Abstract
Background
Delays to breast cancer treatment can lead to more aggressive and extensive treatments, increased expenses, increased psychological distress, and poorer survival. We explored the individual and area level factors associated with the interval between diagnosis and first treatment in a population-based cohort in Queensland, Australia.
Methods
Data from 3216 Queensland women aged 20 to 79, diagnosed with invasive breast cancer (ICD-O-3 C50) between March 2010 and June 2013 were analysed. Diagnostic dates were sourced from the Queensland Cancer Registry and treatment dates were collected via self-report. Diagnostics-treatment intervals were modelled using flexible parametric survival methods.
Results
The median interval between breast cancer diagnosis and first treatment was 15 days, with an interquartile range of 9–26 days. Longer diagnostic-treatment intervals were associated with a lack of private health coverage, lower pre-diagnostic income, first treatments other than breast conserving surgery, and residence outside a major city. The model explained a modest 13.7% of the variance in the diagnostic-treatment interval \(\left( {R_{D}^{2} } \right)\). Sauerbrei’s D was 0.82, demonstrating low to moderate discrimination performance.
Conclusion
Whilst this study identified several individual- and area-level factors associated with the time between breast cancer diagnosis and first treatment, much of the variation remained unexplained. Increased socioeconomic disadvantage appears to predict longer diagnostic-treatment intervals. Though some of the differences are small, many of the same factors have also been linked to screening and diagnostic delay. Given the potential for accumulation of delay at multiple stages along the diagnostic and treatment pathway, identifying and applying effective strategies address barriers to timely health care faced by socioeconomically disadvantaged women remains a priority.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2020 breast cancer surpassed lung cancer as the most diagnosed cancer worldwide, with an estimated 2.3 million new cases [1]. Amongst women, breast cancer accounts for approximately 1 in 4 cancer diagnoses and 1 in 6 cancer-related deaths globally [1]. In Australia, the age-standardised incidence rate of breast cancer has been steadily increasing, and it was estimated that approximately 20,000 Australian women were diagnosed with breast cancer in 2021 [2]. Understanding the factors that contribute to and exacerbate the breast cancer burden remains a high priority.
In Australia, 5-year survival varies from as high as 99% for stage I breast cancer to 20–35% for stage IV breast cancer [2]. Critically, prolonged pathways to treatment are associated with larger tumour sizes, the presence of cancer cells in the lymph nodes, later stage cancers [3,4,5,6,7,8,9], and reduced survival [8, 10,11,12]. Moreover, increased wait-times for treatment can result in the need for more aggressive and extensive treatments [13], increased expenses and increased psychological distress [14]. At present, timely detection and treatment offer the best chance of improving breast cancer outcomes, and, consequently, are a key focus of breast cancer management and care [15]. However, improving timely care and treatment first requires identifying the factors that contribute to unnecessary delay.
There is an extensive literature examining time to detection and diagnosis [16], with socioeconomic disadvantage typically associated with later detection and longer wait times for diagnosis [15, 17,18,19]. However, the interval between diagnosis and treatment has received relatively less attention in the literature. Studies carried out in various countries suggest that many of the factors associated with later detection and diagnosis also predict the length of the diagnosis-treatment interval, for example, ethnicity/race [20, 21], education [13], and remoteness [22]. However, we are aware of no large-scale studies investigating the extent to which individual and area level factors affect the time interval between diagnosis and treatment in an Australian context. Given that accumulation of delay at multiple stages along the diagnostic and treatment pathway may harm outcomes and contribute to the breast cancer outcome gradients seen in Australia [19, 23], it is important to identify factors that potentially may affect the wait-time for initial treatment following a breast cancer diagnosis. As such, we analysed data from a large population-based study of women diagnosed with breast cancer in Queensland, Australia to quantify the wait time between diagnosis and first treatment and to identify any individual and area level factors that predict the interval.
Methods
Study population
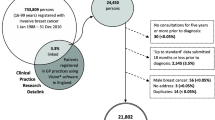
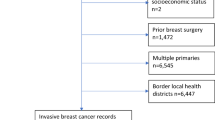
Analyses were conducted using data from the Breast Cancer Outcome Study—a longitudinal study of women from Queensland, Australia aged 20 to 79 years with a histologically confirmed diagnosis of invasive breast cancer between the 1st of March 2010 and the 30th of June 2013. The study used telephone and self-administered questionnaires to collect individual-level data from English speaking women diagnosed with invasive breast cancer, identified through the Queensland Cancer Register. Clinical, diagnostic, and treatment information was obtained from medical records at 12 months post-diagnosis. A total of 5426 potentially eligible women were identified through the Queensland Cancer Register, of whom 3326 (61%) met all eligibility criteria and responded. Full details of the eligibility criteria, data sourcing, and the telephone interview are described in [23]. Women living in major cities were less likely to participate (p = 0.04), and non-respondents were more likely to be diagnosed with advanced disease (p = 0.03) [23].
Data preparation
Date of breast cancer diagnosis and clinical data was sourced from the Queensland Cancer Register, where diagnostic date reflects the first date of investigation from pathology, or the date indicated on hospital admission notification. First treatment date and type were collected through self-report. Patient self-reported date of surgeries (94% of the breast conserving surgery, 87% of the mastectomy) was cross checked with clinical records and the correlation was high (r = 0.99), indicating a high degree of reliability for the 95.1% of women whose first treatment was surgical. The diagnostic-treatment interval was modelled as the number of days between diagnosis and first treatment. Specifically, we modelled diagnostic-treatment intervals up to a maximum of 3 months (90 days). Thirteen cases with intervals greater than 90 days were treated as censored. Left uncensored, these extreme observations increased model complexity, in the form are greater degrees of freedom and the need for additional time-dependencies, and, in some cases, caused model convergence issues. Importantly, censoring these extreme values had minimal effect on the coefficient estimates and model fit. Ninety-seven respondents reported their first treatment occurring prior to the date of diagnosis. That is, they had a negative diagnostic-treatment interval. Many of these intervals, if not most, can be assumed to reflect data entry errors given the median length of the negative diagnostic-treatment intervals was − 168 days. As the negative intervals cannot be modelled here, all negative intervals were removed. Negative diagnostic-treatment intervals were associated with later stage breast cancer at diagnosis (p = 0.04) and first treatments other than BCS or mastectomy (p < 0.001). Separately, 123 participants reported inconsistent information with respect to first treatment type and first treatment date and were removed. These discrepant cases overlapped greatly (58%) with negative diagnostic-treatment intervals (p < 0.001) and were strongly associated with first treatment types other than BCS and mastectomy (p < 0.001).
One-hundred and eighty-seven women reported the same date for diagnosis and first-treatment—an interval of zero days. The majority of these intervals likely reflect confirmation of diagnosis at treatment and were recoded as 0.5 to allow for the modelling of log-time. Importantly, inspection of interval data revealed a severely compressed distribution—many ties concentrated below the median. To break ties and resolve model convergence issues that arose with increasing model complexity, we applied uncorrelated uniform noise—\(Unif\left( {0, \pm\,0.01} \right)\) days—to the diagnostic-treatment interval. To discount the introduction of bias, we compared coefficient estimates derived from the original interval data to those derived from the transmuted (plus noise) data, using simplified Weibull (df = 1) models. Only negligible differences were observed that did not affect interpretation.
Finally, all treatment types other than breast conserving surgery (BCS) or mastectomy (chemotherapy, Herceptin, hormone, radiotherapy, other surgery, or therapy) were aggregated as ‘other’ due to small counts in each of these categories. Remoteness of residence when diagnosed with breast cancer was categorised using the Australian Bureau of Statistics Remoteness Index (ARIA+), which is a measure of accessibility and remoteness based on geographical location [24]. We aggregated the Outer Regional, Remote and Very Remote categories due to small counts in each of these categories. Age at diagnosis was mean centred and visual inspection of martingale residuals showed that age at diagnosis appeared approximately linear on the log cumulative hazard scale.
Model derivation
The length of the diagnostic-treatment interval (days) was modelled using flexible parametric survival analysis (Royston–Parmar models). The approach involves fitting restricted cubic polynomial splines to flexibly model the baseline log-cumulative hazard. The method allows the estimation of absolute measures of effect (e.g. baseline hazard rates) at all time points, and extrapolation of the time-to-event function. Additionally, the use of splines addresses the potentially unrealistic assumption of constant or monotonic hazard inherent to parametric survival models [25]. The selection of scales and number of degrees of freedom (knots) for the baseline spline function was made using the Bayesian information criterion (BIC) statistic and Akaike information criterion (AIC). Knot position was set using 2 boundary knots (smallest and largest uncensored log interval-times) and m interior knots based on empirical centiles of the log treatment-time distribution [26]. The data were best captured using the log cumulative hazard (proportional hazard) scale with 3 degrees of freedom—log cumulative odds models with degrees of freedom > 2 failed to converge.
Candidate predictors and potential confounders were identified from a literature search of individual and area level factors previously associated with delays to cancer detection, diagnosis and treatment, and cancer outcomes more broadly. Potential model covariates were identified using univariable analyses coupled with likelihood ratio tests. Covariates with evidence of an association with the diagnostic-treatment interval at p < 0.3 were tested in the multivariable building process. We then used an iterative backwards selection process and removed predictors one at time to arrive at the final adjusted multivariable model. To test for time-dependent effects (TD), we first entered a time-dependent effect for each covariate into the multivariable model separately. We then used a forward selection process, entering time-dependent terms into the model one at a time, in order of greatest evidence of time-dependency (lowest p value). Time dependencies were identified using likelihood-ratio tests and were only included in the final model when p < 0.01. A more conservative threshold was used to buffer against over-fitting and multiple testing. For simplicity, time-dependent effects were initially modelled using the same degrees of freedom as the baseline spline function (df = 3). Once appropriate time-dependent effects had been identified, BIC and AIC criteria indicated that a solution with 2 degrees of freedom for time-dependent effects provided the best model fit.
In contrast to typical applications of survival analysis, here we are modelling time to treatment—a desirable outcome—so the interpretation of model coefficients is in a sense reversed. Specifically, coefficients less than 1 convey a disadvantage—less likely to have received treatment by a given timepoint. For clarity, where one might otherwise refer to survival curves, here we refer to treatment curves, and their shape is the inverse to traditional survival curves. Additionally, hazard ratios are referred to as treatment ratios. Analyses were run in Stata (version 16.1, StataCorp) using the stpm2 package.
Model discrimination
The discrimination performance reflects the ability of a time-to-event model to assign higher risks to individuals who experience earlier events—those who indeed have higher risk of the event. We assessed the discrimination performance of our model using Royston and Sauberbrei’s D statistic. Royston and Sauberbrei’s D statistic measures the separation of the treatment curves and can be interpreted as an estimate of the log treatment ratio comparing two groups of equal size [27]. The goodness of fit for the full model was calculated using Royston and Sauberbrei’s \(R_{D}^{2}\). Finally, to assess the discrimination performance of individual predictors in the model, we calculated Royston and Sauberbrei’s D for the model after removing predictors from the model one at a time, adding them sequentially to the model, and as individual predictors (see Supplementary Table 1). It is important to note that, in non-proportional hazard models, \(R_{D}^{2}\) is analogous to but not strictly interpretable as a measure of explained variance. However, it is still a useful index of determination and for comparing the relative contributions of the individual predictors in the model [28].
Cluster analysis
As an alternative to using the model to generate treatment curves for hypothetical cases, we utilised cluster analysis to identify actual sub-populations within our sample potentially at greater risk of longer diagnostic-treatment intervals. K-medoid clustering [29] (partitioning around medoids—the point within a cluster where dissimilarity with all other points is a minimum) using Gower’s distance [30] to measure (dis) similarity was performed over the model covariates. Age and Stage at diagnosis were excluded from the cluster analysis on the grounds that they carried minimal prognostic information. The optimal number of clusters was determined using the Silhouette method. The clusters were then entered into a flexible parametric model (df = 3) with a time-dependent component (df = 2) to derive treatment curves for each cluster.
Results
Sample characteristics
The final model was run over a sample of 3216 participants. The mean age at diagnosis was 57.6 (SD 10.9) years and the median interval between breast cancer diagnosis and first treatment was 15 days, with an interquartile range of 9–26 days. The treatment curves varied by key factors (Fig. 1). Details regarding the sample breakdown and definitions for all variables retained in the final model and candidate variables can be found in Tables 1 and 2, respectively.
Coefficient estimates from the final flexible parametric model are presented in Table 3. Private health insurance and remoteness category were modelled as time-dependent (TD) effects. Adding time-dependencies to the model increases the model’s complexity and makes interpreting the time-dependent coefficients (treatment ratios) difficult. This is because the time-dependent treatment ratios, by definition, vary over the interval. Additionally, when multiple time-dependencies are added, the treatment ratio of time-dependent covariates depends on the levels of the other time-dependent covariates in the model. Here we report treatment ratios (TR) at two timepoints—15- and 30-day intervals—where the treatment ratios for private health insurance and remoteness category have been calculated at the most common level of the other time-varying covariate—living in a major city and full private health insurance, respectively. Treatment ratios calculated across the other levels of the time-varying covariates showed only minimal differences. Treatment ratios over the full distribution for private health insurance and remoteness category are reported in Supplementary Fig. 1. To better highlight differences amongst the covariates, we refer to the treatment probabilities at discrete timepoints (see Table 4).
Broadly speaking, the final model shows that, on average, wait-times for first treatment following breast cancer diagnosis were shorter for those with full private health insurance, those living in a major city, those with higher pre-diagnostic income, and those whose initial treatment was BCS. Note that we observed a significant but small association between tumour grade and the diagnostic-treatment interval in the multivariable model. However, we chose to exclude tumour grade from the final model on the grounds that the effect was not clinically relevant—differences of 1 day between grade 3 and grade 1—and added additional complexity to the model by adding an additional time dependency. Stage at diagnosis was included in the final model to control for potential confounding, particularly of treatment type, and given its prognostic importance in other contexts. Note though that it was not associated with the outcome here and produced only minimal changes to the coefficients of the other variables. To better capture the difference between groups, particularly for time-dependent effects, the treatment probabilities for each group at 15 (sample median) and 30 days after diagnosis—a loose treatment guideline [22]—are shown in Table 4, along with the predicted treatment curves in Fig. 2. Treatment probabilities and curves for the levels of each predictor are derived from directly adjusted treatment curves. This approach involves estimating a treatment curve for every combination of covariates and averaging them according to weights defined by the frequency of the covariate pattern. The resulting estimates reflect the probability of having received treatment at a given point in time, if each group had the distribution of covariates in the study sample. The final column of Table 4 shows the estimated median diagnostic-treatment interval by covariate level and gives a sense of the differences in wait-times for treatment between the groups.
The final model explained approximately 13.8% of the variance in diagnostic-treatment intervals, \(R_{D}^{2} = 0.138 \left( {95\% {\text{CI}}\;0.118, \;0.158} \right)\), with a Royston and Sauerbrei’s D of 0.82, demonstrating low to moderate discrimination performance of the model. Nearly all the prognostic information is carried by private health insurance, \(R_{D}^{2} = 0.211 \left( {95\% {\text{CI}}\;0.179, 0.243} \right)\) as a single predictor model. Separately, the remaining predictors, age at diagnosis, pre-diagnostic income, and treatment type together accounted for approximately 4.9% of the variance, \(R_{D}^{2} = 0.049 \left( {95\% {\text{CI}}\;0.037, \;0.061} \right)\) (Supplementary Table 1). The unusual pattern whereby \(R_{D}^{2}\) decreased with the addition of significant predictors in the model, to the extent that private health insurance alone appears to account for more variance than the final model, is likely related to a shifting baseline function, from which \(R_{D}^{2}\) is derived.
Much of the variance in the diagnostic-treatment interval remains unexplained, however, some of this variation may be unrelated to the specific characteristics and circumstances of the women in the study. That is, some of the variation may reflect the randomness of daily routine and situation; for example, some patients reported delays to treatment due to the major floods in Brisbane in 2011, factors that are of less interest in a model aimed at capturing systematic differences. We extended the model to include ‘explicit treatment delay’ to potentially capture and quantify some of this additional variance. Those who explicitly reported experiencing personal or practical delays to their first breast cancer treatment experienced longer intervals between diagnosis and first treatment, on average, than those who did not report a delay, p < 0.001. Inclusions of explicit treatment delay into the model improved discrimination performance (Sauerbrei’s D = 1.03) and explained an additional 6.5% of the variance in diagnostic-treatment intervals, \(R_{D}^{2} = 0.202 \left( {95\% {\text{CI}}\,0.182,\, 0.224} \right)\).
Cluster analysis
The Silhouette method identified five optimal clusters. Figure 3 shows (a) the distribution of diagnostic-treatment intervals for all clusters, (b) the covariate patterns for each cluster, and (c) the adjusted treatment curves for each cluster. Importantly, the clusters are differentiated along the diagnostic-treatment interval. The median diagnostic-treatment interval increases across the clusters, where the cluster 1 median is 12 days between diagnosis and first treatment compared to 27 days for cluster 6. At the sample median of 15 days, 64% and 19% of women in cluster 1 and cluster 6 had received their first treatment, respectively (see Fig. 3). At 30 days post-diagnosis, only 6% of women in cluster 1 had not received their first treatment, whilst 40% of women in cluster 6 were still waiting for their first treatment.
a Distribution of diagnostic-treatment intervals by cluster. b Radar plot showing the characteristics of women within each cluster. The concentric circles reflect the percentage of women in each cluster with a given characteristic, where the centre reflects 0% and expands outwards to 100%. Jitter (2°) has been added to the clusters to help differentiate them. c Directly adjusted treatment curves derived from the flexible parametric model (df = 3, TD df = 2), by cluster. The shaded bands reflect the 95% confidence intervals
Clusters 5 and 6—the clusters with the longest wait times for first treatment—are dominated by women who had no private health insurance, and a minority that had partial insurance. Remoteness also characterised the clusters: amongst Clusters 1–3, in which most women had full insurance, treatment times increased as the predominant remoteness category changed from major city to outer regional and remote. Clusters in which most women had less physical access to health services (that is, lived outside major cities) but had greater financial access in terms of full health insurance tended to have faster treatment times than women who lived nearer services but did not have full health insurance. The clusters with high proportions of women with full health insurance had approximately equal numbers from each of the categories for pre-diagnostic income. Women in the clusters without full private health insurance also tended to be in the lowest or second to lowest categories for pre-diagnostic income.
Discussion
A central tenet of breast cancer management and care is early detection and diagnosis to expedite treatment, where timely treatment is associated with improved breast cancer outcomes [8, 31,32,33,34]. Delays to the initiation of treatment can lead to poorer prognosis if disease is allowed to advance [3, 4, 11, 31, 34]. Whilst prevention where possible is ideal, timely treatment following diagnosis offers the best chance of reducing breast cancer burden. In the current study, we examined how long women waited for their first treatment following a breast cancer diagnosis, and the factors that predicted their wait-time.
That the median interval between breast cancer diagnosis and first treatment was 15 days, with 84% of the cohort receiving treatment within 30 days of diagnosis, is encouraging from the perspective of breast cancer biology. The estimated breast tumour doubling times vary widely, between 45 and 260 days [4]. Guidelines for an acceptable diagnostic-treatment interval length are scarce. However, it has been suggested that diagnostic-treatment intervals of 30 days or less are unlikely to negatively affect survival [22], and Cancer Australia [35] recommends surgery occurs within 30 days of diagnosis for those not receiving neoadjuvant therapy. We found that approximately one in six women (16%) waited longer than 30 days post-diagnosis for treatment. Bleicher [4] suggests that surgeries should proceed within 90 days of a breast cancer diagnosis, where diagnostic-treatment intervals greater than 90 days have been associated with poorer survival [36]. It is therefore encouraging that only 13 out of 3216 women in our study waited 90 days or longer. Of course, the urgency of treatment may depend heavily on the previous detection and diagnostic pathway.
We identified several socioeconomic factors associated with the breast cancer diagnostic-treatment interval. The predictor with the largest effect size was private health insurance. On average, those with full private health insurance received first-treatment nearly 2 weeks sooner than those with no private health insurance. Moreover, more than 1 in 3 women (37%) with no private health insurance waited longer than 30 days for their first treatment following diagnosis. Note that the effect of health insurance was time-dependent though, and the benefits associated with full private health insurance relative to no private health insurance diminished as the length of the diagnostic-treatment interval increased. Other predictors of treatment wait time included pre-diagnostic income and remoteness, where those earning more and residing in major cities tended to experience shorter wait-times between diagnosis and first treatment. Though small, note that the effect of pre-diagnostic income is independent of private health insurance, indicating that there is advantage attached to income beyond granting access to full private health insurance. Possibly income affords greater flexibility when it comes to the scheduling of treatments, and or the ability to organise existing commitments to prioritise urgent health care. Additionally, we observed an effect of treatment type, whereby patients waited less time for BCS relative to mastectomy and other treatment types, after adjusting for stage at diagnosis. Note that only a small percentage (3.2%) of women in the study cohort received pre-operative neoadjuvant chemotherapy (NAC), where the proportion of patients receiving NAC in Australia has steadily increased over the last decade towards a target of 20% [37, 38]. Importantly, NAC can extend the interval to treatment due to increased multidisciplinary discussion of treatment planning and management [39], suggesting that the interval differences observed here for treatment type may underestimate current differences. Overall, much of the variation in the diagnostic-treatment interval remained unexplained though, even after accounting for a source of variance unrelated to the inherent characteristics of the women in the study—explicit treatment delay. Finally, the underrepresentation of advanced disease in our sample is worth noting. Such bias is difficult to avoid in the study of serious disease, and it is difficult to know what consequence it should have for our interpretation of the results. Given that private health insurance was negatively associated with disease advancement in our sample (p < 0.001), it’s possible that non-responders were less likely to have full private health insurance, and consequently may indicate an underestimation of the true diagnostic-treatment intervals differences reported here.
Whilst many of the differences in diagnostic-treatment intervals we observed were small, it is important to consider that some of these same factors have also been linked to screening and diagnostic delay, and accumulation of delay at multiple stages along the diagnostic and treatment pathway may harm outcomes. Moreover, the cluster analysis suggests that there are dependencies between these predictors in the population, and small effects across multiple factors accumulate, potentially resulting in poorer breast cancer outcomes for those individuals. Although these data are approximately 10 years old now, and may reflect dated treatment pathways, they provide unique insights that are otherwise not possible with more recent, routinely collected data from cancer registers—they do not routinely collect the breadth of socioeconomic data we have reported here. Though breast cancer treatment pathways may have changed, increasing costs in healthcare and growing gaps in health outcomes across socioeconomic groups in Australia [40], suggest that the effects reported here likely persist, and highlights the need for more contemporary data. Additionally, the consequences of variation in cancer treatment and care can take years to manifest and identify. The data reported here are relevant to understanding current inequalities in breast cancer outcomes in Queensland, Australia, and potentially, more broadly wherever socio-economic gradients resemble those in this study. Indeed, Australia boasts one of the best health care systems in the world [41], the patterns of treatment inequality reported here may even be exaggerated in other regions with less equitable and efficient healthcare systems. Identifying effective strategies to reduce the disparity in wait-times for breast cancer treatment faced by socioeconomically disadvantaged women should remain a priority.
Data availability
The data supporting this research are exclusively accessible through a formal Data Sharing Agreement, which can be initiated by contacting the corresponding author, and may be subject to eligibility criteria. The agreement outlines the terms and conditions governing data usage, security, and ethical considerations.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Australian Institute of Health and Welfare; National Breast and Ovarian Cancer Centre (2021) Breast Cancer in Australia: an overview
Arndt V, Sturmer T, Stegmaier C, Ziegler H, Dhom G, Brenner H (2002) Patient delay and stage of diagnosis among breast cancer patients in Germany—a population-based study. Br J Cancer 86:1034–1040. https://doi.org/10.1038/sj.bjc.6600209
Bleicher RJ (2018) Timing and delays in breast cancer evaluation and treatment. Ann Surg Oncol 25(10):2829–2838. https://doi.org/10.1245/s10434-018-6615-2
Burgess CC, Ramirez AJ, Richards MA, Love SB (1998) Who and what influences delayed presentation in breast cancer? Br J Cancer 77:1343–1348. https://doi.org/10.1038/bjc.1998.224
Caplan L (2014) Delay in breast cancer: Implications for stage at diagnosis and survival. Front Public Health 2:87. https://doi.org/10.3389/fpubh.2014.00087
Hanna TP, King WD, Thibodeau S, Jalink M, Paulin GA, Harvey-Jones E, Aggarwal A (2020) Mortality due to cancer treatment delay: systematic review and meta-analysis. Bmj. https://doi.org/10.1136/bmj.m4087
Richards MA, Smith P, Ramirez AJ, Fentiman IS, Rubens RD (1999) The influence on survival of delay in the presentation and treatment of symptomatic breast cancer. Br J Cancer 79(5):858–864. https://doi.org/10.1038/sj.bjc.6690173
Raphael MJ, Biagi JJ, Kong W, Mates M, Booth CM, Mackillop WJ (2016) The relationship between time to initiation of adjuvant chemotherapy and survival in breast cancer: a systematic review and meta-analysis. Breast Cancer Res Treat 160(1):17–28. https://doi.org/10.1007/s10549-016-3960-3
Bleicher RJ, Ruth K, Sigurdson ER, Beck JR, Ross E, Wong YN, Egleston BL (2016) Time to surgery and breast cancer survival in the United States. JAMA Oncol 2(3):330–339. https://doi.org/10.1001/jamaoncol.2015.4508
Coates AS (1999) Breast cancer: delays, dilemmas, and delusions. The Lancet 353(9159):1112–1113. https://doi.org/10.1016/s0140-6736(99)00082-3
Kothari A, Fentiman IS (2003) 22. Diagnostic delays in breast cancer and impact on survival. Int J Clin Pract 57(3):200–203
Jassem J, Ozmen V, Bacanu F, Drobniene M, Eglitis J, Lakshmaiah KC, Zaborek P (2014) Delays in diagnosis and treatment of breast cancer: a multinational analysis. Eur J Public Health 24(5):761–767. https://doi.org/10.1093/eurpub/ckt131
Risberg T, Sørbye SW, Norum J, Wist EA (1996) Diagnostic delay causes more psychological distress in female than in male cancer patients. Anticancer Res 16(2):995–999
Gorin SS, Heck JE, Cheng B, Smith SJ (2006) Delays in breast cancer diagnosis and treatment by racial/ethnic group. Arch Intern Med 166(20):2244–2252. https://doi.org/10.1001/archinte.166.20.2244
Webber C, Jiang L, Grunfeld E, Groome PA (2017) Identifying predictors of delayed diagnoses in symptomatic breast cancer: a scoping review. Eur J Cancer Care 26(2):e12483. https://doi.org/10.1111/ecc.12483
Ermiah E, Abdalla F, Buhmeida A, Larbesh E, Pyrhönen S, Collan Y (2012) Diagnosis delay in Libyan female breast cancer. BMC Res Notes 5(1):1–8. https://doi.org/10.1186/1756-0500-5-452
Nguyen-Pham S, Leung J, McLaughlin D (2014) Disparities in breast cancer stage at diagnosis in urban and rural adult women: a systematic review and meta-analysis. Ann Epidemiol 24(3):228–235. https://doi.org/10.1016/j.annepidem.2013.12.002
Youl PH, Aitken JF, Turrell G, Chambers SK, Dunn J, Pyke C, Baade PD (2016) The impact of rurality and disadvantage on the diagnostic interval for breast cancer in a large population-based study of 3202 women in Queensland, Australia. Int J Environ Res Public Health 13(11):1156. https://doi.org/10.3390/ijerph13111156
Elmore JG, Nakano CY, Linden HM, Reisch LM, Ayanian JZ, Larson EB (2005) Racial inequities in the timing of breast cancer detection, diagnosis, and initiation of treatment. Med Care. https://doi.org/10.1097/00005650-200502000-00007
SheinfeldGorin S, Heck JE, Cheng B, Smith S (2006) Effect of race/ethnicity and treatment delay on breast cancer survival. J Clin Oncol 24(18 Suppl):6063–6063. https://doi.org/10.1200/jco.2006.24.18_suppl.6063
Caplan LS, May DS, Richardson LC (2000) Time to diagnosis and treatment of breast cancer: results from the National Breast and Cervical Cancer Early Detection Program, 1991–1995. Am J Public Health 90(1):130. https://doi.org/10.2105/ajph.90.1.130
Youl PH, Baade PD, Aitken JF, Chambers SK, Turrell G, Pyke C, Dunn J (2011) A multilevel investigation of inequalities in clinical and psychosocial outcomes for women after breast cancer. BMC Cancer 11(1):1–8. https://doi.org/10.1186/1471-2407-11-415
Australian Institute of Health and Welfare (2004) Rural, regional and remote health: a guide to remoteness classifications. Australian Institute of Health and Welfare AIHW Cat. No. PHE 53
Lambert PC, Royston P (2009) Further development of flexible parametric models for survival analysis. Stand Genomic Sci 9(2):265–290
Royston P, Lambert PC (2011) Flexible parametric survival analysis using Stata: beyond the Cox model, vol 347. Stata Press, College Station
Austin PC, Pencinca MJ, Steyerberg EW (2017) Predictive accuracy of novel risk factors and markers: a simulation study of the sensitivity of different performance measures for the Cox proportional hazards regression model. Stat Methods Med Res 26(3):1053–1077. https://doi.org/10.1177/0962280214567141
Royston P (2006) Explained variation for survival models. Stand Genomic Sci 6(1):83–96
Maechler M (2019) Finding groups in data: cluster analysis extended Rousseeuw et al. R Package Vers 2:242–248
Gower JC (1971) A general coefficient of similarity and some of its properties. Biometrics 857–871
Afzelius P, Zedeler K, Sommer H, Mouridsen HT, Blichert-Toft M (1994) Patient’s and doctor’s delay in primary breast cancer: prognostic implications. Acta Oncol 33(4):345–351. https://doi.org/10.3109/02841869409098427
Brazda A, Estroff J, Euhus D, Leitch AM, Huth J, Andrews V, Rao R (2010) Delays in time to treatment and survival impact in breast cancer. Ann Surg Oncol 17(3):291–296. https://doi.org/10.1245/s10434-010-1250-6
McLaughlin JM, Anderson RT, Ferketich AK, Seiber EE, Balkrishnan R, Paskett ED (2012) Effect on survival of longer intervals between confirmed diagnosis and treatment initiation among low-income women with breast cancer. J Clin Oncol 30(36):4493. https://doi.org/10.1200/JCO.2012.39.7695
Neave LM, Mason BH, Kay RG (1990) Does delay in diagnosis of breast cancer affect survival? Breast Cancer Res Treat 15(2):103–108. https://doi.org/10.1007/BF01810782
Cancer Australia (2020) Guidance for the management of early breast cancer. Recommendations and practice points. Australian Government
Jung SY, Sereika SM, Linkov F, Brufsky A, Weissfeld JL, Rosenzweig M (2011) The effect of delays in treatment for breast cancer metastasis on survival. Breast Cancer Res Treat 130(3):953–964. https://doi.org/10.1007/s10549-011-1662-4
Littlejohn DR (2019) Is Australia lagging behind in the use of neoadjuvant chemotherapy for breast cancer?. https://doi.org/10.21037/abs.2019.07.01
Patiniott PD et al (2019) Neoadjuvant chemotherapy rates for breast cancer in Australia—“are we there yet?” Ann Breast Surg 3:9. https://doi.org/10.21037/abs.2019.04.01
Read RL, Flitcroft K, Snook KL, Boyle FM, Spillane AJ (2015) Utility of neoadjuvant chemotherapy in the treatment of operable breast cancer. ANZ J Surg 85(5):315–320. https://doi.org/10.1111/ans.12975
Public Health information Development Unit. Social health atlas of Australia. Inequality graphs: time series. https://phidu.torrens.edu.au/social-health-atlases/graphs/monitoring-inequalityin-australia/whole-pop. Accessed Apr 2023
Schneider EC, Sarnak DO, Squires D, Shah A, Doty MM (2017) Mirror, mirror 2017: international comparison reflects flaws and opportunities for U.S. Health Care, The Commonwealth Fund. http://www.commonwealthfund.org/interactives/2017/july/mirror-mirror/
Acknowledgements
The authors wish to acknowledge the interviewers who conducted interviews on over 3000 women.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. The Breast cancer outcomes study was funded by a Cancer Australia Grant (#100639) and Cancer Council Queensland.
Author information
Authors and Affiliations
Contributions
PY, PDB, JFA, GT and SC conceived and designed the study; JDR analysed the data and drafted the initial manuscript; and PDB and JKC contributed to early drafts. JFA, PY, SC, JD and CP contributed later drafts of the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest. The founding sponsors had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, and in the decision to publish the result.
Ethical approval
Ethical approval for this study was obtained from the Human Research Ethics Committee of Griffith University, Australia (PSY/C4/09/HREC). Approval to access confidential health information was obtained from the Research Ethics and Governance Unit, Queensland Health.
Consent to participate
Informed consent was obtained form all individual participants included in the study and their respective treating doctor.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Retell, J.D., Cameron, J.K., Aitken, J.F. et al. Individual and area level factors associated with the breast cancer diagnostic-treatment interval in Queensland, Australia. Breast Cancer Res Treat 203, 575–586 (2024). https://doi.org/10.1007/s10549-023-07134-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-07134-4