Abstract
Purpose
Delays in adjuvant breast cancer (BC) therapy have been shown to worsen outcomes. However, thus far studies have only evaluated delays to initial treatment, or a particular modality, such as chemotherapy, leaving uncertainty about the role of delay to subsequent therapy and the effects of cumulative delay, on outcomes. We investigated the associations of delays across treatment modalities with survival.
Methods
We included 3368 women with incident stage I–III BC in the Women’s Health Initiative (WHI) enrolled in fee-for-service Medicare who underwent definitive surgery. This prospective analysis characterized treatment delays by linking WHI study records to Medicare claims. Delays were defined as > 8 weeks to surgery, chemotherapy, and radiation from diagnosis or prior treatment. We used Cox proportional hazards models to estimate BC-specific mortality (BCSM) and all-cause mortality (ACM) in relation to treatment delays.
Results
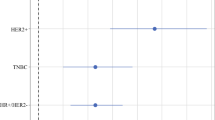
We found 21.8% of women experienced delay to at least one therapy modality. In adjusted analysis, delay to chemotherapy was associated with a higher risk of BCSM (HR = 1.71; 95% CI 1.07–2.75) and ACM (HR = 1.39; 95% CI 1.02–1.90); delay in radiation increased BCSM risk (HR = 1.49; 95% CI 1.00–2.21) but not ACM risk (HR = 1.19; 95% CI 0.99–1.42). Delays across multiple treatment modalities increased BCSM risk threefold (95% CI 1.51–6.12) and ACM risk 2.3-fold (95% CI 1.50–3.50).
Conclusions
A delay to a single treatment modality and delay to a greater extent an accumulation of delays were associated with higher BCSM and ACM after BC. Timely care throughout the continuum of breast cancer treatment is important for optimal outcomes.

Similar content being viewed by others
References
Sealy-Jefferson S, Roseland ME, Cote ML et al (2019) Rural-Urban residence and stage at breast cancer diagnosis among postmenopausal women: the Women's Health Initiative. J Women's Health 28(2):276–283
Bleicher RJ, Ruth K, Sigurdson ER et al (2016) Time to surgery and breast cancer survival in the United States. JAMA Oncol 2(3):330–339
Polverini AC, Nelson RA, Marcinkowski E et al (2016) Time to treatment: measuring quality breast cancer care. Ann Surg Oncol 23(10):3392–3402
Hershman DL, Wang X, McBride R, Jacobson JS, Grann VR, Neugut AI (2006) Delay of adjuvant chemotherapy initiation following breast cancer surgery among elderly women. Breast Cancer Res Treat 99(3):313–321
Zhan QH, Fu JQ, Fu FM, Zhang J, Wang C (2018) Survival and time to initiation of adjuvant chemotherapy among breast cancer patients: a systematic review and meta-analysis. Oncotarget 9(2):2739–2751
Losk K, Vaz-Luis I, Camuso K et al (2016) Factors associated with delays in chemotherapy initiation among patients with breast cancer at a comprehensive cancer center. J Natl Compr Cancer Netw 14(12):1519–1526
Vandergrift JL, Niland JC, Theriault RL et al (2013) Time to adjuvant chemotherapy for breast cancer in National Comprehensive Cancer Network institutions. J Natl Cancer Inst 105(2):104–112
Yu KD, Huang S, Zhang JX, Liu GY, Shao ZM (2013) Association between delayed initiation of adjuvant CMF or anthracycline-based chemotherapy and survival in breast cancer: a systematic review and meta-analysis. BMC cancer. 13:240
Lohrisch C, Paltiel C, Gelmon K et al (2006) Impact on survival of time from definitive surgery to initiation of adjuvant chemotherapy for early-stage breast cancer. J Clin Oncol 24(30):4888–4894
Gagliato Dde M, Gonzalez-Angulo AM, Lei X et al (2014) Clinical impact of delaying initiation of adjuvant chemotherapy in patients with breast cancer. J Clin Oncol 32(8):735–744
Downing A, Twelves C, Forman D, Lawrence G, Gilthorpe MS (2014) Time to begin adjuvant chemotherapy and survival in breast cancer patients: a retrospective observational study using latent class analysis. Breast J 20(1):29–36
Hershman DL, Wang X, McBride R, Jacobson JS, Grann VR, Neugut AI (2006) Delay in initiating adjuvant radiotherapy following breast conservation surgery and its impact on survival. Int J Radiat Oncol Biol Phys 65(5):1353–1360
Gupta S, King WD, Korzeniowski M, Wallace DL, Mackillop WJ (2016) The effect of waiting times for postoperative radiotherapy on outcomes for women receiving partial mastectomy for breast cancer: a systematic review and meta-analysis. Clin Oncol (R Coll Radiol) 28(12):739–749
Punglia RS, Saito AM, Neville BA, Earle CC, Weeks JC (2010) Impact of interval from breast conserving surgery to radiotherapy on local recurrence in older women with breast cancer: retrospective cohort analysis. BMJ 340:845
Zhang WW, Wu SG, Sun JY, Li FY, He ZY (2018) Long-term survival effect of the interval between mastectomy and radiotherapy in locally advanced breast cancer. Cancer Manag Res 10:2047–2054
Chavez-MacGregor M, Clarke CA, Lichtensztajn DY, Giordano SH (2016) Delayed initiation of adjuvant chemotherapy among patients with breast cancer. JAMA Oncol 2(3):322–329
Raphael MJ, Biagi JJ, Kong W, Mates M, Booth CM, Mackillop WJ (2016) The relationship between time to initiation of adjuvant chemotherapy and survival in breast cancer: a systematic review and meta-analysis. Breast Cancer Res Treat 160(1):17–28
American College of Surgeons. CoC quality of care measures. 2019; https://www.facs.org/quality-programs/cancer/ncdb/qualitymeasures. Accessed 12 Nov 2019.
Paskett ED, Caan BJ, Johnson L et al (2018) The Women's Health Initiative (WHI) life and longevity after cancer (LILAC) study: description and baseline characteristics of participants. Cancer Epidemiol Biomarkers Prev 27(2):125–137
Curb JD, McTiernan A, Heckbert SR et al (2003) Outcomes ascertainment and adjudication methods in the Women's Health Initiative. Ann Epidemiol 13(9 Suppl):S122–128
Shin AC, Zheng H, Berthoud HR (2012) Vagal innervation of the hepatic portal vein and liver is not necessary for Roux-en-Y gastric bypass surgery-induced hypophagia, weight loss, and hypermetabolism. Ann Surg 255(2):294–301
Olivotto IA, Lesperance ML, Truong PT et al (2009) Intervals longer than 20 weeks from breast-conserving surgery to radiation therapy are associated with inferior outcome for women with early-stage breast cancer who are not receiving chemotherapy. J Clin Oncol 27(1):16–23
Bellon JR, Come SE, Gelman RS et al (2005) Sequencing of chemotherapy and radiation therapy in early-stage breast cancer: updated results of a prospective randomized trial. J Clin Oncol 23(9):1934–1940
Pinnaro P, Rambone R, Giordano C, Giannarelli D, Strigari L, Arcangeli G (2011) Long-term results of a randomized trial on the sequencing of radiotherapy and chemotherapy in breast cancer. Am J Clin Oncol 34(3):238–244
Toledano A, Azria D, Garaud P et al (2007) Phase III trial of concurrent or sequential adjuvant chemoradiotherapy after conservative surgery for early-stage breast cancer: final results of the ARCOSEIN trial. J Clin Oncol 25(4):405–410
Khanna S, Kim KN, Qureshi MM et al (2017) Impact of patient demographics, tumor characteristics, and treatment type on treatment delay throughout breast cancer care at a diverse academic medical center. Int J Women's Health 9:887–896
Funding
The Women’s Health Initiative (WHI) program is funded by National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts, HHSN268201600018C, HHSN268201600001C, HSN268201600002C, HHSN268201600003C, and HHSN268201600004C. The WHI Life and Longevity after Cancer (LILAC) study was funded by NCI grant UM1 CA173642, and the project to analyze time to treatment was funded by the Seattle Cancer Consortium Support Grant- Safeway Early Career Award awarded to KWR.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author R. Chlebowski has received a speaker honorarium from Novartis and AstraZeneca. Author R. Chlebowski consults for Pfizer, Novartis, AstraZeneca, and Genentech; author J. Roth consults for Bayer, BMS, and Epigenomics Inc. All remaining authors have no conflicts to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent:
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yung, R., Ray, R.M., Roth, J. et al. The association of delay in curative intent treatment with survival among breast cancer patients: findings from the Women’s Health Initiative. Breast Cancer Res Treat 180, 747–757 (2020). https://doi.org/10.1007/s10549-020-05572-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05572-y