Abstract
Young adults with perinatally acquired HIV (PAH) face numerous challenges, including antiretroviral therapy (ART) adherence, managing onward HIV transmission risks and maintaining wellbeing. Sharing one’s HIV status with others (onward HIV disclosure) may assist with these challenges but this is difficult. We developed and tested the feasibility of an intervention to help HIV status sharing decision-making for young adults with PAH. The study used a randomised parallel group feasibility design with 18–25-year-olds in Uganda and 18–29 year-olds in the UK. Participants were randomly assigned to intervention or standard of care (SOC) condition. The intervention consisted of four sessions (3 group, 1 individual) with follow-up support, delivered in person in Uganda and remotely in the UK. Assessments were carried out at: Pre-intervention /baseline; Post-intervention (intervention group only); Six-month follow-up. 142 participants were recruited (94 Uganda, 48 UK; 89 female, 53 male). At six-month follow-up, 92/94 (98%) participants were retained in Uganda, 25/48 (52%) in the UK. Multivariate analysis of combined data from both countries, showed a non-significant effect of intervention condition on HIV disclosure cognitions and affect (p = 0.08) and HIV disclosure intention (p = 0.09). There was a significant intervention effect on well-being (p = 0.005). This study addressed important gaps in understanding acceptable and feasible ways of delivering HIV status sharing support for young people living with PAH across two very different settings. The intervention was acceptable in both countries and feasible in Uganda. In the UK, retention may have been affected by its remote delivery.
Trial registration: ISRCTN Registry, ISRCTN31852047, Registered on 21 January 2019.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Globally, an estimated five million young people (15–25 years) live with HIV, with a significant proportion having acquired HIV perinatally (Perinatally Acquired HIV: PAH) [1]. There are an estimated 170,000 15–24 year olds living with HIV in Uganda [2] (many of whom live PAH) with an HIV prevalence in this age range of 2.9% in females and 0.8% in males [3]. The UK has a small number of people living with PAH [4]. A total of 2,212 children were ever reported to the UK Collaborative HIV Paediatric Study by the end of March 2021 [5]. The majority of the UK cohort is of sub-Saharan African origin, with half born outside the UK [6].
Although young people living with PAH share some similar challenges to those who are behaviourally infected (e.g., adherence to lifelong antiretroviral therapy (ART), potentially compromised health, HIV stigma, risk of onward HIV transmission), other stressors relate specifically to perinatal acquisition. Longstanding HIV infection acquired prior to physiological and immunological development results in chronic clinical complications during childhood that can cause severe morbidity [7]. In addition to dealing with chronic illness and its associated stressors (e.g., hospitalisations, missed school and social opportunities, and pain), young people living with PAH have often experienced multiple caretaking transitions and loss due to parental and/or sibling illness or death. Young adults with PAH have often additionally experienced suboptimal ART regimens, increasing their likelihood of drug resistance [8].
Daily oral ART medication can transform survival for people living with HIV and prevent the risk of onward transmission to partners and infants. However, ART-mediated viral suppression requires daily adherence to medication and is challenging for some. Rates of viral suppression are variable globally in young people living with PAH, with the lowest rates among 13–24-year-olds when compared to younger children or older adults [8]. Only 54.7% of Ugandan 15–24 year olds are virally suppressed, the lowest of any age range [3]. For many young adults, regardless of their HIV status, negotiating their first sexual experiences can be complex, with the importance of condom use varying depending on cultural and religious norms [9, 10]. For young people with PAH, sexual onset will occur alongside knowledge of having a sexually transmittable, stigmatised medical condition and the potential for onward transmission in those not on suppressive ART.
Sharing an HIV-positive status with others (onward HIV disclosure) has the potential to facilitate positive outcomes in the above areas. It is proven that successful viral suppression (< 200 copies HIV RNA/ml) with ART prevents HIV transmission to sexual partners (Undetectable = Untransmittable; U = U) [11, 12]. In situations where viral suppression has not been achieved, however, sharing an HIV-positive status with partners may reduce onward HIV transmission, by fostering communication about safer sex strategies. HIV status sharing may encourage a partner to undergo testing, use prevention strategies such as condoms, pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP), and engage in care/treatment if needed [13].
HIV status sharing has also been shown to have a number of personal benefits [14]. Sharing may help to buffer HIV-related stress and improve wellbeing [15, 16]. Being open about one’s HIV status may facilitate obtaining social support from significant others, which in turn may assist constructive coping, enhance self-esteem and other health-promoting behaviours [16]. Sharing one’s HIV status may also enhance ART adherence, due to greater adherence support from partners, friends or family, and a reduced need to hide medication use in situations where sharing has not occurred [17, 18]. This is important even for young adults who have an undetectable viral load, as they will only remain undetectable if they continue to adhere to ART. Fear of sharing HIV status is commonly cited as a barrier to ART adherence in young people living with PAH [19]. There is also evidence of lower levels of HIV status sharing being associated with poorer engagement with HIV care [20,21,22]. There is no direct evidence of a relationship between HIV disclosure and unprotected sex in those with PAH. There is, however, evidence in other people living with HIV [23, 24]. Lower levels of status sharing, however, has been associated with more partners in a PAH sample [25].
Globally, there are variable rates of self-reported sharing of an HIV-positive status with a partner, ranging from 39 to 97% [26]. These rates appear to be particularly low in young people with PAH. Mugo and colleagues [27] reported that 66% of their sample of youth living with HIV either married or sexually active in Kenya had not shared with their partners. Only 40% of young adults living with PAH in the US reported sharing with all or most of their partners in one study, and 45% reported sharing with no partners when having unprotected sex [13]. There are also low rates of HIV sharing to other (non-partner) members of one’s social network. In a study in Uganda and Kenya only one in five participants aged 13–17 years reported having shared their HIV status with their peers and almost half had told nobody (except health-care providers) about their HIV status [16].
Sharing an HIV status carries a unique challenge for young people with PAH, with concerns about revealing their mother’s and potentially other family members’ HIV status [28]. Negative parental sharing attitudes, including directives to not share, may be internalised [28] with an atmosphere of secrecy and limits to open communication about HIV affecting the young person at home, in their community and in the clinic [29, 30]. The subjective difficulty of sharing one’s HIV status in young people with PAH, particularly in relationships, has been frequently reported, with a fear of rejection, a lack of confidence about sharing (low HIV disclosure self-efficacy), and fear of secondary disclosure from the recipient to others, cited as barriers [28, 31,32,33,34]. There remain important risks of sharing ones’ HIV status, including the threat of rejection, humiliation, stigma and violence [13, 35].
There are fewer reports in the literature relating to facilitators of HIV status sharing. Viljoen et al. [36] reported that trust and intimacy can motivate sharing. HIV status sharing in young people with PAH has been associated with higher levels of HIV disclosure self-efficacy, being older, paternal orphanhood, contributing to family income, regular visits to the HIV clinic, and greater social support through peers [16]. Status sharing has also been associated with females, earlier age of naming (also known as paediatric HIV disclosure, the process of informing children or adolescents of their HIV diagnosis), increased STD knowledge, HIV disclosure intentions, parent–child communication [13] and with lower levels of HIV stigma and depression [27].
Given the potential benefits of sharing ones’ HIV status, there have been efforts to develop multi-session HIV disclosure interventions in other populations of people living with HIV. Serovich and colleagues developed an HIV disclosure intervention for MSM sharing their HIV status with different recipients, for example family members and partners [37,38,39,40]. Across studies, the intervention has not been found to increase HIV disclosure compared to participants in attention control conditions [38,39,40]. The Amagugu intervention aims to assist in maternal HIV disclosure to a child not living with HIV. The intervention is a home-based, lay-counsellor led intervention and has been shown to be effective in increasing mothers’ confidence in their ability to disclose, and increasing disclosure rates compared to baseline rates [41]. The Teach Raising and Communicating with Kids (TRACK) intervention aims to increase mothers living with HIV (MLH) sharing their status with their children. The authors [42] found that participants who took part in the intervention were four times more likely to disclose their status to their children than those in the wait-list control condition.
Aside from stand-alone multicomponent interventions, other approaches to enhancing HIV status sharing have included training community health workers [43], presenting video material [26], support groups, involving peer workers and different methods of partner notification [44]. There are no HIV status sharing interventions specifically designed for young people with PAH, or young people with HIV more generally [45]. However, facilitating onward disclosure has been a small component of multi-component interventions for young people living with HIV [46,47,48,49].
In standard care there is evidence of counselling for adolescents living with HIV stressing the benefits of HV sharing and not acknowledging fears and risks [50]. Consistent with the gaps in the evidence base outlined above, there is a lack of HIV status sharing guidance to support young people with PAH or professionals working with this population [45]. The World Health Organisation (WHO) has called for work in this area, specifying the need for interventions to help adolescent disclosure decision-making, support caregivers and train providers [51]. There is evidence that young people with HIV [52,53,54] and health care workers [55] would like more HIV status sharing support.
We aimed to develop and test the feasibility of a behavioural intervention to empower young adults with perinatally acquired HIV in the UK and Uganda to make decisions about HIV status sharing. The appropriateness of the intervention in high income/low prevalence (e.g., UK) and low income/high prevalence (e.g., Uganda) contexts needs to be assessed, given global evidence of low rates of HIV status sharing. The decision to focus on young adults rather than a younger population was due to higher rates of sexual activity in the former, with potentially more active consideration of sharing than in younger populations, as well as higher mortality and morbidity in this age group [56]. In addition, in this age range, decisions about sharing may be less constrained by one’s family than during earlier adolescence. The novel focus was on sharing with any recipient depending on participant preference. Enhancing sharing with one category of recipient could facilitate sharing with other categories. For example, increased HIV status sharing and communication with friends and family has been shown to be associated with sharing with a partner [13, 33].
We hypothesised that (1) the intervention would be feasible, in relation to recruitment, retention and acceptability (primary study outcome) and (2) participants in the intervention group will have more pro HIV sharing motivation and intention, and higher levels of well-being at follow-up than participants in a standard of care (SOC) group (secondary study outcome).
Methods
Design
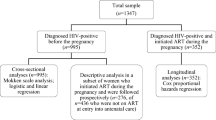
The study used a parallel randomised feasibility design. Participants were randomised to either intervention or SOC condition. Assessments were carried out at pre-intervention/baseline (for both conditions), post-intervention (at the end of the final session, only for the intervention condition), and six-month follow-up (six months from baseline, both conditions). See Fig. 1 for a diagram of the study design.
Setting
The study took place in two countries:
-
1.
UK. Participants were recruited from six inner city NHS clinics providing services for young people living with PAH across three cities, as well as from one UK-based national HIV charity.
-
2.
Uganda. Participants were recruited from a not-for-profit organisation in one city, providing HIV care to young people living with PAH ≥ 18 years.
Inclusion and Exclusion Criteria
Inclusion Criteria
Participants were included if they were aged 18 to 25 years inclusive in Uganda and 18 to 29 years in UK, living with PAH, receiving HIV care at study sites/recruitment sources, and aware of HIV status. The age range was larger in the UK to maximise recruitment.
Exclusion Criteria
Participants were excluded if they had current serious mental health problems, moderate to severe learning disability/executive functioning difficulties, current serious physical health problems with life expectancy < 12 months, unable to understand or communicate in English (UK) or either English or Luganda (Uganda), currently participating in other psychosocial intervention/support research (UK), had participated in the intervention development phase of the study [57], or had another individual in the household who had participated in this phase of the study.
Sample
142 participants were recruited (94 Uganda, 48 UK), a sample size consistent with existing guidance for pilot studies [58]. See Tables 1 and 2 for demographic and clinical characteristics. Enrolment took place between 9th December 2020 and 15th March 2022.
Intervention
The intervention consisted of four-sessions: three group sessions, consisting of a maximum of eight participants, and one individual session. The groups sessions were led by one professional (psychosocial counsellor, clinical nurse specialist, and social worker) and one peer worker. In Uganda the sessions were conducted by bilingual therapists (Luganda and English). Each therapist carried out individual sessions. Therapist training (covering counselling skills, running groups and the intervention) was carried out over eight half days by the first author remotely. The groups were mixed gender. Follow-up support was offered by the peer worker in the six months from baseline to the follow-up data point for both participants and their social network.
The intervention aimed to develop motivation and skills for HIV status sharing, decrease anxiety about HIV sharing and decrease decisional conflict about HIV sharing decision-making. It used a Motivational Interviewing (MI) structure [59]. That is, the first session focused on engaging with participants element before focusing on HIV sharing and evoking motivations to share or not to share in subsequent sessions. The intervention was carried out remotely in the UK due to the COVID-19 pandemic, and in person in Uganda.
The intervention was based on a conceptual model (see Fig. 2), which in turn was based on models of HIV disclosure decision-making and HIV disclosure anxiety [60,61,62,63] and existing evidence of HIV status sharing correlates, barriers and facilitators [13, 16, 64]. In particular, disclosure attitudes, normative beliefs, self-efficacy, planning and support were hypothesised to be important proximal determinants of HIV status sharing. These factors are suggested to be influenced by more distal factors: personal values and HIV stigma.
The components of specific sessions were as follows:
•Session 1—Engaging: ice breaker; intervention aims; ground rules; living with HIV; what do I need to know about HIV to be ready to share?; what is important to me (values clarification exercise)?
•Session 2—Focusing and Evoking: HIV sharing quiz; what reasons are there for not sharing or sharing an HIV status; anxiety about sharing; video—experiences of sharing; personal guidelines about sharing.
•Session 3—Developing HIV Status Sharing Skills: Dramatized video of HIV sharing; If you’ve decided to share to a particular person—where, when and how to share, and what to say; practising sharing; after sharing.
•Session 4—Goal Setting and Planning: Developing a personal sharing plan: assessing goals including reasons for goal and relationship between goal and personal values; developing an action and coping plan. Participants were encouraged to keep a copy of their plan to refer to in the future.
Exercises used role play, modelling, and cognitive restructuring techniques, with both video material and group discussions integrated with interactive exercises. Some components (e.g., values clarification and identifying values-consistent sharing goals) were novel. Each participant was given a workbook to accompany the intervention. The key characteristics of the intervention were adapted for each study context based on earlier formative work, although the core elements of the intervention were the same in each setting. The sessions were one week apart to allow reflection on HIV sharing to take place between sessions. Participants were allowed to move on to the next session if they had missed a previous one.
Intervention Fidelity
All intervention sessions were taped. Ten sessions in each country were reviewed by the one of the research team (after acceptable inter-rater reliability between the research team had been established by jointly rating sessions) for fidelity to the intervention. An intervention checklist and a generic therapy competence tool were used for this task. Feedback was offered to the therapists based on this review, as well as problem-solving supervision. The criteria for acceptable performance were to have been rated as having ‘done well’ on at least three of the following general therapy competencies: Non-verbal communication & active listening; Verbal communication skills; Rapport building & self-disclosure; Exploration, interpretation & normalisation of feelings; Demonstration of empathy, warmth & genuineness, and to have `done’ or `done to some extent’ at least 80% of session activities.
Additional strategies to enhance fidelity included therapist training and the use of an intervention manual (see Supplemental Material 1). In addition, therapists monitored each session that they had facilitated using an intervention session checklist, which was reviewed in supervision. Treatment receipt [65] was assessed in session evaluation and acceptability questionnaires given to participants with questions such as, “How easy was the session to follow?” and “How much effort did it take to participate in the intervention?” with responses recorded on seven-point Likert scales. Treatment enactment [65] was measured in the acceptability questionnaire by asking, “How effective was the intervention in helping you to make decisions about sharing your status?” with responses on a seven-point Likert scale.
Standard of Care Condition
The standard of care condition was routine care. The UK NHS sites, and the Uganda site had dedicated clinics for young people growing up with HIV who have previously been in paediatric care, with peer support and professional psychosocial support available in the Uganda site and in the majority of the UK NHS sites. In these clinics, young people could discuss HIV sharing with their multidisciplinary team, attend with their partner, and have access to a range of other services (e.g., HIV testing, PrEP, family planning, ART adherence support and condom provision). Standard of care in both countries, however, was for there to be no routine or structured psychosocial intervention to facilitate HIV sharing or sharing decision-making. To assess standard of care, participants were asked, “Have you spoken to anyone about sharing your status in the last 6 months?” at the follow-up stage. If yes, they were asked if this was part of their usual care.
Ethics
Ethical approval was granted by a UK NHS research ethics committee and the UK Health Research Authority, and by Royal Holloway University of London Research Ethics Committee. Local approval in the UK was granted by NHS research and development departments. In Uganda, ethical approval was granted by the Joint Clinical Research Centre Ethics Committee and Uganda National Council of Science and Technology. Informed written consent was obtained for all participants.
Measures
Primary Study Outcome
The primary outcome of the study was its feasibility. This was assessed by in relation to recruitment, retention and acceptability. Post intervention acceptability was assessed for participants in the intervention condition by rating 12 items using seven-point Likert scales. An example question was, “How do you feel about the intervention?” A total score was calculated with a range of possible scores of 12 to 84 (α = 0.73). Participants were also asked to rate each session through eight questions (e.g., “How much did you enjoy this session?”) using seven-point Likert scales (α = 0.75). A total score was calculated with higher scores indicating greater levels of acceptability (range of possible scores: 8–56). They were also asked an open question for any comments.
The perceived efficacy of the intervention was assessed for those allocated to the intervention condition in the following way:
-
1.
Participants were asked, “Have you spoken to anyone about sharing your status in the last 6 months?” at the follow-up stage. If yes, they were asked if this was due to taking part in the project.
-
2.
Participants were asked the following questions at the post-intervention point (answered on 7-point Likert scales):
-
a.
How effective was the intervention in helping you to make decisions about sharing your status?
-
b.
How likely is the intervention to be helpful to others in making decisions about sharing their status?
-
c.
How much do you intend to use things that you learned in the intervention in the future?
-
a.
Social harms potentially associated with the intervention were assessed in two main ways:
-
1.
An item on the follow-up demographic questionnaire, “Did anything negative happen as a result of taking part in the project (for example, problems with friends, family, partner; feeling lower)? If yes, please state.”
-
2.
An item on the follow-up disclosure behaviour questionnaire for each disclosure recipient, “How much do you agree with the following statement: Overall they responded positively when they found out that I was HIV positive.” Responses were on a five-point Likert scale from strongly disagree to strongly agree. This question was asked if the participant had shared their status in the last six months.
Secondary Study Outcome Measures
Secondary study outcomes related to whether the aims of the intervention (e.g., increasing HIV disclosure motivation, intention and behaviour) were met. Scales in English were translated into Luganda during the intervention development phase and adapted as necessary [66]. Participants in Luganda were given dual language versions of the measures.
HIV Disclosure Behaviour
HIV disclosure behaviour was assessed through recording (a) the frequency of new disclosure events (first hand or second hand with consent) in the last six months to partners, friends and family, and (b) the proportion of participants’ social network who knew the HIV status of the participant (number of individuals in the social network aware of HIV status divided by the total number in the social network × 100).
Participants were asked to list who was in their social network and then, for each person, were asked a series of questions relating to HIV sharing (e.g., “Do they know that you are HIV positive? How long have they known? Did you tell them yourself?”).
Wellbeing
The 6-item psychological domain from the World Health Organisation Quality of Life brief questionnaire (WHOQOL BREF) [67] was used. This measure has been translated into Luganda with good evidence of reliability and validity [68]. It has also been extensively used with people living with HIV, including young adults with HIV in South Africa [69]. It includes questions on bodily image and appearance, negative feelings, self-esteem, spirituality/religion/personal beliefs, thinking/concentration, and positive feeling, (e.g., “How much do you enjoy life?”) which are answered on 5-point scales (e.g., from 1-not at all to 5-completely) relating to the last four weeks (in this study, α = 0.82 at BL; α = 0.78 at f-up).
Social Support
The 6-item Social Support Questionnaire Short form—SSQ6 [70] was used. For each of the 6 items (e.g., whom can you really count on to help you feel more relaxed when you are under pressure or tense?), respondents indicate the number of people available to provide support and then rate the overall level of satisfaction with the support given in each of the areas from 6-very satisfied to 1-very dissatisfied. Internal consistency in this study was as follows: α = 0.93 at BL; α = 0.90 at f-up. A longer form of this measure has been used with young people living with HIV in Uganda [71].
Hope
The 6-item State Hope Scale was used [72] as a self-report measure of ongoing goal-directed thinking. It includes items such as “There are lots of ways around any problem that I am facing now” and is scored on an 8-point Likert scale from 1 (definitely true) to 8 (definitely false). This measure has been used with young adults in South Africa [73]. In the current study, α = 0.79 at BL; α = 0.79 at f-up.
Decisional Conflict
The 4-item Decisional Conflict Scale was used in relation to decisions to share one’s HIV status with others [74]. The four items are: feeling uncertain (Sure of myself), feeling informed (Understand information), feeling clear about values (Risk–benefit ratio), and feeling supported in decision making (Encouragement). A response of yes scores 1 and a response of no scores 0. Higher total score indicated greater decisional conflict. In this study alpha for the total score was 0.60 at BL and 0.62 at f-up.
HIV Disclosure Cognitions and Affect
The Adolescent HIV Disclosure Cognition and Affect Scale (AHDCAS) [75] was used. This 18-item scale measures negative disclosure attitudes and feelings, positive disclosure attitudes and feelings and disclosure self-efficacy, and has demonstrated good reliability (α = 0.79) and validity in a sample of UK adolescents living with PAH. An example item is “I am confident that I can deal with how others respond if I share my HIV status with them”. Responses are made on a five-point Likert scale from (1) strongly disagree to (5) strongly agree. The minimum score is 18 and the maximum is 90, with higher scores indicating more positive sharing attitudes, feelings about sharing, and sharing self-efficacy. Internal consistency in this study was: α = 0.81 at BL; α = 0.81 at f-up. An additional HIV disclosure intention item, “I intend to tell someone new about my HIV status in the next 6 months”, using the same response options, forms the complete measure. Higher scores indicate greater intention to disclose.
HIV Disclosure Planning Specificity
HIV disclosure planning specificity was assessed by asking the following, relating to action and coping planning: “If you wanted to share your HIV status with someone who did not know your status: (a) How would you do this? (b) How would you respond to what they might say?” Responses were rated on a 0 to 2 scale, with 0 indicating low specificity and 2 indicating high specificity. These questions and the same method of coding responses have been used with adolescents with PAH in the UK [76].
HIV Stigma
The three-item negative self-image subscale from the short form of the HIV stigma scale was used [77]. An example item is “I feel I’m not as good a person as others because I have HIV”, and responses are on a 4-point Likert scale, ranging from strongly disagree (1) to strongly agree (4) (α = 0.74 at BL; α = 0.77 at f-up). The HIV stigma scale has been used extensively, including in young people living with HIV in South Africa [78].
Measurement of Background Variables
Previous HIV Disclosure
Participants were asked about lifetime HIV sharing frequency with the following question – “How many people have you told about your HIV status?”. The following response options were offered: 0, 1, 2, 3, 4–9. 10+.
Demographic and Clinical Variables
Demographic and background variables (current age, ethnic group/tribe, gender, age of paediatric disclosure/naming, parental loss, relationship status, living situation, sexual behaviour, education/occupation) and clinical variables (ART, viral load) were assessed. ART and viral load information was obtained from clinic records.
Procedure
Clinicians or research coordinator approached potentially eligible individuals with study details and took informed consent. After enrolment, stratified block random allocation to condition by country was used, with equal numbers allocated to each condition. Allocation was concealed from the study coordinator in each country. Assessments were conducted remotely via Qualtrics survey software in the UK and mostly in person in Uganda. In Uganda, the measures were administered in a face-to-face group format. Participants read each question and recorded their responses individually. Travel expenses were paid to participants in both the intervention and the SOC conditions. Participants were also reimbursed for completing study measures (UK—£20 at baseline and follow-up, £10 at post-intervention: Uganda—50,000 Shilling at baseline and follow-up, 25,000 Shilling at post-intervention).
Methods used to maximise attendance included communicating about intervention sessions in advance, timetabling sessions at regular times, giving participants the opportunity to meet with a study therapist before the intervention started, offering prompts (Whatsapp and/or phone) and following up when participants did not attend.
Analysis Plan
After descriptive analysis, we conducted multivariate analyses to estimate intervention effects at the six-month data point on three dependent variables: AHDCAS, HIV Disclosure Intention, and WHOQOL-BREF. In all cases we used multilevel (mixed-effects) models to account for the longitudinal design of the study. In the case of HIV Disclosure Intention, the dependent variable consisted of only a single item with five ordered response options. Therefore, we used a multilevel ordinal logistic regression model. The remaining dependent variables were analysed with linear multilevel models, using Satterthwaite approximation to find effective degrees of freedom and compute p-values. In the case of linear models we examined the distribution of residuals to confirm that it did not display obvious deviation from normality. All models, linear or ordinal, had the same random-effects structures, consisting of random, subject-specific intercepts, that accounted for the heterogeneity across individuals in each dependent variable. In all models the main fixed-effects predictors were the intervention condition (intervention vs SOC) and the timepoint (baseline vs follow-up). Additionally, the models included several covariates. For the analyses of the AHDCAS and HIV Disclosure Intention, we included the following covariates: gender, age, country (UK vs Uganda), and lifetime HIV disclosure at baseline (i.e., the total number of people disclosed to). For HIV disclosure intention, we included age of naming. For categorical covariates (gender and country) we used sum contrasts, also known as deviation coding. Continuous covariates (age and lifetime HIV disclosure) were standardized (i.e., centred and scaled by their standard deviation). For analyses with WHOQOL-BREF as the dependent variable we included only gender, age and country as covariates.
The AHDCAS had a large fraction of missing values (31% at baseline and 30% at follow-up) due to participants failing to complete all the scale items. To account for these missing data within our dataset, we conducted an additional imputation analysis using multiple imputation. The results of the models fit on the imputed datasets were consistent with the complete case analyses and revealed the same set of significant predictors (see Supplemental Material 2 for a more detailed report of the imputation analysis).
Results
Primary Study Outcomes
Recruitment and Retention
The initial recruitment target of 94 participants in each country was reduced in the UK due to recruitment difficulties. 142 participants were recruited (94 Uganda, 48 UK; 89 female, 53 male). At six-month follow-up, 92/94 (98%) participants were retained (i.e., completed measures) in Uganda, 25/48 (52%) in the UK. 59/71 (83%) participants were retained from the intervention condition, 58/71 (82%) participants were retained from the SOC condition (See Fig. 3).
Sixty-three participants out of 71 (89%) allocated to the intervention condition attended at least one session. 51/71 (72%) attended all four sessions (and 57/71 (80%) attended either 3 or 4 sessions). The median session length was 112 min (group) and 28 min (individual).
Intervention Acceptability, Use and Perceived Impact
The total score on the intervention acceptability measures (maximum score 84) showed high levels of acceptability in both countries; overall mean 73.18 (sd 6.04); Uganda 73.02 (sd 5.77); UK 73.90 (sd 7.49). The total score on the session evaluation questionnaire (maximum score 56) was also high (i.e., very positive) in both countries: overall median 53 (IQR 49–55); Uganda 52 (IQR 49–55); UK 55 (IQR 52–56).
The sharing recipient identified for the session four goal was partner 29 (50%), friend 14 (24%), family 14 (24%), everyone 1 (2%). Follow-up support was rarely used, with only four participants in Uganda and one participant in the UK contacting the peer worker after the intervention sessions. Thirty eight out of 56 (68%) intervention participants said that they had spoken to someone about HIV sharing in the last six months because of the project. Participants rated the intervention as effective in helping with decisions about sharing (mean 6.29, sd 0.85); likely to be helpful to others (mean 6.23, sd 0.81); and stated that they intended to use the intervention in the future (mean 6.29, sd 0.78).
Nine out of 58 (16%) participants stated that something negative had happened due to taking part in the project. Of these nine, only one indicated a negative impact on their mood. One said that making it to the session was hard. Two said that they were not believed after sharing their status. One said that they were rejected after sharing. Four did not specify the reason for something negative. Eight Uganda participants (5 intervention, 3 SOC) were referred on to other professionals (6 to counsellors, 2 to doctors) over the course of the study. Those referred to doctors has questions regarding their treatment. In relation to assessing HIV disclosure discussions in usual care, 15/54 (28%) in the SOC condition had spoken to a health professional (doctor, nurse, or counsellor) about HIV sharing in the previous 6 months.
Secondary Study Outcomes
Descriptive Analysis
Descriptive scores on measures by condition at different time points are outlined in Table 3.
Several measures showed marked improvements in the intervention group at the end of the intervention, with scores falling back to levels between baseline and post intervention at six-month follow-up (AHDCAS, HIV Disclosure Intention, WHOQOL BREF, HIV Stigma Scale, and the State Hope Scale). The specificity of HIV disclosure plans improved in the intervention condition, and this was maintained at follow up. There was no evidence of greater HIV disclosure planning specificity in the SOC condition.
There was no evidence of a greater frequency of HIV disclosure in those allocated to the intervention condition, although the validity of our disclosure behaviour measure was unclear, and data should be considered with caution. The UK data at baseline and follow-up suggested very small social networks not consistent with the Uganda sample or with a previous UK study where the measure was administered by a researcher [79]. It may be that participants did not continue with the measure given its self-directed and online administration. It also became clear at the data analysis stage that Uganda participants in both conditions at follow-up were not asked about whether they had shared their status with anyone to whom they had not shared their status with at baseline. This error in administration further undermines the credibility of the measure of HIV disclosure behaviour.
Twenty-nine HIV disclosure events in the last six months were reported in the intervention arm at follow-up. In answer to the question, “How much do you agree with the following statement: Overall they responded positively when they found out that I was HIV positive?”, 22/29 (76%) responded agree or strongly agree with only 4/29 (14%) episodes (14%) answered strongly disagree or disagree.
Inferential Analysis
Adolescent HIV Disclosure Cognitions and Affect Scale
The results of this analysis are shown in Table 4. Overall, the only statistically significant predictor of AHDCAS was lifetime HIV disclosure at baseline. Each additional standard deviation in lifetime HIV disclosure at baseline (approximately 1.73 additional people to whom HIV status was disclosed) was associated on average with an increase of 4.59 in the AHDCAS score at both time points. There was a trend for the intervention to be associated with an increase in the ACHDAS score at follow-up relative to the SOC group, β = 4.22, 95% CI [-0.54, 8.97], p = 0.08. A similar pattern was observed when the same analysis was conducted after multiple imputation (see Supplemental Material 2).
HIV Disclosure Intention
The results of this analysis are shown in Table 5. We found a significant effect of lifetime HIV disclosure at baseline, indicating that participants who had disclosed to a larger number of people at baseline were on average also reporting higher HIV disclosure intentions at both time points. Additionally, we found significant effects of country, with Uganda participants reporting higher levels of HIV disclosure intentions than UK participants, and age of naming, with older age of naming associated with higher levels of HIV disclosure intention. There was a trend for the intervention to be associated with an increase in HIV disclosure intentions at follow-up relative to the SOC group, β = 0.95, 95% CI [-0.13, 2.04], p = 0.09.
WHOQOL-BREF
The analysis of the WHOQOL-BREF (Table 6) revealed several significant effects.
Firstly, we found a significant main effect of country, indicating higher well-being in Uganda compared to UK. Secondly, we found a significant main effect of Time with a negative coefficient, indicating that participants in the SOC condition reported lower wellbeing at the follow-up time point. We also found a significant and positive interaction coefficient (time × condition), β = 2.22, 95% CI [0.69, 3.76], p = 0.005 (See Fig. 4).
This suggested that the intervention mitigated the decrease in well-being, and possibly even increased it. To assess whether the intervention increased wellbeing in the intervention group relative to baseline, we re-ran the analysis by flipping the dummy variable coding for intervention and control groups. This analysis revealed that wellbeing in the intervention group was significantly increased with respect to baseline: β = 1.16, 95% CI [0.05, 2.27], t(102.42) = 2.07, p = 0.04. Thus, overall, this analysis revealed that whereas the SOC group reported a decrease in wellbeing at follow-up, the intervention group reported increased levels of wellbeing.
Discussion
Young people with PAH face challenges to wellbeing, managing the risk of onward HIV transmission and adhering consistently to ART medication. The sharing of one’s HIV status may assist in coping with these challenges and, therefore, supporting young people with PAH with their decisions to share their status should be a priority. The HEADS-UP study is the first study to focus on an intervention for HIV sharing among young adults living with PAH. The study was unique in its inclusion of young people from both high income/low prevalence and low income/high prevalence contexts.
The study was feasible in Uganda with excellent recruitment and retention. High rates of retention have been seen in other longitudinal HIV studies in Uganda [80]. Recruitment and retention were more challenging in the UK. Several UK participants allocated to the intervention condition failed to attend a single session. The difference between the countries may have been due to a variety of factors. Recruitment and retention in the UK appeared to be significantly impacted by the COVID-19 pandemic, which resulted in very limited in-person recruitment (at only one site) and the intervention being delivered remotely. The level of reimbursement could have been more motivating in Uganda than in the UK [81]. Finally, cultural differences may have been important. For example, family members appeared to be more involved in recruitment and in supporting retention in Uganda. There was no evidence of different levels of HIV stigma between UK and Uganda participants.
The intervention was highly acceptable and was perceived to be helpful. Participants identified a range of sharing recipients, consistent with the aim of the intervention. There was minimal evidence of social harms associated with the intervention or with HIV sharing that occurred during the study, although these outcomes did occur. This is to be expected given the inherent difficulty in reflecting on HIV sharing and the risks associated with this behaviour. Nevertheless, sharing that occurred over the course of the study was generally appraised positively by participants.
Unexpectedly, the follow-up support offered was rarely used. This may have been due to this being left to the participants to initiate. It may have been helpful to have provided a specific follow-up individual or group session. The SOC participants rarely discussed HIV sharing in their usual care, which suggests that the intervention is not mirroring already occurring conversations with professionals.
There was tentative evidence that the intervention achieved its aims, from both multivariate (wellbeing, HIV sharing motivation and intention) and descriptive (HIV stigma, hope, HIV disclosure planning specificity) analyses. There was no evidence, however, of an effect of the intervention on HIV disclosure behaviour. This may be explained by the short duration of follow-up (6 months), the rarity of HIV sharing and the fact that we did not select participants due to the availability of a potential sharing recipient (e.g., only including participants with a partner who had not been disclosed to). The latter decision may have reduced the opportunity to detect increases in HIV disclosure. In addition, the measure of HIV disclosure behaviour was of questionable validity. The lack of an effect on HIV disclosure was consistent with some intervention studies [39] but not others [43]. The differences between studies may be due to differences in baseline HIV disclosure motivation, comparison groups, the availability of a potential sharing recipient, and the impact of increasing awareness of U = U resulting in participants feeling that they did not need to share with partners.
There was some evidence of an effect of the intervention on HIV sharing motivation and intention, consistent with a UK camp evaluation of adolescents living with PAH [82]. There was also tentative evidence of an effect on HIV disclosure planning specificity, a construct that has not been assessed in other disclosure interventions. There was no evidence of an effect on disclosure decisional conflict, although the reliability of the DCS was poor. There was a significant effect of the intervention on wellbeing, despite this not being the main aim of the intervention. It is notable that motivational interviewing studies have shown similar findings in relation to psychological outcomes even when the focus is on behaviour change [83]. Aside from the multivariate analysis, the fact that in the intervention group improvements in wellbeing were particularly marked at the post-intervention point, and then waned, suggests an intervention effect. Previous HIV disclosure was related to both disclosure motivation and intention at follow-up. Past disclosure has been to shown to relate to disclosure motivation in other studies [75]. This suggests that past disclosure may have gone well, consistent with the generally positive appraisal of sharing that occurred over the course of the study.
It is difficult to assess the generalisabilty of our findings, particularly given the higher rate of viral suppression than expected [8] and the existence of specialist transition clinics at the recruitment sites. Future studies in sub-Saharan Africa could recruit from district level facilities across different regions. Other factors that complicate interpretation of our findings include the impact of the COVID-19 pandemic, differences in HIV prevalence between countries, different standards of care across sites, and therapist characteristics.
Strengths of the study include the range of outcome variables assessed with good evidence of reliability and validity for most measures (including those that we translated and adapted for use in Uganda). We also made considerable efforts to monitor intervention fidelity. Strengths of the intervention include our efforts to create a programme that was relevant to each study context and allowing participants to choose the type of disclosure recipient that they wanted to develop a plan for. The intervention did not depend on recruiting therapists who were trained mental health professionals, which would have limited its potential for future implementation. In fact, it may have been that the involvement of peer workers, in particular, was crucial to its success.
Limitations of the study include the fact that the comparison condition was not attention matched. In addition, there was no assessment of therapist competence at the end of their training [84]. Attempts to establish the study response rate were not successful with unreliable records of who was approached and refused to participate. It would have been useful to have measured HIV knowledge as there was a specific exercise in session one that aimed to increase confidence in participants’ knowledge about HIV (to assist in HIV sharing). Limitations of the intervention include the need to wait until enough people had enrolled to run therapy groups. Supervision was limited by this being conducted online and, in the case of the Ugandan therapists, not in their first language. In addition, supervision was largely conducted in pairs or with all four therapists together, rather than being individual. Individual supervision may have enabled a safer space for peer workers, in particular, to explore the personal impact of conducting the intervention and providing appropriate support. Regarding the intervention itself, more focus may have been helpful on reflecting on family attitudes to sharing, providing example sharing statements, and outlining external support options, including mental health support. Finally, there were unanswered questions about whether it was appropriate or helpful to include participants with mild learning disabilities.
Future studies could include an adequately powered RCT of the intervention, perhaps comparing the four-session intervention with a single session intervention modelled on session four, along with a cost-effectiveness analysis. A larger sample size would allow for analysis of mediating mechanisms to be undertaken, as well as sub-group analysis (e.g., comparing intervention effects by country). Longer follow-up periods could be used, given the low frequency of HIV sharing. The use of an active comparison group, to control for non-specific therapy factors, would strengthen the design of the study. Future research could develop and test the intervention with younger people with PAH, perhaps soon after HIV naming. In addition, further consideration should be given for how to involve parents and siblings. Many issues associated with sharing an HIV status are similar regardless of the population. Adapting the HEADS-UP intervention for other populations of people living with HIV could, therefore, be undertaken.
The clinical significance of potential intervention effects (e.g., on wellbeing, HIV sharing motivation and intention) is not known. However, the acceptable nature of the intervention, the low frequency of routine discussions about HIV sharing in usual care, and the potential benefits of HIV status sharing suggest that the study might be clinically important. Aside from its efficacy, though, consideration should be given to whether the intervention is implementable. When designing the intervention, we decided that four sessions was the shortest number of sessions to explore the inherent ambivalence associated with HIV sharing in way that was supportive. We continue to believe this is the case, although it may be that the final session can be used as a stand-alone intervention if someone is ready to share. This session took less time to deliver than anticipated.
Regardless of whether the HEADS-UP intervention is delivered in full or in part in routine care, the study suggests that clinics could do more to facilitate discussions about HIV sharing. It may be that developing guidelines and toolkits based on the HEADS-UP and similar interventions would be helpful in this regard. Other suggestions include identifying a professional within each clinic to support HIV sharing, routinely asking patients to identify a person whom they might consider sharing their status with and encouraging the identification of a personal sharing buddy; a person from the individual’s social network who can support decisions to share. The waning of effects between post-intervention and follow-up also suggests that such minimal interventions in routine care might be helpful to maintain the effects of the intervention.
Different ways of delivering the intervention should be considered. We are currently developing and testing a digital, modular, individualised version of the intervention for adults of sub-Saharan African ethnicity living with HIV in the UK. If the group format is retained, one way to reach sufficient people is to carry out the intervention remotely, across countries or even regions. Our study, however, suggests caution given the poor retention in the UK with the remotely delivered intervention. Other options may involve grouping sessions together or tying in sessions with other appointments. The training of therapists (delivered online) was lengthy and considerable ongoing supervision was offered to ensure fidelity to the intervention. This is unlikely to be possible in routine practice. Different ways of delivering training should be considered, for example, online group training and supervision, self-directed and video-supported training. Carrying out the intervention with just peer therapists may be feasible, including young people who have undertaken the programme. This may reduce the training burden. Peer support for HIV sharing has been suggested by young adults living with PAH in a recent study [85].
Availability of Data and Material
Anonymised electronic data from the study is available on the Figshare data repository, freely accessible under Creative Commons CC BY licence.
Change history
20 May 2024
A Correction to this paper has been published: https://doi.org/10.1007/s10461-024-04367-2
References
WHO. Maternal, newborn, child and adolescent health 2020. https://www.who.int/maternal_child_adolescent/topics/adolescence/hiv/en/.
Commission UA. Uganda HIV & AIDS Factsheet. 2022.
UPHIA. Uganda population-based HIV impact assessment. 2022.
Collins IJ, Foster C, Tostevin A, Tookey P, Riordan A, Dunn D, et al. Clinical status of adolescents with perinatal HIV at transfer to adult care in the UK/Ireland. Clin Infect Dis. 2017;64(8):1105–12.
CHIPS. Summary Data 2023. http://www.chipscohort.ac.uk/patients/summary-data/#_ftn1.
Judd A, Davies MA. Adolescent transition among young people with perinatal HIV in high-income and low-income settings. Curr Opin Hiv Aids. 2018;13(3):236–48.
Lowenthal ED, Bakeera-Kitaka S, Marukutira T, Chapman J, Goldrath K, Ferrand RA. Perinatally acquired HIV infection in adolescents from sub-Saharan Africa: a review of emerging challenges. Lancet Infect Dis. 2014;14(7):627–39.
Patel K, Seage GR 3rd, Burchett SK, Hazra R, Van Dyke RB, Pediatric HIVACS. Disparities in HIV viral suppression among adolescents and young adults by perinatal infection. Am J Public Health. 2019;109(7):9.
Mileti FP, Mellini L, Sulstarova B, Villani M, Singy P. Exploring barriers to consistent condom use among sub-Saharan African young immigrants in Switzerland. AIDS Care. 2019;31(1):113–6.
Blackstone SR, Nwaozuru U, Iwelunmor J. Factors influencing contraceptive use in Sub-Saharan Africa: a systematic review. Int Q Community Health Educ. 2017;37(2):79–91.
Rodger AJ, Cambiano V, Bruun T, Vernazza P, Collins S, van Lunzen J, et al. Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. JAMA. 2016;316(2):171–81.
Rodger AJ, Cambiano V, Bruun T, Vernazza P, Collins S, Degen O, et al. Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study. Lancet. 2019;393(10189):2428–38.
Weintraub A, Mellins CA, Warne P, Dolezal C, Elkington K, Bucek A, et al. Patterns and correlates of serostatus disclosure to sexual partners by perinatally-infected adolescents and young adults. AIDS Behav. 2017;21(1):129–40.
Whembolua GL, Conserve DF, Thomas K, Handler L. A systematic review of HIV serostatus disclosure among African immigrants in Europe. J Immigr Minor Health Center Minor Public Health. 2016;19:947–58.
Brown MJ, Serovich JM, Laschober TC, Kimberly JA, Lescano CM. Mediating effects of depressive symptoms on perceived social support and HIV disclosure: assessing moderation by sex. AIDS Behav. 2019;23(3):636–48.
Nostlinger C, Bakeera-Kitaka S, Buyze J, Loos J, Buve A. Factors influencing social self-disclosure among adolescents living with HIV in Eastern Africa. AIDS Care. 2015;27(Suppl 1):36–46.
Mi T, Li X, Zhou G, Qiao S, Shen Z, Zhou Y. HIV disclosure to family members and medication adherence: role of social support and self-efficacy. AIDS Behav. 2020;24(1):45–54.
Dessie G, Wagnew F, Mulugeta H, Amare D, Jara D, Leshargie CT, et al. The effect of disclosure on adherence to antiretroviral therapy among adults living with HIV in Ethiopia: a systematic review and meta-analysis. BMC Infect Dis. 2019;19(1):528.
Buchanan AL, Montepiedra G, Sirois PA, Kammerer B, Garvie PA, Storm DS, et al. Barriers to medication adherence in HIV-infected children and youth based on self- and caregiver report. Pediatrics. 2012;129(5):e1244–51.
Ojwang VO, Penner J, Blat C, Agot K, Bukusi EA, Cohen CR. Loss to follow-up among youth accessing outpatient HIV care and treatment services in Kisumu. Kenya AIDS care. 2016;28(4):500–7.
Watson-Jones D, Balira R, Ross DA, Weiss HA, Mabey D. Missed opportunities: poor linkage into ongoing care for HIV-positive pregnant women in Mwanza, Tanzania. PLoS ONE. 2012;7(7):e40091.
Izudi J, Okoboi S, Lwevola P, Kadengye D, Bajunirwe F. Effect of disclosure of HIV status on patient representation and adherence to clinic visits in eastern Uganda: a propensity-score matched analysis. PLoS ONE. 2021;16(10):e0258745.
Hightow-Weidman LB, Phillips G 2nd, Outlaw AY, Wohl AR, Fields S, Hildalgo J, et al. Patterns of HIV disclosure and condom use among HIV-infected young racial/ethnic minority men who have sex with men. AIDS Behav. 2013;17(1):360–8.
Okorie CN, Gutin SA, Getahun M, Lebu SA, Okiring J, Neilands TB, et al. Sex specific differences in HIV status disclosure and care engagement among people living with HIV in rural communities in Kenya and Uganda. PLOS Glob Public Health. 2023;3(4):e0000556.
Dempsey AG, MacDonell KE, Naar-King S, Lau CY, Adolescent Medicine Trials Network for HIVAI. Patterns of disclosure among youth who are HIV-positive: a multisite study. J Adolesc Health. 2012;50(3):315–7.
Conserve DF, Groves AK, Maman S. Effectiveness of interventions promoting HIV serostatus disclosure to sexual partners: a systematic review. AIDS Behav. 2015;19(10):1763–72.
Mugo C, Seeh D, Guthrie B, Moreno M, Kumar M, John-Stewart G, et al. Association of experienced and internalized stigma with self-disclosure of HIV status by youth living with HIV. AIDS Behav. 2021;25(7):2084–93.
Hogwood J, Campbell T, Butler S. I wish I could tell you but I can’t: adolescents with perinatally acquired HIV and their dilemmas around self-disclosure. Clin Child Psychol Psychiatry. 2013;18(1):44–60.
Kajubi P, Bagger S, Katahoire AR, Kyaddondo D, Whyte SR. Spaces for talking: communication patterns of children on antiretroviral therapy in Uganda. Child Youth Serv Rev. 2014;45:38–46.
Bernays S, Paparini S, Gibb D, Seeley J. When information does not suffice: young people living with HIV and communication about ART adherence in the clinic. Vulnerable Child Youth Stud. 2016;11(1):60–8.
Greenhalgh C, Evangeli M, Frize G, Foster C, Fidler S. Intimate relationships in young adults with perinatally acquired HIV: partner considerations. AIDS Care. 2013;25(4):447–50.
Fernet M, Wong K, Richard ME, Otis J, Levy JJ, Lapointe N, et al. Romantic relationships and sexual activities of the first generation of youth living with HIV since birth. AIDS Care. 2011;23(4):393–400.
Wiener LS, Battles HB. Untangling the web: a close look at diagnosis disclosure among HIV-infected adolescents. J Adolesc Health. 2006;38(3):307–9.
Zgambo M, Arabiat D, Ireson D. It cannot happen, never: a qualitative study exploring youth views on disclosure of HIV diagnosis to their sexual partners in Southern Malawi. J Assoc Nurses AIDS Care: JANAC. 2021;32(6):652–61.
Hult JR, Wrubel J, Branstrom R, Acree M, Moskowitz JT. Disclosure and nondisclosure among people newly diagnosed with HIV: an analysis from a stress and coping perspective. AIDS Patient Care STDS. 2012;26(3):181–90.
Viljoen L, Wademan D, Hoddinott G, Bond V, Seeley J, Bock P, et al. The act of telling: South African women’s narratives of HIV status disclosure to intimate partners in the HPTN 071 (PopART) HIV prevention trial. Womens Health (Lond). 2021;17:1745506521998204.
Serovich JM, Laschober TC, Brown MJ, Kimberly JA. Assessment of HIV disclosure and sexual behavior among Black men who have sex with men following a randomized controlled intervention. Int J STD AIDS. 2018;29(7):673–9.
Serovich JM, Laschober TC, Brown MJ, Kimberly JA. Evaluation of HIV disclosure behavior following a randomized controlled disclosure intervention for men who have sex with men living with HIV. Arch Sex Behav. 2018;47(7):2051–9.
Serovich JM, Laschober TC, Brown MJ, Kimberly JA, Lescano CM. Effects of a decision-making intervention to help decide whether to disclose HIV-positive status to family members on well-being and sexual behavior. Arch Sex Behav. 2020;49(6):2091–101.
Serovich JM, Laschober TC, Brown MJ, Kimberly JA. Longitudinal findings on changes in and the link between HIV-related communication, risky sexual behavior, and relationship status in men who have sex with men living with HIV. Sex Transm Dis. 2017;44(12):732–8.
Rochat TJ, Stein A, Cortina-Borja M, Tanser F, Bland RM. The Amagugu intervention for disclosure of maternal HIV to uninfected primary school-aged children in South Africa: a randomised controlled trial. The lancet HIV. 2017;4(12):e566–76.
Schulte MT, Armistead L, Murphy DA, Marelich W. Multisite longitudinal efficacy trial of a disclosure intervention (TRACK) for HIV+ mothers. J Consult Clin Psychol. 2021;89(2):81–95.
Lukyamuzi Z, Nabisere RM, Nakalega R, Atuhaire P, Kataike H, Ssuna B, et al. Community health workers improve HIV disclosure among HIV-affected sexual partners in rural Uganda: a quasi-experimental study. Glob Health Sci Pract. 2022;10(5).
Kennedy CE, Fonner VA, Armstrong KA, O’Reilly KR, Sweat MD. Increasing HIV serostatus disclosure in low and middle-income countries: a systematic review of intervention evaluations. AIDS. 2015;29(Suppl 1):S7–23.
Evangeli M, Foster C. Who, then what? The need for interventions to help young people with perinatally acquired HIV disclose their HIV status to others. AIDS. 2014;28(Suppl 3):S343–6.
Gore-Felton C, Rotheram-Borus MJ, Weinhardt LS, Kelly JA, Lightfoot M, Kirshenbaum SB, et al. The healthy living project: an individually tailored, multidimensional intervention for HIV-infected persons. AIDS Educ Prev. 2005;17(1 Suppl A):21–39.
Murphy DA, Marelich WD, Graham J, Payne DL. Children affected by maternal HIV/AIDS: feasibility and acceptability trial of the Children United with Buddies (CUB) intervention. Clin Child Psychol Psychiatry. 2015;20(1):117–33.
Snyder K, Wallace M, Duby Z, Aquino LDH, Stafford S, Hosek S, et al. Preliminary results from Hlanganani (coming together): a structured support group for HIV-infected adolescents piloted in Cape Town, South Africa. Child Youth Serv Rev. 2014;45:114–21.
Rotheram-Borus MJ, Lee MB, Murphy DA, Futterman D, Duan N, Birnbaum JM, et al. Efficacy of a preventive intervention for youths living with HIV. Am J Public Health. 2001;91(3):400–5.
Toska E, Cluver LD, Hodes R, Kidia KK. Sex and secrecy: how HIV-status disclosure affects safe sex among HIV-positive adolescents. AIDS Care. 2015;27(Suppl 1):47–58.
WHO. WHO recommendations on adolescent sexual and reprodcutive health and rights. Geneva: World Health Organisation; 2018.
Rochat TJ, Mkwanazi N, Bland R. Maternal HIV disclosure to HIV-uninfected children in rural South Africa: a pilot study of a family-based intervention. BMC Public Health. 2013;13:147.
Thoth CA, Tucker C, Leahy M, Stewart SM. Self-disclosure of serostatus by youth who are HIV-positive: a review. Journal of behavioral medicine. 2013.
Murphy DA, Roberts KJ, Hoffman D, Molina A, Lu MC. Barriers and successful strategies to antiretroviral adherence among HIV-infected monolingual Spanish-speaking patients. AIDS Care. 2003;15(2):217–30.
Bott S, Obermeyer CM. The social and gender context of HIV disclosure in sub-Saharan Africa: a review of policies and practices. SAHARA J: J Soc Asp HIV/AIDS Res Alliance/SAHARA, Hum Sci Res Council. 2013;10(Suppl 1):S5-16.
Foster C, Ayers S, McDonald S, Frize G, Chhabra S, Pasvol TJ, et al. Clinical outcomes post transition to adult services in young adults with perinatally acquired HIV infection: mortality, retention in care and viral suppression. AIDS. 2020;34(2):261–6.
Evangeli M, Foster C, Musiime V, Fidler S, Seeley J, Gnan G. A randomised feasibility trial of an intervention to support sharing of HIV status for 18–25-year olds living with perinatally acquired HIV compared with standard care: HIV Empowering Adults’ Decisions to Share-UK/Uganda Project (HEADS-UP). Pilot Feasibility Stud. 2020;6:141.
Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. Brit Med J. 2008;337(7676).
Miller WR, Rollnick S. Motivational interviewing, Third Edition: helping people change: Guilford; 2012.
Evangeli M, Wroe AL. HIV disclosure anxiety: a systematic review and theoretical synthesis. AIDS Behav. 2017;21(1):1–11.
Evangeli M, Kagee A. A model of caregiver paediatric HIV disclosure decision-making. Psychol Health Med. 2016;21(3):338–53.
Greene K. An integrated model of health disclosure decision-making. In: Afifi TD, Afifi WA, editors. Uncertainty and information regulation in interpersonal contexts: theories and applications. New York: Routledge; 2009. p. 226–53.
Chaudoir SR, Fisher JD, Simoni JM. Understanding HIV disclosure: a review and application of the disclosure processes model. Soc Sci Med. 2011;72(10):1618–29.
Bakeera-Kitaka S, Nabukeera-Barungi N, Nostlinger C, Addy K, Colebunders R. Sexual risk reduction needs of adolescents living with HIV in a clinical care setting. AIDS Care. 2008;20(4):426–33.
Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci DS, Ory M, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol. 2004;23(5):443–51.
Evangeli M, Foster C, Musiime V, Fidler S, Seeley J, Frize G, et al. Cultural adaption, translation, preliminary reliability and validity of key psychological and behavioural measures for 18 to 25 year-olds living with HIV in Uganda: a multi-stage approach. AIDS Behav. 2023.
Skevington SM, Lotfy M, O'Connell KA, Group W. The World Health Organization's WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res: Int J Qual Life Asp Treat Care Rehabil. 2004;13(2):299–310.
Martin F, Russell S, Seeley J. The WHOQOL BREF questionnaire in Luganda: validation with sample including people living with HIV in Uganda. Norwich: University of East Anglia; 2013.
Cronje JH, Williams M, Steenkamp L, Venter D, Elkonin D. The quality of life of HIV-infected South African university students: experiences with the WHOQOL-HIV-Bref. AIDS Care. 2017;29(5):632–5.
Sarason IG, Sarason BR, Shearin EN, Pierce GR. A brief measure of social support: Practical and theoretical implications. Journal of Social and Personal Relationships. 1987;4(497–510).
Mutumba M, Bauermeister JA, Harper GW, Musiime V, Lepkowski J, Resnicow K, et al. Psychological distress among Ugandan adolescents living with HIV: examining stressors and the buffering role of general and religious coping strategies. Global Public Health. 2016.
Snyder CR, Sympson SC, Ybasco FC, Borders TF, Babyak MA, Higgins RL. Development and validation of the State Hope Scale. J Pers Soc Psychol. 1996;70(2):321–35.
Gibbs A, Desmond C, Barnett T, Shahmanesh M, Seeley J. Is hope associated with HIV-acquisition risk and intimate partner violence amongst young women and men? A cross-sectional study in urban informal settlements in South Africa. AIDS Care. 2023;35(6):833–40.
Legare F, Kearing S, Clay K, Gagnon S, D’Amours D, Rousseau M, et al. Are you SURE?: assessing patient decisional conflict with a 4-item screening test. Canadian family physician Medecin de famille canadien. 2010;56(8):e308–14.
Evangeli M. The adolescent HIV disclosure cognition and affect scale: preliminary reliability and validity. J Pediatr Psychol. 2017;42(6):711–20.
Evangeli M, Hinch R, Nesbitt L, Abbas M. Developing a coding scheme for adolescents’ HIV disclosure plans. Unpublished.
Reinius M, Wettergren L, Wiklander M, Svedhem V, Ekstrom AM, Eriksson LE. Development of a 12-item short version of the HIV stigma scale. Health Qual Life Outcomes. 2017;15(1):115.
Filiatreau LM, Wright M, Kimaru L, Gomez-Olive FX, Selin A, Twine R, et al. Correlates of ART use among newly diagnosed HIV positive adolescent girls and young women enrolled in HPTN 068. AIDS Behav. 2020;24(9):2606–15.
Lehmann G, Prime K, Foster C, Frize G, Fidler S, Evangeli M, editors. The relationship between sharing one’s HIV status and agentic and communal values in young adults with perinatally acquired HIV. AIDS Impact; 2019 July 2019; London.
Kiwanuka N, Mpendo J, Asiimwe S, Ssempiira J, Nalutaaya A, Nambuusi B, et al. A randomized trial to assess retention rates using mobile phone reminders versus physical contact tracing in a potential HIV vaccine efficacy population of fishing communities around Lake Victoria, Uganda. BMC Infect Dis. 2018;18(1):591.
Foster C, McDonald S, Frize G, Ayers S, Fidler S. “Payment by Results”–financial incentives and motivational interviewing, adherence interventions in young adults with perinatally acquired HIV-1 infection: a pilot program. AIDS Patient Care STDS. 2014;28(1):28–32.
Evangeli M, Lut I, Ely A. A longitudinal evaluation of an intensive residential intervention (camp) for 12–16 year olds living with HIV in the UK: evidence of psychological change maintained at six month follow-up. AIDS Care. 2019;31(1):85–9.
Lundahl B, Kunz C, Brownell C, Tollefson D, Burke BL. A meta-analysis of motivational interviewing: 25 years of empirical studies. Res Soc Work Pract. 2010;20:137–60.
Borrelli B. The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. J Public Health Dent. 2011;71(s1):S52–63.
Aurpibul L, Tangmunkongvorakul A, Detsakunathiwatchara C, Masurin S, Srita A, Meeart P, et al. Social effects of HIV disclosure, an ongoing challenge in young adults living with perinatal HIV: a qualitative study. Front Public Health. 2023;11:1150419.
Acknowledgements
We would like to thank ViiV Healthcare UK, who funded the study, in particular Chris Stainsby and Serufusa Sekidde. We would also like to thank Juliet Ategeka, Jade Robinson and Sam Harris for data entry, Niamh Hinkley for literature searching, and Jane Vosper for therapist supervision. Intervention components were developed with assistance from Bill Miller, Teresa Moyers, Magda Conway, Dorothy Dow, Creative Colony and Bored Digital. Participating sites were: UK: St. Mary’s Hospital, London: Caroline Foster, Paula Seery, Hana Jayadel, Sara Ayers; St. George’s Hospital, London: Katia Prime, Lisa Hamzah; King’s College Hospital London: Elizabeth Hamlyn, Sally Hawkins; Chiva: Amanda Ely, Abi Carter; Heartlands Hospital, Birmingham: Claire Robertson, Gerry Gillian; North Manchester General Hospital: Katherine Ajdukiewicz. Uganda: Victor Musiime, Annette Uwizera, William Matovu. We would also like to thank all therapists, members of both advisory groups and all participants.
Funding
This study was funded by ViiV Healthcare UK Ltd., 980 Great West Road, Brentford, Middlesex, TW8 9GS, UK.
Author information
Authors and Affiliations
Contributions
ME was involved in funding acquisition, study design, project administration, supervision, writing, editing and statistical analysis. SF, GF, CF, VM and JS were involved in study design. GG and AU were involved in study coordination, recruitment, data collection, preparing intervention materials and assessing intervention fidelity. ML was involved in statistical analysis. All authors were involved in reviewing, and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical Approval
The study was given ethical approval by a UK NHS Research Ethics Committee (IRAS:252582) and the UK Health Research Authority, by the Uganda National Council of Science and Technology (HS2636), and by institutional review boards at the Joint Clinical Research Centre, Uganda (JC0319) and Royal Holloway, University of London, UK.
Consent to Participate and Publish
Written consent was sought from participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: “In the article, the Acknowledgements text were incorrectly given as “We would like to thank ViiV Healthcare UK, who funded the study, in particular Chris Stainsby and Serufusa Sekidde. We would also like to thank Juliet Ategeka, Jade Robinson and Sam Harris for data entry, Niamh Hinkley for literature searching, and Jane Vosper for therapist supervision. Intervention components were developed with assistance from Bill Miller, Teresa Moyers, Magda Conway, Dorothy Dow, Creative Colony and Bored Digital. We would also like to thank all study collaborators, therapists, members of both advisory groups and all participants” but should have been “We would like to thank ViiV Healthcare UK, who funded the study, in particular Chris Stainsby and Serufusa Sekidde. We would also like to thank Juliet Ategeka, Jade Robinson and Sam Harris for data entry, Niamh Hinkley for literature searching, and Jane Vosper for therapist supervision. Intervention components were developed with assistance from Bill Miller, Teresa Moyers, Magda Conway, Dorothy Dow, Creative Colony and Bored Digital. Participating sites were: UK: St. Mary’s Hospital, London: Caroline Foster, Paula Seery, Hana Jayadel, Sara Ayers; St. George’s Hospital, London: Katia Prime, Lisa Hamzah; King’s College Hospital London: Elizabeth Hamlyn, Sally Hawkins; Chiva: Amanda Ely, Abi Carter; Heartlands Hospital, Birmingham: Claire Robertson, Gerry Gillian; North Manchester General Hospital: Katherine Ajdukiewicz. Uganda: Victor Musiime, Annette Uwizera, William Matovu. We would also like to thank all therapists, members of both advisory groups and all participants.”
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Evangeli, M., Gnan, G., Musiime, V. et al. The HIV Empowering Adults’ Decisions to Share: UK/Uganda (HEADS-UP) Study—A Randomised Feasibility Trial of an HIV Disclosure Intervention for Young Adults with Perinatally Acquired HIV. AIDS Behav 28, 1947–1964 (2024). https://doi.org/10.1007/s10461-024-04294-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-024-04294-2