Abstract
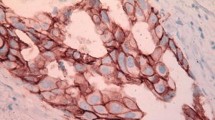
Adjacent ductal carcinoma in situ (DCIS) is found in approximately 45% of invasive ductal carcinomas (IDC) of the breast. Pure DCIS overexpresses HER2 in approximately 45%. There is uncertainty whether adjacent DCIS impacts on the response to neoadjuvant chemotherapy and trastuzumab as well as whether HER2 expression in IDC component or adjacent DCIS changes throughout treatment. Core biopsies and surgical tissue from participants of the GeparQuattro study with HER2-positive IDC were centrally examined for the area of invasive ductal component and adjacent DCIS before and after receiving neoadjuvant anthracycline–taxane–trastuzumab containing chemotherapy. HER2 overexpression in IDC and adjacent DCIS was quantified separately by immunohistochemistry using the Ventana™ automated staining system. Pathological complete response (pCR) was defined as no residual invasive or non-invasive tumor tissue. Fifty-nine (37.3%) of 158 IDCs presented with adjacent DCIS at diagnosis. These tumors showed lower regression grades than pure IDC (P = 0.033). The presence of adjacent DCIS was an independent negative predictor of pCR [odds ratio 0.42 (95% CI 0.2–0.9), P = 0.027]. Adjacent DCIS area decreased from pre-treatment to surgery (r = 0.205) with 30 (50.8%) IDCs with adjacent DCIS showing complete eradication of adjacent DCIS. HER2 status of adjacent DCIS was highly correlated with HER2 status of IDC component before (r = 0.892) and after treatment (r = 0.676). Degree of HER2 overexpression of the IDC component decreased in 16 (33.3%) out of 49 patients without a pCR. These 16 IDCs showed lower RGs compared to the 33 IDCs with unchanged HER2 expression (P = 0.055). HER2-positive IDCs with adjacent DCIS is less responsive to neoadjuvant chemotherapy and trastuzumab compared to pure IDC. However, complete eradication of adjacent DCIS is frequently observed. HER2-overexpression of the invasive ductal component decreases in a subset of tumors, which showed less tumor regression.

Similar content being viewed by others
References
Gao Y, Niu Y, Wang X, Wei L, Lu S (2009) Genetic changes at specific stages of breast cancer progression detected by comparative genomic hybridization. J Mol Med 87:145–152
Steinman S, Wang J, Bourne P, Yang Q, Tang P (2007) Expression of cytokeratin markers, ER-alpha, PR, HER-2/neu, and EGFR in pure ductal carcinoma in situ (DCIS) and DCIS with co-existing invasive ductal carcinoma (IDC) of the breast. Ann Clin Lab Sci 37:127–134
Aubele M, Mattis A, Zitzelsberger H, Walch A, Kremer M, Welzl G, Hofler H, Werner M (2000) Extensive ductal carcinoma in situ with small foci of invasive ductal carcinoma: evidence of genetic resemblance by CGH. Int J Cancer 85:82–86
Alexe G, Dalgin GS, Ganesan S, Delisi C, Bhanot G (2007) Analysis of breast cancer progression using principal component analysis and clustering. J Biosci 32:1027–1039
Iakovlev V, Arneson N, Wong V, Wang C, Leung S, Iokovleva G, Warren K, Pintilie M, Done S (2008) Genomic differences between pure ductal carcinoma in situ of the breast and that associated with invasive disease: a calibrated aCGH study. Clin Cancer Res 14:4446–4454
Wong H, Lau S, Yau T, Cheung P, Epstein RJ (2010) Presence of an in situ component is associated with reduced biological aggressiveness of size-matched invasive breast cancer. Br J Cancer 102(9):1391–1396
Lebeau A, Unholzer A, Amann G, Kronawitter M, Bauerfeind I, Sendelhofert A, Iff A, Löhrs U (2003) EGFR, HER-2/neu, cyclin D1, p21 and p53 in correlation to cell proliferation and steroid hormone receptor status in ductal carcinoma in situ of the breast. Breast Cancer Res Treat 79(2):187–198
Stackievicz R, Paran H, Bernheim J, Shapira M, Weisenberg N, Kaufman T, Klein E, Gutman M (2010) Prognostic significance of HER-2/neu expression in patients with ductal carcinoma in situ. Isr Med Assoc J 12(5):290–295
Kühn T (2010) Ductal carcinoma in situ: clinical perspective. Breast Care 5:227–232
von Minckwitz G, Rezai M, Loibl S, Fasching PA, Huober J, Tesch H, Bauerfeind I, Hilfrich J, Eidtmann H, Gerber B, Hanusch C, Kühn T, du Bois A, Blohmer JU, Thomssen C, Dan Costa S, Jackisch C, Kaufmann M, Mehta K, Untch M (2010) Capecitabine in addition to anthracycline- and taxane-based neoadjuvant treatment in patients with primary breast cancer: phase III GeparQuattro study. J Clin Oncol 28(12):2015–2023
Untch M, Rezai M, Loibl S, Fasching PA, Huober J, Tesch H, Bauerfeind I, Hilfrich J, Eidtmann H, Gerber B, Hanusch C, Kühn T, du Bois A, Blohmer JU, Thomssen C, Dan Costa S, Jackisch C, Kaufmann M, Mehta K, von Minckwitz G (2010) Neoadjuvant treatment with trastuzumab in HER2-positive breast cancer: results from the GeparQuattro study. J Clin Oncol 28(12):2024–2031
Sinn HP, Schmid H, Junkermann H (1994) Histologic regression of breast cancer after primary (neoadjuvant) chemotherapy. Geburtshilfe Frauenheilkd 54:552–558
Guarneri V, Barbieri E, Dieci MV, Piacentini F, Conte P (2010) Anti-HER2 neoadjuvant and adjuvant therapies in HER2 positive breast cancer. Cancer Treat Rev 36(Suppl 3):S62–S66
Kuerer HM, Buzdar AU, Mittendorf EA, Esteva FJ, Lucci A, Vence LM, Radvanyi L, Meric-Bernstam F, Hunt KK, Symmans WF (2011) Biologic and immunologic effects of preoperative trastuzumab for ductal carcinoma in situ of the breast. Cancer 117:39–47
von Minckwitz G, Kaufmann M, Kümmel S, Fasching PA, Eiermann W, Blohmer JU, Costa SD, Hilfrich J, Jackisch C, Gerber B, du Bois A, Huober J, Hanusch C, Konecny G, Fett W, Stickeler E, Harbeck N, Mehta K, Loibl S, Untch M for the GBG and AGO-B study groups (2011) Correlation of various pathological complete response (pCR) definitions with long-term outcome and the prognostic value of pCR in various breast cancer subtypes. Results from the German neoadjuvant meta-analysis. J Clin Oncol 29(suppl):2011. Abstract 1028. ASCO 2011
Untch M, Fasching PA, Konecny GE, Hasmüller S, Lebeau A, Kreienberg R, Camara O, Müller V, du Bois A, Kühn T, Stickeler E, Harbeck N, Höss C, Kahlert S, Beck T, Fett W, Mehta K, von Minckwitz G, Loibl S (2011) Pathological complete response after neoadjuvant chemotherapy plus trastuzumab predicts favorable survival in HER2-overexpressing breast cancer—results from the TECHNO trial of the AGO and GBG study groups. J Clin Oncol (in press)
Gianni L, Eiermann W, Semiglazov V, Manikhas A, Lluch A, Tjulandin S, Zambetti M, Vazquez F, Byakhow M, Lichinitser M, Climent MA, Ciruelos E, Ojeda B, Mansutti M, Bozhok A, Baronio R, Feyereislova A, Barton C, Valagussa P, Baselga J (2010) Neoadjuvant chemotherapy with trastuzumab followed by adjuvant trastuzumab versus neoadjuvant chemotherapy alone, in patients with HER2-positive locally advanced breast cancer (the NOAH trial): a randomised controlled superiority trial with a parallel HER2-negative cohort. Lancet 375:377–384
Untch M, Loibl S, Bischoff J, Eidtmann H, Kaufmann M, Blohmer J-U, Hilfrich J, Strumberg D, Fasching PA, Kreienberg R, Tesch H, Hanusch C, Gerber B, Rezai M, Jackisch C, Huober J, Kuehn T, Nekljudova V, von Minckwitz G (2010) Lapatinib vs trastuzumab in combination with neoadjuvant anthracycline–taxane-based chemotherapy: primary efficacy endpoint analysis of the GEPARQUINTO STUDY (GBG 44). SABCS, San Antonio, Dec 2010. Abstract S3-1
Baselga J, Bradbury I, Eidtmann H, Di Cosimo S, Aura C, De Azambuja E, Gomez H, Dinh P, Fauria K, Van Dooren V, Paoletti P, Goldhirsch A, Chang T-W, Lang I, Untch M, Gelber RD, Piccart-Gebhart M, on Behalf of the NeoALTTO Study Team. First results of the NeoALTTO Trial (BIG 01-06/EGF 106903): A Phase III, randomized, open label, neoadjuvant study of lapatinib, trastuzumab, and their combination plus paclitaxel in women with HER2-positive primary breast cancer. SABCS, San Antonio, Dec 2010. Abstract S3-3
Gianni L, Pienkowski T, Im Y-H, Roman L, Tseng L-M, Liu M-C, Lluch-Hernandez A, Semiglazov V, Szado T, Ross G. Neoadjuvant pertuzumab (P) and trastuzumab (H): antitumor and safety analysis of a randomized phase II study (‘NeoSphere’). SABCS, San Antonio, Dec 2010. Abstract S3-2
Acknowledgments
We would like to thank Britta Bayer for her excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study is conducted for the German Breast Group and the AGO Breast Group.
Rights and permissions
About this article
Cite this article
von Minckwitz, G., Darb-Esfahani, S., Loibl, S. et al. Responsiveness of adjacent ductal carcinoma in situ and changes in HER2 status after neoadjuvant chemotherapy/trastuzumab treatment in early breast cancer—results from the GeparQuattro study (GBG 40). Breast Cancer Res Treat 132, 863–870 (2012). https://doi.org/10.1007/s10549-011-1621-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-011-1621-0