Abstract
Purpose
To assess whether androgens play a role in explaining the sex related differences in the incidence of colorectal cancer (CRC).
Methods
A nationwide matched cohort study was conducted employing the Prostate Cancer data Base Sweden (PCBaSe) 4.0 during the study period 2006–2016. Prostate cancer (PC) patients receiving androgen deprivation therapy (ADT) were treated as exposed. Prostate cancer-free men from the general population were randomly selected and matched to the index case by birth year and county of residence, forming the unexposed group. All were followed until a diagnosis of CRC, death, emigration, or end of the study period. The risk of CRC among ADT exposed PC patients compared to unexposed cancer-free men was calculated using a flexible parametric survival model and expressed as hazard ratios (HRs) with 95% confidence intervals (CIs).
Results
There was an increased risk of CRC among ADT exposed PC patients compared to unexposed cancer-free men (HR 1.27 [95% CI 1.15–1.41]), in particular an increased risk of adenocarcinoma of the colon (HR 1.33 [95% CI 1.17–1.51]) and more specifically an increased risk of adenocarcinoma of the distal colon (HR 1.53 [95% CI 1.26–1.85]). Examination of latency effects yielded significantly decreased HRs over time for CRC (p = 0.049 for trend).
Conclusions
This population-based study found an increased risk of CRC among PC patients exposed to ADT, specifically adenocarcinoma of the distal colon, which indicates an increased association between ADT (PC + ADT) and CRC but not a positive dose-response trend questioning a true causal effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
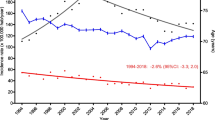
Colorectal cancer (CRC) is the third most common cancer in men, the second most common cancer in women and the second most common cause of cancer death in both sexes when analyzed separately, accounting for 1 in 10 cancer cases and deaths globally [1]. In the past decades the incidence of CRC has increased globally, most of which can be explained by a growing and aging population, however, the incidence would have increased withholding population and age dynamics due to changing age-specific incidence rates [2] mostly attributable to the influence of new dietary patterns, obesity, life-style factors and a lack of health infrastructure and early detection [3]. The odds of developing CRC is higher in men than in women [2], whereas the age-specific incidence rates during the past decades is similar for men and women [4]. However, in more recent times there is a global trend for men to have higher age-specific incidence rates than women [5].
The proximal colon originates from the embryological midgut whereas the distal colon and rectum originate from the hindgut. The two subsites differ partly with regard to mechanisms of carcinogenesis [6] and genetic architectures [7] but a distinct dichotomy has been challenged [8]. The incidence of CRC in the proximal colon is higher in women than in men and the reverse is true for the distal colon and rectum [9]. Other established risk factors for CRC include hereditary factors, abdominal radiation, lifestyle factors, obesity, metabolic syndrome, hyperinsulinemia, and diabetes. Protective factors include daily moderate physical activity and a diet high in whole grains and dietary fibers [10, 11]. The sexes also differ with regard to exposure to risk factors such as smoking [12], alcohol [13], diet [13] and obesity [14]. Regarding sex hormones, higher endogenous testosterone levels have been linked to both a lower risk of CRC in men [15] and a higher risk of CRC in postmenopausal women [16]. Experimental studies have indicated that androgens may have a protective effect against colorectal carcinogenesis, decreasing CRC risk by activating androgen receptors [17]. Furthermore, testosterone deficiency, for example induced by androgen deprivation therapy (ADT) for prostate cancer has been associated with the development of CRC [18], as well as conditions [19, 20] which are known risk factors for CRC such as diabetes and metabolic syndrome [21,22,23].
ADT is either surgical (bilateral orchiectomy) or chemical (gonadotropin-releasing hormone (GnRH) agonists or oral anti-androgens) and has long been a standard treatment for metastatic prostate cancer and is also part of the treatment of prostate cancer patients with locally advanced or high-risk disease as neoadjuvant and adjuvant ADT in conjunction with radiotherapy [24,25,26]. However, ADT is increasingly being used earlier in the course of the disease, such as in patients with biochemical relapse, thus potentially allowing for more prostate cancer patients to be exposed to ADT for a longer period of time.
The relationship between androgens and the risk of CRC needs to be further examined. We therefore hypothesized that androgens decrease the risk of CRC and consequently that ADT increases the risk in men. We further hypothesize that the risk of CRC is dependent on the sub-site of the colon analyzed since they differ in origin and the incidence of CRC in the distal colon and rectum is higher in men. To test these hypotheses, and since the aim of this study was not primarily related to the clinical setting of prostate cancer patients and their risk/benefit of undergoing ADT, but rather to assess whether androgens play a role in explaining the sex related differences in the incidence of CRC, we identified a nationwide cohort of men with prostate cancer who were exposed to different forms of ADT and compared them to a matched cohort of unexposed and cancer-free men.
Methods
Data sources
We used data from Prostate Cancer data Base Sweden (PCBaSe), created when the nationwide and comprehensive National Prostate Cancer Register (NPCR) [27] in Sweden was linked to a number of other national health-care registers and demographic databases including the Total Population Register, Patient Register and Cause of Death Register [28, 29]. PCBaSe contains information from the NPCR, which covers > 98% of all diagnosed cases of prostate cancer compared to the Swedish Cancer Register, became nationwide in 1998 and includes information such as: age at diagnosis, date of diagnosis and data on primary prostate cancer treatment [28, 30, 31]. In this study, we collected data from the latest installment, PCBaSe 4.0, which includes data from 1998 to 2016, and in which a comparison cohort of men without prostate cancer has been created by selecting five prostate cancer-free men in a randomized fashion from the Total Population Register, matched to each of the index cases by birth year (attained age) and county of residence [32]. Data on migration was obtained from the Total Population Register [33] whereas death dates were obtained from the Cause of Death Register [34] and marital status and educational level from The Longitudinal integration database for health insurance and labor market studies (LISA) [35]. Data on drug use was linked to PCBaSe 4.0 from the Prescribed Drug Register [36], which contains data on all prescribed drugs in Sweden since its inception on 1 July 2005.
Study design
We conducted a matched cohort study employing the PCBaSe 4.0 database. Entry time in the study was set from 1 January 2006 (to allow for left truncation of the Prescribed Drug Register as is required in all time-to-event analysis due to the later start date on 1 July 2005) [32] to 31 December 2015. Prostate cancer patients receiving ADT were included in the cohort as exposed, while prostate cancer patients that did not receive ADT and their matched controls were excluded from the study. We used the comparison cohort of men without prostate cancer described above as the unexposed group. This choice of control group was based not on the risk of confounding alone, but also on avoiding misclassification of ADT exposure, and that confining the study population only to men diagnosed with PC would raise concerns on its external validity and relevance for the general population. Men were followed until a diagnosis of colorectal cancer, death, emigration, or end of the study period 31 December 2016, whichever occurred first. Ascertainment of cancer cases was obtained by linkage with the Swedish National Cancer Register in which more than 98% of cancer cases are morphologically verified [37].
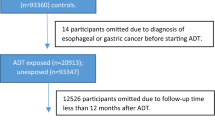
Study population
The source population included all Swedish men diagnosed with prostate cancer during 2006 through 2015 and their matched controls wherefrom the study population was selected consisting of all ADT-exposed prostate cancer patients and their corresponding unexposed cancer-free matched controls. The index date was the date of prostate cancer diagnosis for cases, and the controls were assigned the same index date as their matching case. Follow-up was started at the date of the first ADT prescription for prostate cancer cases and the same date for the corresponding controls. Prostate cancer cases (and their matched controls) with another cancer diagnosis (apart from non-melanoma skin cancer ICD-7: 191) at or prior to start of follow-up, a missing date of prostate cancer diagnosis, or a follow-up time of less than one year were excluded. Furthermore, the first year of follow-up for both cases and controls was excluded to limit the effects of surveillance bias, i.e., patients with a newly diagnosed prostate cancer could be more likely to have another cancer detected due to the diagnostic evaluation of their prostate cancer.
Exposure definitions
All included prostate cancer cases were ADT exposed and their corresponding cancer-free matched controls were considered unexposed to ADT. ADT was administered in the form of anti-androgens (AA), gonadotropin-releasing hormone (GnRH) analogues (i.e., agonists), GnRH + flare protection (by concomitant use of anti-androgens during a restricted time, usually one month), orchiectomy and total androgen blockade (GnRH plus anti-androgens continuously). Some cases were initially placed on watchful waiting at diagnosis and put on ADT at a later date. We only had information on the first prescription of ADT administered to each case of prostate cancer. Cases were considered exposed from the date of first prescription of ADT and were assumed to remain exposed to the same type of ADT until the end of follow-up. To identify incident use of ADT in men who started ADT as opposed to men who had used it for a long period with an unknown start date (before the inception of the Prescribed Drug Register) we needed a wash-out period of six months. Hence, all prostate cancer patients diagnosed before 1 January 2006 (from 1998 to 2005) and their matched controls were excluded from the study.
Outcome definitions
Subtypes of CRC were classified using the 7th version of the International Classification of Diseases (ICD-7) and histology was classified according to WHO/HS/CANC/24.1 histology codes. For adenocarcinoma of the colon ICD-7: 153.0–153.3 was included. Cancer of the appendix (ICD-7 153.4) and Familial polyposis of the colon (ICD-7 153.8) were therefore not included as outcomes (Fig. 1) whereas overlapping lesion of the colon; colon unspecified including large intestine NOS (ICD-7 153.9) was included in the analysis of colorectal and colon cancer but not included as an outcome in the sub-site analyses of proximal and distal colon cancer. Among rectal cancers, cancer of the colorectal junction and rectum proper (ICD-7: 154.0) was included while not including anal cancer (ICD-7: 154.1) as an outcome (Fig. 1). The following WHO/HS/CANC/24.1 histology codes were used and jointly classified as adenocarcinoma: 093 (adenocarcinoma of unknown origin), 094 (adenocarcinoma in situ) and 096 (adenocarcinoma). Colorectal cancers with other histological classifications were omitted from the analyses. Firstly, we analyzed all included sub-sites of the colon and rectum combined. Secondly, we analyzed the colon and rectum separately. Thirdly, we separated the colon into the proximal and the distal parts. Finally, cases that were diagnosed with both colon cancer and rectal cancer simultaneously (double registration in the database) were included in the analysis of all sites of the colon and rectum combined but excluded from all other analyses.
Statistical analyses
The continuous variables of the study population were summarized as means with standard deviations. The categorical variables were described using frequencies with percentages. Crude incidence rates with corresponding confidence intervals (CIs) of CRC in the ADT-exposed prostate cancer group and unexposed cancer-free control group were calculated by dividing the number of newly diagnosed CRC cases over accumulated person-time. The association between use of ADT, including subtypes, and the occurrence of different localizations of colorectal cancer was studied. Hazard Ratios (HRs) with corresponding 95% CIs for developing CRC were calculated comparing each ADT exposure group to the matching ADT-free control group, respectively. HRs were modeled by a flexible parametric survival model using follow-up time as the underlying timescale of research. We decided à priori to employ a flexible parametric survival model. For correlations within matching groups, all CIs were adjusted for the clustering effect. HR > 1 implied a higher risk for the outcome of interest, i.e., CRC or subsites of CRC. The model fitness of either time-constant or time-dependent were compared and since the results of the two different models did not differ substantially, suggesting no significant time-dependent effects, we decided to employ the time-constant model in all main analyses. We also controlled for the potential confounders of age (continuous), attained level of education (Low [< 10 years]; Middle [10–12 years]; High [> 12 years]) and marital status (not married, married, separated, widower). A complete case analysis was performed because the number of missing variables was considered negligible. To study the effect of latency in CRC development, we also grouped prostate cancer patients based on their exposure time to ADT into three separate groups: 1–3 years; 3–5 years; >5 years and modeled the HRs using a Poisson regression model. The HRs for developing CRC were calculated comparing each ADT exposure group to the matching ADT-free control group, respectively (non-cumulative). P-values < 0.05 were considered statistically significant. All statistical analyses were performed using the statistical software Stata (version 16; Stata Corporation, College Station, TX, USA). The study was approved by the Ethical Review Board in Stockholm, Sweden (DNR: 2009/1196-31/1 with amendments DNR: 2009/2124-32 and DNR: 2011/1674-32).
Results
Participants
Following initial exclusions, PCBase encompassed 60,110 patients with prostate cancer and 236,388 matched cancer-free controls. After exclusions (Fig. 1) 25,948 ADT exposed patients with prostate cancer diagnosed between 1 January 2006 and 31 December 2015 and 115,598 unexposed cancer-free controls remained for final analysis. The total follow-up time in the cohort was 521,226.0 person-years and the median follow-up time was 4.2 years (interquartile range 2.5 to 6.6 years). Characteristics of the study participants are presented in Table 1. There were no major differences between exposed and unexposed with regard to age, marital status, or educational level. The time from prostate cancer diagnosis to start of ADT ranged between 0 and 119 months: 65.3% of patients started ADT within 3 months of prostate cancer diagnosis; 14.9% of patients started ADT between 3 and 12 months following prostate cancer diagnosis; 19.8% of patients started ADT more than 12 months after prostate cancer diagnosis. The median (interquartile range 1–3) number of days of waiting time from prostate cancer diagnosis to start of ADT was 49 (25–210) days. The follow-up time was slightly longer for unexposed than ADT exposed.
Risk of colorectal adenocarcinoma
During follow-up, 2,243 participants in the cohort developed a new diagnosis of CRC. Exposure to any form of ADT among prostate cancer patients was followed by an increased risk of CRC (HR 1.27 [95% CI 1.15–1.41]) as compared to ADT unexposed cancer-free matched controls. Stratified into different forms of ADT, there was a significantly increased risk of developing CRC after exposure to AA (HR 1.23 [95% CI 1.04–1.47]) and GnRH + flare (HR 1.22 [95% CI 1.04–1.43]), an increased point estimate but not a significantly increased risk of developing CRC after exposure to GnRH (HR 1.30 [95% CI 0.98–1.72]) or Orchiectomy (HR 1.39 [95% CI 0.95–2.03]), whilst exposure to Total Androgen Blockade (TAB) yielded a decreased point estimate that was not significant (HR 0.87 [95% CI 0.43–1.75]). (Table 2 A). Analysis of latency yielded significantly decreasing HRs over time (p = 0.049 for trend) (Table 3 A).
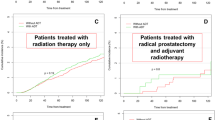
Risk of adenocarcinoma of the colon
During follow-up, 1,447 new cases of adenocarcinoma of the colon were identified. Exposure to any form of ADT among prostate cancer patients was followed by an increased risk of adenocarcinoma of the colon (HR 1.33 [95% CI 1.17–1.51]) as compared to ADT unexposed cancer-free matched controls. Stratified into different forms of ADT, there was a significantly increased risk of developing adenocarcinoma of the colon after exposure to AA (HR 1.29 [95% CI 1.04–1.60]) and GnRH + flare (HR 1.29 [95% CI 1.07–1.56]), but no significant association after exposure to GnRH (HR 1.29 [95% CI 0.91–1.83]), Orchiectomy (HR 1.42 [95% CI 0.89–2.27]), or Total Androgen Blockade (TAB) (HR 0.70 [95% CI 0.26–1.88]), (Table 2 A). Analysis of latency yielded no significant time trend (p = 0.332) (Table 3 A). Among 1,447 cases of adenocarcinoma of the colon identified during follow up, 738 were located in the proximal colon. Exposure to ADT among prostate cancer patients was not associated with a significantly increased risk of developing adenocarcinoma of the proximal colon (any ADT HR 1.13 [95% CI 0.93–1.36]) (Table 2B) and analysis of latency yielded no significant time trend (p = 0.363) (Table 3B). Among 1,447 cases of adenocarcinoma of the colon identified during follow up, 636 were located in the distal colon. Exposure to any form of ADT among prostate cancer patients was followed by an increased risk of adenocarcinoma of the distal colon (HR 1.53 [95% CI 1.26–1.85]), particularly after exposure to GnRH + flare (HR 1.59 [95% CI 1.21–2.08]) (Table 2B). Analysis of latency yielded inconclusive results with an initially increased HR followed by a decreased HR (p = 0.723 for trend) (Table 3B).
Risk of rectal adenocarcinoma
During follow-up, 767 cases of rectal adenocarcinoma were identified. There was no significant increased risk of developing rectal adenocarcinoma among prostate cancer patients exposed to either any form of ADT (HR 1.19 [95% CI 0.99–1.43]) or different forms of ADT (Table 2 A). Examination of latency effects showed an initially increased HR followed by decreased point estimates which taken together yielded significantly decreased HRs over time (p = 0.034 for trend) (Table 3 A).
Discussion
The results of this study indicate that prostate cancer patients exposed to ADT were at an increased risk of CRC, in particular of the distal colon as compared to ADT unexposed cancer-free matched controls. Furthermore, stratified into different forms of ADT, the increased risk was especially evident after exposure to both AA and GnRH + flare. However, time trends indicated that this increased risk was attenuated by time which argues against a dose-response effect.
The strengths of this study lie in the availability of nationwide, comprehensive, and high-quality health-care registers, yielding a large sample size with a substantial number of person-years at risk, a close to complete follow-up and a documented accuracy of cancer diagnoses through ascertainment with the national cancer register. All these factors serve to counteract selection and information biases. As was the case in earlier studies [38, 39], but as an evolution compared to recent findings [18], this study made use of data on the type of ADT prescribed to each prostate cancer patient. Moreover, the number of CRCs classified as unspecified site was small providing robust risk estimates in the overall sub-site analysis and all proximal and distal portions of the colon were evaluated separately.
A number of weaknesses should be highlighted. Follow-up was shorter than we would have liked, despite prostate cancer data being available in the NPCR since 1998, due to the relatively short time since the inception of the Prescribed Drug Register in Sweden in 2005 and the latest version of PCBaSe (version 4) only covering cases through 2016. However, we don’t consider follow-up too short to capture a biologically relevant duration of exposure. One reason for this is that in previous research [39] that reported a dose-response trend of increased CRC risk with a longer duration of ADT exposure, this effect appeared to arise relatively early, perhaps within one year, suggesting that ADT might influence relatively late processes of carcinogenesis. Despite a large sample size, we may have lacked the statistical power in secondary analyses. The stratified analyses of different forms of ADT were hampered by a small number of cases in certain subgroups, especially with regard to proximal and distal colon cancer, resulting in wider CIs and, therefore, less precise estimates. Moreover, our main finding of an increased risk of colorectal cancer could be due to a type I error i.e., a chance finding. However, our main hypothesis of an increased risk of CRC was formulated à priori and based on previously published results. Our results could have been impacted by detection or surveillance bias i.e., an increase in a second primary cancer (CRC) following a diagnosis of a primary cancer (prostate cancer). We tried to reduce the impact of such bias by using a latency time of one year.
Another limitation to our study is the lack of data on a number of potential confounders known to be associated with CRC which might also influence the use of ADT: obesity, diabetes, diet, and other lifestyle-related risk factors [38]. Adverse effects of ADT include the development of known risk factors for CRC such as obesity and diabetes, neither of which were included in our database. One study [39] stated that obesity may be an important confounder because it is known to increase the risk of CRC in men and is possibly associated with advanced prostate cancer which is more likely to be treated with ADT. Another potential concern is that we did not include prostate cancer stage in our analysis. It is conceivable that our study population with a mean age of approximately 75 years and exposed to ADT are more likely to have advanced prostate cancer. Due to both prostate cancer per se and potential side effects of ADT including obesity these patients might be more physically inactive, which has been associated with an increased risk of CRC [40]. Finally, regarding factors such as diet and other lifestyle-related risk factors not included in our database, two studies [18, 38] found that it was unlikely that these factors could have affected the validity of their results as it is unclear why these variables would be differentially distributed between users and non-users of ADT.
Despite all of these potential confounders, other important variables such as age, residential area, marital status, and educational level (a robust measure of socioeconomic status) were adjusted for in the model.
A further limitation to this study which might introduce biases related to misclassification of exposure during follow-up, is that we only had information on the first prescription of ADT. Hence, we assumed prostate cancer cases to remain exposed to the same type of ADT until the end of follow-up. The same assumption that was used in a previous study [39]. Furthermore, we treated prostate cancer patients exposed to ADT as a time-constant exposure and assumed, based on previous research, that prostate cancer patients have a high adherence to treatment [41] although age above 75 years and low-risk prostate cancer were associated with lower adherence. Even so, it was unknown to us whether prescriptions were actually filled at the pharmacy or to what extent patients fully complied with the treatment regimen. However, all such misclassification of exposure resulting mostly from non-adherence to prescribed treatment in an aged population would only serve to dilute the point estimates toward the null.
We opted to only use a control group from the general population as opposed to or including a control group of prostate cancer patients that were not exposed to ADT for several reasons: Firstly, men diagnosed with prostate cancer that do not receive ADT will very likely differ regarding several important potentially controllable but also uncontrollable factors from those treated with ADT which could introduce bias. Secondly, men diagnosed with prostate cancer that do not receive ADT are in fact a heterogenous group considering that many of them have a low-risk prostate cancer that never requires any treatment, while others have tumors that are of higher risk treated with radiotherapy or surgery. Both of these examples of differences within the prostate cancer group raise concerns of bias, particularly confounding by indication which might have uncontrollable and unpredictable effects on the results. Moreover, many prostate cancer patients will experience disease progression and will eventually receive ADT as this is used for palliation for advanced disease. Using men diagnosed with prostate cancer not receiving ADT as a control group would therefore risk adding complexity since many will become exposed which would also raise questions about its robustness and appropriateness as comparison group. Lastly, confining the study population only to men diagnosed with prostate cancer would raise concerns on its external validity and relevance for the general population, i.e., the aim of the study.
This study found an increased risk of CRC, in particular an increased risk of adenocarcinoma of the distal colon among prostate cancer patients exposed to ADT as compared to ADT unexposed cancer-free matched controls. A diagnosis of prostate cancer may lead to a positive change in lifestyle, potentially influencing the exposure to risk factors such as diet, tobacco smoking and obesity, lowering the risk of further malignancy, including CRC. However, such a change in lifestyle would only serve to weaken the association, not refute it. Furthermore, it is conceivable that men with prostate cancer may be more susceptible to the development of CRC. A lower risk of CRC after prostate cancer was reported in one study [42] whereas others reported an increased risk of CRC after a diagnosis of prostate cancer [43, 44].
The association between prostate cancer patients exposed to ADT and an increased risk of CRC is in support with some similar studies [18, 39] but in conflict with others [38]. Gillessen et al. [39] reported the highest risk of CRC after orchiectomy followed by exposure to GnRH. These associations remained after adjusting for potential confounders such as obesity and diabetes. They also found a dose-response effect with a higher risk of CRC with increasing duration of ADT possibly supporting a causal association, whereas our analysis of latency yielded a negative dose-response trend in CRC with significantly decreasing HRs following a longer duration of ADT, weakening the potential for a causal association between prostate cancer patients exposed to ADT and CRC. However, Gillessen’s study was performed entirely among men with prostate cancer potentially introducing bias from confounding by indication. Lu et al. similarly found an increased risk of CRC after orchiectomy as well as an increased risk following ADT. The increased risk was found in the distal colon, which is in line with our results, but also in the rectum [18]. In contrast to these positive studies Assayag et al. similarly found an increased risk of CRC after orchiectomy but not a significantly increased risk following exposure to ADT and no dose-response effect. They hypothesized that it is unlikely that the anti-hormonal effects of GnRH agonists and orchiectomy act differently on colorectal tissues and that the association observed between bilateral orchiectomy and colorectal cancer is better explained by the longer anti-hormonal duration of castration [38]. Since we did not observe any significant effect following orchiectomy on overall CRC risk or after sub-site analysis, we cannot confirm their hypothesis, possibly due to small numbers. Others have found an increased risk of CRC following a diagnosis of prostate cancer but did not include ADT as a separate exposure variable [45]. Two separate studies further concluded that one should not assume that an increased rate of a second cancer is necessarily linked to the treatment of the first cancer [46] and that treatment might not be the only contributor to a higher risk of colon cancer suggesting that similarities in etiologic factors also could contribute [47].
We hypothesized that the risk of CRC following exposure to ADT in prostate cancer patients would be sub-site dependent since the proximal and distal colorectum differ in genetic pathways to disease, the influence of sex-related factors and the distribution of sex hormone receptors [18]. Furthermore, the incidence of CRC in men has consistently been shown to be higher in the distal part of the colon and rectum compared to females [48]. In our all-male cohort, we did indeed find an increased risk in the distal part of the colon.
Endogenous sex hormones and CRC risk has been studied extensively in both experimental and epidemiological settings, but their role remain unclear. Previous research has indicated sex-specific effects of testosterone on CRC development. Higher endogenous testosterone levels was associated with a lower risk of CRC in men [15] but a higher risk of CRC [16] and advanced adenoma [49] in postmenopausal women. However, these results have not been consistently reproduced in the literature and several studies [50,51,52] have found no association between testosterone and CRC risk in both men and women. A recent review and meta-analysis [53] found no associations between endogenous sex steroid hormones in men or postmenopausal women and CRC risk with substantial heterogeneity among women.
The biological mechanisms behind the potentially true association between prostate cancer patients exposed to ADT and CRC risk remain unclear. Androgen receptors are more frequently found in normal colonic mucosa than in colorectal tumors [54, 55]. Several animal studies suggest that androgens may have a protective effect on the development of CRC whereas suppression of androgens may promote it [56,57,58]. In spite of these proposed molecular mechanisms for androgens acting through androgen receptors and their role in CRC carcinogenesis most previous epidemiological and experimental studies show opposing results. There seems to be a relationship between androgens (and therefore ADT) and the development of CRC but this relationship seems to be far more complex and involve both direct mechanisms (androgen receptors) and indirect mechanisms such as stress hormone levels, the innate immune system, bile as well as various risk factors including type 2 diabetes mellitus and metabolic syndrome or a combination of both acting in synergy [59]. These mentioned strong risk factors for CRC are correlated to hyperinsulinemia [60], which together with insulin resistance are linked to obesity and CRC development [61]. Since ADT can cause obesity and hyperinsulinemia which in turn increases the risk of CRC [62] it is conceivable that insulin resistance as a consequence of ADT is another plausible mechanism for the increased CRC risk. Moreover, both androgens and estrogens are hypothesized to prevent tumor growth in part by preventing insulin and insulin-like growth factor (IGF) from binding to their receptors [63] and there is evidence of an association between IGF-1 and the risk of CRC [64]. Furthermore, men with prostate cancer who received endocrine treatment and underwent surveillance were at greater risk of developing IGF-1-related cancers [47]. Thus, obesity as well as metabolic syndrome are risk factors for both prostate cancer [65] as well as CRC, and both are linked to high IGF-1 levels, which in turn is associated with an increased risk of both prostate cancer and CRC [64, 66]. It is clear that future studies should include detailed information on obesity which was not included in our database. An increased risk of colon but not rectal cancer in men, corroborating our findings, was found in one study [67] with increasing anthropometric measurements of obesity alone. One should further take into consideration that although obesity has also been associated with an increased risk of CRC in women, the association seems to be stronger in men and only in men is obesity associated with lower testosterone levels [68]. Increased levels of endogenous estrogen seem to protect women whereas increased levels of endogenous testosterone might decrease the risk of CRC in men [15]. Since increasing adiposity with age leads to higher levels of estrogen in postmenopausal women, whereas it leads to a decline in testosterone levels in men, the relationship between obesity and CRC risk might be attenuated in women but amplified in men [11].
During the past decades, research has failed to reach a consensus regarding the direct connection between androgens and the risk of CRC. Taken together, all previously mentioned epidemiological and experimental evidence to date infer the possibility that the findings in this study may not be causal but a result of an interplay between true sex hormonal effects, the possibility that men with prostate cancer are at greater risk of developing CRC à priori compared to the general population, the impact of known side effects of ADT such as obesity, hyperinsulinemia and insulin resistance which are known risk factors for CRC and the added effects of various forms of residual confounding. Thus, further research is needed that will focus on both epidemiologic data and the molecular mechanisms implicated in CRC, to provide the answer to the role of androgens, and therefore the effect of anti-androgens, in the etiology of CRC.
If the results of the present study can be further verified, the potential future clinical implications may include intensified screening programs for CRC in prostate cancer patients exposed to ADT and a continued awareness that the potential long-term effects of ADT constitute potential risk factors for the development of CRC. However, further research to clarify these relationships is warranted before any large preventive measures are instituted in these populations. Moreover, research should focus on elucidating the biological mechanisms behind possible direct effects of androgens and their receptors in the etiology of CRC to potentially harness any preventive effects and future treatment of prostate cancer patients should strive to employ different forms of ADT with less side effects contributing to an increased risk of CRC.
In conclusion, this Swedish nationwide population-based matched cohort study yielded an increased risk of CRC and more specifically adenocarcinoma of the distal colon, suggesting an increased association between androgen deprivation therapy in prostate cancer patients and CRC. However, we found no dose-response effect which argues against a true causal effect. Future studies are warranted.
Data Availability
All data and materials are available upon request.
Code Availability
All statistical analyses were performed using the statistical software Stata (version 16; Stata Corporation, College Station, TX, USA). All coding is available upon request.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin.
Fitzmaurice C, Abate D, Abbasi N, Abbastabar H, Abd-Allah F, Abdel-Rahman O et al (2019) Global, Regional, and National Cancer incidence, mortality, years of Life Lost, Years lived with disability, and disability-adjusted life-years for 29 Cancer groups, 1990 to 2017: a systematic analysis for the global burden of Disease Study. JAMA Oncol.
Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F (2017) Global patterns and trends in colorectal cancer incidence and mortality. Gut 66(4):683–691
Rutegard M, Shore R, Lu YX, Lagergren P, Lindblad M (2010) Sex differences in the incidence of gastrointestinal adenocarcinoma in Sweden 1970–2006. Eur J Cancer 46(6):1093–1100
Douaiher J, Ravipati A, Grams B, Chowdhury S, Alatise O, Are C (2017) Colorectal cancer-global burden, trends, and geographical variations. J Surg Oncol 115(5):619–630
Iacopetta B (2002) Are there two sides to colorectal cancer? Int J Cancer 101(5):403–408
Huyghe JR, Harrison TA, Bien SA, Hampel H, Figueiredo JC, Schmit SL et al (2021) Genetic architectures of proximal and distal colorectal cancer are partly distinct. Gut 70(7):1325–1334
Yamauchi M, Morikawa T, Kuchiba A, Imamura Y, Qian ZR, Nishihara R et al (2012) Assessment of colorectal cancer molecular features along bowel subsites challenges the conception of distinct dichotomy of proximal versus distal colorectum. Gut 61(6):847–854
Heo JW, Kim SE, Sung MK (2021) Sex differences in the incidence of obesity-related gastrointestinal Cancer. Int J Mol Sci. ;22(3)
Rawla P, Sunkara T, Barsouk A (2019) Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Przeglad gastroenterologiczny 14(2):89–103
Keum N, Giovannucci E (2019) Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroenterol Hepatol 16(12):713–732
WHO. Global Report on Trends in Prevalence of Tobacco Smoking: World Health Organization (2021) ; [Available from: https://www.who.int/publications/i/item/9789240039322
Tabung FK, Brown LS, Fung TT (2017) Dietary patterns and colorectal Cancer risk: a review of 17 years of evidence (2000–2016). Curr Colorectal Cancer Rep 13(6):440–454
Kim H, Giovannucci EL (2017) Sex differences in the association of obesity and colorectal cancer risk. Cancer Causes Control 28(1):1–4
Lin JH, Zhang SM, Rexrode KM, Manson JE, Chan AT, Wu K et al (2013) Association between sex hormones and colorectal cancer risk in men and women. Clin Gastroenterol Hepatol 11(4):419–24e1
Mori N, Sawada N, Iwasaki M, Yamaji T, Goto A, Shimazu T et al (2019) Circulating sex hormone levels and colorectal cancer risk in japanese postmenopausal women: the JPHC nested case-control study. Int J Cancer 145(5):1238–1244
Chen SY, Wulf G, Zhou XZ, Rubin MA, Lu KP, Balk SP (2006) Activation of beta-catenin signaling in prostate cancer by peptidyl-prolyl isomerase Pin1-mediated abrogation of the androgen receptor-beta-catenin interaction. Mol Cell Biol 26(3):929–939
Lu Y, Ljung R, Martling A, Lindblad M (2015) Risk of Colorectal Cancer by Subsite in a swedish prostate Cancer Cohort. Cancer Control 22(2):263–270
Braga-Basaria M, Dobs AS, Muller DC, Carducci MA, John M, Egan J et al (2006) Metabolic syndrome in men with prostate cancer undergoing long-term androgen-deprivation therapy. J Clin Oncol 24(24):3979–3983
Teoh JY, Chiu PK, Chan SY, Poon DM, Cheung HY, Hou SS et al (2015) Risk of new-onset diabetes after androgen deprivation therapy for prostate cancer in the asian population. J Diabetes 7(5):672–680
Aleksandrova K, Nimptsch K, Pischon T (2013) Influence of obesity and related metabolic alterations on Colorectal Cancer Risk. Curr Nutr Rep 2(1):1–9
Esposito K, Chiodini P, Capuano A, Bellastella G, Maiorino MI, Rafaniello C et al (2013) Colorectal cancer association with metabolic syndrome and its components: a systematic review with meta-analysis. Endocrine 44(3):634–647
Giovannucci E (2007) Metabolic syndrome, hyperinsulinemia, and colon cancer: a review. Am J Clin Nutr 86(3):s836–s842
Roach M 3rd, Bae K, Speight J, Wolkov HB, Rubin P, Lee RJ et al (2008) Short-term neoadjuvant androgen deprivation therapy and external-beam radiotherapy for locally advanced prostate cancer: long-term results of RTOG 8610. J Clin Oncol 26(4):585–591
Bolla M, Van Tienhoven G, Warde P, Dubois JB, Mirimanoff RO, Storme G et al (2010) External irradiation with or without long-term androgen suppression for prostate cancer with high metastatic risk: 10-year results of an EORTC randomised study. Lancet Oncol 11(11):1066–1073
Pilepich MV, Winter K, Lawton CA, Krisch RE, Wolkov HB, Movsas B et al (2005) Androgen suppression adjuvant to definitive radiotherapy in prostate carcinoma–long-term results of phase III RTOG 85 – 31. Int J Radiat Oncol Biol Phys 61(5):1285–1290
Cazzaniga W, Ventimiglia E, Alfano M, Robinson D, Lissbrant IF, Carlsson S et al (2019) Mini review on the Use of Clinical Cancer registers for prostate Cancer: the national prostate Cancer Register (NPCR) of Sweden. Front Med 6:51
Hagel E, Garmo H, Bill-Axelson A, Bratt O, Johansson JE, Adolfsson J et al (2009) PCBaSe Sweden: a register-based resource for prostate cancer research. Scand J Urol Nephrol 43(5):342–349
Van Hemelrijck M, Wigertz A, Sandin F, Garmo H, Hellstrom K, Fransson P et al (2013) Cohort Profile: the national prostate Cancer Register of Sweden and prostate Cancer data base Sweden 2.0. Int J Epidemiol 42(4):956–967
Tomic K, Berglund A, Robinson D, Hjalm-Eriksson M, Carlsson S, Lambe M et al (2015) Capture rate and representativity of the national prostate Cancer Register of Sweden. Acta Oncol 54(2):158–163
Tomic K, Sandin F, Wigertz A, Robinson D, Lambe M, Stattin P (2015) Evaluation of data quality in the national prostate Cancer Register of Sweden. Eur J Cancer 51(1):101–111
Van Hemelrijck M, Garmo H, Wigertz A, Nilsson P, Stattin P (2016) Cohort Profile Update: the national prostate Cancer Register of Sweden and prostate Cancer data Base–a refined prostate cancer trajectory. Int J Epidemiol 45(1):73–82
Ludvigsson JF, Almqvist C, Bonamy AK, Ljung R, Michaëlsson K, Neovius M et al (2016) Registers of the swedish total population and their use in medical research. Eur J Epidemiol 31(2):125–136
Godtman R, Holmberg E, Stranne J, Hugosson J (2011) High accuracy of swedish death certificates in men participating in screening for prostate cancer: a comparative study of official death certificates with a cause of death committee using a standardized algorithm. Scand J Urol Nephrol 45(4):226–232
LISA. Longitudinal integration database for health insurance and labour market studies (LISA by Swedish acronym) Statistics Sweden; [Available from: http://www.scb.se/en/services/guidance-for-researchers-and-universities/vilka-mikrodata-finns/longitudinella-register/longitudinal-integration-database-for-health-insurance-and-labour-market-studies-lisa/
Wettermark B, Hammar N, Fored CM, Leimanis A, Otterblad Olausson P, Bergman U et al (2007) The new Swedish prescribed Drug Register–opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf 16(7):726–735
Barlow L, Westergren K, Holmberg L, Talbäck M (2009) The completeness of the Swedish Cancer Register: a sample survey for year 1998. Acta Oncol 48(1):27–33
Assayag J, Yin H, Benayoun S, Pollak MN, Suissa S, Azoulay L (2013) Androgen deprivation therapy and the risk of colorectal cancer in patients with prostate cancer. Cancer Causes Control 24(5):839–845
Gillessen S, Templeton A, Marra G, Kuo YF, Valtorta E, Shahinian VB (2010) Risk of colorectal cancer in men on long-term androgen deprivation therapy for prostate cancer. J Natl Cancer Inst 102(23):1760–1770
Chan AT, Giovannucci EL (2010) Primary prevention of colorectal cancer. Gastroenterology 138(6):2029–43e10
Grundmark B, Garmo H, Zethelius B, Stattin P, Lambe M, Holmberg L (2012) Anti-androgen prescribing patterns, patient treatment adherence and influencing factors; results from the nationwide PCBaSe Sweden. Eur J Clin Pharmacol 68(12):1619–1630
Davis EJ, Beebe-Dimmer JL, Yee CL, Cooney KA (2014) Risk of second primary tumors in men diagnosed with prostate cancer: a population-based cohort study. Cancer 120(17):2735–2741
Ko SH, Baeg MK, Bae WJ, Kim P, Choi MG (2016) Prostate cancer patients may have an increased risk of coexisting advanced colorectal neoplasms. Onco Targets Ther 9:5611–5617
Van Hemelrijck M, Feller A, Garmo H, Valeri F, Korol D, Dehler S et al (2014) Incidence of second malignancies for prostate cancer. PLoS ONE 9(7):e102596
Desautels D, Czaykowski P, Nugent Z, Demers AA, Mahmud SM, Singh H (2016) Risk of colorectal cancer after the diagnosis of prostate cancer: a population-based study. Cancer 122(8):1254–1260
Bae S, Asadi M, Jones I, McLaughlin S, Bui A, Steele M et al (2013) Second primary colorectal cancer in the era of prevalent screening and imaging. ANZ J Surg 83(12):963–967
Van Hemelrijck M, Drevin L, Holmberg L, Garmo H, Adolfsson J, Stattin P (2012) Primary cancers before and after prostate cancer diagnosis. Cancer 118(24):6207–6216
Koo JH, Leong RW (2010) Sex differences in epidemiological, clinical and pathological characteristics of colorectal cancer. J Gastroenterol Hepatol 25(1):33–42
Hang D, He X, Kværner AS, Chan AT, Wu K, Ogino S et al (2021) Plasma sex hormones and risk of conventional and serrated precursors of colorectal cancer in postmenopausal women. BMC Med 19(1):18
Dimou N, Mori N, Harlid S, Harbs J, Martin RM, Smith-Byrne K et al (2021) Circulating levels of testosterone, sex hormone binding globulin and colorectal Cancer risk: observational and mendelian randomization analyses. Cancer Epidemiol Biomarkers Prev 30(7):1336–1348
Hyde Z, Flicker L, McCaul KA, Almeida OP, Hankey GJ, Chubb SA et al (2012) Associations between testosterone levels and incident prostate, lung, and colorectal cancer. A population-based study. Cancer Epidemiol Biomarkers Prev 21(8):1319–1329
Peila R, Arthur RS, Rohan TE (2020) Sex hormones, SHBG and risk of colon and rectal cancer among men and women in the UK Biobank. Cancer Epidemiol 69:101831
Bouras E, Papandreou C, Tzoulaki I, Tsilidis KK (2021) Endogenous sex steroid hormones and colorectal cancer risk: a systematic review and meta-analysis. Discover Oncol 12(1):8
Castagnetta L, Traina A, Campisi I, Calabro M, Maratta A, Saetta A et al (2002) Androgen receptor status in nontumoral and malignant human colorectal tissues. Ann N Y Acad Sci 963:322–325
Meggouh F, Lointier P, Saez S (1991) Sex steroid and 1,25-dihydroxyvitamin D3 receptors in human colorectal adenocarcinoma and normal mucosa. Cancer Res 51(4):1227–1233
Aoki K, Nakajima A, Mukasa K, Osawa E, Mori Y, Sekihara H (2003) Prevention of diabetes, hepatic injury, and colon cancer with dehydroepiandrosterone. J Steroid Biochem Mol Biol 85(2–5):469–472
Izbicki JR, Hamilton SR, Wambach G, Harnisch E, Wilker DK, Dornschneider G et al (1990) Effects of androgen manipulations on chemically induced colonic tumours and on macroscopically normal colonic mucosa in male Sprague-Dawley rats. Br J Cancer 61(2):235–240
Rao CV, Tokumo K, Rigotty J, Zang E, Kelloff G, Reddy BS (1991) Chemoprevention of colon carcinogenesis by dietary administration of piroxicam, alpha-difluoromethylornithine, 16 alpha-fluoro-5-androsten-17-one, and ellagic acid individually and in combination. Cancer Res 51(17):4528–4534
Krasanakis T, Nikolouzakis TK, Sgantzos M, Mariolis-Sapsakos T, Souglakos J, Spandidos DA et al (2019) Role of anabolic agents in colorectal carcinogenesis: myths and realities (review). Oncol Rep 42(6):2228–2244
Pais R, Silaghi H, Silaghi AC, Rusu ML, Dumitrascu DL (2009) Metabolic syndrome and risk of subsequent colorectal cancer. World J Gastroenterol 15(41):5141–5148
Giovannucci E, Michaud D (2007) The role of obesity and related metabolic disturbances in cancers of the colon, prostate, and pancreas. Gastroenterology 132(6):2208–2225
Basaria S (2008) Androgen deprivation therapy, insulin resistance, and cardiovascular mortality: an inconvenient truth. J Androl 29(5):534–539
Slattery ML, Ballard-Barbash R, Edwards S, Caan BJ, Potter JD (2003) Body mass index and colon cancer: an evaluation of the modifying effects of estrogen (United States). Cancer Causes Control 14(1):75–84
Giovannucci E (2001) Insulin, insulin-like growth factors and colon cancer: a review of the evidence. J Nutr 131(11 Suppl):3109s–20s
Gandaglia G, Leni R, Bray F, Fleshner N, Freedland SJ, Kibel A et al (2021) Epidemiology and Prevention of prostate Cancer. Eur Urol Oncol 4(6):877–892
Roddam AW, Allen NE, Appleby P, Key TJ, Ferrucci L, Carter HB et al (2008) Insulin-like growth factors, their binding proteins, and prostate cancer risk: analysis of individual patient data from 12 prospective studies. Ann Intern Med 149(7):461–471 w83-8
Brandstedt J, Wangefjord S, Nodin B, Gaber A, Manjer J, Jirstrom K (2012) Gender, anthropometric factors and risk of colorectal cancer with particular reference to tumour location and TNM stage: a cohort study. Biol Sex Differ 3(1):23
Lin JH, Giovannucci E (2010) Sex hormones and colorectal cancer: what have we learned so far? J Natl Cancer Inst 102(23):1746–1747
Acknowledgements
The authors would like to express their thanks to all staff involved in PCBaSe and to all patients for allowing their data to be used for research purposes. This project was also made possible by the continuous work of the National Prostate Cancer Register of Sweden (NPCR) steering group: Pär Stattin (chair), Ingela Franck Lissbrant (co-chair), Camilla Thellenberg, Johan Styrke, Hampus Nugin, Stefan Carlsson, David Robinson, Mats Andén, Johan Stranne, Jon Kindblom, Thomas Jiborn, Olof Ståhl, Maria Nyberg, Fredrik Sandin, Karin Hellström, Hans Joelsson and Gert Malmberg.
Funding
This study was funded by the Swedish Cancer Society (grant number 180787).
Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Ji Zhang, Richard Shore, Pär Stattin and Mats Lindblad. The first draft of the manuscript was written by Richard Shore and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest/Competing interests
The authors declare that they have no conflict of interest.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. The study was approved by the Ethical Review Board in Stockholm, Sweden (DNR: 2009/1196-31/1 with amendments DNR: 2009/2124-32 and DNR: 2011/1674-32).
Consent to participate
Not applicable since all results were yielded in the analysis of anonymized data.
Consent for publication
Not applicable since all results were yielded in the analysis of anonymized data.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shore, R., Zhang, J., Ye, W. et al. Risk of colorectal adenocarcinoma in men receiving androgen deprivation therapy for prostate cancer; a nationwide cohort study. Cancer Causes Control 34, 949–961 (2023). https://doi.org/10.1007/s10552-023-01736-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-023-01736-5