Abstract
Purpose
To examine how treatment delays brought on by the COVID-19 pandemic impacted the physical and emotional well-being of physicians treating these patients.
Methods
A cross-sectional survey of physician breast specialists was posted from April 23rd to June 11th, 2020 on membership list serves and social media platforms of the National Accreditation Program for Breast Centers and the American Society of Breast Surgeons. Physician well-being was measured using 6 COVID-19 burnout emotions and the 4-item PROMIS short form for anxiety and sleep disturbance. We examined associations between treatment delays and physician well-being, adjusting for demographic factors, COVID-19 testing and ten COVID-19 pandemic concerns.
Results
870 physicians completed the survey, 61% were surgeons. The mean age of physicians was 52 and 548 (63.9%) were female. 669 (79.4%) reported some delay in patient care as a result of the COVID-19 pandemic. 384 (44.1%) and 529 (60.8%) of physicians scored outside normal limits for anxiety and sleep disturbance, respectively. After adjusting for demographic factors and COVID-19 testing, mean anxiety and COVID-19 burnout scores were significantly higher among physicians whose patients experienced either delays in surgery, adjuvant chemotherapy, radiation, breast imaging or specialty consultation. A multivariable model adjusting for ten physician COVID-19 concerns and delays showed that “delays will impact my emotional well-being” was the strongest concern associated with anxiety, sleep disturbance and COVID-19 burnout factors.
Conclusions
Breast cancer treatment delays during the initial surge of the COVID-19 pandemic in the United States were associated with a negative impact on physician emotional wellness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
On January 20, 2020 the first infection with SARS CoV-2 in the United States was reported in Washington State [1]. Since then, over 9 million cases have been reported with over 220,000 deaths [2]. The COVID-19 pandemic required health systems and physicians to prioritize which patients required the most urgent care and resulted in many delays in standard treatment algorithms particularly for patients with cancer. Additionally, on March 13, 2020 the American College of Surgeons (ACS) issued a recommendation to cancel all elective surgeries [3] to conserve personal protective equipment and other resources for COVID-19 positive patients. Although it was questionable whether cancer surgery was considered “elective”, these recommendations were quickly followed by consensus statements from many different societies on how to manage delays in cancer surgery including patients with breast cancer [4,5,6]. A recent survey [7] concluded that 50% of breast centers in Europe reported altered systemic treatments resulting from the COVID-19 pandemic and 20% of patients experienced delays in radiation therapy. However, data on delays for patients with breast cancer in the United States have not yet been reported.
At the time that elective cases were being canceled or delayed, several studies were published that showed that patients with cancer who were infected with SARS CoV-2 were experiencing high rates of death from COVID-19 [8, 9]. Breast physician specialists had to weigh delaying treatment for these patients to conserve resources or proceed with treatment and potentially increase the risk of infection with SARS CoV-2 for their patients and its negative sequelae on outcomes. However, little empirical evidence exists to describe how these delays impacted the physical and emotional well-being of physicians treating these patients. Studies conducted outside the United States have shown that physicians directly caring for patients infected with SARS CoV-2 impacts physician well-being. A study of over 1200 frontline healthcare workers in China in January 2020 reported depression was experienced in approximately 50%, anxiety in 44% and insomnia in 30% [10]. Similarly, another study of 376 healthcare workers from Italy found high rates of emotional exhaustion and somatic symptoms from frontline care of COVID-19 positive patients [11]. A recent meta-analysis of 13 studies showed that just over 20% of frontline workers experienced depression and anxiety [12]. However, these studies examined physicians and other healthcare workers taking direct care of COVID-19 infected patients. There is little empirical evidence examining physicians who were not necessarily caring directly for patients infected by SARS CoV-2 but who were nonetheless experiencing downstream effects of the COVID-19 pandemic such as an inability to provide timely and standard care for their patients with a diagnosed cancer. The impact on physician well-being could potentially affect the future medical care of patients (in the post-pandemic period) since physician well-being and burnout emotions are directly associated with medical errors, absenteeism, relationship discord and substance abuse [13].
To further explore pandemic-related breast cancer treatment delays and potential effects on physicians treating breast cancer, we used a cross sectional survey administered to breast specialists across the country during the initial surge of COVID-19 cases. First, we assessed the scope of treatment delays for breast cancer patients. Second, we assessed the association of these delays with physician anxiety, sleep disturbance and emotions associated with physician burnout.
Methods
Study design and setting
A cross sectional survey was created using a convenience sample of multispecialty physicians specializing in breast cancer. The survey was distributed using RedCap to members of NAPBC-accredited breast centers and ASBrS via social media posts, email and list serves of the ACS and the ASBrS from April 23rd to June 11th, 2020 (See supplementary materials for full version of the survey). Survey questions were created by a group of ten breast physician specialists from across the country based on personal conversations with colleagues, newspaper or social media articles commenting on physician wellness at the time of the study or stories in the news or radio. The 27-item survey was composed of four domains: COVID-19 testing questions, delays or altered treatment plans, COVID-19 concerns and demographic factors (see Appendix for full survey). COVID testing questions focused on coronavirus testing, direct care of infected patients and personal knowledge of persons (non-patients) infected by SARS CoV-2 during that period. Physicians were asked about their perception of how delayed treatments impacted their patient’s overall survival and delivery of care. COVID-19 concerns included how the pandemic was impacting physicians personal and professionally. Demographic factors including number of breast cancer patients seen weekly, age, gender, time in practice, location of practice (by State), type of practice and specialty were also collected.
This study was approved by the Institutional Review Board at NorthShore University HealthSystem. Completion of the survey was considered consent to participate in the study and all responses were de-identified such that responses could not be linked to individual respondents or centers.
Participants
Only physicians who treated breast cancer patients in some capacity and were members of the aforementioned medical societies were eligible to participate. All specialties in breast cancer care were represented, including: surgery, medical and radiation oncology, breast imaging, geneticists, pathology and survivorship.
Outcome measures
Physician anxiety and sleep disturbance were measured with the Patient Reported Outcomes Measurement Information System (PROMIS) 4-item Anxiety and Sleep Disturbance short forms [14, 15]. These validated measures are based on a t-score metric with a mean of 50 and standard deviation of 10. A brief measure of COVID-19 related burnout symptoms was created for this study and was based on known emotions related to physician burnout, including emotional exhaustion, depression, helplessness, and anxiety. This was scored by computing a summary score of these 6 items which were based on a Likert scale of 0 = not at all to 4 = very much) with a possible score range from 0 to 24. In this study, this measure had a normal distribution, with a mean (± SD) of 8.9 ± 6.3. It was strongly correlated with the PROMIS Anxiety scale (r = 0.72) and weakly correlated with the PROMIS Sleep Disturbance scale (r = 0.20). The 6 item set demonstrated strong internal consistency reliability (Chronbach’s α = 0.91), which was not improved by removing any single item.
Statistical analysis
Descriptive statistics and measures of central tendency (e.g., frequencies, percentages, means, standard deviations (SD) were used to summarize the survey results. Pearson correlation coefficients and Chronbach’s α were used to assess preliminary psychometric characteristics of the COVID-19 related burnout item set that was administered. Bivariate differences in outcomes between groups were assessed with the chi-square test or univariate general linear models. Cohen’s d effect sizes were calculated to determine the magnitude of effect of delays on physician emotional well being (d = 0–0.19 trivial effect, 0.20–0.49 small effect, 0.50–0.79 medium effect and > 0.80 large effect). Multivariate general linear models controlling for physician age, gender, years in practice, testing positive for SARS CoV-2 and caring for COVID-19 positive patients using physician wellness and opinions about delays as the outcomes were used to assess differences between physicians whose patients did and did not experience treatment delays. Multiple comparisons between groups were made using the Tukey–Kramer adjustment. Multivariable general linear models with standardized regression coefficients and backward selection method using p < 0.05 to remain in the model were used to identify the treatment delays and COVID-19 concerns most strongly associated with outcomes. Analysis of items with missing data were performed with non-missing observations only. All statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC). p values < 0.05 were considered significant and all tests were two sided.
Results
Demographics of the physician cohort
870 physicians completed the survey. Missing data did not exceed 5% for any individual survey item. Responding physician demographics are listed in Table 1. Mean age was 52 + 11 and 63.9% were female. Surgeons comprised the largest group (n = 547, 61.7%). Participants came from all nine U.S. Census divisions with the greatest proportion from the East North Central division (n = 197, 22.6%) (Fig. 1). 113 (13%) of physicians underwent testing for SARS CoV-2 and only eleven (9.8%) tested positive.
Treatment delays in breast cancer care
Treatment delays and mean length of delays were examined by facility location, practice setting and specialty type (Supplementary Table 1). Overall, 669 (79.4%) physicians reported at least some delay in either breast surgery, systemic or radiation therapy, breast imaging or specialty consultation. Delays in breast surgery (n = 479, 59.4%) and breast imaging (n = 427, 51.6%) were most common. Most respondents (n = 317, 43.3%) reported average delays of one month, 230 (31.4%) reported 2 months, 156 (21.3%) reported 3 months and 29 (4.0%) reported 4 months or longer.
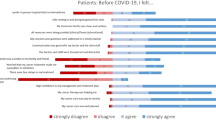
Physician concerns about the COVID-19 pandemic and treatment delays
Surgeons were asked to choose which factors concerned them the most about treatment delays. “Patients becoming anxious” was the factor chosen with the greatest frequency (n = 579, 66.6%), “delays will impact overall survival of patients” was the second most frequent factor (n = 345, 39.7%) and “cancer will get larger” (n = 286, 32.9%) was the third most frequent factor (Supplementary Fig. 1). When physicians were asked about how certain factors related to the pandemic were impacting their practice or personal well-being, 437 (51.3%) of physicians stated they were very or somewhat concerned “that my emotional well-being will be impacted by delays” (Fig. 2).
Physician outcomes of anxiety, sleep disturbance and COVID-19 related burnout
Based on recommended cut-off points for PROMIS Anxiety and Sleep Disturbance scores (0–54 = normal, 55–60 = mild, 61–70 = moderate, > 70 = severe) [16], 384 (44.1%) and 529 (60.8%) of the sample were outside normal limits for anxiety and sleep disturbance respectively. A quarter of the sample (n = 220, 25.3%) reported mild symptoms of anxiety with roughly twice as many reporting symptoms of mild sleep disturbance 466 (53.6%). Amongst the COVID-19 related burnout emotions, “emotional exhaustion” was reported with the highest frequency (n = 291, 33.6%), “anxious” was the second most common (n = 225, 26.1%) and “burnout” was the third most common (n = 190, 22.1%).
Physician anxiety, sleep disturbance and COVID-19 related burnout were significantly associated with demographic factors including COVID-19 testing factors (Table 2). Anxiety and COVID-19 related burnout were significantly associated with physician age, gender and years in practice and sleep disturbance was significantly associated with physician age. There were no significant differences in physician anxiety, sleep disturbance and COVID-19 related burnout between different facility locations, practice settings or physician specialty type. Physicians who took care of COVID-19 positive patients reported significantly higher anxiety, sleep disturbance and COVID-19 related burnout than physicians who did not take care of COVID-19 positive patients (54.5 + 8.6 vs 51.4 + 8.2, p≤ 0.001; 55.2 + 3.7 vs 54.3 + 3.8, p = 0.03; 10.2 + 6.7 vs 7.6 + 5.9, p ≤ 0.001 respectively). Furthermore, physicians who tested positive for SARS CoV-2 reported significantly lower anxiety (48.1 + 8.8 vs 54.5 + 9.1, p = 0.03) and sleep disturbance scores (51.3 + 7.3 vs 54.5 + 3.7, p = 0.02) than those who tested negative for SARS CoV-2.
Physicians whose patients experienced delays in either surgery, adjuvant therapy, breast imaging, radiation therapy, or specialty consultation reported significantly higher anxiety (53.4 + 8.3 vs 50.5 + 8.3, p ≤ 0.001) and COVID-19-related burnout (9.5 + 6.3 vs 7.0 + 6.2, p ≤ 0.001) than those who did not experience delays after adjusting for demographic factors, testing positive for SARS CoV-2 and taking care of COVID-19 patients (Table 2). Examination of Cohen’s d effect sizes suggests that the majority of significant group differences were small in magnitude, however, burnout score differences between groups who experienced delays in specialty consultations were medium in size (d = 0.55).
Nearly half (n = 391, 47.4%) of physicians somewhat or strongly agreed that treatment delays would impact their patient’s overall survival but the majority (n = 623, 73.0%) somewhat or strongly agreed that they were still able to deliver the same high quality care during the COVID-19 pandemic as before the pandemic (Table 3). Physicians who perceived the delays would impact their patient’s survival reported significantly higher anxiety, COVID-19 related burnout and sleep disturbance than physicians who did not feel the delays would impact survival, after adjusting for the aforementioned confounders (54.3 + 8.2 vs 51.2 + 8.0, p ≤ 0.001; 54.9 + 3.8 vs 54.0 + 4.0, p = 0.005; 10.2 + 6.5 vs 7.6 + 5.9, p ≤ 0.001 , respectively) (Table 3). Physicians who felt they could deliver the same high-quality care reported significantly lower anxiety and COVID-19 related burnout compared with physicians who did not feel they could deliver high-quality care (52.2 + 8.2 vs 53.6 + 9.7, p ≤ 0.001; 8.5 + 6.2 vs 9.4 + 7.1, p = 0.002, respectively) (Table 3).
Of the 10 physician concerns about the COVID-19 pandemic (Fig. 2) and the five different treatment delays, “that my emotional well-being will be impacted by delays” was most strongly associated physician concern with anxiety, sleep disturbance and COVID-19 related burnout on multivariable analysis adjusting for physician demographic factors (Supplementary Table 2).
Discussion
For the first time in many physicians’ careers, physicians were forced to delay or significantly alter treatments for their patients because of the COVID-19 pandemic. Our study of over 800 breast specialists across the United States demonstrates that delays for breast cancer patients were quite common with nearly 80% of physicians reporting some type of delay in either screening, systemic treatment or surgery for their patients. During the study period, these same physicians also reported an impact in their physical well-being more than emotional well-being; approximately 44% of all responding physicians had anxiety scores outside the normal ranges, compared to 60% of physicians reporting sleep disturbance scores. We also showed that physicians whose patients experienced delays had higher anxiety and more frequent COVID-19 burnout emotions such as emotional and physical exhaustion, depression and helplessness than physicians who did not have patients experiencing delays. However, the magnitude of these differences was not large. The reasons for these low effect sizes may be multifactorial and not necessarily all captured in our survey. The majority of physicians in this study did not have direct contact with COVID-19 positive patients, there was regional variation in hospital response to the pandemic which would directly impact physician wellness and regional variation in prevalence of the pandemic at the time of the study. Of note, burnout rates were relatively low in this physician population likely because many physicians were not working on the “frontline”. Nonetheless, our data show that the COVID-19 pandemic had at least some impact on physician wellness and in most cases a negative impact.
Physicians expressed many concerns about pandemic-related treatment delays and the direct impact these delays on their patients’ breast cancer outcomes. Nearly half of physicians thought that treatment delays would impact their patients’ survival outcomes. Although the survey did not specifically question which type of treatment delay was perceived to impact survival, our data suggests that the most common delays that occurred were for definitive surgery, corresponding to the majority of respondents being surgeons. However, surgery is often not the first method of treatment for a newly diagnosed breast cancer patient and there are short term alternative treatments for some types of breast cancer besides immediate surgery. For patients with hormone receptor negative or Her2/neu over-expressed disease, neoadjuvant chemotherapy or HER2/neu targeted therapy is preferred and recommended by guidelines [17], with no negative impact on survival. In fact, a recent consortium recommendation statement outlined which breast cancer surgical cases could be safely delayed to later in the course of treatment [4] and a recent multidisciplinary framework states that surgery for older women with breast cancer can be safely delayed because patients can be placed on hormonal therapy [18]. For those patients with hormone receptor positive disease, randomized studies have shown no survival difference between hormone therapy alone versus hormone therapy plus surgery over a limited timeframe [19, 20]. Many recommendation statements issued during the early stages of the pandemic recommended upfront hormonal therapy for early-stage hormone receptor positive patients and consideration of neoadjuvant chemotherapy and/or Her2/neu targeted therapy for hormone receptor negative or HER2neu positive disease [3, 4, 6]. However, it is possible that some physicians may have felt uncomfortable administering systemic therapy given the uncertain mortality risks with infection of SARS CoV-2 and neutropenia due to systemic treatment [8, 9, 21, 22].
Prior to the pandemic, delays in treatment have been reported to impact patient outcomes. It will be many years before we know if delays brought on by the COVID-19 pandemic have impacted survival outcomes of breast cancer patients. Physicians in our study reported a mean delay of two months. In one study, time from diagnosis to first treatment was up to 60 days in 18% of Medicare patients and 24% of patients in the National Cancer Data Base [23]. Time to first treatment also varies by region in the United States and by type of operation [24, 25]. Retrospective studies have shown that delays beyond just 30 days can be associated with incremental decreases in overall survival [26, 27] However, although some aspect of care (such as surgery) was delayed, it is important to remember that many patients in this study were undergoing some type of other treatment such as endocrine therapy.
Interestingly, COVID testing factors impacted physician well-being in an unexpected way. Physicians who tested positive for SARS CoV-2 reported significantly lower anxiety and sleep disturbance than those who tested negative for SARS CoV-2 although the number of physicians who tested positive was low. Perhaps the anticipation of testing positive produces more anxiety and sleep disturbance then actually knowing you are positive. Physicians who tested negative for SARS CoV-2 may not have trusted the test results and would still have to worry about possibly testing positive in the future. There was a lot of uncertainty about testing for COVID-19 at the time of the study. Furthermore, those who were tested for SARS CoV-2 had higher COVID-19 burnout emotions then those who were not tested. This finding may stem from the reason the testing was ordered in the first place such as presence of symptoms, exposure to potential COVID-19 positive patients or having to work in areas of the hospital unfamiliar to breast specialists- all factors that could increase COVID-19 related burnout emotions.
There were several physician-related demographic factors that were independently associated with higher levels of anxiety and COVID-19-related burnout emotions. Compared with older, more experienced physicians and male physicians, female physicians and physicians practicing for shorter periods experienced greater anxiety and burnout emotions. These findings are similar to previous reports of studies suggesting female surgical residents experiencing more burnout then male physicians during their training [28, 29] or during the pandemic [30]. Studies have reported that physicians in their early career are more susceptible to burnout [31] and mid-career physicians often have the highest rates of burnout and emotional exhaustion [32]. Investigators have hypothesized that female physicians suffer more burnout due to more challenging work-life balance issues related to home and childcare responsibilities, as well as harassment and discrimination. While some or all of these factors may have also played a role in the responses from our female physician respondents, deciphering confounding factors in this survey tool is beyond the scope of this study. Nevertheless, our findings are consistent with other studies suggesting that females and less experienced attending physicians reported more burnout rates.
Our study showed a trend toward regional variance in some of the physician well-being outcomes across the country during the study period. Higher physician anxiety and COVID-19 burnout emotions did correlate with regions with higher prevalence rates during the study period. For example, the mid-atlantic region and east north central regions had the highest and second highest rates, respectively, of infection with SARS CoV-2, respectively, during the study period and physician anxiety and COVID-19 burnout scores were highest in these regions. However, sleep disturbance scores fell into higher categories across all regions suggesting that the initial surge of the COVID-19 pandemic had a higher impact on sleep then anxiety for all physicians regardless of location.
Our study is not without limitations. Our data capture one point in time; we have no data on these physician’s anxiety and sleep disturbance prior to the pandemic. Due to the design of our study and time sensitive nature, we are not able to calculate a known response rate. We used social media, email and other networks to quickly recruit breast specialists to report their delays. The majority of respondents were surgeons perhaps because surgeons had to delay many of their patient’s surgeries because of the pandemic. Many respondents had also been in practice for 16 years or longer. Since our findings are subject to selection bias, they are not necessarily generalizable to the entire oncology community who cares for breast cancer patients. While the survey attempted to control for expected increases in anxiety, sleep disturbances, and feelings of burnout from predictable confounding factors such as taking care of COVID + patients, or knowing someone who tested positive for SARS CoV-2 and even important COVID-19 concerns, it is beyond the scope of this survey to be able to account for all such environmental, personal and geographic confounding factors. As such, while our study clearly demonstrates an association between physician self-reported well-being symptoms, the onset of the pandemic and physicians’ perceptions of compromised survival outcomes for their breast cancer patients due to treatment delays, these associations cannot be taken as causal. The COVID-19 pandemic is ongoing, and our survey captures just the beginning of the initial surge of COVID-19 cases in the United States. Since the time of our study, additional knowledge has been gained about how to manage patients infected with SARS CoV-2 and trends in COVID-19 infections are increasing. Physician wellness may be different now compared to the time period of our study.
In conclusion, these findings suggest that physicians taking care of breast cancer patients also experienced compromised well-being despite not having front-line COVID patient care responsibilities. These data can serve as an important guide to those physicians who are currently experiencing the COVID-19 pandemic on a scale similar to the initial surge experienced in the Northeast and other parts of the country. COVID-19 cases continue to increase across the country and more treatment delays may again become a reality for many physicians. Perhaps this study will motivate other hospitals and cancer centers to provide psychosocial support and interventions for physicians that may not have been available during the initial surge of the COVID-19 pandemic. Health systems that deal with these issues directly are the most likely to benefit both in terms of their physician well-being, as well as the safety of their patients.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Holshue ML, DeBolt C, Lindquist S et al (2020) First Case of 2019 Novel Coronavirus in the United States. The New England journal of medicine 382(10):929–936
COVID CDC gov statistics. https://covid.cdc.gov/covid-data-tracker/?utm_source=morning_brew#cases. 2020.
ACS Elective surgery guidelines. https://www.facs.org/covid-19/clinical-guidance/elective-surgery. 2020.
Dietz JR, Moran MS, Isakoff SJ et al (2020) Recommendations for prioritization, treatment, and triage of breast cancer patients during the COVID-19 pandemic. The COVID-19 pandemic breast cancer consortium. Breast Cancer Res Treat 181(3):487–497
ASCO Coronavirus resources. https://www.asco.org/asco-coronavirus-resources/care-individuals-cancer-during-covid-19/disease-specific-information. 2020.
SSO Breast resource during COVID-19 https://www.surgonc.org/wp-content/uploads/2020/03/Breast-Resource-during-COVID-19-3.30.20.pdf. 2020.
Gasparri ML, Gentilini OD, Lueftner D, Kuehn T, Kaidar-Person O, Poortmans P (2020) Changes in breast cancer management during the Corona Virus Disease 19 pandemic: an international survey of the European Breast Cancer Research Association of Surgical Trialists (EUBREAST). Breast 52:110–115
Kuderer NM, Choueiri TK, Shah DP et al (2020) Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet 395(10241):1907–1918
Robilotti EV, Babady NE, Mead PA et al (2020) Determinants of COVID-19 disease severity in patients with cancer. Nat Med 26(8):1218–1223
Lai J, Ma S, Wang Y et al (2020) Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 3(3):e203976
Barello S, Palamenghi L, Graffigna G (2020) Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res 290:113129
Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P (2020) Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun 88:901–907
Shanafelt TD, Balch CM, Bechamps G et al (2010) Burnout and medical errors among American surgeons. Ann Surg 251(6):995–1000
Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D (2008) The Development of Scales for Emotional Distress from the Patient-Reported Outcomes Measurement Information System (PROMIS): Depression, Anxiety, and Anger
Buysse DJ, Yu L, Moul DE et al (2010) Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep 33(6):781–792
PROMIS site health measures. www.healthmeasures.nett/score-and-intrepret/intrepret-scores/promis/promis-score-cut-points. 2020. Accessed Nov 2020.
NCCN guidelines. https://www.nccn.org. 2019.
Freedman RA, Sedrak MS, Bellon JR, et al. (2020) Weathering the storm: managing older adults with breast cancer amid COVID-19 and beyond. J Natl Cancer Instit
Masuda N, Sagara Y, Kinoshita T et al (2012) Neoadjuvant anastrozole versus tamoxifen in patients receiving goserelin for premenopausal breast cancer (STAGE): a double-blind, randomised phase 3 trial. Lancet Oncol 13(4):345–352
Spring LM, Gupta A, Reynolds KL et al (2016) Neoadjuvant endocrine therapy for estrogen receptor-positive breast cancer: a systematic review and meta-analysis. JAMA Oncol 2(11):1477–1486
Desai A, Sachdeva S, Parekh T, Desai R (2020) COVID-19 and cancer: lessons from a pooled meta-analysis. JCO Glob Oncol 6:557–559
Dai M, Liu D, Liu M et al (2020) Patients with cancer appear more vulnerable to SARS-CoV-2: a multicenter study during the COVID-19 outbreak. Cancer Discov 10(6):783–791
Bleicher RJ, Ruth K, Sigurdson ER et al (2012) Preoperative delays in the US Medicare population with breast cancer. J Clin Oncol: Off J Am Soc Clin Oncol 30(36):4485–4492
Bleicher RJ, Chang C, Wang CE et al (2019) Treatment delays from transfers of care and their impact on breast cancer quality measures. Breast Cancer Res Treat 173(3):603–617
Kupstas AR, Hoskin TL, Day CN, Habermann EB, Boughey JC (2019) Effect of Surgery Type on Time to Adjuvant Chemotherapy and Impact of delay on breast cancer survival: a national cancer database analysis. Ann Surg Oncol 26(10):3240–3249
Bleicher RJ, Ruth K, Sigurdson ER et al (2016) Time to surgery and breast cancer survival in the United States. JAMA Oncol 2(3):330–339
Yung R, Ray RM, Roth J et al (2020) The association of delay in curative intent treatment with survival among breast cancer patients: findings from the Women’s Health Initiative. Breast Cancer Res Treat 180(3):747–757
Dahlke AR, Johnson JK, Greenberg CC et al (2018) Gender differences in utilization of duty-hour regulations, aspects of burnout, and psychological well-being among general surgery residents in the United States. Ann Surg 268(2):204–211
Hu YY, Ellis RJ, Hewitt DB et al (2019) Discrimination, abuse, harassment, and burnout in surgical residency training. Engl J Med 381(18):1741–1752
Coleman JR, Abdelsattar JM, Glocker RJ, Force RACT (2020) COVID-19 Pandemic and the Lived Experience of Surgical Residents, Fellows, and Early-Career Surgeons in the American College of Surgeons. J Am College Surg.
Del Carmen MG, Herman J, Rao S et al (2019) Trends and factors associated with physician burnout at a multispecialty academic faculty practice organization. JAMA Netw Open 2(3):e190554
Dyrbye LN, Varkey P, Boone SL, Satele DV, Sloan JA, Shanafelt TD (2013) Physician satisfaction and burnout at different career stages. Mayo Clin Proc 88(12):1358–1367
Funding
There was no funding source for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no disclosures or conflicts to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Yao, K.A., Attai, D., Bleicher, R. et al. Covid-19 related oncologist’s concerns about breast cancer treatment delays and physician well-being (the CROWN study). Breast Cancer Res Treat 186, 625–635 (2021). https://doi.org/10.1007/s10549-021-06101-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-021-06101-1