Abstract
Purpose
Receptor and subtype discordance between primary breast tumours and metastases is a frequently reported phenomenon. The aim of this article is to review the current evidence on receptor discordance in metastatic breast cancer and to explore the benefit of performing a repeat biopsy in this context.
Methods
Searches were undertaken on PubMed and Clinicaltrials.gov for relevant publications and trials.
Conclusion
The current guidelines recommend offering to perform a biopsy of a metastatic lesion to evaluate receptor status. The choice of systemic therapy in metastatic disease is often based on the receptor status of the primary lesion. As therapeutic decision making is guided by subtype, biopsy of the metastatic lesion to determine receptor status may alter treatment. This article discusses discordance rates, the mechanisms of receptor discordance, the effect of discordance on treatment and survival outcomes, as well as highlighting some ongoing clinical trials in patients with metastatic breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer and the second leading cause of cancer-related mortality among women worldwide. Despite advances in treatment, approximately 30% of patients diagnosed with early-stage breast cancer develop metastases during their lifetime [1]. Breast cancer is subtyped into different molecular groups based on immunohistochemistry (IHC) testing for the expression of the two hormone receptors: estrogen receptor (ER) and progesterone receptor (PR) along with human epidermal growth factor receptor 2 (HER2) from formalin fixed paraffin embedded (FFPE) tissue samples taken from core biopsy of the primary breast tumour [2, 3]. The ER, PR and HER2 status of the tumour are used to individualise treatment strategies in breast cancer [4]. The choice of systemic therapy in metastatic disease is often based on the receptor status of the primary lesion. However, discordances between the receptor status of the primary tumour and metastases occur [5,6,7,8,9]. As therapeutic decision making is guided by subtype, biopsy of the metastatic lesion to determine receptor status may alter treatment [10, 11]. Thus, current guidelines recommend offering biopsy of a metastatic lesion to evaluate receptor status [4, 12,13,14]. This review will discuss the rates of receptor discordance and its clinical significance.
Discordance rates
Receptor discordance in metastatic breast cancer describes the phenomena where the ER, PR or HER2 receptor status of the primary tumour subtype has changed when re-testing is performed by immunohistochemistry on the biopsy of corresponding metastatic tumour tissue. Receptor discordance between primary breast cancer and metastases has been investigated in two independent meta-analyses [6, 15]. Aurilio et al. evaluated the discordance rates for ER, PR and HER2 receptors in a total of 9926 tumours across 48 studies. The pooled discordance proportions for ER, PR and HER2 receptors were 20%, 33% and 8%, respectively [6]. A similar meta-analysis performed by Schrijver et al. had comparable results, with discordance rates analysed in 6118 tumours across 39 studies. They reported the pooled discordances rates for ER, PR and HER2 receptors as 19.3%, 30.9% and 10.3%, respectively. This study also reported the direction of conversion, as well as location-specific differences between metastases. The positive-to-negative conversion rates for ER, PR and HER2 were 22.5%, 49.4% and 21.3%, respectively. The negative-to-positive conversion rates for ER, PR and HER2 were 21.5%, 15.9% and 9.5%, respectively. In addition, ER discordance rates were higher in bone (29.3%) and brain (20.8%) than in liver (14.3%) metastases. PR discordance rates were higher in liver (47%) and bone (42.7%) than in brain (23.3%) metastases. No statistically significant differences were observed in HER2 discordance rates between metastatic sites [15].
Intrinsic molecular subtype switching
In addition to receptor discordance by ER, PR and HER2 IHC status, several next generation sequencing (NGS) studies have also reported frequent intrinsic molecular subtype switching in breast cancer [16,17,18,19,20]. Intrinsic molecular subtyping is typically assigned using the PAM50 gene expression based classifier on RNA sequencing data from breast tumours [21, 22]. The intrinsic molecular subtypes are Luminal A, Luminal B, HER2-enriched (HER2-E), basal-like and normal-like. Some studies have reported the clinical subtype by IHC does not completely overlap with the intrinsic molecular subtype by NGS indicating that subtype switching may be more frequent than if only reporting on receptor discordance by IHC [16, 20, 23].
Cejalvo et al. performed targeted gene expression profiling of 123 paired primary and metastatic tumours enriched for skin, lymph node, liver and bone metastases [17]. The rate of intrinsic subtype switching identified was 55.3% in Luminal A, 30% in Luminal B, 23.1% in HER2-E and 0% in basal-like tumours. Similar to ER and PR IHC status discordance rates, subtype switching was more frequent in Luminal type tumours with 40.2% of Luminal A switched to Luminal B while 14.3% of Luminal A/B switched to HER2-E tumours. In a larger more recent NGS study of paired primary tumours and early-course (de novo) metastases enriched for liver, lymph node, skin and soft tissue metastases, Afitmos et al. reported intrinsic subtyping switching occurred in 36% of cases with most Luminal A primary breast tumours changing subtype with metastatic disease [16]. Comparable Luminal A to Luminal B or HER2-E subtype switching rates have been reported in gene expression studies of breast cancer site specific metastases including bone or brain metastases. Priedigkeit et al. had reported in ~ 36% (4/11) cases of ER+ breast cancer Luminal A to Luminal B intrinsic subtype switching in bone metastasis [24]. In breast cancer brain metastases, recurrent gene expression losses in ESR1 (ER) and gene expression gains in ERBB2 (HER2) have been attributed to Luminal (ER+) intrinsic subtype switching [18, 19]. Consistent with this, Cosgrove et al. reported intrinsic molecular subtype switching from primary breast to brain metastases for 27% (12/45) of cases, with 8 Luminal A patients switching to either Luminal B, HER2-E or basal-like subtype; 2 patients switching from normal-like or Luminal B to HER2-E and 2 patients with HER2-E or Luminal A to basal-like subtype [20].
Effect of discordance on treatment and survival outcomes
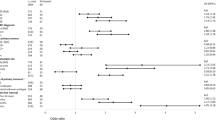
There is conflicting data in the literature with regards to alterations in management and the survival benefit of performing a repeat biopsy of metastases. The majority of studies examining this benefit are small retrospective analyses with variability in laboratory techniques and definitions of recurrence [11, 25,26,27]. To address these limitations, two independent prospective studies were carried out—the DESTINY study[28] and the BRITS study [29]. A pooled analysis of these studies evaluated the clinical impact of performing biopsy of metastatic breast cancer, specifically assessing the proportion of patients who underwent a change in management based on the biopsy results [30]. Of the 289 patients who underwent biopsy of the metastasis, 14.2% had a change in management based on the results. However, these studies failed to definitively assess the effect altering treatment had on patient outcomes, and only the DESTINY trial collected data on overall survival (OS). Receptor discordance was not significantly associated with differences in OS, if treatment was modified accordingly (median OS 27.7 months vs. 30.2 months in the concordant and discordant groups, respectively). Retrospective studies have reported worse survival outcomes in patients with receptor discordance [9, 31, 32], however this may be because of inappropriate targeted therapy in discordant cases. A recent meta-analysis investigating the prognostic significance of receptor discordance showed that a loss of either ER or PR in recurrent tumours was significantly associated with worsened OS [33]. Further large prospective studies with sufficient follow up on treatment response and survival are necessary to determine the true clinical significance of repeat biopsy for patients with metastatic breast cancer.
Mechanisms of receptor discordance
There are many possible aetiologies for receptor discordance between the primary tumour and metastasis. It has been debated whether this discordance is due to technical diagnostic issues or reflects a true biological phenomenon, and it is likely a combination of both. Firstly, technical causes must be considered, as variability occurs in the accuracy and duplicability of IHC staining [34]. Significant variations are more often described in bone metastases, at least to some degree due to the technical issues related to decalcification, which may impact on the reliability of the IHC assessment. In addition, different sampling methods, for example fine needle aspiration or core biopsy versus surgical resection of the tumour, may contribute to discordant receptor results [11, 26, 35]. Furthermore, studies based on next generation sequencing have revealed that both intra-tumour and inter-tumour heterogeneity are of greater incidence than previously thought [36]. This supports the hypothesis that receptor discordance may be evidence of clonal genome evolution [6, 37,38,39]. Tumour heterogeneity may also be attributable to selective pressure of therapy inducing clonal selection with the evolution of a novel tumour cell clone [40,41,42], or small undetected subclones in the primary tumour that only become apparent with metastatic progression [6, 39]. In a prospective study by Hilton et al., a substantial ER discordance rate was reported between the primary tumour and metastases, but there was complete concordance among metastases arising from numerous bone sites, hinting at the existence of a dominant clone dividing from the primary tumour [43]. Biological drift is another possible explanation, as newly acquired biological characteristics in the tumour microenvironment may facilitate metastatic dissemination by enabling tumour cells to travel via the circulatory and lymphatic systems [44, 45].
Studies investigating molecular determinants of intrinsic molecular subtype switching between matched primary breast and metastatic tumour samples have been severely limited [16, 46, 47]. Given that receptor discordance and intrinsic molecular subtyping occurs most significantly in Luminal type tumours, most of these studies have focused on molecular mechanisms of ER subtype switching. ER-HER2 receptor bidirectional molecular pathway cross-talk has been largely reported in the context of endocrine or anti-HER2 therapy resistance in hormone receptor (HR) and HER2-positive breast cancer [48]. It has been proposed that a change in subtype for Luminal type tumours may be as a consequence of this ER-HER2 receptor cross-talk, where ER expression can limit PI3K pathway activity affecting HER2 pathway activation, whilst HER2 overexpression, largely due to copy number amplification, can lead to loss of ER gene expression. Epigenomic, transcriptomic or genomic analysis of Luminal type primary breast tumours which metastasize have proposed loss of ESR1 (ER) gene expression due to either ESR1 (ER) hypermethylation [18], basal-like molecular features such as TP53 and/or PIK3CA mutations [16] or increased expression of FGFR4 [46] and activation of corresponding growth factor signalling pathways may be associated with Luminal A/B to HER2-enriched subtype switching.
Effect of treatment on discordance
Treatment exposure may induce receptor expression loss between the primary tumour and metastasis. This may be through a direct effect [49, 50] or as a result of clonal selection [40, 42]. For example, in line with the description of ER-HER2 receptor cross-talk above, ER and HER2 may alternate as the “dominant” pathway with either endocrine or anti-HER2 targeted therapy, where selective eradication of ER/PR positive cells by hormonal therapy could result in a population of ER/PR negative cells that could subsequently metastasise [51]. In addition to this, the impact of HER2-targeted therapy on HER2 receptor conversion has been investigated. Niikura et al. found that HER2 discordance rates differed significantly based on whether patients received chemotherapy but not based on whether the patients received trastuzumab [52]. However, other authors have not found neoadjuvant chemotherapy or trastuzumab to be associated with significant changes of HER2 status between primary and metastatic breast cancer [29, 53, 54]. The ChangeHER trial included 491 metastatic HER2-positive breast cancer cases treated with pertuzumab and/or T-DM1. This study found a HER2-positivity gain in 20.7% of cases, with some evidence of longer median OS in these patients, although at a not fully statistically significant extent [55].
Future perspectives
Liquid biopsy
Repeat biopsies are often technically difficult, invasive, costly, and limited by the fact that they provide information on mutations present only at a given time and site. A potential alternative for biopsy of metastatic lesions is the minimally invasive “liquid biopsy”, with genomic alterations of the tumour characterised by parallel sequencing of circulating cell-free tumour DNA (cfDNA) [56, 57] or circulating tumour cells (CTCs) [58]. These methods also attempt to tackle the heterogeneity of breast cancer as the cfDNA and CTCs stem from all malignant lesions within the body. While many studies have supported these methods [59,60,61], they are expensive and technically challenging. Additionally, CTCs may represent a different proportion of cells from the bulk metastatic tissue. Thus, serial blood samples provide an interesting alternative to repeat biopsies of metastatic lesions, however further research is needed to fully determine their potential.
Ongoing trials
In an attempt to improve our understanding of the genetic aberrations in metastatic breast cancer, the AURORA trial was established [62]. In this large global study, high coverage targeted gene and RNA sequencing are performed on matched primary and metastatic samples to investigate tumour heterogeneity, clonal evolution, and transcriptional changes. Initial results of the trial found that over half of the patients had molecular changes that could be matched with existing targeted therapies, highlighting the potential benefit of molecular screening in metastatic breast cancer [63]. Ongoing trials, such as SAFIR02 (NCT02299999) [64] and Alliance A071701 (NCT03994796)[65], are investigating the benefit of genetic testing to guide treatment in metastatic breast cancer. The SAFIR02 Breast trial explores using genome analysis as a therapeutic decision tool, which aims at comparing a targeted treatment administered according to identified molecular abnormalities with maintenance chemotherapy [64]. The Alliance trial investigates the benefit of genetic testing in guiding treatment for patients with any solid tumours that have metastasised to the brain using targeted therapies [65].
Conclusion
Receptor and subtype discordance between primary breast tumours and metastases is common. This article reviews the current evidence on the rate of clinical and intrinsic molecular subtype discordance, its clinical significance in terms of management and outcomes, and provides an insight into the future perspectives for patients with metastatic breast cancer.
Data availability
Not applicable.
Abbreviations
- cfDNA:
-
Cell free tumour DNA
- CTCs:
-
Circulating tumour cells
- ER:
-
Estrogen receptor
- FFPE:
-
Formalin fixed paraffin embedded
- HER2-E:
-
Human epidermal growth factor receptor 2-enriched
- HER2:
-
Human epidermal growth factor receptor 2
- HR:
-
Hormone receptor
- IHC:
-
Immunohistochemistry
- NGS:
-
Next generation sequencing
- OS:
-
Overall survival
- PR:
-
Progesterone receptor
References
O’Shaughnessy J (2005) Extending survival with chemotherapy in metastatic breast cancer. Oncologist 10(S3):20–29. https://doi.org/10.1634/theoncologist.10-90003-20
Hammond ME et al (2010) American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol 28(16):2784–2795. https://doi.org/10.1200/jco.2009.25.6529
Wolff AC et al (2018) Human epidermal growth factor receptor 2 testing in breast cancer: American society of clinical oncology/college of American pathologists clinical practice guideline focused update. J Clin Oncol 36(20):2105–2122. https://doi.org/10.1200/jco.2018.77.8738
Van Poznak C et al (2015) Use of biomarkers to guide decisions on systemic therapy for women with metastatic breast cancer: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 33(24):2695–2704. https://doi.org/10.1200/jco.2015.61.1459
Krøigård AB, Larsen MJ, Thomassen M, Kruse TA (2016) Molecular concordance between primary breast cancer and matched metastases. Breast J 22(4):420–430. https://doi.org/10.1111/tbj.12596
Aurilio G et al (2014) A meta-analysis of oestrogen receptor, progesterone receptor and human epidermal growth factor receptor 2 discordance between primary breast cancer and metastases. Eur J Cancer 50(2):277–289. https://doi.org/10.1016/j.ejca.2013.10.004
Sperduto PW et al (2020) Estrogen/progesterone receptor and HER2 discordance between primary tumor and brain metastases in breast cancer and its effect on treatment and survival. Neuro Oncol 22(9):1359–1367. https://doi.org/10.1093/neuonc/noaa025
Hulsbergen AFC et al (2020) Subtype switching in breast cancer brain metastases: a multicenter analysis. Neuro Oncol 22(8):1173–1181. https://doi.org/10.1093/neuonc/noaa013
Lindström LS et al (2012) Clinically used breast cancer markers such as estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 are unstable throughout tumor progression. J Clin Oncol 30(21):2601–2608. https://doi.org/10.1200/jco.2011.37.2482
Lu Y, Tong Y, Chen X, Shen K (2021) Association of Biomarker Discrepancy and Treatment Decision, Disease Outcome in Recurrent/Metastatic Breast Cancer Patients. Front Oncol 11:638619. https://doi.org/10.3389/fonc.2021.638619
McAnena PF et al (2018) Breast cancer subtype discordance: impact on post-recurrence survival and potential treatment options. BMC Cancer 18(1):203. https://doi.org/10.1186/s12885-018-4101-7
Gradishar WJ et al (2020) Breast Cancer, version 32020, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Cancer Netw 18(4):452–478. https://doi.org/10.6004/jnccn.2020.0016
Cardoso F et al (2020) 5th ESO-ESMO International Consensus Guidelines for Advanced Breast Cancer (ABC 5). Ann Oncol 31(12):1623–1649. https://doi.org/10.1016/j.annonc.2020.09.010
Duffy MJ et al (2017) Clinical use of biomarkers in breast cancer: Updated guidelines from the European Group on Tumor Markers (EGTM). Eur J Cancer 75:284–298. https://doi.org/10.1016/j.ejca.2017.01.017
Schrijver W, Suijkerbuijk KPM, van Gils CH, van der Wall E, Moelans CB, van Diest PJ (2018) Receptor Conversion in Distant Breast Cancer Metastases: a Systematic Review and Meta-Analysis. J Natl Cancer Inst 110(6):568–580. https://doi.org/10.1093/jnci/djx273
Aftimos P et al (2021) Genomic and Transcriptomic Analyses of Breast Cancer Primaries and Matched Metastases in AURORA, the Breast International Group (BIG) Molecular Screening Initiative. Cancer Discov 11(11):2796–2811. https://doi.org/10.1158/2159-8290.CD-20-1647
Cejalvo JM et al (2017) Intrinsic subtypes and gene expression profiles in primary and metastatic breast cancer. Cancer Res 77(9):2213–2221. https://doi.org/10.1158/0008-5472.CAN-16-2717
Varešlija D et al (2019) Transcriptome characterization of matched primary breast and brain metastatic tumors to detect novel actionable targets. JNCI 111(4):388–398. https://doi.org/10.1093/jnci/djy110
Priedigkeit N et al (2017) Intrinsic subtype switching and acquired ERBB2/HER2 amplifications and mutations in breast cancer brain metastases. JAMA Oncol 3(5):666–671. https://doi.org/10.1001/jamaoncol.2016.5630
Cosgrove N et al (2022) Mapping molecular subtype specific alterations in breast cancer brain metastases identifies clinically relevant vulnerabilities. Nat Commun 13(1):202. https://doi.org/10.1038/s41467-022-27987-5
Perou CM et al (2000) Molecular portraits of human breast tumours. Nature 406(6797):747–752. https://doi.org/10.1038/35021093
Sorlie T et al (2001) Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 98(19):10869–10874. https://doi.org/10.1073/pnas.191367098
Cheang MC et al (2015) Defining breast cancer intrinsic subtypes by quantitative receptor expression. Oncologist 20(5):474–482. https://doi.org/10.1634/theoncologist.2014-0372
Priedigkeit N et al (2017) Exome-capture RNA sequencing of decade-old breast cancers and matched decalcified bone metastases. JCI Insight 2(17):8. https://doi.org/10.1172/jci.insight.95703
Zidan J, Dashkovsky I, Stayerman C, Basher W, Cozacov C, Hadary A (2005) Comparison of HER-2 overexpression in primary breast cancer and metastatic sites and its effect on biological targeting therapy of metastatic disease. Br J Cancer 93(5):552–556. https://doi.org/10.1038/sj.bjc.6602738
Simmons C et al (2009) Does confirmatory tumor biopsy alter the management of breast cancer patients with distant metastases? Ann Oncol 20(9):1499–1504. https://doi.org/10.1093/annonc/mdp028
Gong Y, Han EY, Guo M, Pusztai L, Sneige N (2011) Stability of estrogen receptor status in breast carcinoma: a comparison between primary and metastatic tumors with regard to disease course and intervening systemic therapy. Cancer 117(4):705–713. https://doi.org/10.1002/cncr.25506
Amir E et al (2012) Prospective study evaluating the impact of tissue confirmation of metastatic disease in patients with breast cancer. J Clin Oncol 30(6):587–592. https://doi.org/10.1200/jco.2010.33.5232
Thompson AM et al (2010) Prospective comparison of switches in biomarker status between primary and recurrent breast cancer: the Breast Recurrence In Tissues Study (BRITS). Breast Cancer Res 12(6):R92. https://doi.org/10.1186/bcr2771
Amir E et al (2012) Tissue confirmation of disease recurrence in breast cancer patients: pooled analysis of multi-centre, multi-disciplinary prospective studies. Cancer Treat Rev 38(6):708–714. https://doi.org/10.1016/j.ctrv.2011.11.006
Wilking U et al (2011) HER2 status in a population-derived breast cancer cohort: discordances during tumor progression. Breast Cancer Res Treat 125(2):553–561. https://doi.org/10.1007/s10549-010-1029-2
Liedtke C et al (2009) Prognostic impact of discordance between triple-receptor measurements in primary and recurrent breast cancer. Ann Oncol 20(12):1953–1958. https://doi.org/10.1093/annonc/mdp263
Shiino S et al (2022) Prognostic significance of receptor expression discordance between primary and recurrent breast cancers: a meta-analysis. Breast Cancer Res Treat 191(1):1–14
Allred DC (2008) Commentary: hormone receptor testing in breast cancer: a distress signal from Canada. Oncologist 13(11):1134–1136. https://doi.org/10.1634/theoncologist.2008-0184
Yonemori K et al (2008) Immunohistochemical profiles of brain metastases from breast cancer. J Neurooncol 90(2):223–228. https://doi.org/10.1007/s11060-008-9654-x
Venur VA, Cohen JV, Brastianos PK (2019) Targeting molecular pathways in intracranial metastatic disease. Front Oncol 9:99. https://doi.org/10.3389/fonc.2019.00099
Shipitsin M et al (2007) Molecular definition of breast tumor heterogeneity. Cancer Cell 11(3):259–273. https://doi.org/10.1016/j.ccr.2007.01.013
Navin N et al (2011) Tumour evolution inferred by single-cell sequencing. Nature 472(7341):90–94. https://doi.org/10.1038/nature09807
Criscitiello C et al (2014) Biopsy confirmation of metastatic sites in breast cancer patients: clinical impact and future perspectives. Breast Cancer Res 16(2):205. https://doi.org/10.1186/bcr3630
Karlsson E, Appelgren J, Solterbeck A, Bergenheim M, Alvariza V, Bergh J (2014) Breast cancer during follow-up and progression: a population based cohort on new cancers and changed biology. Eur J Cancer 50(17):2916–2924. https://doi.org/10.1016/j.ejca.2014.08.014
Pertschuk LP, Axiotis CA, Feldman JG, Kim YD, Karavattayhayyil SJ, Braithwaite L (1999) Marked intratumoral heterogeneity of the proto-oncogene Her-2/neu determined by three different detection systems. Breast J 5(6):369–374. https://doi.org/10.1046/j.1524-4741.1999.97088.x
Mittendorf EA et al (2009) Loss of HER2 amplification following trastuzumab-based neoadjuvant systemic therapy and survival outcomes. Clin Cancer Res 15(23):7381–7388. https://doi.org/10.1158/1078-0432.ccr-09-1735
Hilton JF et al (2011) Acquisition of metastatic tissue from patients with bone metastases from breast cancer. Breast Cancer Res Treat 129(3):761–765. https://doi.org/10.1007/s10549-010-1264-6
Chambers AF, Naumov GN, Vantyghem SA, Tuck AB (2000) Molecular biology of breast cancer metastasis: clinical implications of experimental studies on metastatic inefficiency. Breast Cancer Res 2(6):400–407. https://doi.org/10.1186/bcr86
Shah SP et al (2009) Mutational evolution in a lobular breast tumour profiled at single nucleotide resolution. Nature 461(7265):809–813. https://doi.org/10.1038/nature08489
Garcia-Recio S et al (2020) FGFR4 regulates tumor subtype differentiation in luminal breast cancer and metastatic disease. J Clin Invest 130(9):4871–4887. https://doi.org/10.1172/JCI130323
Vareslija D et al (2019) Transcriptome characterization of matched primary breast and brain metastatic tumors to detect novel actionable targets. J Natl Cancer Inst 111(4):388–398. https://doi.org/10.1093/jnci/djy110
Giuliano M, Trivedi MV, Schiff R (2013) Bidirectional crosstalk between the estrogen receptor and human epidermal growth factor receptor 2 signaling pathways in breast cancer: molecular basis and clinical implications. Breast Care 8(4):256–262. https://doi.org/10.1159/000354253
Broom RJ et al (2009) Changes in estrogen receptor, progesterone receptor and Her-2/neu status with time: discordance rates between primary and metastatic breast cancer. Anticancer Res 29(5):1557–1562
Thomson AH et al (2016) Changing molecular profile of brain metastases compared with matched breast primary cancers and impact on clinical outcomes. Br J Cancer 114(7):793–800. https://doi.org/10.1038/bjc.2016.34
Kurbel S (2005) Selective reduction of estrogen receptor (ER) positive breast cancer occurrence by estrogen receptor modulators supports etiological distinction between ER positive and ER negative breast cancers. Med Hypotheses 64(6):1182–1187. https://doi.org/10.1016/j.mehy.2004.09.026
Niikura N et al (2012) Loss of human epidermal growth factor receptor 2 (HER2) expression in metastatic sites of HER2-overexpressing primary breast tumors. J Clin Oncol 30(6):593–599. https://doi.org/10.1200/jco.2010.33.8889
Xiao C, Gong Y, Han EY, Gonzalez-Angulo AM, Sneige N (2011) Stability of HER2-positive status in breast carcinoma: a comparison between primary and paired metastatic tumors with regard to the possible impact of intervening trastuzumab treatment. Ann Oncol 22(7):1547–1553. https://doi.org/10.1093/annonc/mdq623
Vincent-Salomon A et al (2002) HER2 status in patients with breast carcinoma is not modified selectively by preoperative chemotherapy and is stable during the metastatic process. Cancer 94(8):2169–2173. https://doi.org/10.1002/cncr.10456
Pizzuti L et al (2021) The prognostic relevance of HER2-positivity gain in metastatic breast cancer in the ChangeHER trial. Sci Rep 11(1):13770. https://doi.org/10.1038/s41598-021-92774-z
Schwarzenbach H (2013) Circulating nucleic acids as biomarkers in breast cancer. Breast Cancer Res 15(5):211. https://doi.org/10.1186/bcr3446
Forshew T et al (2012) Noninvasive identification and monitoring of cancer mutations by targeted deep sequencing of plasma DNA. Sci Transl Med 4(136):136. https://doi.org/10.1126/scitranslmed.3003726
Polzer B et al (2014) Molecular profiling of single circulating tumor cells with diagnostic intention. EMBO Mol Med 6(11):1371–1386. https://doi.org/10.15252/emmm.201404033
Pestrin M et al (2015) Heterogeneity of PIK3CA mutational status at the single cell level in circulating tumor cells from metastatic breast cancer patients. Mol Oncol 9(4):749–757. https://doi.org/10.1016/j.molonc.2014.12.001
Rothé F et al (2014) Plasma circulating tumor DNA as an alternative to metastatic biopsies for mutational analysis in breast cancer. Ann Oncol 25(10):1959–1965. https://doi.org/10.1093/annonc/mdu288
De Mattos-Arruda L et al (2014) Capturing intra-tumor genetic heterogeneity by de novo mutation profiling of circulating cell-free tumor DNA: a proof-of-principle. Ann Oncol 25(9):1729–1735. https://doi.org/10.1093/annonc/mdu239
G. Breast International, T. Breast European Adjuvant Studies, S. Frontier, and I. Technology Research Foundation (2021) AURORA: Aiming to Understand the Molecular Aberrations in Metastatic Breast Cancer
Aftimos PG et al (2019) First report of AURORA, the breast international group (BIG) molecular screening initiative for metastatic breast cancer (MBC) patients (pts). Ann Oncol 30:48. https://doi.org/10.1093/annonc/mdz100.003
Unicancer ARC Fondation, and AstraZeneca (2022) SAFIR02_Breast—efficacy of genome analysis as a therapeutic decision tool for patients with metastatic breast cancer
O Alliance for Clinical Trials in, I. National Cancer, and I. Genentech (2024) Genetic testing in guiding treatment for patients with brain metastases
Acknowledgements
Not applicable.
Funding
Open Access funding provided by the IReL Consortium. This research was funded by the RCSI Bons Secours Hospital Dublin StAR MD programme 2022.
Author information
Authors and Affiliations
Contributions
Conceptualisation: GPD, SK, ADKH. Literature search and analysis: GPD, NC. Original draft: GPD. Critically reviewed and edited: GPD, SK, NC, GRD, KG, ST, BH, ADKH. All authors have read and approved the final version of this manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethical approval
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dowling, G.P., Keelan, S., Cosgrove, N.S. et al. Receptor Discordance in Metastatic Breast Cancer; a review of clinical and genetic subtype alterations from primary to metastatic disease. Breast Cancer Res Treat (2024). https://doi.org/10.1007/s10549-024-07431-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10549-024-07431-6