Abstract
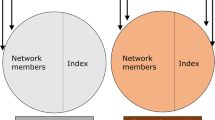
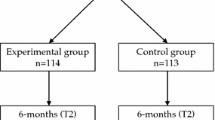
Peer-driven interventions can be effective in reducing HIV injection risk behaviors among people who inject drugs (PWID). We employed a causal mediation framework to examine the mediating role of recall of intervention knowledge in the relationship between a peer-driven intervention and subsequent self-reported HIV injection-related risk behavior among PWID in the HIV Prevention Trials Network (HPTN) 037 study. For each intervention network, the index participant received training at baseline to become a peer educator, while non-index participants and all participants in the control networks received only HIV testing and counseling; recall of intervention knowledge was measured at the 6-month visit for each participant, and each participant was followed to ascertain HIV injection-related risk behaviors at the 12-month visit. We used inverse probability weighting to fit marginal structural models to estimate the total effect (TE) and controlled direct effect (CDE) of the intervention on the outcome. The proportion eliminated (PE) by intervening to remove mediation by the recall of intervention knowledge was computed. There were 385 participants (47% in intervention networks) included in the analysis. The TE and CDE risk ratios for the intervention were 0.47 [95% confidence interval (CI): 0.28, 0.78] and 0.73 (95% CI: 0.26, 2.06) and the PE was 49%. Compared to participants in the control networks, the peer-driven intervention reduced the risk of HIV injection-related risk behavior by 53%. The mediating role of recall of intervention knowledge accounted for less than 50% of the total effect of the intervention, suggesting that other potential causal pathways between the intervention and the outcome, such as motivation and skill, self-efficacy, social norms and behavior modeling, should be considered in future studies.


Similar content being viewed by others
Data Availability
The HPTN 037 study data sets are publicly available and can be requested from the Statistical Center for HIV/AIDS Research and Prevention through the ATLAS Science Portal through https://atlas.scharp.org/cpas/project/HPTN/.
Code Availability
Not applicable.
Abbreviations
- CI:
-
Confidence interval
- TE:
-
Total effect
- CDE:
-
Controlled direct effect
- PE:
-
Proportion eliminated
- IPTW:
-
Inverse-probability-of-treatment weight
- IPMW:
-
Inverse-probability-of-mediator weight
- GEEs:
-
Generalized estimating equations
- HPTN:
-
HIV Prevention Trials Network
- HIV:
-
Human Immunodeficiency Virus
- PWID:
-
People who inject drugs
- RR:
-
Risk ratio
References
Rodger AJ, Cambiano V, Bruun T, et al. Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. JAMA. 2016;316(2):171–81.
Macdonald V, Verster A, Baggaley R. A call for differentiated approaches to delivering HIV services to key populations. J Int AIDS Soc. 2017;20:21658.
Risher K, Mayer K, Beyrer C. The HIV treatment cascade in men who have sex with men, people who inject drugs and sex workers. Curr Opin HIV AIDS. 2015;10(6):420.
Mathers BM, Degenhardt L, Phillips B, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet. 2008;372(9651):1733–45.
Gant Z, Johnson SD, Li J, et al. Diagnoses of HIV Infection in the United States and Dependent Areas (Updated), 2018. 2020.
Rhodes T, Singer M, Bourgois P, et al. The social structural production of HIV risk among injecting drug users. Soc Sci Med. 2005;61(5):1026–44.
Koram N, Liu H, Li J, et al. Role of social network dimensions in the transition to injection drug use: actions speak louder than words. AIDS Behav. 2011;15(7):1579–88.
Lakon CM, Ennett ST, Norton EC. Mechanisms through which drug, sex partner, and friendship network characteristics relate to risky needle use among high risk youth and young adults. Soc Sci Med. 2006;63(9):2489–99.
Tsang MA, Schneider JA, Sypsa V, et al. Network characteristics of people who inject drugs within a new HIV epidemic following austerity in Athens, Greece. J Acquir Immune Defic Syndr. 2015;69(4):499–508.
Baggaley RF, Boily M-C, White RG, et al. Risk of HIV-1 transmission for parenteral exposure and blood transfusion: a systematic review and meta-analysis. AIDS. 2006;20(6):805–12.
Hacker E, Cohn J, Golden MR, et al. HIV pre-exposure prophylaxis (Prep) uptake, initiation, and persistence in the detroit public health STD clinic. Open Forum Infect Dis. 2017;4:S437–S437.
Hess KL, Johnson SD, Hu X, et al. Diagnoses of HIV infection in the United States and dependent areas. HIV Surveill Rep. 2017;2(28):1–25.
Smith DK, Van Handel M, Wolitski RJ, et al. Vital signs: estimated percentages and numbers of adults with indications for preexposure prophylaxis to prevent HIV acquisition-United States, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(46):1291–5.
Degenhardt L, Mathers B, Vickerman P, et al. Prevention of HIV infection for people who inject drugs: why individual, structural, and combination approaches are needed. Lancet. 2010;376(9737):285–301.
Kerrigan D, Weiss E. Peer education and HIV/AIDS: past experience, future directions: report of a consultation. Population Council, Horizons Project; 2000.
Latkin CA. Outreach in natural settings: the use of peer leaders for HIV prevention among injecting drug users’ networks. Public Health Rep. 1998;113:151–9.
Weeks MR, Li J, Dickson-Gomez J, et al. Outcomes of a peer HIV prevention program with injection drug and crack users: the risk avoidance partnership. Subst Use Misuse. 2009;44(2):253–81.
Latkin CA, Donnell D, Metzger D, et al. The efficacy of a network intervention to reduce HIV risk behaviors among drug users and risk partners in Chiang Mai, Thailand and Philadelphia, USA. Soc Sci Med. 2009;68(4):740–8.
Tobin KE, Kuramoto SJ, Davey-Rothwell MA, et al. The step into action study: a peer-based, personal risk network-focused HIV prevention intervention with injection drug users in Baltimore, Maryland. Addiction. 2011;106(2):366–75.
Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111(3):455.
Des Jarlais DC, Friedman SR, Friedmann P, et al. HIV/AIDS-related behavior change among injecting drug users in different national settings. AIDS. 1995;9(6):611–7.
Sikkema KJ, Heckman TG, Kelly JA, et al. HIV risk behaviors among women living in low-income, inner-city housing developments. Am J Public Health. 1996;86:1123–8.
Latkin CA, Mandell W, Vlahov D, et al. The long-term outcome of a personal network-oriented HIV prevention intervention for injection drug users: the safe study. Am J Commun Psychol. 1996;24(3):341–64.
Smyth HL, Pitpitan EV, MacKinnon DP, et al. Assessing potential outcomes mediation in HIV interventions. AIDS Behav. 2021;25:1–14.
Latkin C, Donnell D, Liu TY, et al. The dynamic relationship between social norms and behaviors: the results of an HIV prevention network intervention for injection drug users. Addiction. 2013;108(5):934–43.
Latkin C, Donnell D, Celentano DD, et al. Relationships between social norms, social network characteristics, and HIV risk behaviors in Thailand and the United States. Health Psychol. 2009;28(3):323.
Latkin C, Kuramoto S, Davey-Rothwell M, et al. Social norms, social networks, and HIV risk behavior among injection drug users. AIDS Behav. 2010;14(5):1159–68.
Medley A, Kennedy C, O’Reilly K, et al. Effectiveness of peer education interventions for HIV prevention in developing countries: a systematic review and meta-analysis. AIDS Educ Prev. 2009;21(3):181–206.
Chen HT. Theory-driven evaluations. London: Sage Publications; 1990.
MacKinnon DP. Analysis of mediating variables in prevention and intervention research. NIDA Res Monogr. 1994;139:127–127.
Rogers EM. Diffusion of innovations. New York: Simon and Schuster; 2010.
Robins JM, Greenland S. Identifiability and exchangeability for direct and indirect effects. Epidemiology. 1992;3:143–55.
VanderWeele TJ, Vansteelandt S. Odds ratios for mediation analysis for a dichotomous outcome. Am J Epidemiol. 2010;172(12):1339–48.
Valeri L, VanderWeele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18(2):137.
VanderWeele TJ. Policy-relevant proportions for direct effects. Epidemiology. 2013;24(1):175.
Andrews RM, Didelez V. Insights into the cross-world independence assumption of causal mediation analysis. Epidemiology. 2021;32(2):209–19.
Naimi AI, Kaufman JS, MacLehose RF. Mediation misgivings: ambiguous clinical and public health interpretations of natural direct and indirect effects. Int J Epidemiol. 2014;43(5):1656–61.
Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162(3):199–200.
Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–6.
VanderWeele T. Explanation in causal inference: methods for mediation and interaction. Oxford: Oxford University Press; 2015.
Suzuki E, Evans D, Chaix B, et al. On the “proportion eliminated” for risk differences versus excess relative risks. Epidemiology. 2014;25(2):309.
Yu Y, Liew Z, Wang A, et al. Mediating roles of preterm birth and restricted fetal growth in the relationship between maternal education and infant mortality: a Danish population-based cohort study. PLoS Med. 2019;16(6): e1002831.
Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11(5):550–60.
Winett RA, Anderson ES, Desiderato LL, et al. Enhancing social diffusion theory as a basis for prevention intervention: a conceptual and strategic framework. Appl Prev Psychol. 1995;4(4):233–45.
Buchanan AL, Vermund SH, Friedman SR, et al. Assessing individual and disseminated effects in network-randomized studies. Am J Epidemiol. 2018;187(11):2449–59.
Richiardi L, Bellocco R, Zugna D. Mediation analysis in epidemiology: methods, interpretation and bias. Int J Epidemiol. 2013;42(5):1511–9.
Lipsitch M, Tchetgen ET, Cohen T. Negative controls: a tool for detecting confounding and bias in observational studies. Epidemiology. 2010;21(3):383.
Ghosh D, Krishnan A, Gibson B, et al. Social network strategies to address HIV prevention and treatment continuum of care among at-risk and HIV-infected substance users: a systematic scoping review. AIDS Behav. 2017;21(4):1183–207.
MacKinnon DP. Introduction to statistical mediation analysis. London: Routledge; 2008.
Hoyle RH, Kenny DA. Sample size, reliability, and tests of statistical mediation. Stat Strat Small Sample Res. 1999;1:195–222.
Simmons N, Donnell D, Ou SS, et al. Assessment of contamination and misclassification biases in a randomized controlled trial of a social network peer education intervention to reduce HIV risk behaviors among drug users and risk partners in Philadelphia, PA and Chiang Mai, Thailand. AIDS Behav. 2015;19(10):1818–27.
Acknowledgements
We thank Dr. Carl Latkin for providing access to the HPTN 037 data.
Funding
Drs. Ashley Buchanan, Natallia Katenka, M. Elizabeth Halloran and TingFang Lee were supported by the National Institute on Drug Abuse (NIDA) Avenir Award Number DP2DA046856 of the National Institutes of Health. Dr. Hilary Aroke is supported by a NIDA Diversity Supplement Grant (DP2 DA046856). Dr. M. Elizabeth Halloran was also supported by NIH grant number R01 AI085073; Dr. Forrest W. Crawford by NIDA Award Number 1DP2HD091799-01, and Dr. Carl Latkin was supported by grant number R01DA050470. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
Conception and design: HA, AB, NK, FC. Data Analysis: HA, TL. Data interpretation: All. Manuscript writing: All. Manuscript revisions and approval of final article: All.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
Approved by the University of Rhode Island Institutional Review Board.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aroke, H., Buchanan, A., Katenka, N. et al. Evaluating the Mediating Role of Recall of Intervention Knowledge in the Relationship Between a Peer-Driven Intervention and HIV Risk Behaviors Among People Who Inject Drugs. AIDS Behav 27, 578–590 (2023). https://doi.org/10.1007/s10461-022-03792-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-022-03792-5