Abstract
Pressure ulcer risk assessment might be optimized by incorporating the soft tissue reaction to mechanical loading in the currently used risk assessment scales. Cytokines, like IL-1α, IL-1RA, IL-8, and TNF-α, might be used to determine this tissue reaction, since they are released after 24 h of mechanical loading of epidermal equivalents. In the current study, the release and transport of these cytokines with time was evaluated. Epidermal equivalents were subjected to 20 kPa for different time periods (1, 2, 4, 6, 8, 16, and 24 h). Compared to the unloaded control group, a significant increase was found for IL-1α (4.7-fold), IL-1RA (4.8-fold), and IL-8 (3.6-fold) release after 1 h loading. For TNF-α, the release was significantly increased after 4 h of loading (5.1-fold compared to the unloaded situation), coinciding with the first signs of gross structural tissue damage. These cytokine values were determined in the surrounding medium and a transport model was developed to evaluate the distribution of cytokines inside the culture. These simulations revealed that all IL-8 and TNF-α was released from the keratinocytes, whereas most of the IL-1α and IL-1RA remained inside the keratinocytes during the 24 h loading period. In conclusion, IL-1α, IL-1RA, and IL-8 appear promising biochemical markers for pressure ulcer risk assessment, since their release is increased after 1 h of epidermal loading and before the onset of structural tissue damage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pressure ulcers are areas of soft tissue breakdown, resulting from sustained mechanical loading of the skin and underlying tissues. The prevalence of pressure ulcers in hospitalized patients in the Netherlands is unacceptably high with values exceeding 15%.21 The Dutch National Prevalence Survey demonstrated that grade 1 ulcers, the first stage of superficial ulcers in skin, accounted for approximately 50% of the prevalence of pressure ulcers.21 The high prevalence is partly due to the limitation of the risk assessment and detection techniques. Currently, risk assessment is mainly performed by questionnaires or scales like the Norton,31 Braden,1 and Waterlow scale,42 that involve risk factors for pressure ulcer development such as mobility, age, sex, and incontinence. Most risk assessment scales are based on expert opinion and have a limited scientific background.39 Furthermore, Schoonhoven et al.39 demonstrated that risk assessment scales do not predict the degree of susceptibility with the required accuracy and indeed, up to 30% of the hospitalized patients with pressure ulcers are incorrectly classified. Accordingly, patients with high risk might not receive adequate preventive measures.
Further limitations associated with risk scales are that they have to be relatively simple to complete and they should be integrated within a daily routine in hospitals and nursing homes. This results in the inclusion of relatively easy to record parameters such as age, weight or body mass index, sex, mobility of the patient, etc. From a scientific point of view, these parameters represent properties which do not sufficiently reflect the susceptibility of the individual. A characteristic that can reflect the individuals susceptibility would require the assessment of the physiological response of an individual to a specific load regime. The current study is part of a research program on development of a monitoring system that allows the measurement of a tissue reaction in a clinical setting as a complimentary tool to the used risk scales. It focusses on the suitability of biochemical markers to be used to determine the tissue reaction after mechanical loading.
Ideally, pressure ulcer risk detection should be performed at the skin surface in a noninvasive way. Therefore, cytokines are evaluated that originate from keratinocytes in the superficial layer of the skin, the epidermis. Interleukin-1α (IL-1α) is a pluripotent, multifunctional cytokine that plays a key role in the initiation and development of inflammatory and immune responses.41 Furthermore, this cytokine is known to induce the production of other cytokines, such as interleukin-8 (IL-8) and tumor necrosis factor-α (TNF-α).16,41 Interleukin-1 receptor antagonist (IL-1RA), which is also constitutively produced by keratinocytes in the epidermis, is known to inhibit the activity of IL-1α. In a physiological situation, IL-1α is only removed from the epidermis by desquamation of the stratum corneum, due to the lack of a hydrophobic leader sequence for transmembrane secretion.41 However, chemical exposure, UV irradiation, tape stripping, as well as sustained mechanical loading are known to disrupt the cell membrane and release a large amount of IL-1α from the keratinocytes, which normally retain prodigious intracellular stores of IL-1α in the epidermis.2,5,6,18,19,30,32,43,44
It was shown that mechanical straining of keratinocyte monolayers promotes the expression and release of IL-1α and IL-1RA.25,40 Recently, IL-1α, IL-1RA, IL-8, and TNF-α have been identified as promising markers for pressure ulcer risk detection.4,6 Using an in vitro model system for pressure ulcer development, an increase in the release of these markers from tissue-engineered epidermal equivalents was observed after 24 h of loading (0, 6.7, 10, 13.3, 20, and 26.7 kPa). Commercially available EpiDerm cultures, of which the general morphology is comparable to human epidermis, were used as epidermal equivalents in these studies.7,29 In this study, the cytokine values are determined after 24 h of loading, which is a long period regarding to pressure ulcer risk assessment. Experimental studies have suggested an inverse relationship between tissue damage and pressure magnitude and duration.12,24,38 In the pressure–time curves resulting from these studies, it was suggested that a pressure of 20 kPa (150 mmHg) could lead to tissue breakdown after approximately 3 h.
The aim of the present study is to evaluate the release of cytokines (IL-1α, IL-1RA, IL-8, and TNF-α) in the epidermis in vitro with time. Therefore, the following questions are addressed: What is the release of cytokines into the medium after mechanical loading of epidermal equivalents for various loading periods (1, 2, 4, 6, 8, 16, and 24 h)? What are the cytokine values inside the epidermal equivalents after mechanical loading? Furthermore, transport simulations were performed to establish parameters of cytokine release inside the EpiDerm culture to enable the interpretation of the medium results with respect to the values inside the culture.
Materials and Methods
Experimental Model
Engineered Epidermal Equivalent
A commercially available human epidermal equivalent, EpiDerm (EPI-200, MatTek Corporation, Ashland, MA, USA), was used as an in vitro model of the epidermis in this study. The general morphology of this model system resembled that of normal human epidermis and it was mentioned that the model was suitable for screening irritating substances.29 These EpiDerm cultures are comprised of human-derived epidermal keratinocytes, which have been cultured on standing cell culture inserts (Millipore, Billerica, MA, USA) at the air–liquid interface to form a multilayered, differentiated model of the human epidermis.7
Upon receipt, the EpiDerm cultures were placed in 6-well plates, and were cultured overnight at 37 °C and 5% CO2 in 900 μL/well of hydrocortisone free maintenance medium (EPI-100-MM-HCF, MatTek Corporation, Ashland, MA, USA). The next morning, the cultures were transferred to fresh medium and directly used in ‘pressure–time’ experiments. Seven batches of EpiDerm cultures, of 24 cultures each, were used in this study.
Pressure–Time Experiment
A pressure of 150 mmHg (20 kPa) was applied on top of EpiDerm cultures for various loading times (1, 2, 4, 6, 8, 16, and 24 h). As depicted in Fig. 1a, this pressure was applied using indenters and additional weights,5 which were carefully loaded onto the top of the EpiDerm cultures to prevent damage from impact loading. Unloaded cultures were analyzed at the same time points and were used as control. After each loading period, all the surrounding medium was collected and stored at −80 °C for later analysis of cytokines, further referred to as ‘medium cytokines’. The loaded EpiDerm cultures were gently washed with the provided phosphate-buffered saline (PBS, MatTek Corporation, Ashland, MA, USA) and cut in two equal parts. One part was fixated for histological examination and the other part was used to determine the cytokine values inside the epidermal tissue, further referred to as ‘culture cytokines’. This part was placed in 450 μL of 1% (v/v) Triton X-100 (Merck Chemicals Ltd., Nottingham, UK) in hydrocortisone-free maintenance medium at 4 °C, according to recommendations from the supplier (MatTek Corporation, Ashland, MA, USA). After incubation for at least 8 h, the culture lysates were stored at −80 °C for later analysis of the culture cytokines. The measured culture cytokines (pg) can, upon multiplication by a factor two, be directly compared to the medium cytokines (pg).
(a) Schematic representation of the experimental setup. The EpiDerm culture is surrounded by medium and loaded with an indenter with additional weights. (b) Schematic representation of the numerical set-up with the geometry of the EpiDerm culture (gray) and the medium (white). The dashed-dotted line is the axi-symmetry line
Histological Examination
The part of the EpiDerm culture used for histological examination was fixated in 10% phosphate-buffered formalin and processed for conventional paraffin embedding. The cultures were cut in 5 μm thick slices in transversal direction and stained with Hematoxylin and Eosin (H&E). The tissue morphology was studied by light microscopy.
Membrane Integrity
The cell membrane integrity (cell damage) of the EpiDerm cultures was measured by a colorimetric lactate dehydrogenase (LDH) assay (TOX-7, Sigma-Aldrich Co, St. Louis, MO, USA), according to recommendations from the supplier. This assay measures membrane integrity as a function of the amount of cytoplasmic LDH released into the medium. Briefly, assay mixture was prepared by mixing equal amounts of LDH assay substrate, cofactor and dye solutions. For all cultures, assay mixture was added to the medium in a proportion of two to one. After incubation for 30 min at room temperature in the dark, the color reaction was stopped by 1 M HCl. Plain medium was used as blank in this assay. Absorbance was determined at 490 nm using a plate reader. Background correction was performed at 650 nm.
Cytokines
The levels of IL-1α, IL-1RA, IL-8, and TNF-α in the medium and culture lysates were determined by ELISA. TNF-α was quantified by a Quantikine high sensitive kit (HSTA00C, R&D systems, Abingdon, UK) according to the recommendations from the supplier. For IL-1α, IL-1RA, and IL-8 (M9318, Sanquin Reagents, Amsterdam, the Netherlands) quantification, Maxisorp immunoplates (Nalge Nunc international, Roskilde, Denmark) were coated overnight at room temperature with capture antibody. Subsequently, the plates were blocked with PBS/0.5% BSA for 1 h at room temperature, after which the samples and standards were added to the plates. The concentration of the standard cytokine solution ranged for IL-1α from 7.8 to 1000 pg mL−1, for IL-1RA from 31 to 4000 pg mL−1, for IL-8 from 11.7 to 1500 pg mL−1 and for TNF-α from 0 to 32 pg mL−1. After incubation for 1 h at room temperature and washing (PBS/0.005% Tween-20), detection antibody was added. The plates were, furthermore, incubated with 1:10,000 diluted streptavidin-HRP (M2032, Sanquin Reagents, Amsterdam, The Netherlands) for a period of 30 min. The enzyme reaction was initiated by adding 0.2 mg/mL of o-phenylenediamine dihydrochloride in 0.11 M acetate pH 5.5 and 0.03% hydrogen peroxide and stopped with 2 M H2SO4. Dilution buffer (PBS/0.5% BSA/0.005% Tween-20) was used as blank in this assay. Absorbance was determined at a wavelength of 490 nm using a plate reader. All antibodies and standards were purchased from R&D systems (Abingdon, UK), unless otherwise indicated.
Statistics
The results are expressed as mean and standard error of the mean (SEM). Weighted analyses of variance (ANOVA; SPSS 12.0.1, USA) were used to determine the effect of pressure and loading time on medium, culture, and total (i.e., medium+culture) cytokine values. Dunnett’s multiple comparisons test was used to compare the different loading times (2, 4, 6, 8, 16, and 24 h) to the 1 h loading time for both the loaded (150 mmHg) and unloaded control group (0 mmHg). In addition, contrast was employed to compare the loaded and the unloaded control group to one another at each time point (1, 2, 4, 6, 8, 16, and 24 h). Differences were considered significant at a p-value < 0.05.
Numerical Model
Model Equations
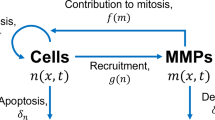
To describe the transport of cytokines through the EpiDerm culture and into the medium, a distinction was made between cytokines that could move freely through the culture and the medium (free cytokines, C f in pg mL−1) and those that were bound to their environment (bound cytokines, C b pg mL−1). The bound cytokines could either be located inside the keratinocytes (C bc) or could be attached to the receptors on the cell-surface membrane (C br pg mL−1). The partial differential equations to describe the transport of cytokines with time (t in s) are given in Eq. (1).
Cytokines that were released from the keratinocytes became free in the extracellular fluid and were described by the source term f (in pg ml−1). Obviously, f = 0 in the medium since no keratinocytes were present here. The second term in the equation for C f reflects the diffusion of cytokines, which was included in both the EpiDerm culture and the medium, and was modeled using Fick’s second law of diffusion. The diffusion coefficient D was obtained from experimental results with values of 2.3 × 10−5 mm2 s−1 for the EpiDerm cultures and 6.9 × 10−5 mm2 s−1 for the medium.10 The remaining terms describe the binding to and the release from the receptors, respectively. These terms were also only taken into account inside the EpiDerm culture. The affinity of the receptors was indicated with the binding constant k b (in mL pg−1 s−1) and the release constant k r (in s−1). The number of receptor sites per keratinocyte was indicated by R t (in pg mL−1). The total cytokine values were comparable at all time points as described in the results section “Cytokine Measurements”, implying that there is a balance between production and degradation of cytokines. Degradation in the medium was measured to be negligible and for convenience, no degradation and no production was assumed in the culture.
The equations were solved using the finite element method. The equations were transformed to the weak form, and subsequently, partial integration and Gauss’ theorem were applied. After linearization, spatial discretization was performed according to Galerkin. For temporal discretization, the Crank–Nicolson scheme was applied. This set of equations was solved using MATLAB.
Model Geometry
The EpiDerm culture, with a diameter of 8 mm, was placed in the middle of a six-well plate with a diameter of 35 mm. The thickness of the EpiDerm culture was determined to be on average 100 μm and due to the dimensions of the cell culture insert was located 1 mm above the bottom of the plate. The medium volume that was added in the experiments filled the well till a height of 1 mm. Therefore, a two-dimensional model, as shown in Fig. 1b, with its axi-symmetric axis perpendicular to the center of the well, was used as geometry for the simulations. The EpiDerm culture and the medium were modeled using 40 and 200 elements, respectively.
Initial and Boundary Conditions
Zero flux was assumed for the boundary conditions of both the outer boundary and along the axi-symmetric axis. The total cytokine values were determined from the experimental results. The initial conditions of the cytokines inside the culture were unknown since the values for free and bound cytokines separately could not be measured. Therefore, the initial value of the free cytokines in the EpiDerm culture (C f0 ) was estimated via a fitting procedure. It was assumed that the free cytokines were in equilibrium with those bound to receptors. From this equilibrium, the initial value of C br was calculated. The medium was added freshly at the start of the experiments and therefore, the initial cytokine value in the medium was zero. So, the initial conditions corresponding to this system were:
Material Parameter Estimation
The material parameters were either obtained from literature, if possible, or identified by fitting the computational results to the experimental observations. The values are summarized in Table 1.
An unknown that was estimated via a fitting procedure was the source term f that represented the cytokines that were released from the keratinocytes. This basal release in the unloaded situation was assumed to be constant. Loading the samples decreased the membrane integrity of the keratinocytes, leading to an additional instantaneous increase of the release of cytokines. This additional release was assumed to decrease with time. These assumptions led to the following equation for the source term in the loaded situation, which is the sum of the additional time-dependent release and the constant basal release, in which the parameters a and b have to be fitted.
In the experiments, four different medium and culture cytokines were determined simultaneously (IL-1α, IL-1RA, IL-8, and TNF-α). Simulating the transport of all cytokines could be done in separate simulations, except for IL-1α and IL-1RA since they bind to the same receptors. To determine all unknown variables, which are C f0 , a, b, and f basal for all cytokines and k b for IL-8 and TNF-α a numerical/experimental method was used.11,26,27 The cost function is based on the sum of the squared differences between the measured concentrations of the cytokines and the calculated concentrations on each time step. This cost function is minimized by means of a Newton minimization procedure. This requires derivatives of the cost function with respect to the material parameters. These derivatives are determined numerically. Starting from an “old” estimate, each parameter is varied with a small amount and then the cost function is calculated by means of a forward numerical analysis. From the difference of the “new” cost function and the “old” cost function the partial derivative to that specific parameter is calculated. This requires n + 1 forward numerical calculations for n different parameters for each iteration. The Newton method converges quadratically, provided that the last estimate is close to the minimum. The initial estimates were determined by manually adjusting parameters until they were close to the experimental results.
Results
Damage Assessment
Figure 2 illustrates the structural tissue damage that was observed as a result of epidermal loading. It was evident that no damage occurred in unloaded cultures (Fig. 2a). After 4 h of loading, the first signs of structural tissue damage appeared in the upper layer of the epidermis (Fig. 2b). Some cell swelling, vacuoles, and necrosis could be detected just below the stratum corneum. Epidermal damage was enhanced with increasing loading times. After 8 h of epidermal loading, more cell swelling and vacuoles could be detected (Fig. 2c). In addition, the stratum corneum appeared less compact and the stratum granulosum was no longer distinguishable. The most severe structural tissue damage was, however, found after 16 and 24 h of loading (Fig. 2d). In addition to the earlier observed structural tissue damage, cell swelling and vacuoles could also be detected in the middle region of the epidermis. Furthermore, the keratinocytes in the lower layer of the epidermis seemed to be compressed.
Histology of unloaded (0 mmHg) EpiDerm cultures (a) and of cultures loaded with 150 mmHg for 4 h (b), 8 h (c), and 24 h (d). The tissue structure of EpiDerm cultures that were loaded for 1 and 2 h are comparable to the unloaded control group (a). Furthermore, the tissue structure after 6 and 16 h of loading are comparable to images (b) and (d), respectively. In (d), the tissue damage is indicated with * indicating cellular necrosis, \(\wedge\) indicating cell swelling and vacuoles, # indicating disruption of the stratum corneum, and + indicating compressed cells. The images were obtained in the middle of the loading region, and the bars indicate a distance of 50 μm
Epidermal loading also affected the cell membrane integrity, as depicted in Fig. 3. An increase in the release of LDH was found in the medium as compared with the unloaded control group (0 mmHg). A first significant increase could be detected after 2 h of loading (4.6-fold vs. 0 mmHg, p < 0.001). This difference in LDH between the loaded (150 mmHg) and unloaded control group further increased with time. The release pattern of the loaded group showed a linear rise at the beginning of the loading period. After 16 h of loading, the release of LDH remained nearly constant with time. Compared to the unloaded control group, a 9.7-fold increase (p < 0.001) in the release of LDH could be measured after 16 h of loading. On the other hand, the release pattern of LDH of the unloaded control group increased minimally with time.
Cytokine Measurements
Cytokine values were measured both in the EpiDerm culture and in the medium. Table 2 illustrates the temporal profiles of cytokine values in medium, culture, and total (culture and medium) during applied loading of 150 mmHg. Although the total cytokine values were significantly different (p < 0.05) at some time points, no general influence of time was observed for any of the four cytokines.
It was evident that the IL-1α and IL-1RA values in the medium were very small compared to the values in the culture during the 24 h of loading, implying that most of IL-1α and IL-1RA remained within the EpiDerm culture (Table 2). By contrast, the medium values of IL-8 and TNF-α were much more comparable to their values in the culture.
The increase in cytokines in the medium was evaluated to investigate the effect of mechanical loading on cytokines release, which is depicted in Fig. 4. After only 1 h of loading, there was a significant increase in the release of IL-1α (4.7-fold vs. 1 h 0 mmHg, p < 0.01), IL-1RA (4.8-fold vs. 1 h 0 mmHg, p < 0.001), and IL-8 (3.6-fold vs. 1 h 0 mmHg, p < 0.01) (Figs. 4a–c). By contrast, a significant increase in TNF-α was only evident after 4 h of epidermal loading (5.1-fold vs. 4 h 0 mmHg, p < 0.05) (Fig. 4d). Furthermore, the values of TNF-α in the medium were very small and could hardly be detected using a high sensitive immunoassay technique. For all cytokines, the difference between the loaded and unloaded control group increased with time. After 16 h of loading, the release of all cytokines remained nearly constant. Compared to the unloaded control group, a 5.1-fold (p < 0.001), 11.7-fold (p < 0.001), 4.8-fold increase (p < 0.001), and 4.8-fold increase (p < 0.001) was found for IL-1α, IL-1RA, IL-8, and TNF-α, respectively, after 16 h of loading. The release pattern of the unloaded control group only slightly increased with time, which was the most evident for IL-1α and IL-8 (Figs. 4a, c).
The values of IL-1α (a), IL-8 (b), IL-1RA (c), and TNF-α (d) in the medium (mean ± SEM) after applying a pressure of 0 and 150 mmHg for various loading times (1, 2, 4, 6, 8, 16, and 24 h). * indicates p < 0.05, ** indicates p < 0.01, and *** indicates p < 0.001 compared to the unloaded control group (0 mmHg). The lines are the fits from the numerical model
Numerical Simulations
Depending on the type of cytokine, different material parameters had to be adapted to find the best fit for the simulated medium values compared to the mean experimental data. The resulting numerical fits for all four cytokines for both the unloaded (solid line) and loaded situations (dashed line) corresponded well with the measured medium values, as illustrated in Fig. 4.
The distribution of the free cytokines in both the EpiDerm culture and the medium after 24 h of loading, which was qualitatively comparable for all four cytokines, is depicted in Fig. 5. The highest values of free cytokines were observed in the EpiDerm culture. The cytokines in the medium were inhomogeneously distributed due to their slow diffusion properties.
Figure 6 shows the resulting release of cytokines from the keratinocytes after the fitting procedure was finished. For the numerical results a conversion was required. In the experiment 900 μL medium was added. The model calculates an average concentration per unit of time, accounting for the axi-symmetry of the system. This concentration was multiplied with 0.9 to get from pg/mL to pg. This leads to the total amount of cytokines in the system.
For the unloaded situation, a constant release was assumed, which is clearly seen in Fig. 6. Mechanical loading resulted in an increased release of cytokines. For IL-1α and IL-1RA, this release returned gradually to normal values after approximately 18 h of loading. The TNF-α release also decreased gradually in the beginning of the loading period whereas the release of IL-8 remained fairly constant, due to the low value of b (Eq. 3) that resulted from the fit. For both IL-8 and TNF-α, the release from the keratinocytes ceased abruptly at approximately 15 h.
To explore the sudden decline in the release of IL-8 and TNF-α, the distribution of cytokines inside the EpiDerm culture was investigated in more detail. For the bound cytokines, difference was made between cytokines that were inside the keratinocytes and those that were bound to receptors. Most of IL-1α and IL-1RA remained inside the keratinocytes during the 24 h loading period, as depicted in Fig. 7. By contrast, all IL-8 and TNF-α was released before the end of the loading period, resulting in the sudden decline in the release as depicted in Fig. 6. Part of these cytokines bound to receptors while the largest part remained free.
Simulated distribution of bound IL-1α (a), IL-1RA (b), IL-8 (c), and TNF-α (d) in the EpiDerm culture after application of 150 mmHg. The dashed line illustrates the total value of bound cytokines (i.e., receptor and total), the solid line illustrates the cytokines bound to receptors and the dash-dotted line the cytokines inside the keratinocytes
Discussion
Cytokines that can be measured in vitro after prolonged mechanical loading are evaluated in the current study, since they might be suitable for pressure ulcer risk detection in vivo. The aim of the present study was to evaluate the pressure–time regulation of the cytokines IL-1α, IL-1RA, IL-8, and TNF-α. Epidermal equivalents were, therefore, subjected to either 0 or 150 mmHg in a custom-built loading device for various loading periods (1, 2, 4, 6, 8, 16, and 24 h). Numerical simulations were performed to estimate the temporal release of cytokines from the keratinocytes inside the culture, based on their measured values in the medium.
In the present study, commercially available EpiDerm cultures were used. These epidermal equivalents provide a representative model to evaluate biochemical markers upon mechanical loading, since the general morphology of the EpiDerm cultures is comparable to that of normal human epidermis.29,35 Indeed, epidermal equivalents, such as EpiDerm, are currently employed as diagnostic models for in vitro toxicology testing.2,9,18,17,33 In these experimental studies, IL-1α release values were comparable with those found in the current study. Furthermore, the observed tissue damage and the release of cytokines into the medium after 24 h of mechanical loading is comparable with an earlier study by Bronneberg et al.,6 indicating that reproducible results can be obtained using the current model system.
Some cell swelling, vacuoles, and necrosis could be detected after 4 h of epidermal loading with 150 mmHg (Fig. 2), which are one of the first signs of cell damage.8 The release of LDH is often measured to assess membrane integrity and was found to be significantly increased after 2 h of mechanical loading, confirming that the cell membrane integrity was indeed affected. The structural tissue damage increased with time, since after 8 h, the stratum corneum appeared to be affected as well. This layer represents the epidermal permeability barrier, that protects the skin against excessive water loss as well as mechanical and chemical insults.15 A less compact stratum corneum might, therefore, indicate loss of structure and function of the epidermal barrier. In the current study, an increase in IL-1α, IL-1RA, and IL-8 was evident in the medium (Fig. 4), prior to the onset of visible tissue damage (i.e., after 4 h of epidermal loading). This increase was first apparent as quickly as 1 h after epidermal loading. There was a much slower release of TNF-α, such that its significant increase only coincided with the first signs of gross tissue damage. In addition, only very small levels of TNF-α were present in the medium (Fig. 4), which could hardly be detected using a ‘high-sensitive’ immunoassay technique.
Upon epidermal loading with 150 mmHg, the release of the cytokines into the medium showed a linear rise until approximately 16 h of loading. These results are in agreement with the observed structural tissue damage, as well as with the extent of cell membrane disruption of LDH leakage. The histology of the EpiDerm cultures showed an increase in tissue damage until a maximum was approximately reached after 16 h of loading. The total cytokine values (i.e., sum of the culture and medium values) remained nearly constant with time, suggesting no additional synthesis of any of the four cytokines during the experiments.
For a detailed evaluation of the described experiments, numerical simulations proved indispensable. In the experiments, it was found that the release of IL-1α and IL-1RA into the medium was much smaller than the values in the culture. For IL-8 and TNF-α, comparable values of culture and medium cytokines were detected. From the numerical simulations it became clear that this difference was due to the bound cytokines that were associated with the keratinocytes. The simulations indicated that the temporal changes in cytokine levels in the medium were a direct result of their transient behavior in the loaded EpiDerm culture. For both IL-8 and TNF-α, the release from the keratinocytes suddenly declined when the total cytokine values were released. Under physiological conditions, this decline would be gradual until all cytokines were released. The implemented constraint, that the values of cytokines inside the keratinocytes cannot be lower than zero, resulted in the sudden decline in the numerical simulations (Fig. 6). This raises some questions with respect to the mathematical form that was chosen for f. Probably in reality the release term f should be a function of C bc , but currently it is not clear what the functional form should be. The saturation that is shown in Fig. 4c for the IL-8 release, however, does point in the direction of a total depletion after 15 h of loading. For TNF-α this effect is less clear, but also here the best fit resulted in a jump condition.
Due to the dimensions of the experimental setup (Fig. 1a), the loading of 150 mmHg was applied in the middle of the EpiDerm culture, resulting in nonuniform deformation of the total culture. Histological examination revealed that the damage beneath the indenter was more severe than the damage adjacent to the indenter, which is comparable to indentation experiments with a skeletal muscle model system.3 However, it was difficult to assess the differences in damage severity and to relate this to different responses of the keratinocytes. Therefore, it was assumed in the simulations that the release from the keratinocytes was homogeneous in the total EpiDerm culture. Furthermore, it has been reported that diffusion is decreased in biological constructs subjected to deformation.20,36 However, identical results were obtained by simulating the experiments with a 50% lower diffusion coefficient, since the EpiDerm culture was very thin compared to its surface area in contact with the medium. Moreover, cytokine transport in the medium was limited due to the low medium diffusion coefficient and not to diffusion inside the EpiDerm culture. So, the diffusion coefficient of the unloaded EpiDerm culture, as measured by Cornelissen et al.,10 was found to be adequate in the current study.
Although the Epiderm cultures have proved their validity in the literature there are of course limitations to the system. Epiderm is a model for epidermis and stratum corneum and may behave differently from normal full skin that is perfused with blood. It is not clear which influence full skin will have on the behavior of the epidermis. A tangible weakness is, that Epiderm does not contain IL-6, which is a very interesting cytokine to study because of it’s role in wound healing. As mentioned above, a drawback of the setup is that the mechanical deformation of the Epiderm specimen is nonuniform. This implies that the external pressure represents a rather complicated mechanical condition and it is difficult to extrapolate results to other loading conditions (e.g., shear). A transport model was used because measurement of the cytokines in the medium only offers indirect information on the processes going on inside the Epiderm specimen. The diffusion equations to describe transport are well established, but the assumptions regarding the interaction terms between free, cell bound, or cell receptor bound cytokines and for the source term are hypothesized and in this primary analysis kept as simple as possible. The objective was to find some phenomenological form for f. Apparently for IL-α and IL-1RA, a fast declining time function has to be chosen and for IL-8 and TNFα a more constant function, but it is clear that more research on this problem is necessary.
In conclusion, cytokines, such as IL-1α, IL-1RA, and IL-8, appear promising biochemical markers for pressure ulcer risk assessment. After 1 h of epidermal loading and before the onset of structural tissue damage, a first increase in the release of IL-1α, IL-1RA, and IL-8 could be observed in the medium as compared with the unloaded control group. On the other hand, TNF-α seems a less promising marker for risk assessment, since an increasing value in the medium was detected when the first signs of tissue damage were already apparent. Furthermore, the values of TNF-α were very small and could hardly be detected using a ‘high sensitive’ immunoassay technique. Numerical modeling enabled an interpretation of the results leading to a first estimate of the kinetics of the cytokines inside the EpiDerm culture.
This study represents a first step in using cytokine measurements to assess the tissue response after mechanical loading. The authors believe that measuring this tissue response improves the risk assessment for pressure ulcers. For further determination of the suitability of these cytokines for risk assessment, it should be established whether they could be measured after prolonged loading in vivo. Furthermore, it would be interesting to examine whether a threshold level of cytokine release exists that distinguishes susceptible from nonsusceptible individuals. Ideally, these in vivo measurements should be quick and noninvasive to enable a fast and objective assessment of the risk of an individual subject. Furthermore, it needs to be established in future studies whether the cytokine values differentiate susceptible from nonsusceptible subjects. The authors believe that measuring the cytokine release alone might not be sufficient to reflect the status of soft tissues and further research might be focussed on measuring the cytokine release in combination with other markers like lactate production34 or transcutaneous oxygen and carbon dioxide tension.23
References
Bergstrom, N., B.J. Braden, A. Laguzza, V. Holman. The Braden scale for predicting pressure sore risk. Nurs. Res. 36:205–210, 1987
Bernhofer, L.P., S. Barkovic, Y. Appa, K.M. Martin. I L-1α and IL-1RA secretion from epidermal equivalents and the prediction of the irritation potential of mild soap and surfactant based consumer products. Toxicol. In Vitro. 13:231–239, 1999
Breuls, R.G.M, C.V.C. Bouten, C.W.J. Oomens, D.L. Bader, F.P.T. Baaijens. Compressiuon induced cell damage in engineered muscle tissue: an in vitro model to study pressure ulcer aetiology. Ann. Biomed. Eng. 31:1357–1364, 2003
Bronneberg, D. Biochemical markers for early detection of superficial pressure ulcers. PhD thesis, Eindhoven, University of Technology, 2007
Bronneberg, D., C.V.C. Bouten, C.W.J. Oomens, P.M. van Kemenade, F.P.T. Baaijens. An in vitro model system to study the damaging effects of prolonged mechanical loading of the epidermis. Ann. Biomed. Eng. 34:506–514, 2006
Bronneberg, D., S.W. Spiekstra, L.H. Cornelissen, C.W.J. Oomens, S. Gibbs, F.P.T. Baaijens, C.V.C. Bouten. Cytokine and chemokine release upon prolonged mechanical loading of the epidermis. Exp. Dermatol. 16:567–573, 2007
Cannon, C.L., P.J. Neal, J.A. Southee, J. Kubilus, M. Klausner. New epidermal model for dermal irritancy testing. Toxicol. In Vitro. 8:889–891, 1994
Cobb, J.P., R.S. Hotchkiss, I.E. Karl, T.G. Buchman. Mechanisms of cell injury and death. Br. J. Anaesth. 77:3–10, 1996
Coquette, A., N. Berna, A. Vanderbosch, M. Rosdy, B. De Wever, Y. Poumay. Analysis of interleukin-1α (IL-1α) and interleukin-8 (IL-8) expression and release in in vitro reconstructed human epidermis for the prediction of in vivo skin irritation and/or sensitization. Toxicol. In Vitro. 17:311–321, 2003
Cornelissen, L. H., D. Bronneberg, C. W. J. Oomens, and F. P. T. Baaijens. Diffusion measurements in epidermal tissues with fluorescent recovery after photobleaching. Skin Res. Technol. 14:462–467, 2008. doi:10.1111/j.1600-0846.2008.00313.x
Cox, M.A.J., D. Gawlitta, N.J.B. Driessen, C.W.J. Oomens, F.P.T. Baaijens. The non-linear mechanical properties of soft engineered biological tissues determined by finite spherical indentation , Comput. Methods Biomech. Biomed. Engin., 11:585–592, 2008
Daniel, R.K., D.L. Priest, D.C. Wheatley. Etiologic factors in pressure sores: An experimental model. Arch. Phys. Med. Rehabil. 62:492–498, 1981
Dower S.K., S.R. Kronheim, C.J. March, P.J. Conlon, T.P. Hoppand, S. Gillis, D.L. Urdal. Detection and characterization of high affinity plasma membrane receptors for human interleukin 1. J. Exp. Med. 162:501–515, 1985
Dripps, D.J., B.J. Brandhuber, R.C. Thompson, S.P. Eisenberg. Interleukin-1 (IL-1) receptor antagonist binds to the 80 kDa IL-1 receptor but does not initiate IL-1 signal transduction. J. Biol. Chem. 266:10331–10336, 1991
Elias, P.M., D.S. Friend. The permeability barrier in mammalian epidermis. J. Cell. Biol. 65:180–191, 1975
Enk, A.H., S.I. Katz. Early events in the induction phase of contact sensitivity. J. Invest. Dermatol. 99: 39S–41S, 1992
Faller, C., M. Bracher. Reconstructed skin kits: reproducibility of cutaneous irritancy testing. Skin Pharmacol. Appl. Skin Physiol. 15:74–91, 2002
Faller, C., M. Bracher, N. Dami, R. Roguet. Predictive ability of reconstructed human epidermis equivalents for the assessment of skin irritation of cosmetics. Toxicol. In Vitro. 16:557-572, 2002
Flint, M.S., R.J. Dearman, I. Kimber, S.A. Hotchkiss.. Production and in situ localization of cutaneous tumour necrosis factor α (TNF-α) and interleukin 6 (IL-6) following skin sensitization. Cytokine. 10:213–219, 1998
Gefen, A., L.H. Cornelissen, D. Gawlitta, D.L. Bader, C.W.J. Oomens. The free diffusion of macromolecules in tissue engineered skeletal muscle subjected to large compression strains. J. Biomech. 41:845-853, 2008
Halfens, R. J., J. M. M. Meijers, J. C. L. Neyens, and M. P. W. Offermans. Rapportage resultaten landelijke prevalentiemeting zorgproblemen. Universiteit Maastricht, 2007
Idriss, H.T., J.H. Naismith. TNF-α and the TNF receptor superfamily: structure-function relationship(s). Microsc. Res. Tech. 50:184–195, 2000
Knight, S.L., R.P. Taylor, A.A. Polliack, D.L. Bader. Establishing predictive indicators for the status of loaded soft tissues. J. Appl. Physiol. 90:2231–2237, 2001
Kosiak, M. Etiology of decubitus ulcers. Arch. Phys. Med. Rehabil. 42:19-29, 1961
Lee, R.T., W.H. Briggs, G.C. Cheng, H.B. Rossiter, P. Libby, T. Kupper. Mechanical deformation promotes secretion of IL-1 alpha and IL-1 receptor antagonist. J. Immunol. 159:5084–5088, 1997
Meijer, R., L.F.A. Douven, C.W.J. Oomens. Characterisation of Anisotropic and Non-linear Behaviour in Human Skin in-vivo, Comp. Meth. Biomech. & Biomed. Engng., 1:13–27, 1999
Meuwissen, M.H.H., C.W.J. Oomens, F.P.T. Baaijens, R. Petterson, J.D. Janssen. Determination of elasto-plastic properties of aluminium using a mixed numerical-experimental method, J. Mater. Process. Technol., 75:204-211, 1998
Michel, G., L. Kemény, R. U. Peter, A. Beetz, C. Ried, P. Arenberger, and T. Ruzicka. Interleukin-8 receptor-mediated chemotaxis of normal human epidermal cells. FEBS Lett. 305:241–243, 1992
Netzlaff, F., C.M. Lehr, P.W. Wertz, U.F. Schaefer. The human epidermis models EpiSkin, SkinEthic and EpiDerm: an evaluation of morphology and their suitability for testing phototoxicity, irritancy, corrosivity, and substance transport. Eur. J. Pharm. Biopharm. 60:167–178, 2005
Nickoloff, B.J., Y. Naidu. Perturbation of epidermal barrier function correlates with initiation of cytokine cascade in human skin. J. Am. Acad. Dermatol. 30:535–546, 1994
Norton, D. Calculating the risk: Reflections on the Norton Scale. Decubitus. 2:24–31, 1989
Oxholm, A., P. Oxholm, B. Staberg, K. Bendtzen. Immunohistological detection of interleukin I-like molecules and tumour necrosis factor in human epidermis before and after UVB-irradiation in vivo. Br. J. Dermatol. 118: 369–376, 1988
Perkins, M.A., R. Osborne, F.R. Rana, A. Ghassemi, M.K. Robinson. Comparison of in vitro and in vivo human skin responses to consumer products and ingredients with a range of irritancy potential. Toxicol. Sci. 48:218–229, 1999
Polliack, A.A., R. Taylor, D. L. Bader. Sweat analysis following pressure ischaemia in a group of debilitated subjects. J. Rehabil. Res. Dev. 34:303–308, 1997
Ponec, M., E. Boelsma, S. Gibbs, M. Mommaas. Characterization of reconstructed skin models. Skin Pharmacol. Appl. Skin Physiol. 15:4–17, 2002
Quinn, T.M., P. Kocian, J. Meister. Static compression is associated with decreased diffusivity of dextrans in cartilage explants. Arch. Biochem. Biophys. 384:327–334, 2000
Qwarnstrom E.E., R.C. Page, S. Gillis, S.K. Dower. Binding, internalization, and intracellular localization of interleukin-1β in human diploid fibroblasts. J. Biol. Chem. 263:8261–8269, 1988
Reswick, J., J. Rogers. Bed Sore Mechanics. London: MacMillan Press, 1976, pp. 301–310
Schoonhoven, L., J.R. Haalboom, M.T. Bousema, A. Algra, D.E. Grobbee, M.H. Grypdonck, E. Buskens. Prospective cohort study of routine use of risk assessment scales for prediction of pressure ulcers. Br. Med. J. 325:797–801, 2002
Takei, T., H. Kito, W. Du, I. Mills, B.E. Sumpio. Induction of interleukin (IL)-1α and β gene expression in human keratinocytes exposed to repetitive strain: their role in strain-induced keratinocyte proliferation and morphological change. J. Cell. Biochem. 69:95–103, 1998
Uchi, H., H. Terao, T. Koga, M. Furue. Cytokines and chemokines in the epidermis, J. Dermatol. Sci. 24:29–38, 2000
Waterlow, J. Pressure sores: A risk assessment card. Nurs. Times. 81:49–55, 1985
Wood, L.C., S.M. Jackson, P.M. Elias, C. Grunfeld, K.R. Feingold. Cutaneous barrier perturbation stimulates cytokine production in the epidermis of mice. J. Clin. Invest. 90:42–47, 1992
Wood, L.C., A.K. Stalder, A. Liou, I.L. Campbell, C. Grunfeld, P.M. Elias, K.R. Feingold. Barrier disruption increases gene expression of cytokines and the 55 kD TNF receptor in murine skin. Exp. Dermatol. 6:98–104, 1997
Acknowledgments
This work was financially supported by SenterNovem, an agency from the Ministry of Economic Affairs in the Netherlands.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Cornelissen, L.H., Bronneberg, D., Bader, D.L. et al. The Transport Profile of Cytokines in Epidermal Equivalents Subjected to Mechanical Loading. Ann Biomed Eng 37, 1007–1018 (2009). https://doi.org/10.1007/s10439-009-9652-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-009-9652-y