Abstract
The objective of this study is to extract pathological brain networks from interictal period of E/MEG recordings to localize epileptic foci for presurgical evaluation. We proposed here a resting state E/MEG analysis framework, to disentangle brain functional networks represented by neural oscillations. By using an Embedded Hidden Markov Model, we constructed a state space for resting state recordings consisting of brain states with different spatiotemporal patterns. Functional connectivity analysis along with graph theory was applied on the extracted brain states to quantify the network features of the extracted brain states, based on which the source location of pathological states is determined. The method is evaluated by computer simulations and our simulation results revealed the proposed framework can extract brain states with high accuracy regarding both spatial and temporal profiles. We further evaluated the framework as compared with intracranial EEG defined seizure onset zone in 10 patients with drug-resistant focal epilepsy who underwent MEG recordings and were seizure free after surgical resection. The real patient data analysis showed very good localization results using the extracted pathological brain states in 6/10 patients, with localization error of about 15 mm as compared to the seizure onset zone. We show that the pathological brain networks can be disentangled from the resting-state electromagnetic recording and could be identified based on the connectivity features. The framework can serve as a useful tool in extracting brain functional networks from noninvasive resting state electromagnetic recordings, and promises to offer an alternative to aid presurgical evaluation guiding intracranial EEG electrodes implantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brain function and dysfunction are encoded in spatiotemporally distributed networks. Functional neuroimaging has evolved from activation imaging, such as functional MRI task-based activation imaging and EEG/MEG (E/MEG) source localization of focal activities, to distributed imaging of brain networks, such as resting state fMRI connectivity imaging (Boerwinkle et al. 2017; Khoo et al. 2017; Lee et al. 2018), and resting state spontaneous mapping and imaging from electrophysiological measurements (Mantini et al. 2007; Canuet et al. 2011; Coito et al. 2016; Case et al. 2018). Recent studies suggest that network analysis of resting state intracranial EEG (iEEG) recordings can allow localization of seizure-onset-zone (SOZ) for up to 88% accuracy and predict seizure outcome (Jiang et al. 2022a). A scientific question of importance to neuroimaging is: can we estimate brain activity and connectivity associated with tasks and behaviors from resting state electrophysiological recordings over the scalp? The answer to this question may have implications to broad neuroimaging of brain function and dysfunction. In particular, this may aid identification and imaging of epileptic networks from brief resting state scalp E/MEG recordings.
Epilepsy is a chronic neurological disorder affecting over 65 million people in the world (Moshé et al. 2015; Thijs et al. 2019). While antiseizure medication (ASMs) serve as the primary treatment, about 30% of the patients do not respond to any combination of multiple ASMs (Palmini et al. 1991; Engel 2008). These patients may benefit from surgical intervention (Rosenow and Lüders 2001; Duncan et al. 2016) or brain stimulation (Ben-Menachem 2002; Vonck et al. 2002) targeting at the epileptogenic zone (EZ) (Rosenow and Lüders 2001). Thus, accurate estimation of the epileptic network and localization of the EZ plays an important role in guiding the resection surgery and in directing brain stimulation.
Clinically, the criteria for defining the EZ are far from being standardized (Stefan et al. 1987; Jehi 2018). In practice, patients go through a comprehensive presurgical evaluation including multiple imaging modalities. Among all functional imaging approaches, the high temporal resolution of E/MEG allows the detection of the brain dynamics more efficiently than other non-invasive imaging techniques (Cohen 1968; Sekihara et al. 2001; Hara et al. 2007; Agirre-Arrizubieta et al. 2009; Dai et al. 2012; Sohrabpour and He 2021). To further improve the spatial resolution of E/MEG and enable exploration of cortical activities, electrophysiological source imaging (ESI) (Brodbeck et al. 2011; Michel and He 2017; He et al. 2018, 2020; Pizzo et al. 2019; Seeber et al. 2019;) is widely used to localize and image the sources of scalp recorded E/MEG signals. The localization accuracy of ESI in presurgical evaluation has been demonstrated by multiple studies (Brodbeck et al. 2011; Kaiboriboon et al. 2012; Beniczky et al. 2016; Jiang et al. 2022b; Sun et al. 2022).
To better estimate the epileptic network, many studies with E/MEG recordings have utilized biomarkers such as seizures or interictal epileptic discharges (IEDs) (Gotman and Gloor 1976; Gotman and Marciani 1985; He et al. 1987; Ding and He 2006; Agirre-Arrizubieta et al. 2009; Yang et al. 2011; de Curtis et al. 2012; Heers et al. 2014, 2016; Chowdhury et al. 2015; Sohrabpour et al. 2016, 2020; Ye et al. 2021; Sun et al. 2022), and high frequency oscillations, to localize the EZ (Lu et al. 2014; Cai et al. 2021). While the convenience of analyzing selected IEDs must be acknowledged, it is also widely known that the selection of IEDs is highly dependent on the readers’ expertise (Kural et al. 2020; Ye et al. 2021), not to mention the extensive human labor involved during this procedure. Co-existing of multiple types of IED also adds to the burden of visual inspection and identification. While direct seizure source localization shows superior accuracy of localizing Seizure Onset Zone (SOZ) (Yang et al. 2011; Lu et al. 2012; Beniczky et al. 2016; Ye et al. 2021), it remains challenging to capture in clinical routine examinations. More approachable and data-driven methodologies that can be integrated into clinical decision-making are still in great need.
Interests in utilizing the resting state have been emerging, whose major advantage is that they can be estimated without the need to wait for a seizure to occur or a concordant IED to be identified (Hsiao et al. 2015; Krishnan et al. 2015). Recent fMRI findings suggested a limited number of large-scale distributed networks of temporally correlated spontaneous activity (Beckmann et al. 2005; Damoiseaux et al. 2006; Smith et al. 2013; Zhang et al. 2015; Boerwinkle et al. 2017), while the task-positive cerebral activities may be highly complicated. In E/MEG signal with high temporal resolution, similar networks have been extracted as transient activations and shown to have distinct band-limited oscillatory power (Baker et al. 2014; Vidaurre et al. 2016). Altered dynamics of these large-scale networks, on the other hand, has been associated with various neurological disorders such as Alzheimer’s disease (Stam et al. 2005; De Haan et al. 2008), Parkinson’s disease (Müller et al. 2001; Cao et al. 2015), chronic pain (Case et al. 2019) and schizophrenia (Lefebvre et al. 2016; Naim-Feil et al. 2018; Kottaram et al. 2019). These types of large-scale network analysis are of greater interest for epilepsy patients due to the relationship between EZ localization and epileptic network estimation, where it is essential to identify and then remove or disconnect certain nodes of the epileptic network. In other words, disentanglement of pathological network for the purpose of source localization is of importance for focal epilepsy patients, and potentially for delineating brain normal function as well as various dysfunctions.
In this context, one natural direction is to consider the E/MEG resting state signal as a finite-state model that can be described in terms of intrinsic spatiotemporal dynamics (Khanna et al. 2015). The method of studying E/MEG resting state recordings, therefore, is by defining the state space based on variables of interest and describing changes in brain activity in terms of state characteristics, such as the duration or frequency of occurrence of specific states. One realization of the method is the so-called “microstates”, where four discrete states are defined by E/MEG topography and remains stable for 80–120 ms before rapidly transitioning to another (Lehmann et al. 1987; Pascual-Marqui et al. 1995; Michel and Koenig 2018). Several studies following this framework have explored the differences between patients with neurological disorders and healthy controls, where significant differences were found in the occurrence of states or the transition matrix (Khanna et al. 2015). While such analysis confirmed the existence of underlying abnormal pattern with or without IED existing (Yuan et al. 2012; Khanna et al. 2015; Ahmadi et al. 2020), abundant spatiotemporal information is missed during the procedure since the signal is filtered into certain frequency bands (alpha, theta, etc.) before being fed into the framework (Lehmann et al. 1987; Michel and Koenig 2018; Poulsen et al. 2018). Moreover, the brain state extraction is based on four topography templates, which makes it challenging to obtain foci-related localization information (Shaw et al. 2019).
Hidden Markov Model (HMM) has been adopted to address the issues and has shown comparable outcome if used in extracting the four aforementioned microstates (Lee and Choi 2003; Eddy 2004; Ossadtchi et al. 2005). In HMM, each state will be characterized with the transition to other states, instead of relying on the topographic templates, thus more refined classification of brain states is achievable (Rabiner and Juang 1986). To further address the spatiotemporal information as missed by static state-space analysis, one way is to explicitly model the spatiotemporal correlation between channels in a time window, which was used in previous studies when a limited number of channels is involved (Sohrabpour et al. 2016; Quinn et al. 2018). Alternatively, a computationally feasible solution is through space embedding (Vidaurre et al. 2016). Embedded Hidden Markov Model (EHMM) has been shown to effectively extract hidden brain states in source-space as applied in event related potential analysis or spontaneous activities in healthy subjects (Jebara et al. 2007; Quinn et al. 2018; Vidaurre et al. 2018). These extracted brain states were compared to functional brain networks from functional MRI (fMRI) or PET studies, showing that spontaneous brain activities are not random but forming highly coherent functional networks, which can be separated with the EHMM framework (Vidaurre et al. 2016).
The existing evidence suggests that the transient neural activity of the brain has quasi-stable properties and could be evaluated with a network view. To further quantify brain dynamics, network analyses from various structural and functional modalities have also emerged aiming at providing a better understanding of network characteristics of the epileptic brain, especially the changes in these characteristics related to surgery outcome. Graph theory has been found useful in seizure detection (Supriya et al. 2023), and found to correlate with the location of the resected cortical regions in patients who were seizure free after surgery (Wilke et al. 2011). Small-worldness was also found to be an important property where brain networks could be distinguished from random networks and was used to differentiate epilepsy patients from controls (Smit et al. 2008; Lithari et al. 2012; Farahani et al. 2019). Several other studies (Elisevich et al. 2011; Coito et al. 2016) have shown disruptions in various network features, and achieved lateralization in temporal lobe epilepsy patients. In this regard, network measures provide a quantitative approach to characterize complex network dynamics and can lead to a better understanding of the epileptic network in addition to providing a valuable diagnostic tool.
In this work, we aim to integrate the strength of brain state space approaches and network analysis based on connectivity, to better disentangle the pathological networks from resting state E/MEG signal, thus, to estimate the EZ. We firstly adopted EHMM as the brain state extraction algorithm and verified its accuracy with computer simulations. We then applied the framework to MEG recordings of ten focal epilepsy patients and analyzed the extracted states with commonly used connectivity metrics to identify the pathological states. By doing so, we observed concordant results between the estimated foci from the proposed resting state analysis approach and the SOZ identified from clinical evaluations, especially in those patients who had abundant IEDs.
Methods
The general analysis framework can be summarized as a two-step strategy as shown in Fig. 1. Firstly, we designed a brain state extraction framework by adapting an Embedded Hidden Markov Model (EHMM) and verified the model using Monte Carlo simulation. Next, the extracted brain states undergo a connectivity analysis to extract the connectivity features and related network attributes. A Graph Feature Index was designed based on the network features, to identify the pathological states among all extracted brain states. The extracted pathological states were compared to the clinical findings to evaluate the performance of the proposed framework.
The overall study pipeline. (i) In step 1, a time window of the original E/MEG data were embedded to create the embedded E/MEG. Independent Component Analysis (ICA) was applied on the data to decompose the data into topographical components and their corresponding activation. The activations were then put through the Hidden Markov Model to estimate the brain states. The estimated states were multiplied by the independent component again to transform back to the original E/MEG space to generate the spatiotemporal brain states. (ii). In step 2, source imaging was applied on the extracted brain states to project sensor space activity to the source space activity. The connectivity features were extracted using Partial Directed Coherence (PDC) and were further used to identify the pathological states. The localization error of the identified pathological states, as compared with intracranial EEG defined seizure onset zone, was used to evaluate the accuracy of the proposed framework
Embedded Hidden Markov Model
In the Hidden Markov Model (HMM), it is assumed that a time series can be described using a hidden sequence of a finite number of states and each state will be characterized with the transition to other states. To facilitate the process, we adapted a well-established Bayesian variational learning algorithm. Assuming state space dimension has the dimension of \(K\), hidden state variables \({\text{s}} = \left\{ {s_{1} \ldots s_{T} } \right\}\), and the observed data is denoted by \({\text{y}} = \left\{ {y_{1} \ldots y_{T} } \right\}\) for the time points \(t_{1} \ldots t_{T}\). The initial state probability is denoted by \({\uppi } = \left\{ {\pi_{1} \ldots \pi_{K} } \right\}\), where \(\pi_{{\text{i}}} = p\left( {s_{1} = q_{{\text{i}}} } \right)\) where variable \(q_{{\text{i}}}\) represents the \({\text{i}}\)th state for i = 1,…,K. Set \(a_{t}\) to be the transition probability where element \(a_{{t,\left( {i,j} \right)}} = p(s_{t + 1} = { }q_{j} |s_{t} = { }q_{i} )\) describes the probability of transitioning from hidden state \(s_{{\text{i}}}\) to \(s_{{\text{j}}}\) from time \(t\) to \(\left( {t + 1} \right)\). Let \(A = \left\{ {A_{1} , \ldots ,A_{{\text{T}}} } \right\}\), where \(A_{{\text{t}}}\) denote the transition probability matrix at time t.
We then set the term \({ }b_{i} \left( {y_{t} } \right) = p\left( {y_{t} {|}s_{t} = q_{{\text{i}}} { },\theta } \right)\) to denote the emission probability distribution. In order to describe the multi-channel E/MEG data, we assume that the emission probability for hidden state as the multivariate Gaussian distribution described by
where \(\theta_{i} = \left\{ {\mu_{i} ,{\Sigma }_{i} } \right\},\) \(\mu_{i}\) being the mean vector, and \({\Sigma }_{i}\) being the covariance matrix. We then denote the parameters as \({\Theta } = \left\{ {\theta_{1} , \ldots ,\theta_{K} } \right\}\).
With all the parameters, the joint distribution \({\text{p}}\left( {{\text{y}},{\text{s}}|{\Theta },A,{ }\pi } \right)\) is then written as
In the basic HMM, the observation \({\text{y}}\) should be the original E/MEG data. This model, on one hand, detects the instantaneous spatial changes and can trace state transitions, but on the other hand, discards rich information of the spectral interactions among the channels (e.g., oscillations leading to repeating patterns, propagation of the oscillations, etc.). EHMM can be applied to capture temporal dynamics of the signal. In this study, we adapted the framework of a time-delay embedded HMM (Vidaurre et al. 2018), where the E/MEG activities over a time window are described using a Gaussian distribution with zero means which is equivalent to using a standard HMM on an embedding transformation of the original data. Many methods can be applied to construct the embedding space of the original data (Seide et al. 2003; Jebara et al. 2007; Vidaurre et al. 2016). Naturally, Independent Component Analysis (ICA) is one of the preferred choices, as the goal of ICA (making the outputs statistically independent being sensitive to higher-order statistics) aligns with the features of data to be extracted, as shown by previous studies (Nam et al. 2002; Seide et al. 2003; Patel et al. 2008; Yuan et al. 2012; Chen et al. 2013; Hsu et al. 2018; Ye et al. 2021).
With ICA as an embedding tool, instead of feeding the entire embedded E/MEG into the HMM model, we firstly performed an ICA decomposition on the embedded E/MEG and the original signal can be written as:
where \({ }IC_{i}\) is the independent components, and \({ }Y_{i} { }\) being the activation for the components. Thus, we transformed the original signal from actual channel space (each value representing the activation amplitude in one E/MEG channel) into the component space (each value representing the activation amplitude for one independent component). Instead of the actual signal, \(Y{ }\) was used as the input to the Hidden Markov Model. After HMM inference, the hidden states are extracted and represented as \(S_{j} { }\), which is a weighting with dimension of \(N\) defined on the component space.
We then multiply \(S_{j}\) to the components as:
to reverse from component space to the actual data space. Eventually, we have the extracted states as transient E/MEG segments representing brain states inferred from the Hidden Markov Model.
Variational Bayes (VB) were used to infer the model parameters, which assumes additional factorizations in the space of parameters and needs all prior distributions to be conjugate (Vidaurre et al. 2016, 2018; Quinn et al. 2018). By using the Expectation–Maximization algorithm acting on one group of parameters at a time, variational Bayes inference minimizes the so-called free energy (Rezek and Roberts 2005).
The code regarding HMM was written in MATLAB 2019b and partial code regarding the free energy evaluation is based on the literatures and toolboxes provided (Rezek and Roberts 2005; Vidaurre et al. 2016, 2018; Quinn et al. 2018).
Simulation Protocol
Monte Carlo simulation with synthesized MEG data was used to verify if the EHMM model can extract states accurately. Synthesized MEG data were generated based on the following assumptions: (i) the brain states can be segmented into a few distinguished states; (ii) the brain states can be characterized as the oscillation with different spectral features and different spatial activations. The procedure for generating simulated MEG signals is depicted in Fig. 2.
Overview of simulation protocol. The chain of brain states was generated based on the state transition matrix and the state spatiotemporal profile. The chain of activation went through forward modeling to generate the synthesized MEG. Different levels of noise were added to the synthesized MEG. The simulated MEG signals were then put into the EHMM framework. The results were compared to the simulation parameters to verify the accuracy of EHMM model
With the aforementioned assumption, we simulated each trial as a MEG segment with a few brain states, and each state was represented by an oscillation. For the spatial profile, Colin Brain template in Brainstorm toolbox was used as the head model (Tadel et al. 2011), and the cortical surface was segmented into 15,002 cortical vertices. For each brain state, we randomly selected one cortical point as the source location. In the cases of multiple sources, the distance between any two sources was set to be larger than 5 cm. For the temporal profile of each state, a frequency value was picked from 2 to 20 Hz to generate the temporal activations.
We first calculated the source level activations. The source level activation was simulated as multiple events where each event is one brain state activated for a certain length of time. To mimic a realistic case where the brain states are transitioning to each other, a Markov Model (Hidden Markov Model with Emission probability as an identity matrix) was used to simulate the time course. A transition matrix was then randomly generated as the probability of one state transitioning to the other one. The initial event was randomly drawn from all states and the following states were generated based on the transition matrix. Note that when one brain state is activated, i.e., when one region on the cortex is activated, the other regions remain silent. For each event, the activation time is randomly selected from 20 to 200 ms to represent the transient brain activities (Vidaurre et al. 2018). For a given length, the activation time course (oscillatory activity) was multiplied by a tapering Tukey window to mimic the state transition edge effect.
After obtaining the source level activation, we performed forward modeling to generate the synthesized E/MEG signal. While this technique is applicable on both EEG and MEG, we used a 102 channel Elekta MEG montage with magnetometers as the sensor configuration. A one-layer boundary element method head model was used to calculate the scalp MEG using the OpenMEEG toolbox (Gramfort et al. 2010) and the leadfield matrix was generated. Note that both three-layer BEM model (scalp, skull, and brain) and one-layer BEM model (brain only) are widely used (Hallez et al. 2007; Gramfort et al. 2010; Tanaka and Stufflebeam 2014). In this study, we adapted one-layer model since the neuromagnetic signals are minimally affected by the tissue conductivity (Hamalainen and Sarvas 1989). A 2-min source activation was multiplied by the leadfield matrix to generate a 2-min MEG signal.
Different scenarios were simulated to evaluate the proposed framework. We varied the number of states from 4 to 7, with 4 being the most commonly used number for many state-space model as mentioned before. Also, Gaussian white noise was added to the generated signal to reach signal-to-noise ratio of 0 dB, 5 dB, and 10 dB to simulate the noise-contaminated MEG signals (Jiang et al. 2022b).
For each condition, 100 trials were simulated. The synthesized MEG recordings were fed into the EHMM framework. To be consistent with the literatures, a 100 ms embedding window was adapted and 50 initializations were used to obtain stable solution through empirical testing. Two types of result were then obtained from the EHMM framework: the spatiotemporal brain states profile represented by brief segments of MEG recordings, and the posterior probability for each of the states. The posterior probability was then put through the Viterbi algorithm (Eddy 2004; Pulford 2006) to get the most probable state activation.
Simulation Evaluation
The result states were firstly compared to the simulated brain states to create 1-on-1 match by ranking the differences between all the pairs. To be more specific, all result brain states were compared to all simulated brain states, and the pair with smallest absolute difference was firstly selected, and the two matched states were removed from the pool. The next pair was then selected from the remaining values until each of the result states was matched to a simulated state. After doing so, for each trial, three evaluation metrics were obtained by comparing estimated states to its matching simulated brain state:
-
(i)
The result states were projected onto the source space using a Linearly Constrained Minimum Variance (LCMV) vector beamformer (Van Veen and Buckley 1988; Woolrich et al. 2011). The Localization Errors (LEs) were calculated as the Euclidian distance from maximum of cortical source activation to the matching simulated brain state source location. LEs were averaged for all the brain states within each trial.
-
(ii)
A fast Fourier transform (FFT) was performed on each extracted state. The frequency with the highest power were extracted for each brain state to represent the temporal profile. The value was then compared to the simulated oscillation frequency for each state and the absolute difference was calculated. The absolute differences between all result states and simulated states were averaged.
-
(iii)
The correlation between result transition matrix and the simulated transition matrix in the 2-min MEG segments were calculated. For any timepoint \(t\), if the current classified state \(s_{t} =\) \(q_{i}\) was different from the state \(s_{{{\text{t}} + 1}} = { }q_{j}\), a transition from state \(q_{{\text{i}}}\) to \(q_{{\text{j}}}\) was counted. We use \(N_{{{\text{i}} \to {\text{j}}}}\) to denote the number of transitions from state \(q_{{\text{i}}}\) to \(q_{{\text{j}}}\), the transition probability matrix \(\overline{A}\) is calculated as \(\overline{a}_{i,j} = { }\frac{{N_{{{\text{i}} \to {\text{j}}}} }}{{\mathop \sum \nolimits_{k = 1}^{K} N_{{{\text{i}} \to {\text{k}}}} }}\).
In this case, we were neglecting the self-transition phenomenon where the brain state remains the same for two consecutive events. A smoothing procedure was introduced to detect the events with long durations and to break these events into smaller events. Note that the simulation transition matrix used to generate the MEG segment is slightly different from the actual simulated transition matrix, since the latter is a realization of the former based on Bayesian model, which could be different from trial to trial. In this simulation, we were comparing the result transition matrix to the latter, and the correlation coefficient (between 0 and 1) was obtained.
Patient Data Acquisition and Preprocessing
The patients included in this study underwent MEG and intracranial EEG (iEEG) monitoring at the University of Pittsburgh Medical Center (UPMC) as a clinical routine. The data analysis study was approved by and performed in accordance with the regulations of the Institutional Review Boards (IRB) of Carnegie Mellon University and University of Pittsburgh.
A total of 10 focal drug-resistant epilepsy patients were included in this study. The patients were selected based on the following criteria: (1) Patients who underwent pre-surgical evaluation, including MEG recordings and MRI; (2) patients who underwent iEEG monitoring and the identified SOZ electrodes were located on the cortical regions (rather than subcortical locations such as amygdala or hippocampus); (3) patients who underwent resective surgery and had a postoperative follow-up of at least 12 months; (4) patients who had Engel I surgical outcome as rated by clinicians.
Each patient underwent a 306-channel recording using the Elekta MEG system (Elekta Neuromag, Helsinki, Finland) with 102 magnetometers and 204 planar gradiometers; a 10-min run with magnetometers only (102 channels) was used in this study. The recorded MEG was band-pass filtered between 1 and 50 Hz. For each patient, an individual cortex surface model, a Desikan-Killiany (DK) atlas (Desikan et al. 2006), and a one-layer boundary element method (BEM) model were constructed from the pre-operational MRI. The sensors were co-registered using anatomical landmarks including Nasion, left pre-auricular point (LPA), right pre-auricular point (RPA), and digitized head points. The lead-field matrix was then calculated using the OpenMEEG (Gramfort et al. 2010) software in MATLAB. The preprocessing steps were all conducted with the Brainstorm software (Tadel et al. 2011).
Brain State Extraction and Source Imaging
For each patient, the resting state data were visually inspected for removal of bad segments and bad channels. EOG and ECG channel was extracted from the original recording to remove EOG and ECG artifact. After that, the 10-min data were segmented into 2-min epochs and fed into the EHMM model to obtain the estimated brain states. For each epoch, two parameters, the 100 ms embedding window and 50 randomized initializations, were adapted from simulation.
After obtaining the states from the EHMM model, the brain states (sensor data) were projected onto the source space using a LCMV vector beamformer carried out separately on each state.
Network Construction and Feature Index
Partial directed coherence (PDC) was used to estimate the directed functional interactions for each brain states. PDC is based on the concept of Granger-causality (Baccalá and Sameshima 2001; He et al. 2019) and is computed using multivariate autoregressive (MVAR) models which simultaneously models multiple time series. To reduce the dimension for MVAR calculation and reduce spatial leakage, after obtaining the LCMV solution, we mapped each individual cortex to the 68-ROI DK brain atlas as described before and averaged the source activation for each region. Thus, we computed PDC using the source activity of the 68 regions. For each state, the connectivity matrix (ROIs × ROIs) represented the flow from one ROI to another, averaged over the frequency range (1–50 Hz).
Graph Feature Index for Brain States
With the PDC connectivity pattern constructed, we selected 20% largest values corresponding to the major information flow in the network and obtained a weighted undirected network \(G = \left( {V,{ }E} \right)\) consisting of a set of vertices \(V\) and a set of edges \(E\) between them. An edge \(c\) connects vertex \(v_{i}\) with vertex \(v_{j}\). In this study, two metrics were used to describe global network properties, namely the average clustering coefficient and the betweenness centrality difference.
Clustering coefficient (CC) is a characteristic parameter to describe local clustering features of a network. The clustering coefficient for a vertex is then given by a proportion of the number of links between the vertices within its neighborhood divided by the number of links that could possibly exist between them. For each node, a high CC value indicates tight connections to the neighboring nodes thus forming a local hub. In a small world network, i.e., the physiological brain network such as resting state networks where most of the nodes connected to their nearest neighbors, but a few of them can spread over a long range, average CC are relatively high. In the pathological network, or the epileptic network, one would assume that only a few nodes occupying the most outflow where most of the other nodes are “muted”, which would lead to a low averaged CC value.
Betweenness centrality (BC), on the other route, is a key metric that is used to identify important actors in a network. It is a graph analysis technique based on shortest path enumeration. This metric is widely used to identify the key nodes in the brain networks (Wilke et al. 2011). We averaged BC value in the left hemisphere and the right hemisphere, and the difference is used to represent the lateralization of the network. Higher difference between the two hemispheres indicates a more lateralized network while a lower difference value indicates a more balanced network. We also observed that betweenness centrality value differences follow a normal distribution, which further verified our assumption.
The two metrics are meant to evaluate the properties of individual brain states. From previous studies as well as experiences, a pathological state is usually corresponding to the abnormal strong cortical activations where one node is driving the other parts of the brain. With this assumption, the qualified pathological state should be corresponding to a smaller averaged clustering coefficient (ACC) value and a larger betweenness centrality difference (BCD) value, which corresponds to a more centralized hub as well as a lateralized driving spot. After empirical investigations, we designed the Graph Feature Index (GFI) as:
where a higher GFI represents higher probability to be a pathological state. The network analysis was performed using NetworkX toolbox implemented Python (Hagberg et al. 2008).
Evaluation Metrics
Seizure onset electrodes identified from iEEG were extracted and marked by experienced epileptologists for each patient. Localization error was defined as the minimum distance between the source location with the maximum activation from the LCMV solution to the closest SOZ electrode, for each extracted state.
For each patient, five 2-min segments were analyzed, and all extracted brain states underwent a hierarchical clustering based on the connectivity patterns. The localization error was averaged within the cluster and the GFI is calculated for each of the grouped states based on the averaged connectivity pattern. The state with the highest GFI was identified as the pathological state for each patient.
Interictal Epileptiform Discharges Analysis
Interictal Epileptiform Discharges (IEDs) were also analyzed to provide a baseline. For each patient, the MEG waveform was visually inspected to identify the IEDs. Two researchers must agree on the identified IEDs, for an identified event to be listed as an IED. While multiple types of IED were found in these patients, only IEDs showed concordant source localization results with the identified SOZ region were included for further analysis, as the purpose of this IED analysis was to provide a benchmark instead of investigating the diversity of IEDs. The IEDs identified were averaged and then fed into source imaging algorithm (LCMV) to obtain the source solution. The localization error was also calculated as the minimum distance between the source location with the maximum activation from the LCMV solution to the closest SOZ electrode.
Results
Simulation Results
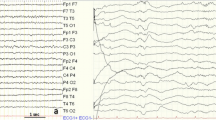
Figure 3A shows an example of one trial with 4 simulated states with 0 dB noise, represented by four different colors. The simulated MEG is overlaid with colors to represent the current simulated brain states. The top row on the right shows scalp topo maps corresponding to 4 simulated states. The EHMM framework successfully extracted the states, represented by the topo maps in sensor space, as shown in the bottom row on the right.
Simulation results. A Example of one trial with 4 simulated states, represented by four different colors. The simulated MEG is overlaid with colors to represent the current simulated brain states. The EHMM framework successfully extracted the states, represented by the topo maps in sensor space. This trial is with 0 dB noise. B Quantitative evaluations. Left panel: Localization error (in mm). The extracted states were projected to the cortex and the source region with maximum activation was compared to the simulated source (dipole model). For each trial, the average localization error was calculated for all the matched state pairs. The black bar indicates standard error. Right top panel: Frequency Difference (in Hz). The maximum frequency for each state was extracted and compared to the simulated frequency. Right bottom panel: transition matrix correlation. The correlation between simulated transition matrix and the result transition matrix was calculated for each trial
Figure 3B shows simulation evaluation results. Under various SNRs (0, 5, 10 dB) and various number of states (N = 4, 5, 6, 7), the EHMM provided robust estimates of source location overall. The localization error increases as the SNR decreases. This indicates that in the simulation setting, SNR could influence the EHMM’s performance largely, but the results remain reasonably stable even with low signal-to-noise ratio of 0 dB. Additionally, the localization errors increase as the number of simulated brain states increases, but generally the localization error is less than or around 10 mm.
From Fig. 3B, it can also be seen that the frequency differences are small. The frequency differences represent the differences between the simulated oscillation and the obtained brain state temporal profile. The difference of approximately 1 Hz indicates that the EHMM framework not only captured the spatial information but also the intrinsic oscillatory power of the brain states. Moreover, one of the features of HMM model over other clustering methods is the ability to accurately capture state transition, and this can be observed from the correlation between simulated transition matrix and the obtained transition matrix.
Patient State Feature Extraction
Figure 4 shows an example in one patient, where a right temporal SOZ was identified. The patient underwent right temporal lobectomy and was seizure-free at 1-year follow up. A segment of MEG time course is shown in Fig. 4B where two extracted states were shown by the pale green boxes. The left-side state is showing a more balanced and spread-out connectivity, while the right-side state is showing a centralized activation from the right posterior temporal region. The representative topo map for the example patient can be found in Fig. 4C, which shows a clear right lateral temporal dipolar source pattern.
Patient Example. A Example of one patient with right temporal epilepsy. Green color shows the resection and each dot represent one intracranial EEG (iEEG) electrode. The red color shows the iEEG defined seizure onset zone. The yellow color shows the seizure spread. B A segment of MEG data and two example brain states. In each of the brain network figure, each grey dot represents the center of one ROI in the DK atlas. The red color edges represent the strongest connection between the ROIs (maximum PDC value). The orange color edges represent the strongest 5 connections. The yellow edges connecting dots represent the strongest 20 connections. The first state lasted longer and showed bilateral, spread-out network with local hubs. The latter state showed lateralized, centralized activation. The connectivity patterns were thresholded differently to better represent the network features. C The topo map of the identified pathological state. The time point with highest global field potential is selected as the localization error is calculated in this time point
In 10 patients studied, we extracted on average 6 different brain states (as shown in Fig. 5A). We then calculated the Averaged Clustering Coefficient and the Betweenness Centrality Difference to get the Graph Feature Index (GFI) for each state. The range of GFI varies from 0 to 0.03. Points with GFI larger than 0.025 forms cluster which exhibited smaller localization error.
Pathological state analysis results. A The number of extracted brain states for all patients. Majority of the patients had 6–7 brain states extracted. B Resting state analysis comparing to the IED analysis, in 6 patients with concordant IED cluster. Red lines indicate worse results while green lines indicate better LE. C Localization error for individual patient, by using the state with highest GFI to represent the pathological state. The colors are corresponding to the colors in B)
Extracted Pathological States vs IED Analysis
If we select the state with largest GFI as the most pathological state, the individual patient outcome was then represented by this selected pathological state. For each state, we selected the time point with the highest energy to extract the source imaging results and compared to the iEEG-defined SOZ.
Figure 5C shows localization error for each of 10 patients studied (LE = 60.0, 11.6, 9.2, 129.9, 119.2, 13.8, 8.4, 23.4, 69.0, and 24.9 mm for patient #1, #2, …, #10, respectively). As shown in Fig. 5C, 6/10 patients (patient #2, #3, #6, #7, #8 and #10) showed localization errors around 10–20 mm. These are considered to be quite positive results given that they are estimated from noninvasive resting state 10 min MEG recordings. In 6/10 patients, we extracted good amount of IEDs (> 5) and conducted the source localization on the averaged extracted IED. In these 6 patients (patient #1, #2, #3, #7, #8, and #10), we compared the results from the extracted pathological state to the IED analysis results and showed comparable results in 5/6 patients (patient #2, #3, #7, #8, and #10) as shown in Fig. 5B. In one patient (patient #6) where no consensus can be reached using IED analysis, the resting state analysis still gave a 13.82 mm result (as shown in Fig. 5C, dark red point). On the other hand, in another patient (patient #1) where IED analysis revealed resonable localization error of 26.9 mm, the resting state analysis had a fairly large localization error of 59.9 mm. Note that in patients #2 and #3, the resting state analysis showed localization results that are closer to the SOZ electrodes than the IED analysis, but in another patient (patient #10), the IED analysis revealed better localization of SOZ than the resting state analysis. These results suggest that the resting state analysis may not always be consistent with the IED analysis in source localization, and further investigation is warranted in a large number of patients for longer duration of resting state data.
Discussion
In this study, we have developed a new framework to analyze the resting state E/MEG recordings for the purpose of identifying and stratifying the underlying brain processes. Our framework includes a two-step strategy. We firstly segmented the E/MEG signal into a few transient spatiotemporal brain states using an embedded Hidden Markov Model. After that, a graph-feature-index combining betweenness centrality difference and the average clustering coefficients is generated to evaluate the likelihood of a brain state to be considered as pathological state or not. We evaluated our proposed framework using computer simulations, and validated our framework in ten focal epilepsy patients who are seizure-free after resective surgery. In these patients, we retrospectively applied the proposed method on a 10-min MEG recording for each patient. The identified pathological state source localization results were compared to the SOZ identified from iEEG recordings. In 6/10 patients, we obtained, from a 10-min resting state noninvasive MEG recordings, concordant results with the iEEG-defined SOZ and obtained average localization error of 15.23 mm. In the subgroup of patients where interictal epileptiform discharges are abundant, the concordance rate is particularly high. It is noteworthy that while the validation was performed on epilepsy patients with MEG recordings, our proposed framework is applicable to both MEG and EEG.
Resting states analysis has been pursued from various angles. Several MEG or EEG analysis methods have been considered for network analysis in patients with neurological disorders (Antonakakis et al. 2016; Rotondi et al. 2016), focusing on connectivity measures such as coherence analysis (Elisevich et al. 2011) and phase lag index analysis (Nissen et al. 2016, 2017) on coarsely-parcellated brain models. Topographical microstate analysis, as described before, is another emerging field, where a few typical patterns in raw E/MEG are extracted and compared to healthy subjects to identify patients from healthy controls (Yuan et al. 2012; Khanna et al. 2015). Although good accuracy can be obtained, especially combined with machine-learning methods (Kr et al. 2018; Ahmadi et al. 2020), the extracted states as well as their transitions are more representative in a group level instead of individual level. While some studies showed good accuracy in identifying epilepsy patients from healthy controls or lateralization in TLE patients (Coito et al. 2016; Nissen et al. 2017; Vollmar et al. 2018), these previous findings heavily rely on the patient groups and the control groups. Moreover, an epileptic seizure onset zone, as needed in the clinical diagnosis for presurgical planning, is still challenging to obtain through the aforementioned studies. A merit of our proposed framework, in this context, is that we can extract the brain states and identify the pathological state for an individual patient without the need to compare with the baseline from a control group. More specifically, the majority of the physiological states in MEG recordings would be the normal “baseline” activity of the brain while the abnormal activations would stand out and be detected through our proposed framework, thus potentially indicating where the epileptogenic tissue is located.
Due to the complex nature of the brain networks especially in epileptic brain, the physiological or the normal brain states and the pathological or the epileptic brain states could be mixed. Our solution to this problem was two-fold. We first followed the state-space model and adapted the EHMM where we make the most use of the high temporal resolution of E/MEG recordings to capture transient spatio-temporal dynamics and verified with simulation. In real patient analysis, even with disentangled brain states, the feature of a so-called “pathological state” is not yet fully understood or fully investigated. The underlying pathology of seizure generation most likely involves both abnormal brain structures and aberrant connections among these regions, leading to skewed large-scale network phenomena (Engel et al. 2013). In this work, we did not exclude the interictal epileptiform discharges from the original recording to create the so-called “spike-free” resting state recording (Grouiller et al. 2011). In practice, interrater reliability is still a challenging issue for correct identification of IEDs (Bagheri et al. 2017; Jing et al. 2020), and multiple types of IEDs co-existing in the interictal data also contribute to the complexity (Ye et al. 2021). Excluding IEDs, on one hand, may demonstrate the power of such analysis, while on the other hand, could be biased towards the IEDs selected to remove. Moreover, since the essence of HMM is dependent on the state transition (Eddy 2004), removal of an important component from the recording could potentially jeopardize the integrity of the algorithm itself. By including entire segments of data, we treat the IED-related network as a part of the brain states and relies on the EHMM to separate the states from others. The abnormality of the IED networks as studied previously (Erem et al. 2015) could then contribute to identify such abnormality from the normal resting state network.
We then focused on application of graph theory, which provides a mathematical framework to characterize different topological properties of a network's organization, and has been applied on various data format to aid the presurgical evaluation or estimation of source regions responsible for neurological disorders (Wilke et al. 2011; Case et al. 2019). We calculated the averaged clustering coefficient to reflect overall properties of the network. A higher ACC is related to a more connected network with tight local connection, which is often seen in many of the large-scale physiological whole-brain networks. Betweenness centrality is computed based on the fraction of all shortest paths in the network that contain a given node. In other words, BC reflects the number of shortest paths from all nodes to all others that have to pass through a specific node. As such, a higher value of BC reflects the hubness of a node as an important, highly integrated influencer in the network. Early work in applying graph theory to epilepsy research indicated the usefulness of BC in characterizing epileptic network (Wilke et al. 2011). We used BC to determine the lateralization of the source, where differences of BC value between the left and right hemisphere were calculated to represent how lateralized the network connection is. It was observed in our data that majority of the extracted brain states show a high ACC value, and the BCD value follows a normal distribution, which aligns with prior whole-brain network studies conducted on healthy patients or epilepsy patients (Baker et al. 2014; García-Prieto et al. 2017; Farahani et al. 2019). An epileptiform-related state, by comparing the topography to the IED, showed a low ACC value and high BCD value (Smit et al. 2008; García-Prieto et al. 2017). One possible explanation is that a pathological state tends to have the focused energy around the SOZ to facilitate the emission of IED or seizures (Bagheri et al. 2017). The connectivity is likely to increase in the SOZ and potentially in regions far from the SOZ, but to decrease for SOZ neighbors, leading to a global reduction of strength, leading to a decreased ACC. Thus, centralized regions tend to strengthen their connections with other hub regions but not so with the rest of the brain, leading to an increased BCD. One thing to note here is that while in some cases, brain networks extracted can be correlated with the healthy brain networks, we do not tend to build the one-on-one bonds, since the epileptic brain could be very different from the normal ones even if we performed a solid segmentation.
With the proposed resting state analysis framework, we were able to achieve a 60% accurate extraction of pathological states with a 15 mm localization error through rigorous comparison to iEEG-defined SOZ, while in some patients the GFI is not giving us the best results. It was also observed that in those patients with inaccurate results, even though we used the state with the highest GFI to represent the putative pathological results, the highest GFI is still much smaller than that in the other patients. Combined with the fact that we were not able to find a concordant IED cluster with a good amount of IEDs in 4/10 patients, this might indicate that the data is not long enough for the proposed framework to separate a valid abnormal pattern, or the pathological states were potentially blurred by the noise due to the non-invasive recordings. While such a caveat is inevitable in data-driven framework, it should be noted that such cases would be challenging for clinicians as well. Moreover, in one patient where standard IED extraction failed to lead to any conclusive results, we extracted a pathological state with good performance (patient #6, dark red in Fig. 5C). In a word, the analysis was performed on a 10-min MEG recording and the pathological states were extracted in a data-driven manner, which could provide an overview of the data for clinical diagnosis and as a potential pre-filtering process to identify states/intervals of interest for the clinical team. The value of the proposed framework is particularly high when longer recordings are available, where manual search is not possible or practical.
Some technical limitations should be addressed in future investigations. While the PDC connectivity and the network features are both widely used in many other literatures, much more potential parameters could be tested to improve the performance of the proposed framework (Mantini et al. 2011; Malinowska et al. 2014; Niso et al. 2015; Molen 2016). For example, in the present study, we used 68-ROIs brain network for the PDC connectivity computation in order to obtain sublobar accuracy suitable for source localization. Such computation based on MVAR model is costly and complex. Future investigation should assess if a fewer number of nodes may be used that would lead to efficient PDC connectivity computation while still reserving spatial resolution needed for source localization. Also, further investigation will be needed if 20% maximal PDC values would be optimal when extracting the pathological states. Several studies have adapted more advanced machine learning algorithms to test for the best combination of parameters (Jin and Chung 2017; Kr et al. 2018; Wu et al. 2020), which should be considered for future studies. We included only patients who had a good surgical outcome or in whom the focus was confidently localized with source imaging on IEDs. Future studies could explore the prediction of different degrees of non–seizure freedom. Along these lines, future studies should also contemplate the changes that occur in different segments of the data, which has been clustered by hierarchical clustering method in this framework due to the short duration of the MEG recording (10 min). In longer recordings where the distribution and the involvement of brain networks could vary and the occurrence of the pathological state could vary (Karoly et al. 2016), a more curated framework with sliding windows could be more informative in evaluating the different stages of the resting state data. Transition matrix, as an important feature of the Hidden Markov Model, was not fully investigated due to the short duration of the data and the relatively small patient population. Future studies could look into mechanisms of the pathological states and interactions with the other brain networks for a further understanding of the epileptogenesis. Despite all these impediments, our results promise an alternative way to identifying and stratifying epileptic networks from noninvasive resting-state recordings.
Conclusion
In summary, we have proposed a data-driven framework to extract pathological state from noninvasive resting state electromagnetic recordings and evaluated the approach in computer simulations and in a group of 10 drug resistant focal epilepsy patients. Our results indicate that the brain networks can be disentangled from the resting-state noninvasive electromagnetic recordings and could be identified based on the connectivity features. The data-drive framework requires minimal human intervention and could potentially guide the intracranial EEG implantation and assisting pre-surgical planning for focal epilepsy patients. Given the generalizability of state space brain network model, the proposed framework may have applications to various neuroscience research and clinical management of a number of brain disorders.
References
Agirre-Arrizubieta Z, Huiskamp GJMM, Ferrier CH, van Huffelen AC, Leijten FSS (2009) Interictal magnetoencephalography and the irritative zone in the electrocorticogram. Brain 132:3060–3071. https://doi.org/10.1093/brain/awp137
Ahmadi N, Pei Y, Carrette E, Aldenkamp AP, Pec henizkip M (2020) EEG-based classification of epilepsy and PNES: EEG microstate and functional brain network features. Brain Inform. https://doi.org/10.1186/s40708-020-00107-z
Antonakakis M, Dimitriadis SI, Zervakis M, Micheloyannis S, Rezaie R, Babajani-Feremi A, Zouridakis G, Papanicolaou AC (2016) Altered cross-frequency coupling in resting-state MEG after mild traumatic. Brain Inj 102:1–11. https://doi.org/10.1016/j.ijpsycho.2016.02.002
Baccalá LA, Sameshima K (2001) Partial directed coherence: a new concept in neural structure determination. Biol Cybern 84:463–474. https://doi.org/10.1007/PL00007990
Bagheri E, Dauwels J, Dean BC, Waters CG, Westover MB, Halford JJ (2017) Interictal epileptiform discharge characteristics underlying expert interrater agreement. Clin Neurophysiol. https://doi.org/10.1016/j.clinph.2017.06.252
Baker AP, Brookes MJ, Rezek IA, Smith SM, Behrens T, Smith PJP, Woolrich M (2014) Fast transient networks in spontaneous human brain activity. eLife. https://doi.org/10.7554/eLife.01867
Beckmann CF, DeLuca M, Devlin JT, Smith SM (2005) Investigations into resting-state connectivity using independent component analysis. Philos Trans R Soc B 360:1001–1013. https://doi.org/10.1098/RSTB.2005.1634
Beniczky S, Rosenzweig I, Scherg M, Jordanov T, Lanfer B, Lantz G, Larsson PG (2016) Ictal EEG source imaging in presurgical evaluation: high agreement between analysis methods. Seizure 43:1–5. https://doi.org/10.1016/j.seizure.2016.09.017
Ben-Menachem E (2002) Vagus-nerve stimulation for the treatment of epilepsy. Lancet Neurol 1:477–482
Boerwinkle V, Mohanty D, Foldes S, Guffey D, Minard CG, Vedantam A, Raskin JS, Lam S, Bond M, Mirea L, Adelson PD, Wilfong AA, Curry DJ (2017) Correlating resting state functional MRI connectivity by independent component analysis-based epileptogenic zones with intracranial EEG localized seizure onset zones and surgical outcomes in prospective pediatric intractable epilepsy study. Brain Connect 7:424–442. https://doi.org/10.1089/brain.2016.0479
Brodbeck V, Spinelli L, Lascano AM, Wissmeier M, Vargas MI, Vulliemoz S, Pollo C, Schaller K, Michel CM, Seeck M (2011) Electroencephalographic source imaging: a prospective study of 152 operated epileptic patients. Brain 134:2887–2897. https://doi.org/10.1093/brain/awr243
Cai Z, Sohrabpour A, Jiang H, Ye S, Joseph B, Brinkmann BH, Worrell GA, He B (2021) Noninvasive high-frequency oscillations riding spikes delineates epileptogenic sources. Proc Natl Acad Sci USA 118(17):e20111301. https://doi.org/10.1073/pnas.2011130118
Canuet L, Ishii R, Pascual-marqui RD, Iwase M, Kurimoto R, Aoki Y, Ikeda S, Takahashi H, Nakahachi T, Takeda M (2011) Resting-state EEG source localization and functional connectivity in schizophrenia-like psychosis of epilepsy. PLoS ONE 6(11):e27863. https://doi.org/10.1371/journal.pone.0027863
Cao C, Li D, Jiang T, Ince NF, Zhan S, Zhang J, Sha Z, Sun B (2015) Resting state cortical oscillations of patients with parkinson disease and with and without subthalamic deep brain stimulation: a magnetoencephalography study. J Clin Neurophysiol 32:109–118. https://doi.org/10.1097/WNP.0000000000000137
Case M, Shirinpour S, Zhang H et al (2018) Increased theta band EEG power in sickle cell disease patients. J Pain Res 11:67–76. https://doi.org/10.2147/JPR.S145581
Case M, Shirinpour S, Vijayakumar V et al (2019) Graph theory analysis reveals how sickle cell disease impacts neural networks of patients with more severe disease. NeuroImage Clin 21:101599. https://doi.org/10.1016/j.nicl.2018.11.009
Chen J, Ros T, Gruzelier JH (2013) Dynamic changes of ICA-derived EEG functional connectivity in the resting state. Hum Brain Mapp 868:852–868. https://doi.org/10.1002/hbm.21475
Chowdhury RA, Zerouali Y, Hedrich T et al (2015) MEG–EEG information fusion and electromagnetic source imaging: from theory to clinical application in epilepsy. Brain Topogr 28:785–812. https://doi.org/10.1007/s10548-015-0437-3
Cohen D (1968) Magnetoencephalography: evidence of magnetic fields produced by alpha-rhythm currents. Science. https://doi.org/10.1126/science.161.3843.784
Coito A, Genetti M, Pittau F, Iannotti GR, Thomschewski A, Holler Y, Trinka E, Wiest R, Seeck M, Michel CM, Plomp G, Vulliemoz S (2016) Altered directed functional connectivity in temporal lobe epilepsy in the absence of interictal spikes: a high density EEG study. Epilepsia 57:402–411. https://doi.org/10.1111/epi.13308
Dai Y, Zhang W, Dickens DL, He B (2012) Source connectivity analysis from MEG and its application to epilepsy source localization. Brain Topogr 25:157–166. https://doi.org/10.1007/s10548-011-0211-0
Damoiseaux JS, Rombouts SARB, Barkhof F, Scheltens P, Stam CJ, Smith SM, Beckmann CF (2006) Consistent resting-state networks across healthy subjects. Proc Natl Acad Sci USA 103:13848–13853. https://doi.org/10.1073/pnas.0601417103
de Curtis M, Jefferys JGR, Avoli M (2012) Interictal Epileptiform discharges in partial epilepsy: complex neurobiological mechanisms based on experimental and clinical evidence. In: Noebels JL, Avoli M, Rogawski MA et al (eds) Jasper’s basic mechanisms of the epilepsies, 4th edn. National Center for Biotechnology Information, Bethesda
De Haan W, Stam CJ, Jones BF, Zuiderwijk IM, van Dijk BW, Scheltens P (2008) Resting-state oscillatory brain dynamics in Alzheimer disease. J Clin Neurophysiol 25:187–193. https://doi.org/10.1097/WNP.0B013E31817DA184
Desikan RS, Ségonne F, Fischl B, Quinn BT, Dickerson BC, Blacker D, Buckerner RL, Dale AM, Maguire RP, Hyman BT, Albert MS, Killiany RJ (2006) An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage 31:968–980. https://doi.org/10.1016/j.neuroimage.2006.01.021
Ding L, He B (2006) Spatio-temporal EEG source localization using a three-dimensional subspace FINE approach in a realistic geometry inhomogeneous head model. IEEE Trans Biomed Eng 53:1732–1739. https://doi.org/10.1109/TBME.2006.878118
Duncan JS, Winston GP, Koepp MJ, Ourselin S (2016) Brain imaging in the assessment for epilepsy surgery. Lancet Neurol 15:420–433. https://doi.org/10.1016/S1474-4422(15)00383-X
Eddy SR (2004) What is a hidden Markov model? Nat Biotechnol 22:1315–1316. https://doi.org/10.1038/nbt1004-1315
Elisevich K, Shukla N, Moran JE, Smith B, Schultz L, Mason K, Barkley GL, Tepley N, Gumenyuk V, Bowyer SM (2011) An assessment of MEG coherence imaging in the study of temporal lobe epilepsy. Epilepsia 52:1110–1119. https://doi.org/10.1111/j.1528-1167.2011.02990.x
Engel J (2008) Surgical treatment for epilepsy: too little, too late? J Am Med Assoc 300:2548–2550
Engel J, Thompson PM, Stern JM et al (2013) Connectomics and epilepsy. Curr Opin Neurol 26:186–194
Erem B, Hyde DE, Peters JM, Duffy FH, Brooks DH, Warfield SK (2015) Combined delay and graph embedding of epileptic discharges in EEG reveals complex and recurrent nonlinear dynamics. In: Proc—Int Symp Biomed Imaging 2015-July, pp 347–350. https://doi.org/10.1109/ISBI.2015.7163884
Farahani FV, Karwowski W, Lighthall NR (2019) Application of graph theory for identifying connectivity patterns in human brain networks: a systematic review. Front Neurosci 13:1–27. https://doi.org/10.3389/fnins.2019.00585
García-Prieto J, Bajo R, Pereda E (2017) Efficient computation of functional brain networks: toward real-time functional connectivity. Front Neuroinform 11:1–18. https://doi.org/10.3389/fninf.2017.00008
Gotman J, Gloor P (1976) Automatic recognition and quantification of interictal epileptic activity in the human scalp EEG. Electroencephalogr Clin Neurophysiol 41:513–529. https://doi.org/10.1016/0013-4694(76)90063-8
Gotman J, Marciani MG (1985) Electroencephalographic spiking activity, drug levels, and seizure occurence in epileptic patients. Ann Neurol 17:597–603. https://doi.org/10.1002/ana.410170612
Gramfort A, Papadopoulo T, Olivi E, Clerc M (2010) OpenMEEG: opensource software for quasistatic bioelectromagnetics. Biomed Eng Online. https://doi.org/10.1186/1475-925X-9-45
Grouiller F, Thornton RC, Groening K, Spinelli L, Duncan JS, Schaller K, Siniatchkin M, Lemieux L, Seeck M, Michel CM, Vulliemoz S (2011) With or without spikes: localization of focal epileptic activity by simultaneous electroencephalography and functional magnetic resonance imaging. Brain 134:2867–2886. https://doi.org/10.1093/brain/awr156
Hagberg AA, Schult DA, Swart PJ (2008) Exploring network structure, dynamics, and function using NetworkX. In: 7th Python in Science Conference (SciPy 2008), pp 11–15
Hallez H, Vanrumste B, Grech R, Muscat J, Clercq WD, Vergult A, D’Asseler Y, Camilleri KP, Fabri SG, Van Huffel S, Lemahieu I (2007) Review on solving the forward problem in EEG source analysis. J NeuroEngineering Rehabil. https://doi.org/10.1186/1743-0003-4-46
Hamalainen MS, Sarvas J (1989) Realistic conductivity geometry model of the human head for interpretation of neuromagnetic data. IEEE Trans Biomed Eng 36:165–171
Hara K, Lin FH, Camposano S, Foxe DM, Grant PE, Bourgeois BF, Ahlfors SP, Stufflebeam SM (2007) Magnetoencephalographic mapping of interictal spike propagation: a technical and clinical report. Am J Neuroradiol 28:1486–1488. https://doi.org/10.3174/ajnr.A0596
He B, Musha T, Okamoto Y, Homma S, Nakajima Y, Sato T (1987) Electric dipole tracing in the brain by means of the boundary element method and its accuracy. Trans Biomed Eng IEEE 6:406–414
He B, Sohrabpour A, Brown E, Liu Z (2018) Electrophysiological source imaging: a noninvasive window to brain dynamics. Annu Rev Biomed Eng 20:171–196. https://doi.org/10.1146/annurev-bioeng-062117-120853
He B, Astolfi L, Valdes-Sosa PA, Marinazzo D, Palva SO, Bener CG, Michel CM, Koenig T (2019) Electrophysiological brain connectivity: theory and implementation. IEEE Trans Biomed Eng 66:2115–2137. https://doi.org/10.1109/TBME.2019.2913928
He B, Ding L, Sohrabpour A (2020) Electrophysiological mapping and source imaging. In: He B (ed) Neural engineering. Springer, Cham, pp 379–413
Heers M, Hedrich T, An D, Dubeau F, Gotman J, Grova C, Kobayashi E (2014) Spatial correlation of hemodynamic changes related to interictal epileptic discharges with electric and magnetic source imaging. Hum Brain Mapp 35:4396–4414. https://doi.org/10.1002/hbm.22482
Heers M, Chowdhury RA, Hedrich T, Dubeau F, Hall JA, Lina JM, Grova C, Kobayashi E (2016) Localization accuracy of distributed inverse solutions for electric and magnetic source imaging of interictal epileptic discharges in patients with focal epilepsy. Brain Topogr 29:162–181. https://doi.org/10.1007/s10548-014-0423-1
Hsiao F, Yu H, Chen W, Kwan S (2015) Increased intrinsic connectivity of the default mode network in temporal lobe epilepsy : evidence from resting-state MEG recordings. 1–18. https://doi.org/10.1371/journal.pone.0128787
Hsu SH, Pion-Tonachini L, Palmer J, Miyakoshi M, Makeig S, Jung TP (2018) Modeling brain dynamic state changes with adaptive mixture independent component analysis. Neuroimage 183:47–61. https://doi.org/10.1016/j.neuroimage.2018.08.001
Jebara T, Song Y, Thadani K (2007) Spectral clustering and embedding with hidden markov models. In: Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics)
Jehi L (2018) The epileptogenic zone: Concept and definition. Epilepsy Curr 18:12–16. https://doi.org/10.5698/1535-7597.18.1.12
Jiang H, Kokkinos V, Ye S, Urban A, Bagic A, Richardson M, He B (2022a) Interictal SEEG resting-state connectivity localizes the seizure onset zone and predicts seizure outcome. Adv Sci. https://doi.org/10.1002/advs.202200887
Jiang X, Ye S, Sohrabpour A, Bagic A, He B (2022b) Imaging the extent and location of spatiotemporally distributed epileptiform sources from MEG measurements. NeuroImage Clin 33:102903. https://doi.org/10.1016/j.nicl.2021.102903
Jin SH, Chung CK (2017) Electrophysiological resting-state biomarker for diagnosing mesial temporal lobe epilepsy with hippocampal sclerosis. Epilepsy Res 129:138–145. https://doi.org/10.1016/j.eplepsyres.2016.11.018
Jing J, Herlopian A, Karakis I et al (2020) Interrater reliability of experts in identifying interictal epileptiform discharges in electroencephalograms. JAMA Neurol. https://doi.org/10.1001/jamaneurol.2019.3531
Kaiboriboon K, Lüders HO, Hamaneh M, Turnbull J, Lhatoo SD (2012) EEG source imaging in epilepsy—practicalities and pitfalls. Nat Rev Neurol 8:498–507. https://doi.org/10.1038/nrneurol.2012.150
Karoly PJ, Freestone DR, Boston R, Grayden DB, Himes D, Leyde K, Seneviratne S, Berkovic S, O’Brien T, Cook MJ (2016) Interictal spikes and epileptic seizures: their relationship and underlying rhythmicity. Brain 139:1066–1078. https://doi.org/10.1093/brain/aww019
Khanna A, Pascual-Leone A, Michel CM, Farzan F (2015) Microstates in resting-state EEG: current status and future directions. Neurosci Biobehav Rev 49:105–113. https://doi.org/10.1016/j.neubiorev.2014.12.010
Khoo HM, Hao Y, von Ellenrieder N, Zazubovits N, Hall J, Olivier A, Dubeau F, Gotman J (2017) The hemodynamic response to interictal epileptic discharges localizes the seizure-onset zone. Epilepsia 58:811–823. https://doi.org/10.1111/epi.13717
Kottaram A, Johnston LA, Cocchi L, Ganella EP, Everall I, Pantelis C, Kotagiri R, Zalesky A (2019) Brain network dynamics in schizophrenia: reduced dynamism of the default mode network. Hum Brain Mapp 40:2212–2228. https://doi.org/10.1002/HBM.24519
Kr V, Rajagopalan SS, Bhardwaj S et al (2018) Machine learning detects EEG microstate alterations in patients living with temporal lobe epilepsy. Seizure 61:8–13. https://doi.org/10.1016/j.seizure.2018.07.007
Krishnan B, Vlachos I, Wang ZI, Mosher J, Najm I, Burgess R, Iasemidis L, Alexopoulos AV (2015) Clinical Neurophysiology Epileptic focus localization based on resting state interictal MEG recordings is feasible irrespective of the presence or absence of spikes. Clin Neurophysiol 126:667–674. https://doi.org/10.1016/j.clinph.2014.07.014
Kural MA, Duez L, Sejer Hansen V, Larsson PG, Rampp S, Schulz R, Tankisi H, Wennberg R, Bibby BM, Scherg M, Beniczky S (2020) Criteria for defining interictal epileptiform discharges in EEG: a clinical validation study. Neurology 94:e2139–e2147. https://doi.org/10.1212/WNL.0000000000009439
Lee H, Choi S (2003) PCA+HMM+SVM for EEG pattern classification. In: Proc—7th Int Symp Signal Process Its Appl ISSPA 2003, vol 1, pp 541–544. https://doi.org/10.1109/ISSPA.2003.1224760
Lee K, Khoo HM, Lina JM, Dubeau F, Gotman J, Grova C (2018) Disruption, emergence and lateralization of brain network hubs in mesial temporal lobe epilepsy. NeuroImage Clin 20:71–84. https://doi.org/10.1016/j.nicl.2018.06.029
Lefebvre S, Demeulemeester M, Leroy A, Delmaire C, Lopes R, Pins D, Thomas P, Jardri R (2016) Network dynamics during the different stages of hallucinations in schizophrenia. Hum Brain Mapp 37:2571–2586. https://doi.org/10.1002/HBM.23197
Lehmann D, Ozaki H, Pal I (1987) EEG alpha map series: brain micro-states by space-oriented adaptive segmentation. Electroencephalogr Clin Neurophysiol 67:271–288. https://doi.org/10.1016/0013-4694(87)90025-3
Lithari C, Klados MA, Papadelis C, Pappas C, Albani M, Bamidis PD (2012) How does the metric choice affect brain functional connectivity networks? Biomed Signal Process Control 7:228–236. https://doi.org/10.1016/j.bspc.2011.05.004
Lu Y, Yang L, Worrell GA, He B (2012) Seizure source imaging by means of FINE spatio-temporal dipole localization and directed transfer function in partial epilepsy patients. Clin Neurophysiol 123:1275–1283. https://doi.org/10.1016/j.clinph.2011.11.007
Lu Y, Worrell GA, Zhang HC, Lin Y, Brinkmann B, Nelson C, He B (2014) Noninvasive imaging of the high frequency brain activity in focal epilepsy patients. IEEE Trans Biomed Eng 61:1660–1667. https://doi.org/10.1109/TBME.2013.2297332
Malinowska U, Badier JM, Gavaret M, Bartolomei F, Chauvel P, Benar CG (2014) Interictal networks in Magnetoencephalography. Hum Brain Mapp 35:2789–2805. https://doi.org/10.1002/hbm.22367
Mantini D, Perrucci MG, Del GC, Romani GL, Corbetta M (2007) Electrophysiological signatures of resting state networks in the human brain. PNAS 104(32):13170–13175. https://doi.org/10.1073/pnas.0700668104
Mantini D, Della Penna S, Marzetti L, de Pasquale F, Pizzella V, Corbetta M, Romani GL (2011) A signal-processing pipeline for magnetoencephalography resting-state networks. Brain Connectivity 1(1):49–59. https://doi.org/10.1089/brain.2011.0001
Michel CM, He B (2017) EEG mapping and source imaging. In: D. S, F. L da S (eds) Niedermeyer’s Electroencephalography: basic principles, clinical applications, and related fields, 7th edn. Wolters Kluwer & Lippincott Williams & Wilkins, Philadelphia, pp 1135–1156
Michel CM, Koenig T (2018) EEG microstates as a tool for studying the temporal dynamics of whole-brain neuronal networks: a review. Neuroimage 180:577–593. https://doi.org/10.1016/j.neuroimage.2017.11.062
Moshé SL, Perucca E, Ryvlin P, Tomson T (2015) Epilepsy: new advances. Lancet 385:884–898. https://doi.org/10.1016/S0140-6736(14)60456-6
Müller V, Lutzenberger W, Pulvermüller F, Mohr B, Birbaumer N (2001) Investigation of brain dynamics in Parkinson’s disease by methods derived from nonlinear dynamics. Exp Brain Res 136:103–110. https://doi.org/10.1007/s002210000638
Naim-Feil J, Rubinson M, Freche D, Grinshpoon A, Peled A, Moses E, Levit-Binnun N (2018) Altered brain network dynamics in schizophrenia: a cognitive electroencephalography study. Biol Psychiatry Cogn Neurosci Neuroimaging 3:88–98. https://doi.org/10.1016/J.BPSC.2017.03.017
Nam H, Yim T-G, Han SK, Oh JB, Lee SK (2002) Independent component analysis of ictal EEG in medial temporal lobe epilepsy. Epilepsia 43:160–164. https://doi.org/10.1046/j.1528-1157.2002.23501.x
Niso G, Carrasco S, Gudín M, Maestu F, del-Pozo F, Pereda E, (2015) What graph theory actually tells us about resting state interictal MEG epileptic activity. NeuroImage Clin 8:503–515. https://doi.org/10.1016/j.nicl.2015.05.008
Nissen IA, van Klink NEC, Zijlmans M, Stam CJ, Hillebrand A (2016) Brain areas with epileptic high frequency oscillations are functionally isolated in MEG virtual electrode networks. Clin Neurophysiol 127:2581–2591. https://doi.org/10.1016/j.clinph.2016.04.013
Nissen IA, Stam CJ, Reijneveld JC, van Straaten ECW, Hendriks EJ, Baayen JC, De Witt Hamer PC, Idema S, Hillebrand A (2017) Identifying the epileptogenic zone in interictal resting-state MEG source-space networks. Epilepsia 58:137–148. https://doi.org/10.1111/epi.13622
Ossadtchi A, Mosher JC, Sutherling WW, Greenblatt RE, Leahy RM (2005) Hidden Markov modelling of spike propagation from interictal MEG data. Phys Med Biol 50:3447–3469. https://doi.org/10.1088/0031-9155/50/14/017
Palmini A, Andermann F, Olivier A, Tampieri D, Robitaille Y, Andermann E, Wright G (1991) Focal neuronal migration disorders and intractable partial epilepsy: a study of 30 patients. Ann Neurol. https://doi.org/10.1002/ana.410300602
Pascual-Marqui RDD, Michel CMM, Lehmann D (1995) Segmentation of brain electrical activity into microstates: model estimation and validation. IEEE Trans Biomed Eng 42:658–665. https://doi.org/10.1109/10.391164
Patel A, Alotaibi F, Blume WT, Mirsattari SM (2008) Independent component analysis of subdurally recorded occipital seizures. Clin Neurophysiol 119:2437–2446. https://doi.org/10.1016/j.clinph.2008.07.276
Pizzo F, Roehri N, Medina Villalon S, Trebuchon A, Chen S, Legarde S, Carron R, Gavaret M, Giusiano B, McGonigal A, Bartolomei F, Badier JM, Benar CG (2019) Deep brain activities can be detected with magnetoencephalography. Nat Commun 10:971. https://doi.org/10.1038/s41467-019-08665-5
Poulsen AT, Pedroni A, Langer N, Hansen LK (2018) Microstate EEGlab toolbox: an introductory guide. bioRxiv 1–30. https://doi.org/10.1101/289850
Pulford G (2006) The Viterbi algorithm. IET Semin Dig 2006:53–65. https://doi.org/10.1049/ic:20060556
Quinn AJ, Vidaurre D, Abeysuriya R, Becker R, Nobert AC, Woolrich MW (2018) Task-evoked dynamic network analysis through Hidden Markov Modeling. Front Neurosci 12:1–17. https://doi.org/10.3389/fnins.2018.00603
Rabiner LR, Juang BH (1986) An introduction to hidden markov models. IEEE ASSP Mag. https://doi.org/10.1109/MASSP.1986.1165342
Rezek I, Roberts S (2005) Ensemble hidden markov models with extended observation densities for biosignal analysis. In: Husmeier D, Dybowski R, Roberts S (eds) Probabilistic modeling in bioinformatics and medical informatics. Springer, London, pp 419–450
Rosenow F, Lüders H (2001) Presurgical evaluation of epilepsy. Brain 124:1683–1700. https://doi.org/10.1093/brain/124.9.1683
Rotondi F, Franceschetti S, Avanzini G, Panzica F (2016) Clinical neurophysiology altered EEG resting-state effective connectivity in drug-naïve childhood absence epilepsy. Clin Neurophysiol 127:1130–1137. https://doi.org/10.1016/j.clinph.2015.09.003
Seeber M, Cantonas L-M, Hoevels M, Sesia T, Visser-Vandewalle V, Michel CM (2019) Subcortical electrophysiological activity is detectable with high-density EEG source imaging. Nat Commun 10:753. https://doi.org/10.1038/s41467-019-08725-w
Seide F, Zhou J-L, Deng L (2003) Coarticulation modeling by embedding a target-directed hidden trajectory model into HMM—MAP decoding and evaluation. In: 2003 IEEE international conference on acoustics, speech, and signal processing, 2003. Proceedings. (ICASSP ’03). p I
Sekihara K, Nagarajan S, Poeppel D, Miyashita Y (2001) Reconstructing spatio-temporal activities of neural sources from magnetoencephalographic data using a vector beamformer. In: 2001 IEEE int conf acoust speech signal process proc Cat No01CH37221, vol 3, pp 2021–2024. https://doi.org/10.1109/ICASSP.2001.941346
Shaw SB, Dhindsa K, Reilly JP, Becker S (2019) Capturing the forest but missing the trees: microstates inadequate for characterizing shorter-scale EEG dynamics. Neural Comput 31:2177–2211. https://doi.org/10.1162/neco_a_01229
Smit DJAA, Stam CJ, Posthuma D, Boomsma DI, de Geus EJC (2008) Heritability of “small-world” networks in the brain: a graph theoretical analysis of resting-state EEG functional connectivity. Hum Brain Mapp 29:1368–1378. https://doi.org/10.1002/hbm.20468
Smith SM, Vidaurre D, Beckmann CF et al (2013) Functional connectomics from resting-state fMRI. Trends Cogn Sci 17:666–682. https://doi.org/10.1016/J.TICS.2013.09.016
Sohrabpour A, He B (2021) Exploring the extent of source imaging: recent advances in noninvasive electromagnetic brain imaging. Curr Opin Biomed Eng 18:100277. https://doi.org/10.1016/j.cobme.2021.100277
Sohrabpour A, Ye S, Worrell GA, Zhang W, He B (2016) Noninvasive electromagnetic source imaging and granger causality analysis: an electrophysiological connectome (eConnectome) approach. IEEE Trans Biomed Eng 63:2474–2487. https://doi.org/10.1109/TBME.2016.2616474
Sohrabpour A, Cai Z, Ye S, Brinkmann B, Worrell GA, He B (2020) Noninvasive electromagnetic source imaging of spatiotemporally distributed epileptogenic brain sources. Nat Commun 11:1946. https://doi.org/10.1038/s41467-020-15781-0
Stam CJ, Montez T, Jones BF, Rombouts SARB (2005) Disturbed fluctuations of resting state EEG synchronization in alzheimer’s disease. Clin Neurophysiol 116:708–715. https://doi.org/10.1016/j.clinph.2004.09.022
Stefan H, Pawlik G, Böcher-Schwarz HG, Biersack HJ, Burr W, Penin H, Heiss WD (1987) Functional and morphological abnormalities in temporal lobe epilepsy: a comparison of interictal and ictal EEG J Neurol CT, MRI, SPECT and PET. J Neurol. https://doi.org/10.1007/BF00314081
Sun R, Sohrabpour A, Worrell GA, He B (2022) Deep neural networks constrained by neural mass models improve electrophysiological source imaging of spatiotemporal brain dynamics. Proc Natl Acad Sci USA 119:e2201128119. https://doi.org/10.1073/pnas.2201128119
Supriya S, Siuly S, Wang H, Zhang Y (2023) Epilepsy detection from EEG using complex network techniques: a review. IEEE Rev Biomed Eng 16:292–306. https://doi.org/10.1109/RBME.2021.3055956
Tadel F, Baillet S, Mosher JC, Pantazis D, Leahy RM (2011) Brainstorm: a user-friendly application for MEG/EEG analysis. Comput Intell Neurosci. https://doi.org/10.1155/2011/879716
Tanaka N, Stufflebeam SM (2014) Clinical application of spatiotemporal distributed source analysis in presurgical evaluation of epilepsy. Front Hum Neurosci 8:1–8. https://doi.org/10.3389/fnhum.2014.00062
Thijs RD, Surges R, O’Brien TJ, Sander JW (2019) Epilepsy in adults. Lancet 393:689–701. https://doi.org/10.1016/S0140-6736(18)32596-0
Van Der Molen MW (2016) Clinical neurophysiology graph analysis of EEG resting state functional networks in dyslexic readers. Clin Neurophysiol 127:3165–3175. https://doi.org/10.1016/j.clinph.2016.06.023
Van Veen BD, Buckley KM (1988) Beamforming: a versatile approach to spatial filtering. IEEE ASSP Mag 5:4–24. https://doi.org/10.1109/53.665
Vidaurre D, Quinn AJ, Baker AP, Dupret D, Tejero-Cantero A, Woolrich MW (2016) Spectrally resolved fast transient brain states in electrophysiological data. Neuroimage 126:81–95. https://doi.org/10.1016/j.neuroimage.2015.11.047
Vidaurre D, Hunt LT, Quinn AJ, Hunt BAE, Brooks MJ, Nobre AC, Woolrich MW (2018) Spontaneous cortical activity transiently organises into frequency specific phase-coupling networks. Nat Commun 9:2987. https://doi.org/10.1038/s41467-018-05316-z
Vollmar C, Stredl I, Heinig M, Noachtar S, Remi J (2018) Unilateral temporal interictal epileptiform discharges correctly predict the epileptogenic zone in lesional temporal lobe epilepsy. Epilepsia 59:1577–1582. https://doi.org/10.1111/epi.14514
Vonck K, Boon P, Achten E, Reuck JD, Caemaert J (2002) Long-term amygdalohippocampal stimulation for refractory temporal lobe epilepsy. Ann Neurol 5:556–565. https://doi.org/10.1002/ana.10323
Wilke C, Worrell G, He B (2011) Graph analysis of epileptogenic networks in human partial epilepsy. Epilepsia 52:84–93. https://doi.org/10.1111/j.1528-1167.2010.02785.x
Woolrich M, Hunt L, Groves A, Barnes G (2011) MEG beamforming using Bayesian PCA for adaptive data covariance matrix regularization. Neuroimage 57:1466–1479. https://doi.org/10.1016/j.neuroimage.2011.04.041
Wu W, Zhang Y, Jiang J et al (2020) An electroencephalographic signature predicts antidepressant response in major depression. Nat Biotechnol 38:439–447. https://doi.org/10.1038/s41587-019-0397-3
Yang L, Wilke C, Brinkmann B, Worrell GA, He B (2011) Dynamic imaging of ictal oscillations using non-invasive high-resolution EEG. Neuroimage 56:1908–1917. https://doi.org/10.1016/j.neuroimage.2011.03.043
Ye S, Yang L, Lu Y, Kucewicz MT, Brinkmann B, Nelson C, Sohrabpour A, Worrell GA, He B (2021) Contribution of ictal source imaging for localizing seizure onset zone in patients with focal epilepsy. Neurology 96:e366–e375. https://doi.org/10.1212/WNL.0000000000011109
Yuan H, Zotev V, Phillips R, Drevets WC, Bodurka J (2012) Spatiotemporal dynamics of the brain at rest—exploring EEG microstates as electrophysiological signatures of BOLD resting state networks. Neuroimage 60:2062–2072. https://doi.org/10.1016/j.neuroimage.2012.02.031
Zhang CH, Lu Y, Brinkmann B, Welker K, Worrell GA, He B (2015) Lateralization and localization of epilepsy related hemodynamic foci using presurgical fMRI. Clin Neurophysiol 126:27–38. https://doi.org/10.1016/j.clinph.2014.04.011
Acknowledgements
This work was supported in part by National Institutes of Health grants NS096761 and NS127849, and by a gift from the Pittsburgh Health Data Alliance. We are grateful to Abbas Sohrabpour, Xiyuan Jiang, Zhengxiang Cai, Rui Sun, Haiteng Jiang, and Jason Yang for useful discussions on data analysis. We thank participating patients and their families whose involvement and sacrifice made this work possible. We also acknowledge selfless dedication and invaluable efforts of the University of Pittsburgh Comprehensive Epilepsy Center (UPCEC) team and particularly the staff of the UPMC Presbyterian University Hospital (PUH) Epilepsy Monitoring Unit (EMU).
Funding
Open Access funding provided by Carnegie Mellon University.
Author information
Authors and Affiliations
Contributions
SY and BH developed the methods, performed data analysis, and wrote the initial draft of manuscript. AB collected and prepared clinical data. All authors contributed to revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no competing interest to disclose.
Additional information
Handling Editor: Laurent Koessler.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ye, S., Bagić, A. & He, B. Disentanglement of Resting State Brain Networks for Localizing Epileptogenic Zone in Focal Epilepsy. Brain Topogr 37, 152–168 (2024). https://doi.org/10.1007/s10548-023-01025-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10548-023-01025-z