Abstract
Purpose
Ductal carcinoma in situ (DCIS) is present in more than half of HER2-positive invasive breast cancer (IBC). Recent studies show that DCIS accompanying HER2-positive IBC can be completely eradicated by neoadjuvant systemic therapy (NST). Our aim was to determine the percentage of pathologic complete response of the DCIS component in a nationwide cohort and to assess associated clinicopathologic variables. Furthermore, the impact on surgical treatment after NST was investigated.
Methods
Women diagnosed with HER2-positive IBC, treated with NST and surgery, between 2010 and 2020, were selected from the Netherlands Cancer Registry. Pre-NST biopsy and postoperative pathology reports were obtained from the Dutch Nationwide Pathology Databank and assessed for the presence of DCIS. Clinicopathologic factors associated with DCIS response were assessed using logistic regression analyses.
Results
A DCIS component was present in the pre-NST biopsy in 1403 (25.1%) of 5598 included patients. Pathologic complete response of the DCIS component was achieved in 730 patients (52.0%). Complete response of DCIS occurred more frequently in case of complete response of IBC (63.4% versus 33.8%, p < 0.001). ER-negative IBC (OR 1.79; 95%CI 1.33–2.42) and more recent years of diagnosis (2014–2016 OR 1.60; 95%CI 1.17–2.19, 2017–2019 OR 1.76; 95%CI 1.34–2.34) were associated with DCIS response. Mastectomy rates were higher in IBC+DCIS compared to IBC (53.6% versus 41.0%, p < 0.001).
Conclusion
Pathologic complete response of DCIS occurred in 52.0% of HER2-positive IBC patients and was associated with ER-negative IBC and more recent years of diagnosis. Future studies should investigate imaging evaluation of DCIS response to improve surgical decision making.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neoadjuvant systemic therapy (NST) has gained an important role in the treatment of invasive breast cancer (IBC). Earlier, NST was reserved for locally advanced or inoperable breast cancer, while nowadays NST can be considered in early stage breast cancer [6]. The main goal of NST is to improve oncologic outcomes and additionally to reduce tumor extent in order to improve breast-conserving surgery rates [1, 9]. The response rate depends on the breast cancer subtype, with the highest rates of pathologic complete response (pCR) in HER2-positive or triple-negative IBC [8].
In case of HER2-positive IBC, a ductal carcinoma in situ (DCIS) component accompanies the invasive tumor in 57.4%–71.6% of patients [4, 10]. Some studies show that in IBC patients with a DCIS component, the pCR rate is lower, while others did not find an association between the presence of DCIS and pCR [11, 18, 22]. DCIS was previously considered insensitive to NST, due to its protective basal membrane, less dense micro-vasculature, and lower proliferative state as opposed to IBC [25]. Subsequently, IBC patients with a DCIS component were less likely to undergo breast-conserving surgery, both in case of primary surgery and after NST [10, 24].
Recently, a few studies have shown that the DCIS component accompanying HER2-positive IBC can respond to NST. Von Minckwitz et al. demonstrated that in their population including 59 HER2-positive IBC patients with a DCIS component, 30 (50.8%) showed a pCR of the DCIS component [22]. Groen et al. investigated 138 HER2-positive IBC patients with a DCIS component and showed a pCR of DCIS in 46% of patients after NST. In conclusion, current literature suggests response of the DCIS component in HER2-positive IBC, but these few articles only concerned small study populations.
Therefore, the aim of this study was to determine the rate of pCR of a DCIS component in HER2-positive IBC in a large cohort of patients by performing a nationwide analysis. In addition, the influence of clinicopathologic variables on the rate of pCR of the DCIS component and the impact of the DCIS component on surgical treatment were investigated.
Materials and methods
Data sources and study population
A database from the Netherlands Cancer Registry (NCR) was used for this nationwide retrospective study. Since 1989, trained registrars from the Netherlands Comprehensive Cancer Organization (IKNL) have been collecting data regarding patient, tumor, and treatment characteristics of all newly diagnosed cancer patients in the Netherlands. Upon request, the collected data can be used for research after approval by the privacy board of the IKNL.
Women aged 18 years or older, diagnosed with primary HER2-positive IBC, treated with neoadjuvant chemotherapy and targeted therapy followed by surgery between January 2010 and December 2019 in the Netherlands, were included from the NCR for the present study. This population was subsequently linked to PALGA, the Dutch Nationwide Pathology Databank [3]. In this way, all pre-NST biopsy and postoperative pathology reports were collected. Patients were excluded in case of missing pre-NST or postoperative pathology reports or when treatment differed from the Dutch guidelines at the year of diagnosis.
Neoadjuvant systemic therapy and surgical procedure
NST regimens were based on the national guidelines in the year of diagnosis [12,13,14]. In HER2-positive IBC, NST is recommended in case of tumor size ≥ 5 mm or node-positive IBC. In general, NST consisted of Anthracyclines followed by Docetaxel or Paclitaxel, in combination with Trastuzumab. From 2016 onwards, patients with tumor size ≤ 2 cm received only Paclitaxel in combination with Trastuzumab for 12 weeks, based on the study by Tolaney et al.[19] Trastuzumab was in all patients continued after NST and surgery in the adjuvant setting for one year in total. Dual anti-HER2 blockade consisting of Trastuzumab with Pertuzumab was administered from 2017 onwards.
Surgical treatment after NST consisted of breast-conserving surgery or mastectomy and was at the discretion of the treating surgeon in consultation with the patient.
Pathologic assessment of IBC, DCIS and response
Pathologic examination was performed locally according to the Dutch guideline [12,13,14]. The majority of the pathology laboratories use the Dutch Pathology Module (PALGA) for synoptic reporting, and standard work-up includes tumor subtyping, receptor status, and grading. Receptor status was evaluated for IBC, not for the DCIS component. ER status was determined using immunohistochemistry and considered positive if ≥ 10% of tumor cells stained positive. HER2 status was examined by immunohistochemistry or in situ hybridization, or in a combination, following ASCO CAP guidelines [23]. Tumor grade of IBC was classified according to the modified Bloom-Richardson guideline [2, 5]. In this study population of neoadjuvant treated patients, in general, the IBC grade of the postoperative specimen was recorded in the NCR. In case patients achieved pCR or when the grade in the biopsy was higher, the grade of the biopsy was recorded.
From PALGA, the presence of a DCIS component was collected from the pre-NST and postoperative pathology reports per patient. The grade of the DCIS component and the presence of comedonecrosis and/or calcifications were assessed in the pre-NST biopsy. In case the presence/absence of comedonecrosis and/or calcifications was not described, these variables were not classified as absent but as “missing value”.
Patients with a recorded DCIS component present in the pre-NST biopsy report were classified as IBC+DCIS and included in the analysis on complete response of DCIS. Complete response was defined as the absence of any DCIS in the postoperative specimen. Resection specimens below 30 g were embedded entirely for microscopic review. Larger specimens were sampled at at least 1 slide per cm of the expected tumor region.
Study objectives
Primary endpoint was the percentage of pCR of DCIS in HER2-positive IBC patients with a DCIS component in the pre-NST biopsy. Secondary endpoints were association between complete response of IBC and complete response of DCIS, association of other clinicopathologic variables with complete response of DCIS, and impact of the presence of a DCIS component pre-NST on surgical treatment after NST.
Statistical analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS, version 26, Armonk, New York). Descriptive statistics were used to summarize the study population. Complete response of the DCIS component was calculated as percentage of the patients with IBC+DCIS in the pre-NST biopsy. Pearson’s χ2 test was used to compare IBC response with DCIS response, and in this analysis, IBC response was defined as the absence of invasive breast cancer after NST (ypT0/is). Clinicopathologic variables associated with complete response of DCIS were determined by univariable logistic regression analyses. Subsequently, multivariable logistic regression analyses were performed to adjust for potential confounders. A complete case analysis was performed, in which patients with missing data were excluded from the univariable and multivariable analyses. Surgical treatment was compared between patients with IBC+DCIS and patients with pure IBC in the pre-NST biopsy using Pearson’s χ2 test. A p value ≤ 0.05 was considered statistically significant.
Results
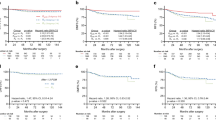
In the period of 2010–2020, 6380 women with HER2-positive IBC received NST followed by surgical treatment in the Netherlands. After exclusion of ineligible patients (n = 782), 5598 patients were included in the study population (Fig. 1). Subsequently, pathology reports were assessed for the presence of DCIS, and 1403 patients (25.1%) showed a DCIS component in the pre-NST biopsy. These patients were included in the analysis on pathologic complete response of the DCIS component. The other 4195 patients (74.9) did not show a DCIS component in the pre-NST biopsy and were excluded from further analyses on DCIS response. An overview of the patient inclusion and classification based on pathology reports is shown in Fig. 1.
Patient characteristics
Baseline characteristics of the 1403 patients with IBC+DCIS are shown in Table 1. Patients were most commonly diagnosed with cT2 tumor (50.7%), ER-positive (63.2%), and morphology of invasive carcinoma no special type (91.9%). IBC grade was most commonly grade 3 (47.7%), followed by grade 2 (46.1%). Patients with clinical tumor status Tis (n = 8) were included in the study population, since they had clinically node-positive disease and were treated with NST. Patients were classified as cTX (n = 18) when IBC was detected in pre-NST biopsy but cT status could not be determined on imaging.
Histopathologic characteristics of the DCIS component in the pre-NST biopsies are also shown in Table 1. Comedonecrosis and calcifications were present in 521 (76.8%) and 457 (61.7%) patients, respectively. The DCIS component was most often grade 3 (n = 774, 62.3%). DCIS grade and IBC grade were concordant in 61.8% of patients (616/997 patients, Supplementary Table 1).
Association between clinicopathologic variables and the complete response of DCIS to NST
As presented in Fig. 1, 52.0% of the patients with a DCIS component in the pre-NST biopsy showed pCR of the DCIS component. The number of patients with complete response of IBC (ypT0/is) in comparison to complete response of the DCIS component is shown in Table 2. Complete response of the DCIS component occurred significantly more often in case of complete response IBC compared to patients with residual IBC (63.4% versus 34.1%, p < 0.001).
The univariable and multivariable logistic regression analyses for clinicopathologic variables associated with complete response of DCIS are shown in Table 3. In univariable analyses, age at diagnosis above 50 (OR 1.41; 95% CI 1.14–1.75), year of diagnosis between 2014–2016 (OR 1.60, 95% CI 1.17–2.19) and between 2017–2019 (OR 1.76, 95% CI 1.34–2.34), clinical tumor status T3 (OR 0.59; 95% CI 0.43–0.82), and ER-negative IBC (OR 1.65; 95% CI 1.33–2.06) were significantly associated with complete DCIS response. Of the pathologic characteristics of the DCIS component, the presence of both comedonecrosis (OR 0.66; 95% CI 0.46–0.94) and calcifications (OR 0.58; 95% CI 0.43–0.78) were significantly associated with a complete response of DCIS to NST. DCIS grade and IBC grade were not associated with DCIS response.
In multivariable logistic regression analyses, year of diagnosis between 2014 and 2016 (OR 1.64; 95% CI 1.06–2.54) and 2017–2019 (OR 1.83; 95% CI 1.23–2.72, and ER-negative IBC (OR 1.81; 95% CI 1.36–2.39) were independently associated with higher odds for pCR of the DCIS component. Clinical tumor status T3 was independently associated with lower odds for pCR of the DCIS component (OR 0.57; 95% CI 0.39–0.85). The other abovementioned univariable clinicopathologic variables did not reach significance after multivariable logistic regression analysis. Comedonecrosis and calcifications were not included in the multivariable logistic regression analysis because of high numbers of missing data, resulting in too many patients being excluded from the analysis.
Surgical treatment after NST
Surgical treatment differed significantly between patients with IBC + DCIS (n = 1403) and patients with pure IBC (n = 4195) in the pre-NST biopsy. Mastectomy was more often performed as primary surgical treatment in patients with IBC + DCIS (n = 742, 52.9%) compared to pure IBC (n = 1681, 40.1%) (p < 0.001). Postoperative pathology outcomes (ypT status) are shown in Supplementary Table 2, for IBC patients and for IBC+DCIS patients, according to primary surgery treatment (BCS versus mastectomy). Of the total of 2423 patients receiving primary mastectomy, 1027 (42.4%) showed complete response (ypT0) in the postoperative pathology specimen.
Discussion
In current studies investigating response to NST in breast cancer treatment, only a few studies have been conducted on the pathologic response of DCIS to NST. To the best of our knowledge, this is the first nationwide analysis investigating a large cohort of HER2-positive IBC patients with a DCIS component, and a pCR of DCIS was found in 52.0% of 1403 patients. In addition, we demonstrated that pCR of the DCIS component was associated with complete response of IBC, ER negativity of IBC and a more recent year of breast cancer diagnosis within this study cohort. Patients with a DCIS component in the pre-NST biopsy were significantly more often treated with mastectomy after NST compared to patients without a DCIS component.
The rate of pCR of the DCIS component is consistent with the outcomes of previous, smaller studies. Groen et al. and von Minckwitz et al. investigated the response of a DCIS component in HER2-positive IBC patients and found a complete response in 46% and 51% of these patients, respectively [7, 22]. Sun et al. found a slightly lower response rate of 35.7% in their population of 129 HER2-postive IBC patients [18]. Goldberg et al. investigated the response of a DCIS component in IBC patients treated with NST and found a response rate of 33%. This lower response rate can be explained by the study population consisting of different IBC subtypes, including HER2-negative. In comparison to these previous studies, a significantly larger number of patients was included in our study. Therefore, this study may be seen as a confirmation of previous results.
In addition, the potential association between clinicopathologic variables and DCIS response was investigated. First, it was found that complete response of the DCIS component occurred significantly more often in case of complete response of IBC (63.4% versus 34.1%, p < 0.001). Previous studies show a high concordance in receptor status and grade between IBC and the accompanying DCIS component [15,16,17]. In our multivariable analysis, ER-negative IBC was found to be significantly associated with complete response of DCIS, which is also associated with higher rates of pCR of the invasive tumor in previous studies [8, 20]. Given that IBC and the accompanying DCIS are comparable in morphology, their response could be affected by the same factors [15,16,17]. In addition, year of diagnosis between 2014 and 2016 and 2017–2019 was significantly associated with complete response of DCIS. This could be explained by the continuous improvements in NST in the recent years, including dual anti-HER2 blockade from 2017 onwards. Unfortunately, our database did not include information on treatment with single or dual anti-HER2 blockade. Yet, Groen et al. did find an independent association of dual anti-HER2 blockade with DCIS response in their analysis of 138 HER2+IBC patients with a DCIS component [7].
This study has strengths and limitations. A strength is the nationwide database of the NCR combined with the Dutch Nationwide Pathology Databank that allowed for evaluation of DCIS response on a large scale, in comparison to previous smaller study populations. Second, various clinicopathologic variables were taken into consideration, which enabled evaluation of association between clinicopathologic variables and complete response of the DCIS component.
There are certain limitations worth mentioning. First, due to the retrospective nature of our database, some variables are missing because of insufficient reporting, in particular regarding the pathologic characteristics of the DCIS component. The presence of a DCIS component in the postoperative specimen is a mandatory field in the Dutch Pathology Module since 2009. Unfortunately, the presence of a DCIS component in the pre-NST biopsy is not a mandatory field in completing the module. However, it has been added as an optional field as of 2016 and is often additionally described in the report. Nevertheless, this could have led to an underreporting of the DCIS component pre-NST by the pathologist focusing on the invasive tumor. Moreover, previous research shows there is a high inter-observer variation between pathologists and laboratories in grading DCIS, and the receptor status of the DCIS component is not yet a standard determination [21]. Therefore, these pathologic characteristics of the DCIS component could not be investigated properly in relation to response.
Second, the pre-NST biopsy collection generates another limitation. Since DCIS can appear outside of the area of the invasive tumor, there may be a risk of missing the DCIS component, when targeting the invasive tumor during biopsy. The presence of a DCIS component can therefore be underestimated and this may affect the complete response rate. Moreover, the location and size of the DCIS component outside of the invasive tumor can influence the possibility to perform breast-conserving surgery, but this was not possible to investigate based on the pre-NST pathology reports. Lastly, the higher mastectomy rate in the patients with a DCIS component could not be further evaluated because our database did not include relevant clinical data (e.g., gene expression, extent of mammographic calcifications, the use of oncoplastic and reconstructive surgery, and patients’ preference regarding surgical treatment).
Further research into complete response of DCIS in HER2-positive IBC is important, because our study confirms the increased mastectomy rate found in previous studies in patients with IBC+DCIS versus patients without a DCIS component (52.9% versus 40.1%, p < 0.001) [10, 24]. In order to implement the potential response of the DCIS component in personalizing surgical treatment after NST, future studies should evaluate whether it is possible to monitor response of the DCIS component by imaging modalities. Moreover, a thorough investigation of pathologic characteristics of the DCIS component in relation to response could be useful to predict DCIS response before start of NST.
In conclusion, in this nationwide retrospective study, we demonstrated that pCR of DCIS to NST occurred in 52.0% of the HER2-positive IBC patients with a DCIS component in pre-NST biopsy. These findings are important to create awareness that the presence of a DCIS component in particular should not necessarily indicate the need for mastectomy. Future studies should investigate the evaluation of DCIS response by imaging and the possibility of increasing the chance of breast-conserving surgery. In addition, further assessment of specific pathologic characteristics of DCIS related to response could possibly predict the chance of pCR.
Data availability
The data used for this retrospective study were obtained via The Netherlands Comprehensive Cancer Organization (IKNL) from the Netherlands Cancer Registry. This specific dataset is generated for the current study by the registration team of IKNL after permission by their privacy board. Therefore, restrictions apply to the availability of the data and this specific dataset is not publicly available. However, the data are available upon reasonable request and with permission of the IKNL.
References
Amoroso V, Generali D, Buchholz T et al (2015) International expert consensus on primary systemic therapy in the management of early breast cancer: highlights of the fifth symposium on primary systemic therapy in the management of operable breast cancer, Cremona, Italy (2013). J Natl Cancer Inst Monogr 2015:90–96. https://doi.org/10.1093/jncimonographs/lgv023
Bloom HJ, Richardson WW (1957) Histological grading and prognosis in breast cancer; a study of 1409 cases of which 359 have been followed for 15 years. Br J Cancer 11:359–377. https://doi.org/10.1038/bjc.1957.43
Casparie M, Tiebosch AT, Burger G et al (2007) Pathology databanking and biobanking in The Netherlands, a central role for PALGA, the nationwide histopathology and cytopathology data network and archive. Cell Oncol 29:19–24. https://doi.org/10.1155/2007/971816
Doebar SC, van den Broek EC, Koppert LB et al (2016) Extent of ductal carcinoma in situ according to breast cancer subtypes: a population-based cohort study. Breast Cancer Res Treat 158:179–187. https://doi.org/10.1007/s10549-016-3862-4
Elston CW, Ellis IO (1991) Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 19:403–410. https://doi.org/10.1111/j.1365-2559.1991.tb00229.x
Fisher B, Bryant J, Wolmark N et al (1998) Effect of preoperative chemotherapy on the outcome of women with operable breast cancer. J Clin Oncol 16:2672–2685. https://doi.org/10.1200/JCO.1998.16.8.2672
Groen EJ, van der Noordaa MEM, Schaapveld M et al (2021) Pathologic response of ductal carcinoma in situ to neoadjuvant systemic treatment in HER2-positive breast cancer. Breast Cancer Res Treat 189:213–224. https://doi.org/10.1007/s10549-021-06235-2
Houssami N, Macaskill P, von Minckwitz G, Marinovich ML, Mamounas E (2012) Meta-analysis of the association of breast cancer subtype and pathologic complete response to neoadjuvant chemotherapy. Eur J Cancer 48:3342–3354. https://doi.org/10.1016/j.ejca.2012.05.023
Kaufmann M, von Minckwitz G, Mamounas EP et al (2012) Recommendations from an international consensus conference on the current status and future of neoadjuvant systemic therapy in primary breast cancer. Ann Surg Oncol 19:1508–1516. https://doi.org/10.1245/s10434-011-2108-2
Kole AJ, Park HS, Johnson SB, Kelly JR, Moran MS, Patel AA (2019) Overall survival is improved when DCIS accompanies invasive breast cancer. Sci Rep 9:9934. https://doi.org/10.1038/s41598-019-46309-2
Labrosse J, Morel C, Lam T et al (2021) The presence of an in situ component on pre-treatment biopsy is not associated with response to neoadjuvant chemotherapy for breast cancer. Cancers (Basel). https://doi.org/10.3390/cancers13020235
NABON (2008) Dutch Guideline ‘Treatment of breast cancer’ (Richtlijn ‘Behandeling van het Mammacarcinoom’). Available at: https://richtlijnendatabase.nl/richtlijn/borstkanker/algemeen.html
NABON (2012) Dutch Guideline ‘Treatment of breast cancer’ (Richtlijn ‘Behandeling van het Mammacarcinoom’). Available at: https://richtlijnendatabase.nl/richtlijn/borstkanker/algemeen.html
NABON (2017) Dutch Guideline ‘Treatment of breast cancer’ (Richtlijn ‘Behandeling van het Mammacarcinoom’). Available at: https://richtlijnendatabase.nl/richtlijn/borstkanker/algemeen.html
O’Connell P, Pekkel V, Fuqua S, Osborne CK, Allred DC (1994) Molecular genetic studies of early breast cancer evolution. Breast Cancer Res Treat 32:5–12. https://doi.org/10.1007/bf00666201
Park K, Han S, Kim HJ, Kim J, Shin E (2006) HER2 status in pure ductal carcinoma in situ and in the intraductal and invasive components of invasive ductal carcinoma determined by fluorescence in situ hybridization and immunohistochemistry. Histopathology 48:702–707. https://doi.org/10.1111/j.1365-2559.2006.02403.x
Steinman S, Wang J, Bourne P, Yang Q, Tang P (2007) Expression of cytokeratin markers, ER-alpha, PR, HER-2/neu, and EGFR in pure ductal carcinoma in situ (DCIS) and DCIS with co-existing invasive ductal carcinoma (IDC) of the breast. Ann Clin Lab Sci 37:127–134
Sun S, van la Parra RFD, Rauch GM et al (2019) Patient selection for clinical trials eliminating surgery for HER2-positive breast cancer treated with neoadjuvant systemic therapy. Ann Surg Oncol 26:3071–3079. https://doi.org/10.1245/s10434-019-07533-2
Tolaney SM, Barry WT, Dang CT et al (2015) Adjuvant paclitaxel and trastuzumab for node-negative, HER2-positive breast cancer. N Engl J Med 372:134–141. https://doi.org/10.1056/NEJMoa1406281
Untch M, Rezai M, Loibl S et al (2010) Neoadjuvant treatment With trastuzumab in HER2-positive breast cancer: results from the geparquattro study. J Clin Oncol 28:2024–2031. https://doi.org/10.1200/jco.2009.23.8451
van Dooijeweert C, van Diest PJ, Willems SM, Kuijpers C, Overbeek LIH, Deckers IAG (2019) Significant inter- and intra-laboratory variation in grading of ductal carcinoma in situ of the breast: a nationwide study of 4901 patients in the Netherlands. Breast Cancer Res Treat 174:479–488. https://doi.org/10.1007/s10549-018-05082-y
von Minckwitz G, Darb-Esfahani S, Loibl S et al (2012) Responsiveness of adjacent ductal carcinoma in situ and changes in HER2 status after neoadjuvant chemotherapy/trastuzumab treatment in early breast cancer–results from the GeparQuattro study (GBG 40). Breast Cancer Res Treat 132:863–870. https://doi.org/10.1007/s10549-011-1621-0
Wolff AC, Hammond MEH, Allison KH et al (2018) Human Epidermal growth factor receptor 2 testing in breast cancer: American society of clinical oncology/college of American pathologists clinical practice guideline focused update. J Clin Oncol 36:2105–2122. https://doi.org/10.1200/jco.2018.77.8738
Wong H, Lau S, Yau T, Cheung P, Epstein RJ (2010) Presence of an in situ component is associated with reduced biological aggressiveness of size-matched invasive breast cancer. Br J Cancer 102:1391–1396. https://doi.org/10.1038/sj.bjc.6605655
Wu W, Kamma H, Ueno E et al (2002) The intraductal component of breast cancer is poorly responsive to neo-adjuvant chemotherapy. Oncol Rep 9:1027–1031
Acknowledgements
The authors gratefully thank the registration team of the Netherlands Comprehensive Cancer Organization for the collection of the data for the NCR. Furthermore, the authors gratefully thank the Dutch Nationwide Pathology Databank (PALGA) for providing the histopathologic data.
Funding
For this study, R. Ploumen received a grant from the Jules Coenegracht Senior Foundation (Maastricht, the Netherlands). The funder had no role in the conceptualization, data collection, analysis, interpretation, or writing.
Author information
Authors and Affiliations
Contributions
RAWP, LFSK, TJAN, and MLS contributed to the study conception and design. Data acquisition and collection were performed by RAWP, TJAN, MLS, and SS. Data interpretation and (statistical) analysis were performed by RAWP, ELC, LFSK, MACEK, SS, TJAN, and MLS. The first draft was written by RAWP and ELC, whereafter all authors provided feedback on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare the following financial interests/personal relationships: Prof. Dr. Smidt reports grants from Nutricia and Servier Pharmaceuticals for microbiome research in colorectal cancer, not related to this study. Dr. T. van Nijnatten received institutional grant support from Bayer, and speaker honoraria from GE Healthcare and Bayer, not related to this study. L. Kooreman reports consulting fees from Novartis and educational fees from SCEM, not related to this study. All other authors declare no conflicts of interest.
Ethical approval
The current study was approved by the institutional ethics and privacy committee of The Netherlands Comprehensive Cancer Organization (IKNL) after reviewing the study protocol.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ploumen, R.A.W., Claassens, E.L., Kooreman, L.F.S. et al. Pathologic complete response of ductal carcinoma in situ to neoadjuvant systemic therapy in HER2-positive invasive breast cancer patients: a nationwide analysis. Breast Cancer Res Treat 201, 227–235 (2023). https://doi.org/10.1007/s10549-023-07012-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-07012-z