Abstract
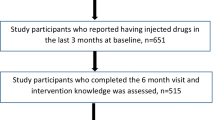
STEP into Action assessed the efficacy of a peer-based HIV prevention intervention in reducing HIV risk behaviors among people who inject drugs (PWIDs) in Baltimore. This analysis examined the effect of the intervention on the change in frequency of conversation about HIV prevention topics over time. 114 participants were randomized into an experimental and 113 into a control group. Data was collected prospectively at 6, 12, and 18 months. The experimental group talked more frequently about HIV prevention topics compared to the control group at 6-month visit. At 18 months relative risk ratios (RRR) remained statistically significant for conversation about the danger of needle sharing (RRR = 3.21) and condom use (RRR = 2.81). The intervention resulted in an increased conversation about HIV prevention among PWIDs, but the sustainability past 6 months remained a challenge; suggesting that interventions should be designed to constantly reinforce communication about HIV prevention among PWIDs.
Resumen
STEP into Action examinó la eficacia de una intervención preventiva basada en pares en reducir los comportamientos de riesgo para el contagio con el Virus de Inmunodeficiencia Humana (VIH) entre usuarios de drogas inyectables (UDI) en Baltimore. Este análisis evaluó el efecto de la intervención en el cambio en la frecuencia de conversaciones sobre temas de prevención de VIH a lo largo del tiempo. Los pacientes fueron aleatoriamente separados en dos grupos, el experimental y el de controles, con 114 y 113 miembros, respectivamente. Los datos fueron recolectados prospectivamente a los 6, 12 y 18 meses. El grupo experimental habló más frecuentemente sobre temas de prevención de VIH que el grupo control, al compararlos 6 meses después de la intervención. A los 18 meses los riesgos relativos (RR) se mantuvieron estadísticamente significativos para las conversaciones sobre el peligro de compartir agujas (RR = 3,21) y sobre uso de condón (RR = 2,81). La intervención dio como resultado un aumento en las conversaciones sobre prevención de VIH entre UDI, pero la sustentabilidad después de 6 meses continúa siendo un desafío, sugiriendo que las intervenciones deben ser diseñadas para reforzar constantemente la comunicación sobre prevención de VIH entre UDI.


Similar content being viewed by others
References
Latkin CA, Davey MA, Hua W. Needle exchange program utilization and entry into drug user treatment: is there a long-term connection in Baltimore, Maryland? Subst Use Misuse. 2006;41(14):1991–2001.
Rudolph AE, Crawford ND, Ompad DC, Benjamin EO, Stern RJ, Fuller CM. Comparison of injection drug users accessing syringes from pharmacies, syringe exchange programs, and other syringe sources to inform targeted HIV prevention and intervention strategies. J Am Pharm Assoc. 2010;50(2):140–7 (2003).
Centers for Disease Control and Prevention. Estimated HIV incidence in the United States, 2007–2010. HIV surveillance supplemental report. 2012;17(4).
Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 U.S. dependent areas—2011. HIV surveillance supplemental report. 2013;18(5).
Baltimore City Health Department. Need exchange program; 2012. http://www.baltimorehealth.org/needle-exchange-info.html. Accessed 9 Mar 2014.
Tempalski B, Pouget ER, Cleland CM, Brady JE, Cooper HL, Hall HI, Lansky A, West BS, Friedman SR. Trends in the population prevalence of people who inject drugs in US metropolitan areas 1992–2007. PLoS One. 2013;8(6):e64789.
Center for HIV Surveillance, Epidemiology and Evaluation. Baltimore City HIV/AIDS epidemiological profile fourth quarter 2012. Maryland Department of Health and Mental Hygiene. http://phpa.dhmh.maryland.gov/OIDEOR/CHSE/Shared%20Documents/Baltimore-City.pdf. Accessed 15 Feb 2014.
Koester S, Glanz J, Baron A. Drug sharing among heroin networks: implications for HIV and hepatitis B and C prevention. AIDS Behav. 2005;9(1):27–39.
Mehta SH, Galai N, Astemborski J, et al. HIV incidence among injection drug users in Baltimore, Maryland (1988–2004). J Acquir Immune Defic Syndr. 2006;43(3):368–72.
De P, Cox J, Boivin JF, Platt RW, Jolly AM, Alexander PE. HIV and HCV discordant injecting partners and their association to drug equipment sharing. Scand J Infect Dis. 2009;41(3):206–14.
Vlahov D, Des Jarlais DC, Goosby E, et al. Needle exchange programs for the prevention of human immunodeficiency virus infection: epidemiology and policy. Am J Epidemiol. 2001;154(12 Suppl):S70–7.
Metzger DS, Navaline H, Woody GE. Drug abuse treatment as AIDS prevention. Public Health Rep. 1998;113(Suppl 1):97–106.
Rhodes T. Risk environments and drug harms: a social science for harm reduction approach. Int J Drug Policy. 2009;20(3):193–201.
Rogers E. Diffusion of innovations. 5th ed. New York: Free Press; 2003.
Bandura A. Social learning theory. Englewood Cliffs: Prentice Hall; 1977.
Turner JC. Social comparison and social identity: some perspectives for intergroup behavior. Eur J Soc Psychol. 1978;5:5–34.
Simoni JM, Nelson KM, Franks JC, Yard SS, Lehavot K. Are peer interventions for HIV efficacious? A systematic review. AIDS Behav. 2011;15(8):1589–95.
Ye S, Yin L, Amico KR, Simoni JM, Vermund SH, Ruan Y, Shao Y, Qian HZ. Efficacy of peer-led interventions to reduce unprotected anal intercourse among men who have sex with men: a meta-analysis. PLoS One. 2014;9(3):e90788.
Johnson BT, Michie S, Snyder LB. Effects of behavioral intervention content on HIV prevention outcomes: a meta-review of meta-analyses. J Acquir Immune Defic Syndr. 2014;66(Suppl 3):S259–70.
Latkin CA. Outreach in natural settings: the use of peer leaders for HIV prevention among injecting drug users’ networks. Public Health Rep. 1998;113(Suppl 1):151–9.
Go VF, Frangakis C, Le Minh N, et al. Effects of an HIV peer prevention intervention on sexual and injecting risk behaviors among injecting drug users and their risk partners in Thai Nguyen, Vietnam: a randomized controlled trial. Soc Sci Med. 2013;96:154–64.
Jain B, Krishnan S, Ramesh S, Sabarwal S, Garg V, Dhingra N. Effect of peer-led outreach activities on injecting risk behavior among male drug users in Haryana, India. Harm Reduct J. 2014;11:3.
Davey-Rothwell MA, Latkin CA. HIV-related communication and perceived norms: an analysis of the connection among injection drug users. AIDS Educ Prev. 2007;19(4):298–309.
Des Jarlais DC, Friedman SR, Friedmann P, et al. HIV/AIDS-related behavior change among injecting drug users in different national settings. AIDS. 1995;9(6):611–7.
Gibson DR, Choi KH, Catania JA, Sorensen JL, Kegeles S. Psychosocial predictors of needle sharing among intravenous drug users. Int J Addict. 1993;28(10):973–81.
Tobin KE, Kuramoto SJ, Davey-Rothwell MA, Latkin CA. The STEP into Action study: a peer-based, personal risk network-focused HIV prevention intervention with injection drug users in Baltimore, Maryland. Addiction. 2011;106(2):366–75.
Rabe-Hesketh S, Skrondal A. Multilevel and longitudinal modeling using Stata, Volume II: categorical responses, counts, and survival. 3rd ed. New York: Taylor & Francis; 2012.
StataCorp LP. Stata data analysis and statistical software: release 13.0. College Station, TX: Stata Corporation; 2013.
Parsons JT, VanOra J, Missildine W, Purcell DW, Gomez CA. Positive and negative consequences of HIV disclosure among seropositive injection drug users. AIDS Educ Prev. 2004;16(5):459–75.
El-Bassel N, Gilbert L, Rajah V, Foleno A, Frye V. Fear and violence: raising the HIV stakes. AIDS Educ Prev. 2000;12(2):154–70.
Maman S, van Rooyen H, Stankard P, Chingono A, Muravha T, Ntogwisangu J, Phakathi Z, Srirak N, Morin FS. NIMH Project Accept (HPTN 043) study team. NIMH Project Accept (HPTN 043): results from in-depth interviews with a longitudinal cohort of community members. PLoS One. 2014;9(1):e87091.
Acknowledgments
This research was supported by the National Institutes of Health/National Institute on Drug Abuse.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mihailovic, A., Tobin, K. & Latkin, C. The Influence of a Peer-Based HIV Prevention Intervention on Conversation About HIV Prevention Among People Who Inject Drugs in Baltimore, Maryland. AIDS Behav 19, 1792–1800 (2015). https://doi.org/10.1007/s10461-015-1048-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1048-4