne B, Kim HS, Ikeno F, Lyons J, Pijls NH, Fearon WF (2013) Fractional flow reserve assessment of left main stenosis in the presence of downstream coronary stenoses. Circ Cardiovasc Interv 6(2):161–165
Maehara A, Mintz GS, Castagna MT, Pichard AD, Satler LF, Waksman R, Laird JR Jr, Suddath WO, Kent KM, Weissman NJ (2001) Intravascular ultrasound assessment of the stenoses location and morphology in the left main coronary artery in relation to anatomic left main length. Am J Cardiol 88(1):1–4
Nørgaard BL, Fairbairn TA, Safian RD, Rabbat MG, Ko B, Jensen JM, Nieman K, Chinnaiyan KM, Sand NP, Matsuo H, Leipsic J, Raff G (2019) Coronary CT angiography-derived fractional flow reserve testing in patients with stable coronary artery disease: recommendations on interpretation and reporting. Radiology 1(5):50. https://doi.org/10.1148/ryct.2019190050
Collet C, Onuma Y, Andreini D, Sonck J, Pompilio G, Mushtaq S, La Meir M, Miyazaki Y, de Mey J, Gaemperli O, Ouda A, Maureira JP, Mandry D, Camenzind E, Macron L, Doenst T, Teichgraber U, Sigusch H, Asano T, Katagiri Y, Morel MA, Lindeboom W, Pontone G, Luscher TF, Bartorelli AL, Serruys PW (2018) Coronary computed tomography angiography for heart team decision-making in multivessel coronary artery disease. Eur Heart J 39(41):3689–3698
Linde JJ, Kelbæk H, Hansen TF, Sigvardsen PE, Torp-Pedersen C, Bech J, Heitmann M, Nielsen OW, Høfsten D, Kühl JT, Raymond IE, Kristiansen OP, Svendsen IH, Vall-Lamora MHD, Kragelund C, de Knegt M, Hove JD, Jørgensen T, Fornitz GG, Steffensen R, Jurlander B, Abdulla J, Lyngbæk S, Elming H, Therkelsen SK, Jørgensen E, Kløvgaard L, Bang LE, Hansen PR, Helqvist S, Galatius S, Pedersen F, Abildgaard U, Clemmensen P, Saunamäki K, Holmvang L, Engstrøm T, Gislason G, Køber LV, Kofoed KF (2020) Coronary CT angiography in patients with non-ST-segment elevation acute coronary syndrome. J Am Coll Cardiol 75(5):453–463
Acknowledgements
None
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was financially supported by the Faculty of Health Sciences, Aarhus University Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This work was financially supported by the Faculty of Health Sciences, Aarhus University Hospital. Dr. JM Jensen and Dr. BL Nørgaard have received unrestricted research grants from Edwards Lifesciences, Siemens, and HeartFlow. Dr. EL Grove has received speaker honoraria or consultancy fees from AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Merck Sharp and Dohme, Pfizer, and Roche. Dr. J Leipsic has received speaker honoraria from GE Healthcare; served as a consultant for Edwards Lifesciences, and served as a consultant for and has stock options in Circle CVI and HeartFlow. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Ethical approval
The study was approved by the Danish Data Protection Agency (1-16-02-110-17) with a waiver for individual informed consent by the regional ethical committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Riedl, K.A., Jensen, J.M., Ko, B.S. et al. Coronary CT angiography derived FFR in patients with left main disease. Int J Cardiovasc Imaging 37, 3299–3308 (2021). https://doi.org/10.1007/s10554-021-02371-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-021-02371-4