Abstract
Purpose
The causes for the survival disparity among Black women with epithelial ovarian cancer (EOC) are likely multi-factorial. Here we describe the African American Cancer Epidemiology Study (AACES), the largest cohort of Black women with EOC.
Methods
AACES phase 2 (enrolled 2020 onward) is a multi-site, population-based study focused on overall survival (OS) of EOC. Rapid case ascertainment is used in ongoing patient recruitment in eight U.S. states, both northern and southern. Data collection is composed of a survey, biospecimens, and medical record abstraction. Results characterizing the survival experience of the phase 1 study population (enrolled 2010–2015) are presented.
Results
Thus far, ~ 650 patients with EOC have been enrolled in the AACES. The five-year OS of AACES participants approximates those of Black women in the Surveillance Epidemiology and End Results (SEER) registry who survive at least 10-month past diagnosis and is worse compared to white women in SEER, 49 vs. 60%, respectively. A high proportion of women in AACES have low levels of household income (45% < $25,000 annually), education (51% ≤ high school education), and insurance coverage (32% uninsured or Medicaid). Those followed annually differ from those without follow-up with higher levels of localized disease (28 vs 24%) and higher levels of optimal debulking status (73 vs 67%).
Conclusion
AACES is well positioned to evaluate the contribution of social determinants of health to the poor survival of Black women with EOC and advance understanding of the multi-factorial causes of the ovarian cancer survival disparity in Black women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The five-year relative survival for ovarian cancer is worse for Black women, at 41%, when compared with White women, at 48% [1]. After stratifying on stage at diagnosis, survival is worse in Black women compared to any other racial group for both early- and late-stage disease [2]. Factors affecting epithelial ovarian cancer (EOC) prognosis are under-studied among Black women despite notable differences in age at diagnosis, clinical-pathological features, and survival compared to White women [3]. The causes for this survival disparity are most likely multi-factorial.
Social determinants of health could contribute to poorer survival in Black women. Lower socioeconomic status (SES), with limited access to care, may lead to more advanced stage at diagnosis and receipt of suboptimal treatment [4]. Social determinants of health can also contribute to individual-level susceptibility factors that lead to poorer prognosis, such as higher prevalence of comorbidities and a higher inflammatory response [5, 6]. A pooled analysis from the Ovarian Cancer in Women of African Ancestry (OCWAA) consortium suggested that several factors including reproductive factors, comorbid conditions, and hormone use appear to mediate ovarian cancer survival differences between Black and White women [7].
To date, no cohort study has focused on Black EOC survivors. Here we present the African American Cancer Epidemiology Study (AACES) [8], the largest cohort of Black women with EOC residing in several U.S. states where we will further explore why EOC survival is poor among Black women. We are pursuing a society to cell approach (Fig. 1), facilitated through multi-level modeling, to address effects at different levels: social determinants of health at the neighborhood and census tract levels that may contribute to disparities in ovarian cancer survival (i.e., deprivation and segregation indices); individual-level factors such as inflammatory-related lifestyle exposures factors, factors known to be associated with cancer survival (e.g., cigarette smoking), and social determinants of health such as socioeconomic status and measures of structural racism (i.e., trust in physicians and perceived discrimination); and tumor (e.g., stage) and cellular features (i.e., tumor immune microenvironment). In AACES we focus on inflammatory factors, given the strong role of inflammation in ovarian carcinogenesis and growing evidence of its role in prognosis [5].
Given its size, geographical diversity, and breadth of data, including biospecimens, the AACES cohort provides a unique resource to advance understanding of the multi-factorial causes of the ovarian cancer survival disparity in Black women. The intent of this paper is to provide a detailed roadmap to our approach in our ongoing, multi-site study of Black women diagnosed with EOC, a rare and highly fatal disease. After assessing risk factor associations in phase 1, our current study goals in phase 2 are focused on predictors of overall survival pursuing a multi-level society to cell approach to address effects at different levels. The role of the analysis in the current manuscript is descriptive, while future analyses will examine predictors of overall survival using a multi-level approach. For this reason, the methods section provides detailed information about the study design and conduct.
Methods
Study population
Phase 1 of the AACES was initiated in 2010 as a multi-site population-based, case–control study, described in detail elsewhere [8]. The study was designed to evaluate genetic and lifestyle risk factors for EOC in Black women, with the intention of also conducting follow-up of the participants to evaluate survival in future. Phase 2 of AACES, which began in 2020, builds upon the infrastructure developed in the AACES phase 1 and focuses on evaluating associations of multi-level factors (neighborhood, lifestyle, and biological factors) with overall survival (OS) of EOC using a prospective cohort design, which combines participants enrolled in AACES phase 1 and newly recruited participants in phase 2. The chosen study sites (Supplemental fig 1) [9] represent geographic diversity as well as an approach for an efficient means for accrual of minority women diagnosed with a rare cancer. Consideration was also given for the proportion of Black residents, the incidence rates of ovarian cancer, and the frequency of newly diagnosed cases of EOC within the geographic regions.
In phase 1, the study sites were selected based on geographic regions with high Black population density and included Alabama, Georgia, Louisiana, metropolitan Detroit, Illinois, New Jersey, North Carolina, Ohio, South Carolina, Tennessee, and Texas. Potential participants were eligible if they had histologically confirmed EOC, self-identified as African American or Black, were 20–79 years of age at diagnosis, and had the ability to complete the interview in English. Rapid case ascertainment was used to identify potential participants with newly diagnosed EOC through state cancer or Surveillance Epidemiology and End Results (SEER) registries and through gynecologic oncology departments at individual hospitals. Participants were recruited between December 2010 and 2015. The data presented in this paper are from women enrolled in phase 1. Based on the AACES phase 1 design and infrastructure, we are currently enrolling women newly diagnosed with invasive epithelial ovarian cancer in phase 2. Our goal is to increase the number of participants recruited in AACES by ~ 50% (n = 300 new participants) and focus on factors associated with OS. The data obtained from women enrolled in phase 2 will be used to annotate biospecimen data. Based on the enrollment in phase 1, we chose a subset of the sites for phase 2 with the largest number of enrolled participants, including the states of Georgia, New Jersey, Louisiana, South Carolina, North Carolina, Tennessee, and the Detroit metropolitan area. A new site, the Southern California SEER registry, is also included in phase 2. Four of the sites participating in phase 2, Georgia, New Jersey, Louisiana, and Southern California, are SEER registries. All sites employ rapid case ascertainment, described below. Informed consent was obtained from all individual participants included in the study. We have established a single IRB using the Western Institutional Review Board-Copernicus Group (WCG IRB) that all sites rely on.
In phase 2, we continue to incorporate the majority of survey questions and indices used in phase 1 to maximize our ability to pool data from the two phases of AACES. However, we have updated some survey questions when we determined improvement was required and added other constructs of interest that were not collected in phase 1, such as financial toxicity (Fig. 2). We now obtain information about genetic counseling in a population that has been shown to be deficient in BRCA1 and BRCA2 testing [10] and we obtain information concerning COVID 19, as phase 2 began during the beginning of the COVID 19 pandemic.
After passive approval from the physician, potential participants from Georgia, New Jersey, and South Carolina are contacted by their cancer registry by mail and by telephone. Participant approval (verbally or by mail) is required from these sites before their contact information is passed to the study team. Participants from California, Louisiana, North Carolina, and Tennessee do not require active approval from the patient to send participant contact information to the study team. Some hospitals in the Detroit metropolitan area require active physician approval before reaching out to the potential participant. This information is displayed in Table 1.
Enrollment and retention strategies
All potential study participants are mailed a packet of introductory material. Consent can be obtained verbally for the study survey, and written consent is obtained for other study activities. The study team reaches out to the participant to complete the food frequency questionnaires, the annual follow-up surveys, and making medical records requests and requests for paraffin-embedded tumor tissue samples. To mitigate obstacles when contacting participants, we implemented several strategies including an identifiable study logo. Additionally, a brochure that highlights aspects of study participation and compensations is mailed to each potential study participant. We also provide a website (https://aaces.emory.edu/) and a toll-free number to accommodate those who want more information. An informational one-page flyer is sent prior to initiating phone contact to alert the patient about the study, informing the patient that she will be contacted by phone. All telephone numbers that are involved with patient contact have a caller ID labeled as “AACES Study Office” or “AACES Study.”
Multiple call attempts are made to reach the potential participant at different times of the day including early evening and weekends. Study participants are given alternative options to complete the survey online or on a paper version if the baseline telephone interview does not offer a desired time commitment and flexibility. Newsletters are sent twice a year that includes recent publications, study updates, and educational materials on topics related to cancer survivorship. The newsletters help to maintain up-to-date contact information. A $50.00 compensation is paid to participants who complete the baseline survey.
Baseline and follow-up surveys
In phase 1, participants completed a baseline telephone survey that collected information on sociodemographic characteristics, medical history, self-reported family history of cancer, lifestyle characteristics [11], perceived daily and lifetime discrimination [12], social support [13, 14], religiosity [15], health insurance status, health care provider access, and trust in physicians [16]. For phase 2, some survey content was revised: social support was switched from the Multidimensional Scale of Perceived Social Support (MSPSS) [13] to the modified Medical Outcomes Study Social Support Survey (mMOS-SS) [14]. We also added additional questions to the phase 2 baseline survey including the Short Form Health Survey (SF-12 version 2) quality of life [17], the Pittsburgh sleep quality index [18], an index for financial toxicity [19], COVID 19 diagnosis, and vaccination, and questions pertaining to genetic testing and counseling (Fig. 2). Both phase 1 and phase 2 include a follow-up survey at approximately one year after baseline interview that addresses changes and updates such as changes in physical activity [11], employment, quality of life (SF-8 in phase 1 and SF-12 version 2 in phase 2) [17, 20], medication use, new diagnoses of cancer and other comorbid conditions in the participant and family members, and genetic counseling and testing. In phase 2, study data for baseline and follow-up surveys were collected and managed using Research Electronic Data Capture (REDCap) hosted at Emory University [21, 22]. The online and hardcopy version of the baseline survey has an abbreviated assessment of some factors including parity, oral contraceptive use, family history, access to care, and symptoms and provides flexibility for the participant who requests this option.
Geocoding and area-level variables
In order to link neighborhood-level variables, we use the participant’s residential address at diagnosis and geocode to latitude and longitude coordinates. These data can be linked to various levels of geospatial data related to indices of socioeconomic status and/or deprivation, environmental pollution, measures of access to care, and more [23,24,25,26,27,28]. This will enable a wider variety and scope of analyses in future using the AACES sample population.
Biospecimen collection
Upon receipt of a written informed consent, we initiate collection of biospecimens, including blood or saliva and tumor tissue. When blood or saliva is obtained, a second $50.00 compensation is paid. In both phases of AACES, we contracted with an outside vendor for blood or saliva collection and anthropometric measurements. If a participant is unwilling or contraindicated to give a blood sample, we offer the option to provide a saliva sample.
For participants who signed a specimen release form, study staff contacts the pathology department at the institution where the patient was diagnosed and request pathology reports and formalin-fixed paraffin-embedded (FFPE) tumor blocks that are representative of the primary ovarian cancer. Emory prepares 25 5-micron slides and selects three cores from the primary tissue to assemble tissue microarrays (TMAs). A pathology slide is prepared for each of the tissues received and stained with hematoxylin and eosin (H&E). Immunofluorescent staining of selected immune markers is in process for both phases [29]. We genotyped all study subjects enrolled in Phase 1 with an available germline DNA sample using the Illumina OncoArray [30]. In phase 2, we are considering using an array that better addresses genetic variation in minority populations [31].
Pathology criteria
Eligible participants for phase 2 were based on International Classification of Diseases for Oncology, 3rd Edition (ICD-O-3) site and morphology codes for EOC which incorporate 2021 updates in the WHO Classification of Tumors, 5th Edition, Volume 4: Female Genital Tumors (see Supplemental table 1). The eligible ICD-O cancer sites are ovary (C56.9), fallopian tube (C57.0), retroperitoneum (C48.0), specified parts of the peritoneum (C48.1), peritoneum (C48.2), overlapping lesions of retroperitoneum & peritoneum (C48.8), and overlapping lesions of female genital organs: tubo-ovarian (C57.8).
Medical record abstraction (acquisition and review)
All study participants in phases 1 and 2, diagnosed with EOC, are asked to sign a medical record release form and tumor tissue release form as well as the name of the institution where the diagnosis took place. Information on each participant’s frontline chemotherapy regimen (neoadjuvant and adjuvant, start and end date, name of agent, number of cycles, dose), debulking surgery (type, date), residual disease, debulking status, CA125 levels before and after adjuvant chemotherapy, white blood cell counts before surgery and treatment, and anthropometric measurements at initiation of chemotherapy is collected to the extent possible.
Follow-up and vital status collection
In phase 1 annual follow-up interviews were attempted to collect the information described above, as well as to capture any updates in contact information and length of OS. The goal for time between baseline interview and follow-up was one year. When follow-up interviews were not possible, a thorough search with the National Death Index was implemented to obtain date and cause of death where applicable. We are also in the process of using LexisNexis to further identify vital status and OS. We plan to continue these processes for phase 2.
Statistical analysis
Variable distribution
We generate descriptive statistics of our study population including basic demographics, clinical characteristics, and inflammatory-related factors that are displayed for all participants at baseline and by follow-up status, which was defined as completion of at least one follow-up survey or not. Demographics include variables, such as age at diagnosis, marital status (single/never married, married/living as married, divorced/separated, widowed), highest level of education achieved (high school or less, some college, college graduate, graduate/professional school), insurance status (uninsured, any Medicaid coverage, Medicare only, combination of private insurance & Medicare, private insurance, other), and total annual family income (< $10,000, $10,000–$24,999, $25,000–$49,999, $50,000–$74,999, $75,000–$100,000, > $100,000). Clinical characteristics included summary stage, FIGO stage, histotype, time between baseline and follow-up surveys (where available), residual disease (residual tumor diameter after cytoreductive debulking surgery; no residual disease, < 1 cm residual tumor diameter, ≥ 1 cm residual tumor diameter, residual disease but unknown size of tumor), and debulking status (optimal [no residual disease or < 1 cm residual tumor diameter], suboptimal [≥ 1 cm residual tumor diameter]); described in further detail below). Physical inactivity is classified into categories of < 2 h per week vs ≥ 2 h per week. Physical Activity Guidelines for Americans (PAGA) consider insufficient physical activity to be < 2.5 h of moderate activity or < 1.25 h of vigorous physical activity [32]. Other factors include aspirin and other non-steroidal anti-inflammatory drug (NSAID) use, body mass index (BMI, kg/m2), smoking status (never, former, current), talc use (ever vs never), oral contraceptive duration (never, < 5 years, ≥ 5 years), hormone replacement therapy duration (never, < 5 years, ≥ 5 years), parity (number of full-term pregnancies), prior diagnosis of breast cancer, prior diagnosis of any cancer, excluding breast cancer, and the Charlson comorbidity index [33]. Chi-squared tests of independence were used to compare the distributions of all variables by follow-up completion status, and the p-values are displayed.
Survival comparisons of AACES participants to SEER data
To better understand the population that is captured by AACES, we used SEER*Stat [34] to compare OS rates from our data to women diagnosed with ovarian cancer between 2008 and 2013 for sufficient sample size and a comparative length of follow-up time. We standardized Kaplan–Meier estimates from Black women in SEER to the AACES age distribution. After fitting several conditional curves based on surviving past specific time points, we determined the OS proportions for Black women within SEER data conditioning on at least 10 months of OS post-diagnosis to account for the low response rates among the sickest women and those with aggressive disease. Additionally, to assess the racial disparity related to OS in our study population we determined the same set of conditional age-standardized Kaplan–Meier estimates for White women. A log-Rank test is used to compare the conditional age-standardized Kaplan–Meier curves from SEER between Black and White women.
We determined age-standardized Kaplan–Meier estimates for the five major histotypes: high-grade serous, low-grade serous, mucinous, clear cell, and endometrioid. Here we also conditioned on at least 10-month OS time to enable comparison of the overall population of Black women with ovarian cancer and the AACES study participants. We also used a Chi-squared test of independence to formally compare the distribution of histotypes in SEER to the distribution within AACES.
Results
Of 1,720 potential participants interviewers attempted to contact, 1,199 (70%) were actively reached. Of these, 592 (49%) were interviewed and 388 (32%) actively refused. Using rapid case ascertainment, the average and median time from diagnosis to the baseline survey interview for participants in phase 1 were 7.1 and 5.8 months, respectively. Among the 592 patients in phase 1, 540 agreed to provide their medical record and tissue sample (91%). Of these, 497 medical records were obtained (92%) and 437 FFPE tumor tissue samples (81%) were obtained. Phase 1 participants have been followed annually through 2016 and again in 2021, with 228 (39%) participants who remain alive and 364 (61%) participants deceased as of the latest update in 2021. For all women with EOC, OS ranged from 0.5 years to 10.6 years with a median of 4.8 years. A total of 577 (97%) participants survived at least 10-month past diagnosis. The mean and median time to the first follow-up survey was 1.6 and 1.2 years, respectively. Participants with 2 or more follow-up survey completions (n = 104) had an average time to first follow-up of 1.3 years (median: 1.2 years).
The participants who did not complete any follow-up survey (n = 294) are further described according to whether they died before being contacted or rather were lost to follow-up. During phase 1, interviewing ended in April 2016 and therefore, 70 (24%) participants who were interviewed at baseline in April 2015 or later were not eligible to complete follow-up surveys until phase 2 had begun but were deceased upon the start of phase 2. An additional 67 (23%) participants who did not complete a follow-up survey died within a year of their baseline interview over the course of phase 1 and 157 (53%) did not complete a follow-up survey due to other reasons (i.e., no answer on the phone, phone number no longer in service, active refusal, passive refusal).
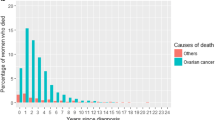
As shown in Table 2, AACES phase 1 participants demonstrated better OS than age-standardized Black women in SEER but were virtually the same after conditioning on OS of at least 10 months. Comparing OS of this age-standardized group of Black women in SEER to that of age-standardized White women in SEER (when looking at unrestricted OS and when conditioning on at least a 10-month OS time), Black women have consistently poorer OS (p-value < 0.0001) (Fig. 3).
Survey results
Characteristics of the phase 1 participants in AACES are summarized in Table 3. Due to some participants opting to complete an abbreviated version of the survey, variables not included in this version, such as insurance status and annual family income, are missing at higher rates (n = 51; 9%). The highest level of education of approximately half of the participants was high school or less (51%), almost half reported a total family income of less than $24,999 annually (45%), one-third of participants were married or living as married (33%), close to one-third of participants were uninsured or had Medicaid coverage (32%), and a further 23% of participants had only Medicare coverage (Table 3). Among women reporting the lowest annual family income in phase 1 (< $10,000), participants were more likely to have Medicaid or no insurance (63%), and have a high school education or less (77%). There were no clear differences in SES-related factors and other basic demographic characteristics by women who completed at least one follow-up survey and those who did not. However, participants who were deceased before the follow-up survey were older at diagnosis than those who could not be followed for other reasons, with a mean age of 61 years (SD = 10.8) compared to 55 years (SD = 11.2) (p < 0.001), respectively.
Overall, almost a quarter of AACES participants had high Charlson scores (≥ 3 weighted score, 24%), more than half reported being obese (BMI one year prior to diagnosis ≥ 30 kg/m2, 59%), more than half reported never smoking (55%), almost two-thirds reported previous talc use (63%), almost two-thirds reported less than two h of physical activity per week (62%), the majority reported never using post-menopausal hormones (83%), and the majority reported ever using oral contraceptives (70%) (Table 3). Of note, obesity did not differ according to participation in the follow-up survey (Table 3). Those who did not participate in the follow-up survey were more likely to report they were a current smoker and less likely to have never smoked compared to those who participated in at least one follow-up survey (current: 37 vs 32%; never: 51 vs 59%) (Table 3). Participants who were deceased before follow-up were more likely to have higher scores on the Charlson comorbidity index than those who were lost to follow-up for other reasons, with 70 and 61% reporting a non-zero Charlson score, respectively (p = 0.086).
Clinical, tumor, and genetic data
The distribution of the tumor characteristics including stage at diagnosis and histotype is shown in Table 3. Most participants were diagnosed at FIGO stage III/IV (63%) and most had high-grade serous tumors (68%). The least common histotypes were low-grade serous (3%) and carcinosarcoma (3%). Those who completed at least one follow-up survey were less likely to have stage III/IV disease compared to those who did not participate, 61 vs 66%, respectively. When comparing participants who completed at least one follow-up survey to those who did not complete a follow-up survey, participants were slightly more likely to be diagnosed with FIGO stage I disease, 27 vs 24%, respectively, and slightly less likely to be diagnosed with FIGO stage IV disease, 16 vs 21%, respectively. The distribution of histologic subtypes was similar across the baseline and follow-up groups, with most women having high-grade serous ovarian cancer.
Half of the women with high-grade serous ovarian cancer who were lost to follow-up were deceased at the first attempt of follow-up (50%), and this was the highest rate among the five major histotypes. Similarly, approximately half of the women diagnosed at FIGO stage III/IV were lost to follow-up because they were deceased at the first attempt to contact (51%). More than half of participants who had suboptimal debulking were lost to follow-up because they were deceased at the first attempted contact (56%).
The proportion of the five major histotypes among participants in AACES compared to the proportion in SEER data for Black women, respectively, are similar: 75.9 vs 77.8% high-grade serous ovarian, 3.3 vs 2.7% low-grade serous, 10.9 vs 7.4% endometrioid, 4.4 vs 4.6% clear cell, and 5.5 vs 7.5% mucinous (p > 0.10). Supplemental fig 1 shows Kaplan–Meier OS curves by the five major histotypes in AACES and in SEER. The poorest OS is seen for women with high-grade serous ovarian cancer, while women with endometrioid tumors have the best OS. To date in AACES, more than two-thirds of women who were diagnosed with high-grade serous ovarian cancer are deceased (69%), compared with approximately one-fifth of women diagnosed with endometrioid ovarian cancer (19%). When comparing these to the Kaplan–Meier estimates from SEER data, we see similar OS for women with high-grade serous, mucinous, and endometrioid cancers.
Twelve participants did not receive debulking surgery. Information on residual disease/debulking status was available on 340 participants (59%). Among women who were missing this information and whose CA125 level at the end of adjuvant chemotherapy was used as a proxy for debulking status (n = 43), 32 women were classified as having optimal debulking (CA125 < 35 units/mL) and 11 women were classified as having suboptimal debulking (CA125 ≥ 35 units/mL). By incorporating CA125 levels, information on debulking status was available on 383 participants (65%) and the missing data were reduced to 209 participants (35%). At baseline, approximately one-third of the participants had any residual disease, while one-third had no gross residual disease. Comparing participants by follow-up survey completion, women who completed at least one follow-up survey were more likely to have no residual disease. Optimal debulking status, which is correlated with residual disease, was also highest among those who participated in at least one follow-up survey.
No information on residual disease was recorded for approximately one-third of the participants. In Supplemental fig 3, we also show that the OS curve among those with missing debulking status fell in-between those whose debulking status was either optimal or suboptimal. Participants with optimal, suboptimal, and missing debulking status have a median OS of 7.1, 3.0, and 4.9 years, respectively. This suggests that data were missing at random with respect to debulking status and therefore imputation of the missing data would likely be unbiased. Using Cox proportional hazards analysis, we find a similar hazard ratio (HR) for the complete case group analysis (HR = 0.43; 95% CI = 0.32, 0.60) compared with the estimate computed using multiple imputation (HR = 0.46; 95% CI = 0.36, 0.60).
AACES has contributed significantly and will continue to contribute to the genetic susceptibility and tumor biomarker research of ovarian cancer in Black women. Our GWAS findings were reported by Manichaikul et al. [35] suggesting similarities and differences in genetic association in Black compared to White women. Initial results from multiplex immunofluorescence staining of immune markers and OS of Black women in AACES are found in Peres et al. [36] and show an attenuated inverse association with survival in Black compared to White women with EOC.
Discussion
Here we describe a multi-level approach to determine associations between epithelial ovarian cancer survival and factors associated with the social and built environment, individual patient characteristics, and the tumor immune microenvironment with the goal to examine the full spectrum of exposure variables and clinical factors to help characterize the “whole person.” Our scientific rationale is based on the premise that multiple factors contribute to the poor survival of ovarian cancer among Black women compared with other racial and ethnic groups and that many of these factors have a synergistic relationship or mediate the relationship with inflammatory and immune processes. We will be using multi-level modeling to address different effects identified at different levels: individual, neighborhood, and census tract that will be used to formulate a general multi-level model for survival experience [37,38,39].
The purpose of the study is to generate needed evidence to address the racial disparity in EOC survival. Most large medical claims databases examining racial and ethnic differences in ovarian cancer survival lack information on lifestyle behaviors and beliefs that may be key to the interactions with the health care system. AACES provides a rigorously designed and truly unique resource to achieve our goal of understanding factors that influence mortality to better understand why Black women experience worse survival after a diagnosis of EOC. AACES integrates key data that will address this critical evidence gap and provide a major step forward in understanding multi-level predictors of poor EOC prognosis in Black women. The resulting evidence will inform translational strategies to reduce this racial disparity. To illustrate this point, we recently published a paper based on AACES phase 1 participants that showed perceived everyday discrimination was associated with prolonged symptom duration, whereas more commonly evaluated determinants of access to care and trust in physicians were not [40].
A major strength of AACES is that participants reside in over 12 geographic regions in the U.S., both in the east and west coast as well as southern and northern regions. With substantial proportions of the cohort having relatively low levels of household income, education, and insurance coverage, AACES will be well positioned to assess the contribution of social determinants of health to the racial disparity in ovarian cancer survival. Our biospecimen collection represents an unprecedented number of well-annotated specimens and an important resource for the molecular characterization of EOC diagnosed in Black women.
Related to social determinants of health, this cohort is also characterized by a high prevalence of obesity and comorbidities. A large study exploring racial and ethnic disparities found that 36% of Non-Hispanic White women are obese, while 59% of Non-Hispanic Black women are obese [41]. This prevalence of obesity in Black EOC cases is equivalent to the proportion found in our population. In another study using data from the National Health Interview Study (NHIS), the rates of multiple comorbidities are roughly similar to that in the AACES. When age adjusting their estimates, approximately 66% of Non-Hispanic Black women reported either having zero or one comorbidities, while approximately 74% of Non-Hispanic White women reported having 0 or 1 comorbidities [42]. While this raw count is not strictly comparable to the Charlson comorbidity index (some more severe comorbidities are weighted > 1), 60% of the women in our sample have a Charlson score of zero or one. This is naturally a slight undercount of number of comorbidities, so it makes sense for this proportion to fall under that of the general population.
The distribution of the variables related to social determinants of health along with the high prevalence of factors such as obesity and comorbidities that lead to worse prognosis will enable the AACES to generate needed evidence on the role that these factors, alone and in combination, that contribute to Black women having the lowest survival from ovarian cancer. Integrating information such as mentioned above related to perceived discrimination will further enrich the insights that can be gained in this patient population.
The distribution variables such as income, education, and insurance point to a generally lower SES. Having a lower SES may lead to diagnostic delay and less access to treatment after diagnosis, both of which can have impacts on cancer survival [43]. These effects can come from both the individual and the neighborhood level, so a multi-level approach that the wide variety of data collected within AACES will be key to fully evaluate these relationships.
Comparisons of the survival of women with EOC in phase 1 of AACES to that in the SEER database suggests that AACES phase 1 participants are representative of those who survive at least 10 months since their diagnosis. Therefore, our study population may underrepresent the sickest patients diagnosed with EOC. When conditioning on having survived at least 10 months, the survival among Black women in AACES is worse compared to White women diagnosed with EOC in the SEER database. Due to these findings, inferences from the AACES results will likely not be as generalizable to women with the most severe disease. The appearance of poorer low-grade serous ovarian cancer survival and better clear cell ovarian cancer survival in the AACES sample may be due to the small number of women with these histotypes in AACES. Some of this could also be due to differences in stage at diagnosis. Due to the underrepresentation of the sickest patients diagnosed with EOC, women diagnosed with clear cell tumors at a later stage and poorer prognosis could be missing from the AACES sample.
We compared baseline data among women in AACES phase 1 who did or did not participate in at least one follow-up survey showing differences with those completing at least one follow-up survey being younger at diagnosis, having fewer comorbid conditions, being less likely to have ever smoked, having less distant stage disease at diagnosis, and having less residual disease after debulking surgery. The higher proportion of women who completed a follow-up survey reporting a previous breast cancer could be underrepresenting women who had more severe breast cancer and did not survive long enough to develop ovarian cancer. Approximately 50% of study subjects completed at least one follow-up survey and these women had a median survival of more than 6 years compared to less than 5 years for AACES 1 phase participants overall. In SEER, the median survival time among Black women with EOC is approximately 5 years. Therefore, women completing the follow-up survey are survivors of a highly fatal disease and overrepresent younger women with less severe disease and lower comorbidity burden. Nevertheless, AACES appears to have a similar survival experience compared to the few studies addressing ovarian cancer survival. A study from Australia reported an average follow-up of 7.3 years with only 45% alive after 5 years from diagnosis [44] and a recent cohort study of ovarian cancer patients in China reported a median follow-up time of 3.1 years [45], although these studies do not include Black women with EOC.
We will continue to improve our methods for accrual of patients. As funding for AACES phase 2 began in 2020, we will continue adapting our methods to accommodate ongoing COVID 19 pandemic challenges. Our findings will have the potential to shed light on the causes of the persistent racial disparities in EOC survival and provide strategies toward cancer health equity.
Data availability
The datasets generated during and/or analyzed during the current study are available on reasonable request, in accordance with NIH data sharing policy.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A (2022) Cancer statistics 2022. CA: cancer j clin 72(1):7–33. https://doi.org/10.3322/caac.21708
Peres LC, Schildkraut JM (2020) Racial/ethnic disparities in ovarian cancer research. Adv Cancer Res 146:1–21. https://doi.org/10.1016/bs.acr.2020.01.002
Schildkraut JM, Peres LC, Bethea TN, Camacho F, Chyn D, Cloyd EK, Bandera EV, Beeghly-Fadiel A, Lipworth L, Joslin CE, Davis FG, Moorman PG, Myers E, Ochs-Balcom HM, Setiawan VW, Pike MC, Wu AH, Rosenberg L (2019) Ovarian Cancer in Women of African Ancestry (OCWAA) consortium: a resource of harmonized data from eight epidemiologic studies of African American and white women. Cancer causes & control : CCC 30(9):967–978. https://doi.org/10.1007/s10552-019-01199-7
Kaufman M, Cruz A, Thompson J, Reddy S, Bansal N, Cohen JG, Wu Y, Vadgama J, Farias-Eisner R (2019) A review of the effects of healthcare disparities on the experience and survival of ovarian cancer patients of different racial and ethnic backgrounds. J cancer metas treat 5:13. https://doi.org/10.20517/2394-4722.2018.25
Peres LC, Hebert JR, Qin B, Guertin KA, Bandera EV, Shivappa N, Camacho TF, Chyn D, Alberg AJ, Barnholtz-Sloan JS, Bondy ML, Cote ML, Funkhouser E, Moorman PG, Peters ES, Schwartz AG, Terry PD, Schildkraut JM (2019) Prediagnostic proinflammatory dietary potential is associated with all-cause mortality among African-American women with high-grade serous ovarian carcinoma. J Nutr 149(9):1606–1616. https://doi.org/10.1093/jn/nxz098
Vrieling A, Kampman E (2010) The role of body mass index, physical activity, and diet in colorectal cancer recurrence and survival: a review of the literature. Am J Clin Nutr 92(3):471–490. https://doi.org/10.3945/ajcn.2010.29005
Harris HR, Guertin KA, Camacho TF, Johnson CE, Wu AH, Moorman PG, Myers E, Bethea TN, Bandera EV, Joslin CE, Ochs-Balcom HM, Peres LC, Rosenow WT, Setiawan VW, Beeghly-Fadiel A, Dempsey LF, Rosenberg L, Schildkraut JM (2022) Racial disparities in epithelial ovarian cancer survival: An examination of contributing factors in the Ovarian cancer in women of African Ancestry (OCWAA) consortium. Int J Cancer. https://doi.org/10.1002/ijc.34141 (Advance online publication)
Schildkraut JM, Alberg AJ, Bandera EV, Barnholtz-Sloan J, Bondy M, Cote ML, Funkhouser E, Peters E, Schwartz AG, Terry P, Wallace K, Akushevich L, Wang F, Crankshaw S, Moorman PG (2014) A multi-center population-based case-control study of ovarian cancer in African-American women: the African American cancer epidemiology study (AACES). BMC Cancer 14:688. https://doi.org/10.1186/1471-2407-14-688
U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on 2020 submission data (1999–2018): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; www.cdc.gov/cancer/dataviz, released in June 2021.
McBride CM, Pathak S, Johnson CE, Alberg AJ, Bandera EV, Barnholtz-Sloan JS, Bondy ML, Cote ML, Moorman PG, Peres LC, Peters ES, Schwartz AG, Terry PD, Schildkraut JM (2022) Psychosocial factors associated with genetic testing status among African American women with ovarian cancer: results from the African American cancer epidemiology study. Cancer 128(6):1252–1259. https://doi.org/10.1002/cncr.34053
International Physical Activity Questionnaire (2016) Accessed Jan 15 2016 https://sites.google.com/site/theipaq/.
Sternthal SN, Williams DR (2011) Racial disparities in health: how much does stress really matter? Du Bois Rev 8:95–113. https://doi.org/10.1017/S1742058X11000087
Zimet GD, Dahlem NW, Zimet SG, Farley GK (1988) The multidimensional scale of perceived social support. J Pers Assess 52:30–41. https://doi.org/10.1207/s15327752jpa5201_2
Moser A, Stuck AE, Silliman RA, Ganz PA, Clough-Gorr KM (2012) The eight-item modified medical outcomes study social support survey: psychometric evaluation showed excellent performance. J Clin Epidemiol 65(10):1107–1116. https://doi.org/10.1016/j.jclinepi.2012.04.007
Lannin DR, Mathews HF, Mitchell J, Swanson MS, Swanson FH, Edwards MS (1998) Influence of socioeconomic and cultural factors on racial differences in late-stage presentation of breast cancer. JAMA 279:1801–1807. https://doi.org/10.1001/jama.279.22.1801
Anderson LA, Dedrick RF (1990) Development of the trust in physician scale: a measure to assess interpersonal trust in patient-physician relationships. Psychol Rep 67(3 pt 2):1091–1100. https://doi.org/10.2466/pr0.1990.67.3f.1091
Ware J., Kosinski M., Turner-Bowker D., et al. QualityMetric Incorporated; Lincoln, RI: 2002. SF12v2: How to Score Version 2 of the SF-12 Health Survey.
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213. https://doi.org/10.1016/0165-1781(89)90047-4
de Souza JA, Yap BJ, Wroblewski K, Blinder V, Araújo FS, Hlubocky FJ, Nicholas LH, O’Connor JM, Brockstein B, Ratain MJ, Daugherty CK, Cella D (2017) Measuring financial toxicity as a clinically relevant patient-reported outcome: the validation of the comprehensive score for financial toxicity (COST). Cancer 123(3):476–484. https://doi.org/10.1002/cncr.30369
Ware JE, Kosinski M, Dewey JE, Gandek B (2001) How to Score and Interpret Single-Item Health Status Measures: A Manual for Users of the SF-8 Health Survey. Lincoln RI: QualityMetric Inc 15:10
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Harris PA, Taylor R, Minor BL, Elliot V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN, REDCap Consortium (2019) The REDCap consortium: building an international community of software partners. J biomed inform 95:103208. https://doi.org/10.1016/j.jbi.2019.103208
Yost K, Perkins C, Cohen R, Morris C, Wright W (2001) Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer causes control: CCC 12(8):703–711. https://doi.org/10.1023/a:1011240019516
Singh GK (2003) Area deprivation and widening inequalities in US mortality, 1969–1998. Am J Public Health 93(7):1137–1143. https://doi.org/10.2105/ajph.93.7.1137
Sampson RJ, Raudenbush SW, Earls F (1997) Neighborhoods and violent crime: a multilevel study of collective efficacy. Science (New York, NY) 277(5328):918–924. https://doi.org/10.1126/science.277.5328.918
United States Department of Agriculture. USDA ERS - Documentation. Accessed June 23, 2021. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/documentation
Kolak M, Bhatt J, Park YH, Padrón NA, Molefe A (2020) Quantification of Neighborhood-level social determinants of health in the Continental United States. JAMA Netw Open 3(1):e1919928. https://doi.org/10.1001/jamanetworkopen.2019.19928
Krieger N, Waterman PD, Spasojevic J, Li W, Maduro G, Van Wye G (2016) Public health monitoring of privilege and deprivation with the index of concentration at the extremes. Am J Public Health 106(2):256–263. https://doi.org/10.2105/AJPH.2015.302955
Hoyt CC (2021) Multiplex immunofluorescence and multispectral imaging: forming the basis of a clinical test platform for immuno-oncology. Front Mol Biosci 8:674747. https://doi.org/10.3389/fmolb.2021.674747
Phelan CM, Kuchenbaecker KB, Tyrer JP, Kar SP, Lawrenson K, Winham SJ, Dennis J, Pirie A, Riggan MJ, Chornokur G, Earp MA, Lyra PC Jr, Lee JM, Coetzee S, Beesley J, McGuffog L, Soucy P, Dicks E, Lee A, Barrowdale D, Pharoah P (2017) Identification of 12 new susceptibility loci for different histotypes of epithelial ovarian cancer. Nat Genet 49(5):680–691. https://doi.org/10.1038/ng.3826
Tamura K, Stecher G, Kumar S (2021) MEGA11: molecular evolutionary genetics analysis version 11. Mol Biol Evol 38(7):3022–3027. https://doi.org/10.1093/molbev/msab120
Cannioto RA, LaMonte MJ, Kelemen LE, Risch HA, Eng KH, Minlikeeva AN, Hong CC, Szender JB, Sucheston-Campbell L, Joseph JM, Berchuck A, Chang-Claude J, Cramer DW, DeFazio A, Diergaarde B, Dörk T, Doherty JA, Edwards RP, Fridley BL, Friel G, Moysich KB (2016) Recreational physical inactivity and mortality in women with invasive epithelial ovarian cancer: evidence from the ovarian cancer association consortium. Br J Cancer 115(1):95–101. https://doi.org/10.1038/bjc.2016.153
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–83. https://doi.org/10.1016/0021-9681(87)90171-8
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence—SEER Research Plus Data, 17 Registries, Nov 2021 Sub (2000–2019)—Linked To County Attributes—Total U.S., 1969–2020 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2022, based on the November 2021 submission.
Manichaikul A, Peres LC, Wang XQ, Barnard ME, Chyn D, Sheng X, Du Z, Tyrer J, Dennis J, Schwartz AG, Cote ML, Peters E, Moorman PG, Bondy M, Barnholtz-Sloan JS, Terry P, Alberg AJ, Bandera EV, Funkhouser E, Wu AH, African American Cancer Epidemiology Study (AACES) and the Ovarian Cancer Association Consortium (OCAC) (2020) Identification of novel epithelial ovarian cancer loci in women of African ancestry. Int j cancer 146(11):2987–2998. https://doi.org/10.1002/ijc.32653
Peres LC, Colin-Leitzinger C, Sinha S, Marks JR, Conejo-Garcia JR, Alberg AJ, Bandera EV, Berchuck A, Bondy ML, Christensen BC, Cote ML, Doherty JA, Moorman PG, Peters ES, Moran Segura C, Nguyen JV, Schwartz AG, Terry PD, Wilson CM, Fridley BL, Schildkraut JM (2022) Racial differences in the tumor immune landscape and survival of women with high-grade serous ovarian carcinoma. Cancer epidemiol biomark & prev: pub American Association Cancer Res cosponsored American Soc Prevent Oncol 31(5):1006–1016. https://doi.org/10.1158/1055-9965.EPI-21-1334
Carroll R, Lawson AB, Zhao S (2019) Temporally dependent accelerated failure time model for capturing the impact of events that alter survival in disease mapping. Biostatistics 20(4):666–680. https://doi.org/10.1093/biostatistics/kxy023
VanderWeele TJ (2011) Causal mediation analysis with survival data. Epidemiol (Cambridge, Mass) 22(4):582–585. https://doi.org/10.1097/EDE.0b013e31821db37e
Onicescu G, Lawson A, Zhang J, Gebregziabher M, Wallace K, Eberth JM (2017) Bayesian accelerated failure time model for space-time dependency in a geographically augmented survival model. Stat Methods Med Res 26(5):2244–2256. https://doi.org/10.1177/0962280215596186
Mullins MA, Peres LC, Alberg AJ, Bandera EV, Barnholtz-Sloan JS, Bondy ML, Funkhouser E, Moorman PG, Peters ES, Terry PD, Schwartz AG, Lawson AB, Schildkraut JM, Cote ML (2019) Perceived discrimination, trust in physicians, and prolonged symptom duration before ovarian cancer diagnosis in the African American cancer epidemiology study. Cancer 125(24):4442–4451. https://doi.org/10.1002/cncr.32451
Karnes JH, Arora A, Feng J, Steiner HE, Sulieman L, Boerwinkle E, Clark C, Cicek M, Cohn E, Gebo K, Loperena-Cortes R, Ohno-Machado L, Mayo K, Mockrin S, Ramirez A, Schully S, Klimentidis YC (2021) Racial, ethnic, and gender differences in obesity and body fat distribution: an all of us research program demonstration project. PLoS ONE 16(8):e0255583. https://doi.org/10.1371/journal.pone.0255583
Ward BW, Schiller JS (2013) Prevalence of multiple chronic conditions among US adults: estimates from the national health interview survey, 2010. Prev Chronic Dis 10:E65. https://doi.org/10.5888/pcd10.120203
Peterson CE, Rauscher GH, Johnson TP, Kirschner CV, Barrett RE, Kim S, Fitzgibbon ML, Joslin CE, Davis FG (2014) The association between neighborhood socioeconomic status and ovarian cancer tumor characteristics. Cancer causes & control: CCC 25(5):633–637. https://doi.org/10.1007/s10552-014-0357-7
Nagle CM, Purdie DM, Webb PM, Green A, Harvey PW, Bain CJ (2003) Dietary influences on survival after ovarian cancer. Int J Cancer 106(2):264–269. https://doi.org/10.1002/ijc.11204
Jiang L, Gong TT, Gao S, Li XQ, Liu FH, Wen ZY, Wei YF, Yan S, Hou R, Wu QJ (2021) Pre-diagnosis dairy product intake and ovarian cancer mortality: results from the ovarian cancer follow-up study (OOPS). Front Nutr 8:750801. https://doi.org/10.3389/fnut.2021.750801
Acknowledgments
We would like to acknowledge the AACES interviewers, Brandy Arredondo, Rachel Boehm, Dannelle Charles, Melody Chavez, Lauren Dempsey, Kierstin Faw, Juliana Fucinari, Mary Kan, Mary Beth Kolbicz, Arianna Mason, Juana Paniagua, and Maelia Pendley. We also acknowledge the individuals responsible for facilitating case ascertainment across the sites, including Kevin Ward and Mackenzie Crawford (Georgia); Tingting Li and Lauren Maniscalco (Louisiana); Dhanya Chanumolu and Myneka Macenat (New Jersey); Paul Terry (Tennessee); Ann Hamilton (California), Mary Beth Kolbicz (Michigan); Cynthia Webb, JoElla Marting, and Heather Tipaldos (North Carolina); and Maxwell Akonde, Stephanie Chiodini, and Deb Hurley (South Carolina). Data collection was supported by the Rutgers Cancer Center Institue of New Jersey Cancer Prevention and Outcomes Data Support Shared Resouces.
Funding
The AACES study was funded by the National Cancer Institute (R01CA142081 & R01CA237318). Additional support was provided by Metropolitan Detroit Cancer Surveillance System (MDCSS) with federal funds from the National Cancer Institute, National Institute of Health, Dept. of Health and Human Services, under Contract No. HHSN261201000028C and the Epidemiology Research Core, supported in part by NCI Center Grant (P30CA22453) to the Karmanos Cancer Institute, Wayne State University School of Medicine. This work has been supported in part by the Participant Research, Interventions, and Measurements Core Facility at the H. Lee Moffit Cancer Center & Research Institute, an NCI designated Comprehensive Cancer Center (P30-CA076292).
Author information
Authors and Affiliations
Contributions
The following authors were a part of the writing group: JMS, LFD, CJ, AJA, PT, EVB, BQ, HM, MLC, MA, and ESP. The analysis was completed by CJ. The following authors provided comments and edits to the manuscript: LP, PM, AGS, ME, and ABL. The following authors helped in development of the surveys: PM and JMS. The following authors helped in data collection: JMS, AJA, PM, EVB, PT, MA, ESP, MLC, JM, MB, AGS, and HM.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was approved by the Western Institutional Review Board-Copernicus Group (WCG IRB).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schildkraut, J.M., Johnson, C., Dempsey, L.F. et al. Survival of epithelial ovarian cancer in Black women: a society to cell approach in the African American cancer epidemiology study (AACES). Cancer Causes Control 34, 251–265 (2023). https://doi.org/10.1007/s10552-022-01660-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-022-01660-0