Abstract
Within the field of robots in medical education, most of the work done during the last years has focused on surgeon training in robotic surgery, practicing surgery procedures through simulators. Apart from surgical education, robots have also been widely employed in assistive and rehabilitation procedures, where education has traditionally focused in the patient. Therefore, there has been extensive review bibliography in the field of medical robotics focused on surgical and rehabilitation and assistive robots, but there is a lack of survey papers that explore the potential of robotics in the education of healthcare students and professionals beyond their training in the use of the robotic system. The scope of the current review are works in which robots are used as didactic tools for the education of professionals in health sciences, investigating the enablers and barriers that affect the use of robots as learning facilitators. Systematic literature searches were conducted in WOS and Scopus, yielding a total of 3812 candidate papers. After removing duplicates, inclusion criteria were defined and applied, resulting in 171 papers. An in-depth quality assessment was then performed leading to 26 papers for qualitative synthesis. Results show that robots in health sciences education are still developed with a roboticist mindset, without clearly incorporating aspects of the teaching/learning process. However, they have proven potential to be used in health sciences as they allow to parameterize procedures, autonomously guide learners to achieve greater engagement, or enable collective learning including patients and instructors "in the loop". Although there exist documented added-value benefits, further research and efforts needs to be done to foster the inclusion of robots as didactic tools in the curricula of health sciences professionals. On the one hand, by analyzing how robotic technology should be developed to become more flexible and usable to support both teaching and learning processes in health sciences education, as final users are not necessarily well-versed in how to use it. On the other, there continues to be a need to develop effective and standard robotic enhanced learning evaluation tools, as well good quality studies that describe effective evaluation of robotic enhanced education for professionals in health sciences. As happens with other technologies when applied to the health sciences field, studies often fail to provide sufficient detail to support transferability or direct future robotic health care education programs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Common definitions of robots describe them as machines that resemble a living creature capable of moving independently, performing complex and, often repetitive tasks (Sarrica et al., 2019). Such definitions have a strong bias towards early industrial robots as manipulators that can grasp and move objects in industrial environments. Nowadays, robots can cooperate closely with humans to perform jobs with greater precision and efficiency, for example surgical robots (Bonatti et al., 2021; Chen et al., 2021; Sharma & Bhardwaj, 2021), with an increasing importance since the COVID-19 pandemic.
In fact, in terms of employing robots in health sciences, the field of surgery has been the most active during the last three decades (Ginoya et al., 2021; Leal Ghezzi & Campos Corleta, 2016; Peters et al., 2018). However, robots have been increasingly used in the province of health sciences to perform a wide number of health related tasks (Kyrarini et al., 2021). Apart from surgical robotics, many other classifications have been proposed in the literature for health related robotics (Boubaker, 2020). One of the most widespread of such classifications is the one found in Cianchetti et al., (2018) who categorized health sciences related robotics as: medical robotics (Mapara & Patravale, 2017) including surgery (Collins & Wisz, 2020; Kadakia et al., 2020), diagnosis (Kaan & Ho, 2020; Tavakoli et al., 2020) and drug delivery devices (Mapara & Patravale, 2017; Nguyen et al., 2020); assistive robotics (Giansanti, 2021), such as wearable robots (Bai et al., 2018) and rehabilitation devices (Alias et al., 2017; Mohebbi, 2020), and human body mimicking robots including phantom devices (Hughes et al., 2020; Takeoka et al., 2017) and body-part simulators (Cz et al., 2012; Horvath et al., 2020).
Focusing on employing robots in health sciences education, again most of the work done during the last years has focused in surgeon training in robotic surgery (Collins & Wisz, 2020; Forgione & Guraya, 2017; Kadakia et al., 2020; Khalafallah et al., 2020). In this sense, it is common to practice surgery procedures through simulators, as the handling of robotic surgery devices requires additional skills (Azadi et al., 2021; Badash et al., 2016). In addition, preoperative planning or workflow optimization in the operating room can also be simulated in order to increase patient safety in the context of robotic surgery (Lovegrove et al., 2017). There is also a trend towards a standardized validated robotic surgery training curricula (Altok et al., 2018; Chen et al., 2020a, b), as the majority of current training is delivered with traditional methods such as laboratories that have access to cadavers or phantoms and dedicated training robots (Chen et al., 2020a, b).
In terms of assistive and rehabilitation robotics, education has traditionally focused in the patient, whether from the point of view of improving their quality of life (Gochoo et al., 2020; Louie et al., 2020; Pu et al., 2020), providing them with knowledge about their disease or a medical procedure they are about to undergo (Blanson Henkemans et al., 2013), or focusing on teaching them about the use of an aiding technology, such as wearable or rehabilitation devices (Ciullo et al., 2020; Mohebbi, 2020).
Physical mimicking systems (e.g., phantoms) have traditionally been used in training of medical students, both for diagnosis and practicing medical procedures (Cooper & Taqueti, 2004). However, to date most of these simulation training devices are still merely designed to reproduce the physical properties of tissues, human organs (Altok et al., 2018) or whole body (Wallace et al., 2010).
In terms of survey papers, there has been extensive review bibliography in the field of medical robotics (Cianchetti et al., 2018; Troccaz et al., 2019). Most of the recent surveys focus on surgical robots (Chen et al., 2021; Chen et al., 2020a, b; Gifari et al., 2019; Simaan et al., 2018; Peters et al., 2018; Díaz et al., 2017) and rehabilitation and assistive robots (Giansanti, 2021; Meng et al., 2017; Mohebbi, 2020; Rupal et al., 2017).
However, based on the existing bibliography, there is a lack of survey papers that explore the potential of robotics in the education of professionals in health sciences beyond the training in the use of the technical system itself (e.g., handling a surgery robotic platform or a rehabilitation device). As other works have shown (Murata et al., 2017; Lee et al., 2020b), the use of robotic technology in health sciences education provides professionals with learning scenarios that are more motivating, collaborative, interactive, and help to make medical training safer and more creative. Moreover, technological enhanced learning approaches have gained even more importance since the COVID-19 pandemic (García-Peñalvo et al., 2020, 2021). Therefore, the aim of the present survey is to explore the use of robotics as didactic tools for conveying learning in health sciences, to gain insights of how robotic technology is being incorporated in the teaching/learning process of health professionals, and if and how robotics is being added to their training curricula as a complement to traditional education methods. Research goals can be translated into the following main research questions: How are robotics considered in the health sciences education literature beyond surgical robots and the manipulation of robotic instruments? How are robotics integrated into the teaching/learning of health sciences? Are there documented added-value benefits of the use of robotics against other approaches?
Putting all together, we were interested in investigating the enablers and barriers that affect the use of robots as didactic tools for the education of health sciences professionals.
Methodology
The following sections describe the process undertaken, which follows the recommendations of the Associations for Medical Education in Europe (AMEE) (R. Sharma et al., 2015), complemented with the recommendations of Kitchenham (2007), Petersen (2015) and (García-Holgado et al., 2020).
Review scope and eligibility criteria
The scope of the current review are works in which robots are used as didactic tools for the education of professionals in health sciences. However, this statement needs more clarification, both in terms of what robots and didactic tools will be considered in the following sections.
Firstly, the review is oriented towards the education of professionals in health sciences, so those studies where robots are used to support professionals in the education of patients are out of the scope of the current review (Gochoo et al., 2020; Louie et al., 2020).
Current review does not consider proposals where there is no "physical" element, for example software robots where an AI (artificial intelligence) system runs on a host computer (Eckert et al., 2019), or virtual representations of robotic devices and/or patients without any type of robotic feedback (Fontanelli et al., 2019; Haji et al., 2021).
Finally, in terms of their use as didactic tools, the inclusion of papers in the current review is determined by the modelling goals of the robot. Robots provide an approximate representation of a real-world process which can be executed to perform a simulation. Within the health sciences field, this representation (model) of the real world can be categorized as (Jörg et al., 2013): (1) application model, that captures the procedure (Application-Centric); (2) system model, that captures the implementation of the robotic system (System-Centric); (3) patient model, that captures the environment with the focus on the patient (Patient-Centric). Taking the above classification into account, pure system – centric robotic education papers (e.g. providing trainees with skills in the use of a particular robotic device as in (Chen et al., 2020a, b; Khalafallah et al., 2020)) are out of the scope of this systematic review.
In addition, this review does not consider haptic simulators for surgical training, where the physical properties of the human body are parameterized to formulate the haptic model for the surgery simulator. There are various reasons for excluding such studies. On the one hand, the borderline of whether such systems could be considered robotic constructions or software robots with a haptic interface is in many cases unclear. Secondly, it is often difficult to establish if they are system-centric or application-centric didactic tools. Last but not least, there exists extensive and recent review bibliography in the field, as it has been one of the main subjects of technology-related medical education during the last decades (Chen et al., 2020a, b; Ginoya et al., 2021; Sharma & Bhardwaj, 2021; Chen et al., 2021; Bonatti et al., 2021).
Database selection
The databases in which to conduct the search were selected according to the following criteria:
-
The database is available for the authors’ institutions.
-
The database accepts the use of logical expressions or a similar mechanism.
-
The database allows full-length searches or searches only in specific fields of the works.
-
The database allows additional filtering options such as publication year or publication language.
-
The database is one of the most relevant in the main research areas of interest within this review process: education, health sciences and robotics.
Taking the above criteria into account, the search was conducted in the following electronic databases: Web of Science and Scopus. Both databases are commonly used in medicine, as they include most Embase, Cochrane and Medline results. In fact, medicine is the largest category of WoS and Scopus related papers over the last 15 years (Zhu & Liu, 2020). On the other hand, returned results include more knowledge domains than those returned by specialized databases, which a major point considering the interdisciplinarity nature of the current review.
Search string
Several searches where piloted in order to identify which terms added value to the search (see “Appendix 1”).
The final search strings used in the search are shown in Table 1. Wildcards were employed to maintain the search broad enough, complemented with proximity operators in such a way that the terms related with education and health sciences do not appear too far apart in the returned papers, and the strings returned a manageable number of results. In addition, while reviewing the piloted obtained results, it was observed that including terms related with simulation biased the results towards non-robotic interfaces. For that reason, and to include studies related with robotic human patient simulators, a second complementary search was performed which only focused on those terms.
Inclusion and exclusion criteria
The following inclusion criteria (IC) were developed by the two authors (SMP) and (FjGP) and employed to include or exclude a paper from the later analysis. If any of the papers failed to meet the IC, it was not further considered.
-
IC1: The papers focused on robotics AND
-
IC2: Those robotic solutions were utilized in health sciences education AND
-
IC3: The papers were written in English AND
-
IC4: The papers were published in peer-reviewed Journals, Books, Conferences or Workshops AND
-
IC5: Papers had a document body that was more than three pages long. Papers shorter than 3 pages are excluded from the review to speed up the review process as they are unlikely to fulfil the quality criteria.
Quality assessment criteria
To assess the quality of the primary studies, a quality checklist was developed by the two authors (SMP) and (FjGP). The quality assessment checklist consists of a series of questions to be answered from reading of the paper content. The objective of the checklist was that final included papers were able to provide as much information as possible related to the main research questions, and to avoid subjectivity in the final inclusion of studies in the synthesis. The answer to each of the questions was labeled as Yes/Partially/No and given a score of 0/0.5/1 respectively. The Yes/Partially/No values stand for: Yes = information is explicitly present in the paper; Partially = information is implicit/stated; No = information is not inferable. A score of 6 was used as a cut-off point to ensure that the studies clearly met the criteria, as it was observed that several papers with a score below 6, although related to the study topic, did not contain sufficient information to adequately answer the research questions. The considered checklist was as follows:
-
1.
Are the research aims related to teaching/learning with robots for health science professionals? Y/N/partial
-
2.
Is the use of a robotic platform clearly justified? Y/N/partial
-
3.
Is the robot goal clearly described? Y/N/partial
-
4.
Is the teaching/learning process clearly described? Y/N/partial
-
5.
Is there any kind of evaluation of the teaching/learning process? Y/N/partial
-
6.
Are data on the evaluation of the proposed solution available? Y/N/partial
-
7.
Are metrics clearly described and specified? Y/N/partial
-
8.
Is the proposed methodology compared against traditional teaching/learning approaches? Y/N/partial
-
9.
Are the links between data, interpretation and conclusions made clear? Y/N/partial
-
10.
Is the modelling approach patient or application—centric (not system-centric)? Y/N/partial
Study inclusion
The protocol followed consisted of the main steps as described below. The process was carried out using Google spreadsheets and is available at the following link: https://bit.ly/3eKhD3a
-
1.
The search was conducted by the first author (SMP) in the selected databases and using the query strings previously described. All the results were collected in.csv format including title, abstract, authors, publication year, publication venue, etc.
-
2.
The inclusion criteria were then applied by (SMP) to the downloaded list of candidate papers. In those cases where the title and abstract were not sufficient to make a decision, both authors (SMP) and (FjGP) assessed independently the entire content of the paper and discussed its inclusion until a consensus was made. The resultant candidate papers were added to another sheet of the spreadsheet document.
-
3.
The papers were then read in detail and analyzed by (SMP) based on the quality assessment checklist, and the results were collected in another spreadsheet. Additionally, (FjGP) double screened a sample of the excluded papers in step 2. Those papers with an overall score lower than 6 were excluded from the synthesis. Those papers which were instances of the same work were also excluded. Also, (SMP) double-checked that papers with an score higher than 6 clearly met the review scope (i.e. paper describes a physical robot, the robot is employed for the education of professionals in health sciences, robot model is not system-centric), and created an additional spreadsheet entitled “Additionally excluded papers with reasons” for further reference (see https://bit.ly/3eKhD3a). Uncertainties and conflicts with respect to article selection were resolved by discussion between both authors (SMP) and (FjGP).
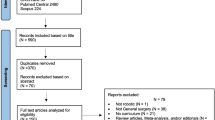
Following the above steps, the obtained results are shown in Figure 1 which is an adaptation of the PRISMA flow diagram (Moher et al., 2009) and maps out the number of records identified, included and excluded, and the final obtained papers.
Data extraction
A qualitative data analysis approach was followed to extract relevant data from the selected studies. The conducted process followed three major stages:
-
1.
Papers were first read in detail localizing chunks of text related to each research question and were highlighted for further analysis.
-
2.
Pattern labels to assign symbolic meaning to the highlighted information were created. Related patterns were grouped to find, extract, and categorize the segments relating to a particular research question.
-
3.
A second in depth read of the text was performed and data was retrieved and stored in a spreadsheet (https://bit.ly/3eKhD3a) following the coding created during stage 2.
The following data extraction groups and labels were created by (SMP) and (FjGP) for each research question:
Related to research question 1: How are robotics considered in the health sciences education literature beyond surgical robots and the manipulation of robotic instruments? To answer this question, we considered the robot goal (a general description of the robotic construction); the skills objective of training; the related health sciences field and the target group of health professionals. It has to be noted that, while the health sciences field is easily inferable, because there are countless professional roles in the health sciences, the intent of the target group was to be all inclusive rather than providing specific professional roles.
Related to research question 2: How are robotics integrated into the teaching/learning of health sciences? To answer this second question, we followed the work of (Jörg et al., 2013) related to the use of technology in medical education. We considered three types of training goals (prevention, diagnosis, or treatment); as another category, we labelled the studies that focused on modelling a health procedure as application-centric, and as patient-centric studies those that focused on modelling the patient; furthermore, application-centric models could be related to a concrete task or a complete procedure. In addition, we divided patient-centric studies into general approaches that model the anatomical or physiological properties of the human body, or case-specific if they also incorporate the restrictive parameters caused by a disease or impairment. To extract this information, we sticked to the objectives indicated by the authors even though additional modelling categories and applications could be inferred from the possibilities of the robots developed.
Related to research question 3: Are there documented added-value benefits of the use of robotics against other approaches? We considered whether the teaching/learning process was described in the paper, and if the acceptance of trainees was collected (e.g. questionnaires, discussion groups, etc.). Complementary, and similar to other approaches aiming to investigate the effects of the use of technology in medical education (van Gaalen et al., 2021), we used the framework proposed by Cook et al. (2008) for the classification of the teaching/learning process evaluation. The framework allows to classify the studies as descriptive, justificative and clarificatory. Descriptive studies focus on observation and describe what has been done without making any comparison. Justificative studies make comparisons between interventions, but without a proper conceptual framework which explains the observed effects. Clarificatory studies apply a theoretical background to explain the effects and differences of the interventions and make a clear statement of the future lines of research based on the observed effects.
Results
Results of the extracted data are summarized in “Appendix 2”.
Robot description
Most of the robots used as didactic tools in the studies (n = 22) are robotic instances of what are known as human patient simulators (HPS), differing in the body part they simulate (see”Appendix 2″ for a detailed description). From these, many replicate just extremity joints such as the upper limb (e.g. (Lee et al., 2020a, b)) or the hip and knee (Frey et al., 2006). However, some studies like (Frey et al., 2006) complement the robotic construction with a non-actuated human mannequin to resemble the rest of the human body, and other multimodal feedback channels such as screens or voice synthesis. A variant of these approaches are wearable robots used as impairment simulator of the knee joint (Ishikawa et al., 2015) and ankle + feet (Okumura et al., 2013). In addition, four studies present a robot that resembles the whole human body (e.g. (Lin et al., 2020)) with a varying number of DOFs in each body joint depending on their goal. In (Chihara et al., 2013) and (Moosaei et al., 2017) they present human-like robotic heads, able to simulate the muscle movements of the human face. The number of degrees of freedom (DOFs) simulated in all these robotic constructions is variable, but in general they match the ones of the human joint they simulate.
Organ simulation robots are described in four studies, where the robotic construction models different physiological properties. Usually, these robotic constructions are combined with phantom materials that provide the anatomical resemblance (Formosa et al., 2018).
Finally, two studies (Couto et al., 2017; Sampsel et al., 2014) employ humanoid robotic mobile platforms (with displacement capability), and in (Hong et al., 2019) the robot simulates a hands-on process, in which the pre-recorded movements of an experienced surgeon are transferred to the trainee.
Teaching/training goals
Teaching and training goals are mostly related to treatment training robots. Of these, six focus on manual rehabilitation of extremity joints. Other treatments include dental procedures, cardiopulmonary resuscitation (CPR), radiosurgery, mechanical ventilation, and surgery.
Diagnosis is the training goal of twelve studies. Again, half (n = 6) of those studies focus on the manual examination and diagnosis of extremities. Other studies aimed at training diagnostic skills include endoscopy training as in (Pepley et al., 2016) and colonoscopy training as in (Formosa et al., 2018). Finally, one paper (Moosaei et al., 2017) focuses on enhancing the skills to detect pain in facial expressions.
Fewer studies are focused on prevention. These include (Lin et al., 2020) which aims to prevent harming the patient during transfer to and from wheelchairs; (Couto et al., 2017) focused on the education of health professionals in hand hygiene practices, and (Lee et al., 2020a, b) focused on the prevention of upper-limb joint pain in the elderly by means of exercises. In addition, the goals of (Pepley et al., 2016) and (Formosa et al., 2018) include the early detection and prevention of diseases.
Target groups & health sciences field
Studies target groups correspond to the nature of the robot and the training goals. As such, eleven studies lay in the province of physiotherapy and are oriented to physical therapy related students or practitioners, nine studies are focused on nursery skills development and two relate to dentists and dental assistants. Other specialties include gastroenterologists (Formosa et al., 2018), neurologists (Chihara et al., 2013), and surgeons (Hong et al., 2019). However, while in most cases the health sciences field and related specialty is described by the authors or can be easily inferred, few studies (e.g. (Swain, 2017) for nurse students or (Horvath et al., 2020) for intensive care unit interns) make an explicit distinction regarding the adequate level of knowledge of the target group (e.g. student vs intern vs resident vs fellow vs attending).
Modelling category and level
Nine studies are purely patient centric. From these, eight simulate one or more case specific functional impairments of body joints (e.g. muscle spasticity (Othman et al., 2018), lead-pipe rigidity (Ishikawa et al., 2015) or limitation of motion range (Lee et al., 2020a, b)).
Only application—centric models can be found in eleven studies. Modelled procedures range from tele-rounding in ICUs (Sampsel et al., 2014) to correct transfer of patients to and from wheelchairs (Lin et al., 2020) or protocol when epileptic seizure (Zubrycki et al., 2019). Examples of modelled basic tasks are detect pain in facial expressions (Moosaei et al., 2017) or hand hygiene (Couto et al., 2017).
The rest of the studies include both modelling the patient / symptomatology and the associated procedure, e.g. in (Takanobu et al., 2007), where a human-like dental robot simulator models full body joint movements, facial expressions, eye tracking, mouth movements, and vomiting reflex and blood effusion during teeth drilling. In addition, the robot is remotely controlled by a supervisor to model diverse dental procedures.
Research type & evaluation method
Overall, almost half (n = 11) of the studies are descriptive and analyze the benefits of the robotic didactic tool by means of expert assessment or comparing its performance against data obtained from patients’ databases. Eleven studies are justificative, and interventions are composed by students/trainees vs. experts, laypersons vs. experts, between experts, and between students. Evaluation methods are commonly based on questionnaires or analyzing differences in parameterized data captured by the robotic platform. Other evaluation methods include the comparison of stroke patients ability to move an impaired hand before and after following a 60 days recovery program with a robotic intervention (Sharifi et al., 2016) and discussion groups (Swain, 2017). It must be noted that, although proposing a justificative approach, some studies do not specify the number of participants in each intervention (Couto et al., 2017). In fact, only four clarificatory studies were found (Moosaei et al., 2017; Sampsel et al., 2014; Swain, 2017; Wang et al., 2015).
Teaching/learning process
Even though all studies clearly stated the educational goal of the proposed robotic platform, only nine studies describe in greater or lesser detail the teaching/learning process (e.g., teaching methodology, environment configuration, whether the practitioner/student needs directions, if the robot needs to be remotely operated, etc.).
Within those studies that do not describe the educational approach, we can consider Fleming & Mills VARK model (Fleming & Mills, 1992) to infer the learning process based on the robot goal. Therefore, kinesthetic learning can be inferred in most of studies that do not detail the learning methodology but develop human joint robotic simulators, as robots are referred to as didactic tools for manual diagnosis or treatment (e.g. (Kong et al., 2021) or (Lee et al., 2020a, b)). Also, a hands-on learning is inferred from (Formosa et al., 2018) and (Pepley et al., 2016), as the robot goal is to simulate the environmental conditions faced when performing a colonoscopy or endoscopy, such as physiological properties or disturbances from patient movement. The same considerations can be extracted from (Zhou et al., 2004) and (Horvath et al., 2020), where the robots are respiratory motion simulators for performing radiosurgery and for correctly applying mechanical ventilators respectively.
On the other hand, visual learning is expected in (Chihara et al., 2013), where an expressive robotic head emulates the facial nervous system when performing facial expressions. The student is expected to gain skills in the diagnosis of cranial neuropathies through the visual examination of facial symptoms. The same approach appears in (Moosaei et al., 2017), where a robotic head simulates pain expressions to be recognized by the learner.
In (Hong et al., 2019) a hand-over-hand educational approach is proposed as an enhancement to passive haptic feedback simulators commonly employed in surgery education. Haptic feedback is given to the trainees based on the recordings of movements made by a specialized surgeon during surgery tasks. During training, the robot goes together with the trainee’s hand and applies slight forces that simulate hand-over-hand guidance. A similar approach is shown in (Sharifi et al., 2016), where authors propose an additional variant based on a network-connected multiagent system for hemiparetic wrist of stroke patients’ rehabilitation. Here the guiding force feedback can be averaged over a network of interconnected wrist rehabilitation devices, allowing different configurations with one or more instructors or patients in the robotic network.
Visual and auditory learning are employed in (Couto et al., 2017), where the Robot performs video lectures, encouraging speeches and examples for the education of intensive care unit worker professionals in hand hygiene practices. Also, in (Zubrycki et al., 2019) the robot is shown simulating an epilepsy seizure during educational workshops on epilepsy.
Robotic platforms are also employed either autonomously or remotely operated as the pathway to deliver the learning content and guide the educational process. For instance, in (Sampsel et al., 2014) instructor assists trainees in ICU tele-rounding through the use of a remotely controlled mobile robotic platform that accompanies them. In (Takanobu et al., 2007) and (Abe et al., 2018) the instructor evaluates the performance of dental students giving instructions to the patient robot via a PC interface, simulating a real study case through voice synthesis and patient behavior.
In (Lin et al., 2020) the robot autonomously guides and evaluates the learning process. By following a predefined checklist of steps for patient transfer procedures, voice commands and limb posture of the robotic patient can be used by nurses and students and to identify the steps to be executed during training. Meanwhile, the robot records its movements to provide feedback of the correctness of the procedure.
Robot acceptance
A small number of studies consider the acceptance of robots by the users. User acceptance is compiled by using questionnaires that include the acceptance of the technology (e.g. (Abe et al., 2018)), by qualitative description of observed effects (Couto et al., 2017) or by using discussion groups (Swain, 2017; Zubrycki et al., 2019). As extracted from the results, the overall acceptance by the participants is good, as the health students and professionals perceive them as useful tools for learning.
Discussion
To the best of the authors' knowledge, there is scarce literature focused on describing the factors affecting teaching–learning in health sciences education, apart from those focused-on training in the use of surgeon robots or surgeon robotic simulators. Given that robots are technological tools, we can follow a similar approach of other works that involve the use of technology to improve educational processes to analyze the obtained data. A recent systematic review on the factors affecting e-learning in health sciences education (Regmi & Jones, 2020) indicates as factor enablers: facilitate learning, learning in practice, systematic approach to learning and the integration of e-learning into curricula. As for factor barriers: poor motivation and expectation, resource-intensive, not suitable for all disciplines/contents and lack of its skills. Similar enablers and barriers can be transposed to robotic technology in the discussion of the results found.
In terms of the enablers observed in our survey that coincide with those obtained by Regmi & Jones the following can be depicted:
Robots facilitate learning and quality assurance. Overall, results obtained from the analyzed papers seem to support this statement. For example, the results shown in (Sampsel et al., 2014), which studies the use of a remote telepresence robotic system in nursing education show that from 69 total respondents including faculty staff, clinical staff and 56 students, the majority (75%) felt that the robot was a good teaching/learning tool. In (Swain, 2017), they divided into two groups: one received training in CPR with and without the robotic simulator. Mixed methods (questionnaires and discussion groups were employed to determine if subjects were more comfortable in clinical setting after unexpected event using a robotic human patient simulator. Their results show that the robot helps transferring deeper tacit knowledge through experience and provide more effective training than explicit procedural learning.
Robots foster learning in practice. it can be seen from the analyzed studies that most of the work focus on kinesthetic learning, utilizing robots as hands-on practice didactic tools. Kinesthetic learning has long proven to be useful in medical training, for example in anatomy learning (Hernandez et al., 2020), as it provides four different effective learning modes: concrete experience, reflective observation, abstract conceptualization, and active experimentation (Kolb, 1983). In several of the works analyzed that describe users' judgement, there is a common opinion that robots are useful for learning in practice, as robots can faithfully reproduce real symptoms and simulate illness effects.
Robots allow a systematic approach to learning. The fact that robots allow to parameterize symptoms and reproduce them in a systematic way means that trainees can reliably repeat the same training, both in terms of patient-centric and procedure-centric approaches (e.g. (Lin et al., 2020)). Moreover, robots allow the inclusion of real patient data to emulate the physiological implications of a disease such as its severity in a systematic way (e.g. (Zakaria et al., 2014)).
As for the coinciding observed barriers, they include the following:
Poor motivation and expectation. Contrary to the results shown by (Regmi & Jones, 2020) in terms of e-learning, the use of other technology enhanced learning (TEL) in the health sciences field has proven to enrich and facilitate the transmission of didactic content, favoring medical training and motivating the students for example by using virtual or augmented reality (Escalada-Hernández et al., 2019; González Izard et al., 2020; Izard et al., 2018). However, when using robotic technology, the users’ attitudes towards robots is a major concern, as robotic appearance and behavior influences and hinders their acceptance, especially when these robots resemble human beings (Müller et al., 2020; Savela et al., 2018). This important aspect of robotic technology is considered in few of the compiled studies. Further acceptance—focused research needs to be done to consider them as motivating, given that the questionnaires of the reviewed studies bias towards robot utility in pilot studies, and little towards user acceptance and long-term usage.
Robots may not be suitable for all disciplines/contents. This barrier can be inferred by the number of studies that coincide in the same health sciences field and robotic goals. It can be observed that most studies focus on diagnosis and treatment, while few focus on prevention. In addition, there is a dominant number of robots focused on modelling and simulating upper or lower limbs for physicians training. These results may come from the fact that traditionally robots have been built as industrial robotic arms as heavy objects manipulators to grasp and move objects in industrial environments. As such, most of the research done by robotic developers has focused on the study of the kinematic chain of robotic arms, which can be translated into the movement of joints present in human limbs.
Robots are resource intensive. Most of the studies in this systematic review use ad-hoc robotic constructions, which means that both their development process and their use and maintenance require specialized personnel. However, given the increasing development of commercial robotic platforms, the trend should be towards commercialization of specialized robotic constructions, with the consequent reduction in the cost of operation and maintenance. This evolution has already been observed both in surgical robots and in low-cost haptic simulators for training with these robots (Ginoya et al., 2021). There are some examples of using commercial components in the retrieved studies that diminish the development needed resources. For instance in (Couto et al., 2017) the low-cost humanoid robot MeccaNoid G15KS (Meccano Engineering & Robotics, n.d.) is employed. Or in (Sampsel et al., 2014), where a mobile platform is used endowed with the InTouch Health commercial software (Intouchhealth, n.d.).
The use of robots requires IT skills. Following the above discussion, ad-hoc constructions lead to the need for IT experts to manage them, which results in robots that do not evolve from piloted laboratory tests as is the case in most of the studies found. Even using commercial software, the need of IT skills is shown when evaluating the educational process (e.g. (Sampsel et al., 2014)).
Integration of robot-mediated learning into curricula. It is precisely in terms of integrating the activity developed with the robot into the training curricula that we observe the greatest hindering factor. This makes one of the enablers for health sciences e-learning described in (Regmi & Jones, 2020), to become a barrier when using robots. Contrary to what is happening in the field of robotic surgery, where there is a trend towards standardized validated curricula (Forgione & Guraya, 2017; Chen et al., 2020a, b; Khalafallah et al., 2020), the use of robots in other health sciences fields seems to be far from standardized. The above-described barriers appear to be some of the causes for this delay. In addition, and maybe since the analyzed works are commonly developed by roboticists, it has been observed in most of the studies a lack of educational approach. For example, the training methodology is scarcely described nor is the target group specifically detailed. Even more, few studies make an explicit distinction regarding the adequate level of knowledge of the target group (e.g., student vs intern vs resident vs fellow vs attending). Our results seem consistent with those reported by (Nicoll et al., 2018), where they performed a systematic review of the literature relating to the evaluation of technology enhanced learning (TEL) programs for professionals in health sciences. As they described in their work, there continues to be a need to develop effective and standard TEL evaluation tools, and good quality studies that describe effective evaluation of TEL education for professionals in health sciences. Studies often fail to provide sufficient detail to support transferability or direct future TEL health care education programs.
Educational theories and learning processes that may facilitate the incorporation of robots in the teaching/learning process
As extracted from the previous discussion, different types of robots have different appearances and structures (hardware), software, and behavior. These features play an important role in determining the instructional activities and the learning objectives (Ferrada-Ferrada et al., 2020; Herrero, 2020). As these technological tools are usually developed from a roboticist perspective, they lack a common approach for their inclusion in the health sciences teaching/learning process. Applying well-established educational theories and learning processes could help overcoming the observed barriers.
In classical conditioning, for instance, a response to a stimulus is reinforced when it is followed by a positive reward effect. In this sense, major efforts should be put in endowing robots with user-friendly interfaces and interaction modalities (Camargo et al., 2021). On top of that, we observed few studies that considered user acceptance. Acceptance of robots by the users (students and teachers) should be further explored during and after robotic development, so to better adapt their design to users’ expectations. Also, in classical conditioning a response to a stimulus will become stronger through exercise and repetition. This is provided by robots as they allow repetition of the same procedure. However, besides repeating general procedures or mimicking a joint movement, it may be important to endow robots with more "case-specific" capabilities, that foster problem-based learning by consistently simulating specific symptomatology of real patients as students will encounter when they practice.
Standardization of procedures when developing robots can reduce differences in their appearance and behavior. Following Ausubel's theory, using already developed and tested robotic components (e.g., using software already present in pcs) can help in reducing the need for IT skills, as learners will absorb new information by tying it to their existing knowledge. Also, employing user centered design principles and multimodal interaction that include human communication channels (i.e., voice or sound) can mitigate this barrier.
The use of robots beyond patient simulators should be promoted. For instance, fostering shadow learning as shown in (Sampsel et al., 2014), where they employ a mobile telepresence robotic system during nursing rounding. Results revealed that usefulness emerged in the areas of productivity, function, and observation, as participants felt that the robot facilitates course quality assurance when the lead faculty is not on site, and productivity was associated to the ability of the lead faculty to multitask.
In relation to the above and considering Bandura’s social learning theory, it has been long demonstrated that prosocial robots elicit more prosocial behavior among users. Studies suggest that social responsive machines increase de acceptance of users towards them, as the feeling of affinity towards the machine reduces negative perceptual feedback. However, special care must be taken when developing a social robot, so to avoid falling into the uncanny valley if the user perceives a mismatch between robot’s appearance and behavior (Cheetham, 2017). Moreover, cultural, age and gender differences should be taken into account when employing robots in health sciences education (for example, eastern cultures often rate lower levels of the uncanny valley than western cultures (Korn et al., 2021). Again, following user centered design principles and further analyzing the acceptance of robots by the users during the design process could help mitigating this effect.
From the above discussion, the case of (Lee et al., 2020a, b) is an example of how the development process for this type of robots should be approached. Instances of the same work (Murata et al., 2017; Lee et al., 2019a, 2019b; 2020b) show how the focus evolves from the mere robot design to the development of the control interface and automatic data capture and feedback that eases both the manipulation of the robot and a self-learning approach for students.
Limitations
As with any research procedure, there could be threats to its validity and limitations in the current systematic review. The first threat is that the inclusion of all the relevant studies in the field is not guaranteed. This threat was mitigated by piloting different searches, analyzing the retrieved results, and combining different databases. However, as can be depicted from the results, the number of papers that have reached the final stage after applying the quality criteria is quite low if compared with the number of papers retrieved from the search. To the best of the authors’ knowledge, one of the main reasons is that the research field of robotic technology in the education of health professionals is not a consolidated field beyond surgery education, so scarce information can be retrieved. For that reason, the search scope was broadened to capture as much information as possible within the limits of the established review scope, and a methodology for screening has been followed. Another limitation arises by employing only the retrieved abstract for screening. As the abstracts of publications contain way less information than is contained in the full paper, this could lead to a bias in the search results.
Another limitation is that due to the scope of the studies that merge different fields (education, health, and robotics), most of the papers do not provide detailed descriptions for all the research questions. In addition, the identification of criteria for classification was not obvious in many cases, as many papers contained vague or fuzzy descriptions of the data to be extracted. For example, in terms of application-centric and system-centric robots there is a thin line in between determining if a robot is used to teach a procedure or if it is a system used to train the skills to handle a robotic tool. Furthermore, the boundary between what is and what is not a robot is a delicate one. To mitigate these effects, we tried to keep the review scope as concrete as possible, only considering robots those constructions that clearly showed together sensing, computing and acting capabilities with more or less degree of autonomy as described by the IEEE (What Is a Robot?, n.d.). The abovementioned threads were also mitigated by following a review protocol that involved both authors and tried to assure the quality of the obtained studies. Additionally, both researchers independently reviewed full texts during the process and discussed jointly to resolve uncertainties and reach consensus when necessary.
Finally, it must be noted that due to the review scope many papers devoted to surgery robots and haptic simulators have been discounted from the final review. In any case, given that there are several studies and surveys dedicated to the training of robots in surgery as well as to the study of haptic interfaces, the authors consider that this survey can be complementary to those studies.
Conclusion
This systematic review provides a broad overview of how robotics is integrated and considered in the health sciences education literature, beyond well-established surgical robots and system-centric approaches, by scoping the enablers and barriers that affect the use of robots as didactic tools for the education of professionals in health sciences.
Results show that, although there exist documented added-value benefits of the use of robots as didactic tools in medical education, further research on the issues found needs to be done to foster their inclusion in the curricula of health sciences professionals. On the one hand, by analyzing how robotic technology should be developed to become more flexible and usable to support both teaching and learning processes in health sciences education, as final users are not necessarily well-versed in how to use it. On the other, there continues to be a need to develop effective and standard robotic enhanced learning evaluation tools, as well good quality studies that describe effective evaluation of robotic enhanced education for professionals in health sciences. As happens with other technologies when applied to the health sciences field, studies often fail to provide sufficient detail to support transferability or direct future robotic health care education programs.
If robots in health sciences education are developed with a roboticist mindset, without clearly incorporating aspects of the learning process beyond development, they may remain as proofs of concept. Incorporating elements of learning may promote the potential for robots to improve parameterizing of results, autonomously guide learners to achieve greater engagement, and allow collective (multi-agent) learning including patients and instructors "in the loop".
References
Abe, S., Noguchi, N., Matsuka, Y., Shinohara, C., Kimura, T., Oka, K., Okura, K., Rodis, O. M. M., & Kawano, F. (2018). Educational effects using a robot patient simulation system for development of clinical attitude. European Journal of Dental Education: Official Journal of the Association for Dental Education in Europe, 22(3), e327–e336. https://doi.org/10.1111/eje.12298
Alias, N. A., Huq, M. S., Ibrahim, B. S. K. K., & Omar, R. (2017). The efficacy of state of the art overground gait rehabilitation robotics: A bird’s eye view. Procedia Computer Science, 105, 365–370. https://doi.org/10.1016/j.procs.2017.01.235
Altok, M., Achim, M. F., Matin, S. F., Pettaway, C. A., Chapin, B. F., & Davis, J. W. (2018). A decade of robot-assisted radical prostatectomy training: Time-based metrics and qualitative grading for fellows and residents. Urologic Oncology, 36(1), 13.e19-13.e25. https://doi.org/10.1016/j.urolonc.2017.08.028
Azadi, S., Green, I. C., Arnold, A., Truong, M., Potts, J., & Martino, M. A. (2021). Robotic surgery: The impact of simulation and other innovative platforms on performance and training. Journal of Minimally Invasive Gynecology, 28(3), 490–495. https://doi.org/10.1016/j.jmig.2020.12.001
Badash, I., Burtt, K., Solorzano, C. A., & Carey, J. N. (2016). Innovations in surgery simulation: A review of past, current and future techniques. Annals of Translational Medicine, 4(23), 453. https://doi.org/10.21037/atm.2016.12.24
Bai, S., Gurvinder, S., & V., & Thomas G. S. (2018). Wearable Exoskeleton systems: Design, control and applications. IET Digital Library. https://doi.org/10.1049/PBCE108E
Blanson Henkemans, O. A., Bierman, B. P. B., Janssen, J., Neerincx, M. A., Looije, R., van der Bosch, H., & van der Giessen, J. A. M. (2013). Using a robot to personalise health education for children with diabetes type 1: A pilot study. Patient Education and Counseling, 92(2), 174–181. https://doi.org/10.1016/j.pec.2013.04.012
Bonatti, J., Wallner, S., Crailsheim, I., Grabenwöger, M., & Winkler, B. (2021). Minimally invasive and robotic coronary artery bypass grafting—A 25-year review. Journal of Thoracic Disease, 13(3), 1922–1944. https://doi.org/10.21037/jtd-20-1535
Boubaker, O. (2020). Chapter 7—Medical robotics. In O. Boubaker (Ed.), Control Theory in Biomedical Engineering (pp. 153–204). Academic Press. https://doi.org/10.1016/B978-0-12-821350-6.00007-X
Camargo, C., Gonçalves, J., Conde, M. Á., Rodríguez-Sedano, F. J., Costa, P., & García-Peñalvo, F. J. (2021). Systematic literature review of realistic simulators applied in educational robotics context. Sensors, 21(12), 4031. https://doi.org/10.3390/s21124031
Cheetham, M. (2017). Editorial: The uncanny valley hypothesis and beyond. Frontiers in Psychology. https://doi.org/10.3389/fpsyg.2017.01738
Chen, I.-H.A., Ghazi, A., Sridhar, A., Stoyanov, D., Slack, M., Kelly, J. D., & Collins, J. W. (2020a). Evolving robotic surgery training and improving patient safety, with the integration of novel technologies. World Journal of Urology. https://doi.org/10.1007/s00345-020-03467-7
Chen, L.W.-Y., Goh, M., Goh, R., Chao, Y.-K., Huang, J.-J., Kuo, W.-L., Sung, C.W.-H., Lu, J.C.-Y., Chuang, D.C.-C., & Chang, T.N.-J. (2021). Robotic-assisted peripheral nerve surgery: A systematic review. Journal of Reconstructive Microsurgery. https://doi.org/10.1055/s-0040-1722183
Chen, R., Rodrigues Armijo, P., Krause, C., Robotic Task Force, S. A. G. E. S., Siu, K.-C., & Oleynikov, D. (2020b). A comprehensive review of robotic surgery curriculum and training for residents, fellows, and postgraduate surgical education. Surgical Endoscopy, 34(1), 361–367. https://doi.org/10.1007/s00464-019-06775-1
Chihara, T., Wang, C., Niibori, A., Oishio, T., Matsuoka, Y., Sessa, S., Ishii, H., Nakae, Y., Matsuoka, N., Takayama, T., & Takanishi, A. (2013). Development of a head robot with facial expression for training on neurological disorders. IEEE International Conference on Robotics and Biomimetics (ROBIO), 2013, 1384–1389. https://doi.org/10.1109/ROBIO.2013.6739659
Cianchetti, M., Laschi, C., Menciassi, A., & Dario, P. (2018). Biomedical applications of soft robotics. Nature Reviews Materials, 3(6), 143–153. https://doi.org/10.1038/s41578-018-0022-y
Ciullo, A. S., Veerbeek, J. M., Temperli, E., Luft, A. R., Tonis, F. J., Haarman, C. J. W., Ajoudani, A., Catalano, M. G., Held, J. P. O., & Bicchi, A. (2020). A novel soft robotic supernumerary hand for severely affected stroke patients. Ieee Transactions on Neural Systems and Rehabilitation Engineering, 28(5), 1168–1177. https://doi.org/10.1109/TNSRE.2020.2984717
Collins, J. W., & Wisz, P. (2020). Training in robotic surgery, replicating the airline industry. How far have we come? World Journal of Urology, 38(7), 1645–1651. https://doi.org/10.1007/s00345-019-02976-4
Cook, D. A., Bordage, G., & Schmidt, H. G. (2008). Description, justification and clarification: A framework for classifying the purposes of research in medical education. Medical Education, 42(2), 128–133. https://doi.org/10.1111/j.1365-2923.2007.02974.x
Cooper, J., & Taqueti, V. (2004). A brief history of the development of mannequin simulators for clinical education and training. Quality & Safety in Health Care, 13(Suppl 1), i11–i18. https://doi.org/10.1136/qshc.2004.009886
Couto, B. R. G., Alvim, A., Silva, I. L. A. da, Horta, M., Júnior, J. J. da C., & Starling, C. (2017). Using Ozires, a Humanoid Robot, to Continuing Education of Healthcare Workers: A Pilot Study. International Conference on Computer Supported Education. International Conference on Computer Supported Education. https://doi.org/10.5220/0006312302930299
Cz, N. A., Komeda, T., & Low, C. Y. (2012). Design of upper limb patient simulator. Procedia Engineering, 41, 1374–1378. https://doi.org/10.1016/j.proeng.2012.07.324
Díaz, C. E., Fernández, R., Armada, M., & García, F. (2017). A research review on clinical needs, technical requirements, and normativity in the design of surgical robots. The International Journal of Medical Robotics + Computer Assisted Surgery: MRCAS, 13(4). https://doi.org/10.1002/rcs.1801
Eckert, M., Volmerg, J. S., & Friedrich, C. M. (2019). Augmented reality in medicine: Systematic and bibliographic review. Jmir Mhealth and Uhealth, 7(4), e10967. https://doi.org/10.2196/10967
Escalada-Hernández, P., Soto Ruiz, N., & San Martín-Rodríguez, L. (2019). Design and evaluation of a prototype of augmented reality applied to medical devices. International Journal of Medical Informatics, 128, 87–92. https://doi.org/10.1016/j.ijmedinf.2019.05.004
Ferrada-Ferrada, C., Carrillo-Rosúa, J., Díaz-Levicoy, D., & Silva Díaz, F. (2020). Robotics from stem areas in primary school: A systematic review. https://doi.org/10.14201/eks.22036
Fleming, N. D., & Mills, C. (1992). Not another inventory, rather a catalyst for reflection. To Improve the Academy, 11(1), 137–155. https://doi.org/10.1002/j.2334-4822.1992.tb00213.x
Fontanelli, G., Selvaggio, M., Ferro, M., Ficuciello, F., Vendittelli, M., & Siciliano, B. (2019). Portable dVRK: An augmented V-REP simulator of the da Vinci Research Kit. https://doi.org/10.12700/aph.16.8.2019.8.6
Forgione, A., & Guraya, S. Y. (2017). The cutting-edge training modalities and educational platforms for accredited surgical training: A systematic review. Journal of Research in Medical Sciences: THe Official Journal of Isfahan University of Medical Sciences, 22, 51. https://doi.org/10.4103/jrms.JRMS_809_16
Formosa, G. A., Prendergast, J. M., Peng, J., Kirkpatrick, D., & Rentschler, M. E. (2018). A modular endoscopy simulation apparatus (MESA) for robotic medical device sensing and control validation. IEEE Robotics and Automation Letters, 3(4), 4054–4061. https://doi.org/10.1109/LRA.2018.2861015
Frey, M., Hoogen, J., Burgkart, R., & Riener, R. (2006). Physical interaction with a virtual knee joint—the 9 DOF haptic display of the munich knee joint simulator. Presence, 15(5), 570–587. https://doi.org/10.1162/pres.15.5.570
García-Holgado, A., Marcos-Pablos, S., & García-Peñalvo, F. (2020). Guidelines for performing Systematic Research Projects Reviews. International Journal of Interactive Multimedia and Artificial Intelligence, 6(Regular Issue). https://www.ijimai.org/journal/bibcite/reference/2778
García-Peñalvo, F. J., Corell, A., Abella-García, V., & Grande, M. (2020). La evaluación online en la educación superior en tiempos de la COVID-19. Education in the Knowledge Society (EKS), 21, 26–26. https://doi.org/10.14201/eks.23086
García-Peñalvo, F. J., Corell, A., Abella-García, V., & Grande-de-Prado, M. (2021). Recommendations for Mandatory Online Assessment in Higher Education During the COVID-19 Pandemic. In D. Burgos, A. Tlili, & A. Tabacco (Eds.), Radical Solutions for Education in a Crisis Context: COVID-19 as an Opportunity for Global Learning (pp. 85–98). Springer. https://doi.org/10.1007/978-981-15-7869-4_6
Giansanti, D. (2021). The social robot in rehabilitation and assistance: What Is the Future? Healthcare, 9(3), 244. https://doi.org/10.3390/healthcare9030244
Gifari, M. W., Naghibi, H., Stramigioli, S., & Abayazid, M. (2019). A review on recent advances in soft surgical robots for endoscopic applications. The International Journal of Medical Robotics + Computer Assisted Surgery: MRCAS, 15(5), e2010. https://doi.org/10.1002/rcs.2010
Ginoya, T., Maddahi, Y., & Zareinia, K. (2021). A historical review of medical robotic platforms. Journal of Robotics, 2021, e6640031. https://doi.org/10.1155/2021/6640031
Gochoo, M., Vogan, A. A., Khalid, S., & Alnajjar, F. (2020). AI and Robotics-Based Cognitive Training for Elderly: A Systematic Review. 2020 IEEE / ITU International Conference on Artificial Intelligence for Good (AI4G), 129–134. https://doi.org/10.1109/AI4G50087.2020.9311076
González Izard, S., Juanes Méndez, J. A., García-Peñalvo, F. J., & Moreno Belloso, C. (2020). App Design and Implementation for Learning Human Anatomy Through Virtual and Augmented Reality. In D. Burgos (Ed.), Radical Solutions and eLearning: Practical Innovations and Online Educational Technology (pp. 199–213). Springer. https://doi.org/10.1007/978-981-15-4952-6_13
Haji, Z., Arif, A., Jamal, S., & Ghafoor, R. (2021). Augmented reality in clinical dental training and education. JPMA. The Journal of the Pakistan Medical Association, 71(Suppl 1)(1), S42–S48.
Hakogi, H., Ohaba, M., Kuramochi, N., & Yano, H. (2005). Torque control of a rehabilitation teaching robot using magneto-rheological fluid clutches. JSME International Journal Series B Fluids and Thermal Engineering, 48(3), 501–507. https://doi.org/10.1299/jsmeb.48.501
Hernandez, J. E., Vasan, N., Huff, S., & Melovitz-Vasan, C. (2020). Learning styles/preferences among medical students: Kinesthetic learner’s multimodal approach to learning anatomy. Medical Science Educator, 30(4), 1633–1638. https://doi.org/10.1007/s40670-020-01049-1
Herrero, J. F. Á. (2020). Pensamiento computacional en Educación Infantil, más allá de los robots de suelo. Education in the Knowledge Society (EKS), 21, 11–11. https://doi.org/10.14201/eks.22366
Hong, K., Sun, Y., He, J., Lei, Y., & Yang, L. (2019). Preliminary design of a robotic system for kinaesthetic training of surgical tasks. The Journal of Engineering, 2019(14), 490–494. https://doi.org/10.1049/joe.2018.9405
Horvath, M. A., Hu, L., Mueller, T., Hochstein, J., Rosalia, L., Hibbert, K. A., Hardin, C. C., & Roche, E. T. (2020). An organosynthetic soft robotic respiratory simulator. APL Bioengineering, 4(2), 026108. https://doi.org/10.1063/1.5140760
Hughes, J., Maiolino, P., Nanayakkara, T., & Iida, F. (2020). Sensorized Phantom For Characterizing Large Area Deformation of Soft Bodies for Medical Applications. In 2020 3rd Ieee International Conference on Soft Robotics (robosoft) (pp. 278–284).
Intouchhealth. (n.d.). Retrieved April 29, 2021, from https://intouchhealth.com/virtual-care-platform
Ishikawa, S., Okamoto, S., Isogai, K., Akiyama, Y., Yanagihara, N., & Yamada, Y. (2015). Assessment of robotic patient simulators for training in manual physical therapy examination techniques. PLoS ONE, 10(4), e0126392. https://doi.org/10.1371/journal.pone.0126392
Izard, S. G., Juanes, J. A., García Peñalvo, F. J., Estella, J. M. G., Ledesma, M. J. S., & Ruisoto, P. (2018). Virtual reality as an educational and training tool for medicine. Journal of Medical Systems, 42(3), 50. https://doi.org/10.1007/s10916-018-0900-2
Jörg, S., Konietschke, R., & Klodmann, J. (2013). Classification of Modeling for Versatile Simulation Goals in Robotic Surgery. In S. Lee, K.-J. Yoon, & J. Lee (Eds.), Frontiers of Intelligent Autonomous Systems (pp. 357–368). Springer. https://doi.org/10.1007/978-3-642-35485-4_31
Kaan, H. L., & Ho, K. Y. (2020). Clinical adoption of robotics in endoscopy: Challenges and solutions. JGH Open, 4(5), 790–794. https://doi.org/10.1002/jgh3.12412
Kadakia, N., Malek, K., Lee, S. K., Lee, E. J., Burruss, S., Srikureja, D., Mukherjee, K., & Lum, S. S. (2020). Impact of robotic surgery on residency training for herniorrhaphy and cholecystectomy. The American Surgeon, 86(10), 1318–1323. https://doi.org/10.1177/0003134820964430
Khalafallah, Y. M., Bernaiche, T., Ranson, S., Liu, C., Collins, D. T., Dort, J., & Hafner, G. (2020). Residents’ views on the impact of robotic surgery on general surgery education. Journal of Surgical Education. https://doi.org/10.1016/j.jsurg.2020.10.003
Kitchenham, B., & Charters, S. (2007). Guidelines for performing Systematic Literature Reviews in Software Engineering (Technical Report EBSE-2007–01). Keele University. https://citeseerx.ist.psu.edu/viewdoc/citations;jsessionid=63DD20E0FE338672FE516A3853AA3628?doi=10.1.1.117.471
Kolb, D. A. (1983). Experiential Learning: Experience as the Source of Learning and Development (1st edition). Prentice Hall.
Kong, J., Kwon, Y., & Yi, H. (2021). Development of 6 DOF upper-limb patient simulator for hands-on rehabilitation education. IEEE Transactions on Network and Service Management. https://doi.org/10.1109/TNSM.2021.3053645
Korn, O., Akalin, N., & Gouveia, R. (2021). Understanding cultural preferences for social robots: A study in German and Arab Communities. ACM Transactions on Human-Robot Interaction, 10(2), 12:1–12:19. https://doi.org/10.1145/3439717
Kyrarini, M., Lygerakis, F., Rajavenkatanarayanan, A., Sevastopoulos, C., Nambiappan, H. R., Chaitanya, K. K., Babu, A. R., Mathew, J., & Makedon, F. (2021). A survey of robots in healthcare. Technologies, 9(1), 8. https://doi.org/10.3390/technologies9010008
Leal Ghezzi, T., & Campos Corleta, O. (2016). 30 years of robotic surgery. World Journal of Surgery, 40(10), 2550–2557. https://doi.org/10.1007/s00268-016-3543-9
Lee, M., Ameyama, K., Yamazoe, H., & Lee, J.-H. (2020a). Necessity and feasibility of care training assistant robot (CaTARo) as shoulder complex joint with multi-DOF in elderly care education. ROBOMECH Journal, 7(1), 12. https://doi.org/10.1186/s40648-020-00160-7
Lee, M., Murata, K., Ameyama, K., Yamazoe, H., & Lee, J.-H. (2019a). Development and quantitative assessment of an elbow joint robot for elderly care training. Intelligent Service Robotics, 12(4), 277–287. https://doi.org/10.1007/s11370-019-00282-x
Lee, M., Yamazoe, H., & Lee, J.-H. (2019b). Elderly care training using real-time monitoring system with care training assistant elbow robot (CaTARo-E). 2019b 16th International Conference on Ubiquitous Robots (UR), 259–264. https://doi.org/10.1109/URAI.2019b.8768793
Lee, M., Yamazoe, H., & Lee, J.-H. (2020b). Fuzzy-Logic based Care Training Quantitative Assessment using Care Training Assistant Robot (CaTARo). 2020b 17th International Conference on Ubiquitous Robots (UR), 602–607. https://doi.org/10.1109/UR49135.2020b.9144846
Lin, C., Ogata, T., Zhong, Z., Kanai-Pak, M., Maeda, J., Kitajima, Y., Nakamura, M., Kuwahara, N., & Ota, J. (2020). Development and validation of robot patient equipped with an inertial measurement unit and angular position sensors to evaluate transfer skills of nurses. International Journal of Social Robotics. https://doi.org/10.1007/s12369-020-00673-6
Louie, W.-Y. G., Korneder, J., Hijaz, A., & Sochanski, M. (2020). Investigating therapist vocal nonverbal behavior for applications in robot-mediated therapies for individuals diagnosed with autism. In A. R. Wagner, D. Feil-Seifer, K. S. Haring, S. Rossi, T. Williams, H. He, & S. Sam Ge (Eds.), Social robotics (pp. 416–427). Springer. https://doi.org/10.1007/978-3-030-62056-1_35
Lovegrove, C. E., Abe, T., Aydin, A., Veneziano, D., Sarica, K., Khan, M. S., Dasgupta, P., & Ahmed, K. (2017). Simulation training in upper tract endourology: Myth or reality? Minerva Urologica E Nefrologica = The Italian Journal of Urology and Nephrology, 69(6), 579–588. https://doi.org/10.23736/S0393-2249.17.02873-9
Maeda, Y., Hirano, T., Sato, N., Morita, Y., Ukai, H., Sanaka, K., Takao, K., & Satonaka, A. (2012). Development of knee joint robot for students becoming therapists—Development of training program for skill attainment in manual therapy techniques. 2012 12th International Conference on Control, Automation and Systems, 1573–1576.
Mapara, S. S., & Patravale, V. B. (2017). Medical capsule robots: A renaissance for diagnostics, drug delivery and surgical treatment. Journal of Controlled Release, 261, 337–351. https://doi.org/10.1016/j.jconrel.2017.07.005
Meccano Engineering & Robotics. (n.d.). Retrieved April 29, 2021, from http://www.meccano.com/meccanoid-about
Meng, Q., Meng, Q., Yu, H., & Wei, X. (2017). A survey on sEMG control strategies of wearable hand exoskeleton for rehabilitation. 2017 2nd Asia-Pacific Conference on Intelligent Robot Systems (ACIRS), 165–169. https://doi.org/10.1109/ACIRS.2017.7986086
Mohebbi, A. (2020). Human-robot interaction in rehabilitation and assistance: A review. Current Robotics Reports, 1(3), 131–144. https://doi.org/10.1007/s43154-020-00015-4
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. https://doi.org/10.1371/journal.pmed.1000097
Moosaei, M., Das, S. K., Popa, D. O., & Riek, L. D. (2017). Using Facially Expressive Robots to Calibrate Clinical Pain Perception. 2017 12th ACM/IEEE International Conference on Human-Robot Interaction (HRI, 32–41.
Müller, B. C. N., Gao, X., Nijssen, S. R. R., & Damen, T. G. E. (2020). I, Robot: How human appearance and mind attribution relate to the perceived danger of robots. International Journal of Social Robotics. https://doi.org/10.1007/s12369-020-00663-8
Murata, K., Yamazoe, H., Chung, M. G., & Lee, J.-H. (2017). Elderly care training robot for quantitative evaluation of care operation—Development of robotic elbow joint to imitate elderly people’s elbow. IEEE/SICE International Symposium on System Integration (SII), 2017, 1028–1033. https://doi.org/10.1109/SII.2017.8279358
Nguyen, K. T., Hoang, M. C., Choi, E., Kang, B., Park, J.-O., & Kim, C.-S. (2020). Medical microrobot—A drug delivery capsule endoscope with active locomotion and drug release mechanism: Proof of concept. International Journal of Control, Automation and Systems, 18(1), 65–75. https://doi.org/10.1007/s12555-019-0240-0
Nicoll, P., MacRury, S., van Woerden, H. C., & Smyth, K. (2018). Evaluation of technology-enhanced learning programs for health care professionals: systematic review. Journal of Medical Internet Research, 20(4), e131. https://doi.org/10.2196/jmir.9085
Okumura, H., Okamoto, S., Ishikawa, S., Akiyama, Y., Isogai, K., Hirano, Y., & Yamada, Y. (2013). Wearable dummy to simulate equinovarus for training of physical therapists. The SICE Annual Conference, 2013, 2272–2277.
Othman, N. A., Che Zakaria, N. A., & Mohd Ramli, M. H. (2018). PLC system to optimize training device of upper limb spasticity / Nurul Atiqah Othman [et al.]. Journal of Mechanical Engineering (JMechE), 15(2), 127–141.
Park, H.-S., Kim, J., & Damiano, D. L. (2012). Development of a Haptic Elbow Spasticity Simulator (HESS) for improving accuracy and reliability of clinical assessment of spasticity. IEEE Transactions on Neural Systems and Rehabilitation Engineering: A Publication of the IEEE Engineering in Medicine and Biology Society, 20(3), 361–370. https://doi.org/10.1109/TNSRE.2012.2195330
Pepley, D., Yovanoff, M., Mirkin, K., Han, D., Miller, S., & Moore, J. (2016, January 1). Design of a virtual reality haptic robotic central venous catheterization training simulator. 40th Mechanisms and Robotics Conference. ASME 2016 International Design Engineering Technical Conferences and Computers and Information in Engineering Conference, IDETC/CIE 2016. https://doi.org/10.1115/DETC2016-59560
Peters, B. S., Armijo, P. R., Krause, C., Choudhury, S. A., & Oleynikov, D. (2018). Review of emerging surgical robotic technology. Surgical Endoscopy, 32(4), 1636–1655. https://doi.org/10.1007/s00464-018-6079-2
Petersen, K., Vakkalanka, S., & Kuzniarz, L. (2015). Guidelines for conducting systematic mapping studies in software engineering: An update. Information and Software Technology, 64, 1–18. https://doi.org/10.1016/j.infsof.2015.03.007
Pu, L., Moyle, W., Jones, C., & Todorovic, M. (2020). The effect of using PARO for people living with dementia and chronic pain: A pilot randomized controlled trial. Journal of the American Medical Directors Association, 21(8), 1079–1085. https://doi.org/10.1016/j.jamda.2020.01.014
Regmi, K., & Jones, L. (2020). A systematic review of the factors – enablers and barriers – affecting e-learning in health sciences education. BMC Medical Education, 20(1), 91. https://doi.org/10.1186/s12909-020-02007-6
Rupal, B. S., Rafique, S., Singla, A., Singla, E., Isaksson, M., & Virk, G. S. (2017). Lower-limb exoskeletons: Research trends and regulatory guidelines in medical and non-medical applications. International Journal of Advanced Robotic Systems, 14(6), 1729881417743554. https://doi.org/10.1177/1729881417743554
Sampsel, D., Vermeersch, P., & Doarn, C. R. (2014). Utility and effectiveness of a remote telepresence robotic system in nursing education in a simulated care environment. Telemedicine Journal and E-Health: THe Official Journal of the American Telemedicine Association, 20(11), 1015–1020. https://doi.org/10.1089/tmj.2014.0038
Sarrica, M., Brondi, S., & Fortunati, L. (2019). How many facets does a “social robot” have? A review of scientific and popular definitions online. Information Technology & People, 33(1), 1–21. https://doi.org/10.1108/ITP-04-2018-0203
Savela, N., Turja, T., & Oksanen, A. (2018). Social Acceptance of robots in different occupational fields: A systematic literature review. International Journal of Social Robotics, 10(4), 493–502. https://doi.org/10.1007/s12369-017-0452-5
Sharifi, I., Talebi, H. A., & Motaharifar, M. (2016). A framework for simultaneous training and therapy in multilateral tele-rehabilitation. Computers & Electrical Engineering, 56, 700–714. https://doi.org/10.1016/j.compeleceng.2016.08.002
Sharma, A., & Bhardwaj, R. (2021). Robotic surgery in otolaryngology during the Covid-19 pandemic: A safer approach? Indian Journal of Otolaryngology and Head & Neck Surgery, 73(1), 120–123. https://doi.org/10.1007/s12070-020-02032-3
Sharma, R., Gordon, M., Dharamsi, S., & Gibbs, T. (2015). Systematic reviews in medical education: A practical approach: AMEE guide 94. Medical Teacher, 37(2), 108–124. https://doi.org/10.3109/0142159X.2014.970996
Simaan, N., Yasin, R. M., & Wang, L. (2018). Medical technologies and challenges of robot-assisted minimally invasive intervention and diagnostics. Annual Review of Control, Robotics, and Autonomous Systems, 1, 465–490.
Swain, D. E. (2017). Advanced human-computer interactions with a patient simulator: moving towards A smart campus and a learning health system. In Knowledge Discovery and Data Design Innovation: 14 (pp. 107–126). WORLD SCIENTIFIC. https://doi.org/10.1142/9789813234482_0006
Takanobu, H., Omata, A., Takahashi, F., Yokota, K., Suzuki, K., Miura, H., Madokoro, M., Miyazaki, Y., & Maki, K. (2007). Dental patient robot as a mechanical human simulator. IEEE International Conference on Mechatronics, 2007, 1–6. https://doi.org/10.1109/ICMECH.2007.4280065
Takeoka, T., Takiguchi, S., Uemura, M., Miyazaki, Y., Takahashi, T., Kurokawa, Y., Makino, T., Yamasaki, M., Mori, M., & Yuichiro Doki, A. (2017). Assessment potential of a new suture simulator in laparoscopic surgical skills training. Minimally Invasive Therapy & Allied Technologies: MITAT: Official Journal of the Society for Minimally Invasive Therapy, 26(6), 338–345. https://doi.org/10.1080/13645706.2017.1312456
Tavakoli, M., Carriere, J., & Torabi, A. (2020). Robotics, smart wearable technologies, and autonomous intelligent systems for healthcare during the COVID-19 pandemic: An analysis of the state of the art and future vision. Advanced Intelligent Systems, 2(7), 2000071. https://doi.org/10.1002/aisy.202000071
Troccaz, J., Dagnino, G., & Yang, G.-Z. (2019). Frontiers of medical robotics: From concept to systems to clinical translation. Annual Review of Biomedical Engineering, 21, 193–218. https://doi.org/10.1146/annurev-bioeng-060418-052502
van Gaalen, A. E. J., Brouwer, J., Schönrock-Adema, J., Bouwkamp-Timmer, T., Jaarsma, A. D. C., & Georgiadis, J. R. (2021). Gamification of health professions education: A systematic review. Advances in Health Sciences Education, 26(2), 683–711. https://doi.org/10.1007/s10459-020-10000-3
Wallace, D., Gillett, B., Wright, B., Stetz, J., & Arquilla, B. (2010). Randomized controlled trial of high fidelity patient simulators compared to actor patients in a pandemic influenza drill scenario. Resuscitation, 81(7), 872–876. https://doi.org/10.1016/j.resuscitation.2010.02.026
Wang, C., Duan, L., Li, M., Lu, Z., Shen, Y., Wei, J., Shi, Q., Wang, Y., Zecca, M., Li, W., & Wu, Z. (2015). Development an arm robot to simulate the lead-pipe rigidity for medical education. IEEE International Conference on Information and Automation, 2015, 619–624. https://doi.org/10.1109/ICInfA.2015.7279361
What Is a Robot? - ROBOTS: Your Guide to the World of Robotics. (n.d.). Retrieved April 28, 2021, from https://robots.ieee.org/learn/what-is-a-robot/
Zakaria, N. A., & Binti C., Komeda, T., Yee Low, C., & Inoue, K. (2014). Emulating upper limb disorder for therapy education. International Journal of Advanced Robotic Systems, 11(11), 183. https://doi.org/10.5772/58893
Zhou, T., Tang, J., Dieterich, S., & Cleary, K. (2004). A robotic 3-D motion simulator for enhanced accuracy in CyberKnife stereotactic radiosurgery. International Congress Series, 1268, 323–328. https://doi.org/10.1016/j.ics.2004.03.296
Zhu, J., & Liu, W. (2020). A tale of two databases: The use of Web of Science and Scopus in academic papers. Scientometrics, 123(1), 321–335. https://doi.org/10.1007/s11192-020-03387-8
Zubrycki, I., Szafarczyk, I., & Granosik, G. (2019). Participatory design of a robot for demonstrating an epileptic seizure. Advanced Robotics, 33(7–8), 338–349. https://doi.org/10.1080/01691864.2019.1601597
Acknowledgements
This research was partially funded by the Spanish Government Ministry of Science and Innovation through the AVisSA project grant number (PID2020-118345RB-I00), and the University of Salamanca project grant numbers (PIC2-2021-12) and (ID2021/191).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marcos-Pablos, S., García-Peñalvo, F.J. More than surgical tools: a systematic review of robots as didactic tools for the education of professionals in health sciences. Adv in Health Sci Educ 27, 1139–1176 (2022). https://doi.org/10.1007/s10459-022-10118-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10459-022-10118-6