Abstract
WHOQOL-AGE is a promising quality of life (QOL) tool that has not been fully validated in Asia. The present study aimed to verify its factor structure and psychometric properties among community-dwelling older adults in Singapore. This study was cross-sectional and used data (N = 593) from the Community Health and Intergenerational study that interviewed older adults between 2018 and 2021. Confirmatory factor analysis (CFA) was used to examine the factor structure of the WHOQOL-AGE, and Cronbach’s alpha coefficients were employed to examine internal consistency. Spearman’s rho correlations coefficients between WHOQOL-AGE and other related scales (Satisfaction with Life and the Friendship) examined convergent validity. A Pearson’s correlation coefficient between WHOQOL-AGE and compassion scale examined discriminant validity. An independent t test was used to demonstrate known-groups validity, examining differences in QOL scores between individuals with and without chronic medical conditions. Findings supported a bifactor model with more satisfactory goodness-of-fit indices than the original two-factor model and the two-correlated factor model. WHOQOL-AGE showed adequate internal consistency (Cronbach’s alpha coefficients > .70). Good convergent validity was demonstrated by moderate-to-large correlations between WHOQOL-AGE and satisfaction with life (rs = .54) as well as social connectedness (rs = .33). Discriminant validity was shown by low correlations between WHOQOL-AGE and compassion (r = .19). Findings also indicated good known-groups validity (p < 0.01). The WHOQOL-AGE showed promising psychometric properties using an Asian convenience sample and can be useful in large-scale studies or busy clinical settings.
Similar content being viewed by others
Introduction
Owing to the advances in medicine and improved technology, many diseases can be treated effectively, resulting in decreased morbidity and mortality, and an increase in life expectancy worldwide (Bengtsson and Keilman 2019; Kyu et al. 2018). Countries continue to need population-based health data to adapt to the changing healthcare landscape by understanding their community public health problems, in order to plan and evaluate effective healthcare policies and treatment (Balogun et al. 2017; Hickey et al. 2010; Shrestha et al. 2015). Quality of Life (QOL) is a complex multidimensional concept that has been a target for research and practice worldwide (Bulamu et al. 2015; Haraldstad et al. 2019; Pequeno et al. 2020; The WHOQOL Group 1998). For instance, QOL instruments guide healthcare providers to make decisions about disease management (Llewellyn & Skevington 2016), provide policy makers and researchers with population-based data to inform policies (Fernandez-Mayoralas et al. 2012; Purba et al. 2018; National Council of Social Service 2017), and design preventive and rehabilitation programs (Aw et al. 2019; Chung et al. 2015).
According to the WHOQOL Group (1994), QOL is defined as “the individuals’ perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns.” Despite generic QOL measures having advantages such as allowing researchers to compare QOL between healthy and sick individuals, and across different social and cultural backgrounds, it has been argued that they may not capture areas of QOL relevant to older adults such as social participation, autonomy/independence, or safe living environment (Bowling et al. 2012; Gabriel & Bowling 2004; Kalfoss and Halvorsrud 2009; Power et al. 2005). Furthermore, older adults reported that it was their capability to achieve things or participate in valued activities that contributed to their QOL, while health served as a catalyst (Makai et al. 2014; Milte et al. 2014). As such, specific QOL instruments for older adults were developed such as the 43-item Elderly Quality of Life Index (Paschoal et al. 2008) and the 24-item WHOQOL—Older adults (WHOQOL-OLD; Power et al. 2005) that is used in conjunction with the 26-item Abbreviated World Health Organization Quality of Life questionnaire (WHOQOL-BREF; Skevington et al. 2004). However, their long administration time may pose a challenge for older adults to complete, especially when time is limited (e.g., clinical setting). Findings from a systematic review (Pequeno et al. 2020) indicated that research studies reported using easier and shorter measures such as the Medical Outcomes Study Short-Form 36/12 (SF-12/36; Ware et al. 1993) as compared to longer WHOQOL assessments. Hence, to address WHOQOL-OLD’s long administration time and SF-36/12’s lack of specific domains important to older adults, the WHOQOL-AGE was developed (Caballero et al. 2013).
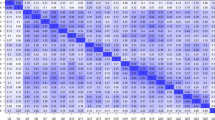
The 13-item WHOQOL-AGE was derived from the EUROHIS-QOL 8-item index (Schmidt et al. 2006) and the WHOQOL-OLD short-form version 1 (Fang et al. 2012) to create a questionnaire that contained items from different domains relevant to older adults such as psychological, physical, environmental and social QOL, as well as capture their abilities in sensory abilities, social participation, autonomy, future activities and intimacy, which are all related to QOL. This short instrument was designed to be used in large-scale studies and busy clinical settings. The WHOQOL-AGE has been validated in countries such as Finland, Poland, Spain and Taiwan, showing good psychometric properties (Caballero et al. 2013; Lin et al. 2020; Santos et al. 2018; Özcan & Eser 2020), refer to Table 1. Findings confirmed a scale that comprised one second-order factor representing QOL and two first-order factors, where the overall QOL item 1 loaded on both factors (see left figure in Fig. 1). Results from the original study revealed a two-factor model with cross-loading on item Q1 and showed good internal consistency (Cronbach’s α = 0.91), strong convergent validity with satisfaction with life (r = 0.75) and discriminant validity with net affect validity (r = 0.35) as well as good known-groups validity between healthy (M = 74.19, SD = 13.21) and physical ill (M = 64.29, SD = 16.29) individuals (p < 0.001) (Caballero et al. 2013). The study by Santos further explored the multidimensionality of the WHOQOL-AGE and tested two structural models (Santos et al. 2018): a bifactor model and two-correlated factor model (see middle and right figures in Fig. 1). Findings provided evidence that the factor structure of the WHOQOL-AGE fitted better with a bifactor model and demonstrated partial invariance across three European countries. Although the WHOQOL-AGE showed partial invariance across three countries, there is a need to examine the scale structure for different cultures and populations. Moreover, in their analyses, the original model (Caballero et al. 2013) was not compared. Another study subsequently compared several factor structures of a translated WHOQOL-AGE among Taiwanese older adults and examined measurement invariance (Lin et al. 2020). Results favored the bifactor model found in a previous study conducted in Europe (Santos et al. 2018), whereby goodness-of-fit indices were the best among all the previously proposed models. In addition, WHOQOL-AGE was found to have measurement invariance across genders, educational levels, living settings and ages. This provided further evidence of a bifactor model underlying the scale in another cultural setting and population (Lin et al. 2020).
The Turkish version of the WHOQOL-AGE was also explored. Findings revealed an alternative two-factor model with different item compositions showed slightly better goodness-of-fit values than the original scale (Özcan & Eser 2020). However, both models showed poor comparative fit index (CFI) and Tucker-Lewis (TLI) values (< 0.90). It is recommended that a broad range of fit indices (e.g., predictive and absolute fit) and assessment of standardized loadings should be used (Morrison et al. 2017).
Current literature indicated that the psychometric properties of the WHOQOL-AGE have mostly been validated in Europe, while the investigation in Taiwan validated a translated version and did not include external criteria assessment (e.g., concurrent/divergent validity). Cultural and linguistic differences may cause translated questionnaires to have different psychometric properties than the original, so the properties of the original English version need to be examined in an Asian context. Furthermore, the WHOQOL-AGE (Caballero et al. 2013) has been used to assess overall QOL among older adults in Singapore (Shorey et al. 2021; Siew et al. 2021). It is timely that the suitability of this tool is formally established for general use in Singapore. This will deepen the understanding of the WHOQOL-AGE factor structure and accumulate further psychometric evidence for QOL literature. The validation of the WHOQOL-AGE would add evidence that the interpretation of scores is valid, encouraging professionals to continue using this tool to describe the QOL of the general population or specific groups in Singapore (e.g., people with health chronic conditions), and provide support for this tool to be used as a baseline and outcome measure to evaluate the effect of clinical and/or public health interventions on QOL. The validation of the WHOQOL-AGE would also allow the comparison of findings obtained in Singapore and Western countries. Therefore, the objectives of this study are to
-
1.
verify the factor structure of the WHOQOL-AGE using another Asian sample,
-
2.
evaluate the reliability and validity of the WHOQOL-AGE.
Methods
Design and sampling
This study was cross-sectional and used data collected through the Community Health and Intergenerational (CHI) study in Singapore between 2018 and 2021 (Lee et al. 2020). The CHI study sought to investigate vulnerability and protective factors of aging using a biopsychosocial framework. Eligible participants were older adults of any gender and ethnic group, residing in the community, with or without known medical conditions, and aged between 60 and 91 years. Convenience and snowball sampling were employed. Older adults were recruited via word of mouth, advertisement flyers at community centers and door-to-door house visits conducted by research assistants and nurses. Specifically, participants who lived within a 10 km radius from the research site (situated in the central-west region of Singapore) were recruited. The Department of Statistics of Singapore (2017) verified that over 3000 older adults resided in the Anak Bukit Area (i.e., subzone of central west district) of Singapore, where the research site was located. The present study was part of the larger CHI study and used an overall sample of 593 participants who responded to questionnaires in English (refer to Table 2 for participants’ characteristics). This study was approved by the Ethics Committee of the National University of [Singapore].
Sociodemographic information
Sociodemographic information included age, years of schooling, marital status divided into four categories (single, married, widowed, divorced/separated), gender (male or female), household income level grouped into six categories (no income, below $2000, $2000–$4999, $5000–$7999, $8000–$10,999 or above $11,000) and living arrangements grouped into living alone or living with others. Participants were also asked to indicate yes or no if they had been diagnosed with the following conditions: hypertension, hyperlipidemia, diabetes, stroke, heart conditions, asthma, kidney, chronic obstructive lung disease, tuberculosis, arthritis, osteoporosis, neurodegenerative disorders, cancer, anxiety/depression and thyroid problems. Participants were classified as having a chronic medical condition if they had at least one of the conditions listed above. Similar to previous studies (Klainin-Yobas et al. 2019; Yu et al. 2020), participants’ scores from a range of cognitive tests were evaluated by a panel of psychiatrists and their cognitive status was subsequently categorized as healthy or with cognitive impairment. The panel used Petersen’s (2004) criteria for mild cognitive impairment and assessed subjective cognitive complaints (via Clinical Dementia Rating), presence of objective cognitive impairment, as well as preserved functional independence.
WHOQOL-AGE (Caballero et al. 2013)
The WHOQOL-AGE contains 13 items and assesses general QOL in older adults. Scores range from 13 to 65 and items are rated using a 5-point Likert scale with two types of response format. For instance, items Q1–Q8 responses were classified as bipolar (e.g., very bad to very good), while items Q9–Q13 responses were classified as unipolar (e.g., not at all to completely). Higher scores suggest better QOL. The scale was found to have high internal consistency (e.g., Cronbach’s α values ranging from 0.84 to 0.91), good convergent, discriminant and criterion-related validity (Caballero et al. 2013; Santos et al. 2018; Özcan and Eser 2020).
Satisfaction with life scale (Diener et al. 1985)
The SWLS is a brief 5-item scale that assesses global life satisfaction rated on a 1 (Strongly Disagree) to 7 (Strongly Agree) point Likert scale. Scores range from 5 to 35, with higher scores indicating higher life satisfaction. The SWLS has demonstrated strong internal reliability with Cronbach’s α = 0.88 (Park et al. 2009; Vera-Villarroel et al. 2012) and test–retest reliability, r = 0.82 (Diener et al. 1985). Moreover, the SWLS has been found to positively correlate with QOL (r = 0.49) using the WHOQOL-BREF (Vera-Villarroel et al. 2012).
Friendship Scale (Hawthorne 2006)
The 6-item Friendship Scale measures social connectedness and is scored on a 0 (not at all) to 4 (almost always) scale, with scores ranging from 0 to 24. Higher scores indicated higher levels of social connectedness, while lower scores assessed levels of social isolation. It was found to have good internal reliability (Cronbach’s α = 0.83) and good concurrent and discriminant validity (Hawthorne 2008).
Compassion (Martins et al. 2013)
The 10-item Compassion Scale is used to measure compassion toward others across five domains and has an acceptable internal consistency of Cronbach’s α value of 0.82 (Martins et al. 2013). It uses a 7-point Likert scale with scores ranging from 7 to 70, and higher scores suggest greater level of compassion.
Procedure
Participants were informed of the purpose of the research, procedures and potential risks involved. Thereafter, written consent was obtained. Participants were interviewed by trained research assistants and nurses. Interviews were conducted at the research site or in the participants’ homes. As part of the CHI study, questionnaires and assessments were collected over six separate visits, with each lasting approximately 1–2 h. Participants in this study completed the sociodemographic questionnaire in the first visit. Thereafter, participants completed the WHOQOL-AGE, SWLS, Friendship Scale and Compassion Scale during their second visit. Participants were offered a total of up to SGD$50 as a token of appreciation. The study procedure has been explained in more detail in a prior publication (Lee et al. 2020).
Statistical analysis
The tenability of the hypothesized bifactor structure of the WHOQOL-AGE was investigated through CFA. CFA was used to compare the data against three structural models (refer to Fig. 1) and to explore whether the data obtained in Singapore fitted the bifactor model as found in previous studies (Lin et al. 2020; Santos et al. 2018). The three models included the original two-factor model (Model 1) made up of one second-order and two first-order factors (Caballero et al. 2013), a bifactor model (Model 2) and another two-factor model (Model 3) that was made up of two-correlated factors, both proposed by Santos and colleagues (Santos et al. 2018). The three models were compared using the χ2 difference test, whereby a model that had a significantly lower χ2 indicated a better fit (Lin et al. 2020). Although nonsignificant χ2 values indicate a good fit, the χ2 statistic is known to be sensitive to sample size and might be inflated (significant) when sample sizes are large (Schreiber et al. 2006; Burnham and Anderson 2002). Model fit was also assessed using goodness-of-fit indices, whereby adequate cutoff values were indicated by root-mean-square error of approximation (RMSEA) values < 0.08 (Browne and Cudeck 1992), comparative fit index (CFI) values > 0.90 (Bentler 1990), Standardized Root-Mean-Square Residual (SRMR) values < 0.08 (Hu and Bentler 1999), Tucker-Lewis Index (TLI) values > 0.90 (Bentler 1990) and the lowest Akaike Information Criterion (AIC) value (Schermelleh-Engel et al. 2003). Measurement quality of WHOQOL-AGE was further assessed by the magnitude of standardized loadings (> 0.40) between each latent construct and its manifest variables (Stevens 1996). Cronbach’s α coefficients were calculated to appraise the internal consistency of the WHOQOL-AGE. Convergent validity was examined using Spearman’s rho correlations (rs), while discriminant validity was evaluated by a Pearson’s correlation (r). Correlation coefficients ≥ 0.30 were considered evidence of convergent validity and lower correlation coefficients (r < 0.30) as evidence of discriminant validity (Kaplan and Saccuzzo 2017). Known-group validity was tested using a Student’s independent t test that compared WHOQOL-AGE scores between people with and without chronic medical conditions according to previous research (Caballero et al. 2013). Significant levels were set to an α level of 0.05. All statistical analyses were conducted using R software (R-4.1.1). CFA was conducted using the lavaan package (Rosseel 2012).
Results
WHOQOL-AGE factor structure
The distribution of scores for each item of the WHOQOL-AGE was normally distributed, whereby skewness values ranged between − 1.01 and − 0.29, and kurtosis values ranged between 0.62 and 2.82 (Kline 2011). CFA analyses and χ2 difference test were conducted to compare the data against three structural models (see to Fig. 1) that were identified in previous research (Caballero et al. 2013; Lin et al. 2020; Santos et al. 2018). All three proposed models had significant χ2 (p < 0.001). Among the proposed models, the data fit the hypothesized bifactor model (Model 2) the best. Goodness-of-fit indices obtained in each model are shown in Table 3. Results from the χ2 difference test to compare all three models also indicated that Model 2 significantly outperformed Models 1 (p < 0.001) and 3 (p < 0.001).
Model 2 (bifactor model) comprised a general QOL factor and two latent factors (e.g., F1: bipolar and F2: unipolar response scales). In Model 2, the standardized regression coefficients (i.e., factor loadings) of the general factor QOL were significant, p < 0.05 (see Fig. 2). In the bifactor model, all 13 items are associated with a general factor (loading: 0.352–0.716) to a much higher degree than with the two latent factors (loadings: 0.015–0.600). The general factor, which can be interpreted in terms of general QOL, is thus shown to be the dominant source of the item variances.
In Model 1, first-order standardized regression coefficients were significant (p < 0.001), and the factor loadings of items 1 to 8 on Factor 1 ranged from 0.254 to 0.791, while the factor loadings of item 1 and items 9 to 13 on Factor 2 ranged from 0.458 to 0.685. The second-order standardized loadings of Factor 1 and 2 on general QOL were both 0.865. In Model 3, the first-order factor loadings of Model 3 were significant (p < 0.001), whereby factor loadings of items 1 to 8 on Factor 1 (bipolar response scale) ranged from 0.447 to 0.778 and factor loading of items 9 to 13 on Factor 2 (unipolar response scale) ranged from 0.502 to 0.678.
Internal reliability
Model 2 was used to test for internal consistency of the WHOQOL-AGE. Adequate Cronbach’s alpha values were found for each of the two latent factors (Cronbach’s α coefficient = 0.83 for Factor 1, Cronbach’s α = 0.73 for Factor 2) and the entire WHOQOL-AGE scale (Cronbach’s α coefficient was 0.86), indicating that all domains were consistent and within acceptable ranges (Cohen 1988).
Convergent validity
To assess convergent validity of the WHOQOL-AGE, it was hypothesized that there would be medium-to-large positive correlation coefficients between QOL scores and life satisfaction (measured with the SWLS) as well as social connectedness (as assessed by the FS). Spearman’s correlation analyses revealed a large and statistically significant positive correlation between scores on the WHOQOL-AGE and SWLS scores, rs(591) = 0.54, p < 0.001, and a moderate and significant positive correlation between scores for the WHOQOL-AGE and social connectedness, rs(591) = 0.33, p < 0.001, indicating good convergent validity.
Discriminant validity
To assess discriminant validity, it was hypothesized that there would be low correlation coefficients (r < 0.30) between QOL scores and scores from unrelated constructs such as compassion (measured with the Compassion Scale). A Pearson’s correlation analysis revealed a statistically significant low and positive correlation between QOL scores and level of compassion, r(591) = 0.19, p < 0.001.
Known-groups Validity
Known-groups validity of WHOQOL-AGE was assessed by an independent t test, whereby the WHOQOL-AGE score was compared between participants with and without chronic medical conditions. Similar to previous research (Caballero et al. 2013), it was hypothesized that participants without chronic conditions would have higher QOL scores than those with at least one chronic condition. Results indicated that participants without chronic conditions had significantly higher QOL scores than participants with chronic condition, t(591) = 2.82, p < 0.01, Cohen’s d = 0.31.
Discussion
The present study verified the factor structure of the WHOQOL-AGE using a Singapore sample and evaluated the scale’s reliability and validity. It is important to ensure that the original (English) version of the WHOQOL-AGE’s factor structure can be applied in Singapore. CFA findings revealed that the bifactor model with one general QOL factor and two specific group factors achieved acceptable fit and outperformed both the original second-order factor model and the two-correlated factor model. The bifactor model found in this study provided goodness-of-fit indices such as RMSEA, CFI, SRMR and TLI values that were consistent with a model of QOL previously found in Western (Santos et al. 2018) and Asian (Lin et al. 2020) populations. Findings suggest that the global concept of QOL in older adults in Singapore may be similar to the QOL proposed by WHO (Power et al. 2005; Skevington et al. 2004), whereby the structure of the QOL in Singapore seems to comprise a general component of QOL (items related to psychological, physical, social, sensory, environmental, autonomy and intimacy) and two components related to the questionnaire response scales. Moreover, previous studies using other WHOQOL measures in Singapore demonstrated sound psychometric properties (Suárez et al. 2018).
Factor loadings obtained in the study were similar to Santos et al.’s (2018) study, whereby most of the WHOQOL-AGE items displayed significant factor loadings for the general factor (QOL) as compared to the loadings for the two group factors (bipolar and unipolar response scale). In our community sample, the WHOQOL-AGE appears to capture well the general dimension of QOL. Moreover, it was argued that higher loadings on the general factor indicate that items primarily represent the general QOL construct and suggest against computing the subscale scores (Reise et al. 2010). Inspection of standardized factor loadings in this study also showed that Q2 on sensory abilities made the lowest contribution (below 0.40) to overall QOL. One possible reason could be due to the lack of sensory difficulties experienced by the participants in the present study (e.g., majority in their 60 s), as sensory problems are more prevalent in older adults over 80 years old (Homans et al. 2017) and impede functional independence and QOL with those advanced in age (Cimarolli & Jopp 2014). Additionally, all other items contributed significantly to overall QOL, mirroring previous findings (Lin et al. 2020; Liu et al. 2013), and suggest the importance of various aspects of well-being for overall QOL in older adults. Taken together, factor loadings on the general factor found in this study were generally acceptable, above 0.40 (Brown 2015), suggesting that all 13 items of the WHOQOL-AGE add valuable information to the global QOL.
The pattern of results also showed several items where the loadings were very high on the general and low on the group factor (< 0.10) such as Q1, Q6 and Q7 on Factor 1 (bipolar response scale) as well as Q13 on Factor 2 (unipolar response scale). It is possible that participants may have interpreted and rated Q1 different from the rest of items on Factor 1 due to differently worded bipolar response scales used (e.g., bad vs dissatisfied and good vs satisfied). It is suggested to use the same bipolar response scale and replace Q1 with “How satisfied are you with your quality of life?” to correspond with the rest of the items on Factor 1. Findings are also consistent with literature on QOL (Liu et al. 2013; Suárez et al. 2018) whereby some aspects seemed to contribute most to QOL than others (e.g., self-esteem, personal relationships). Also, Q13 a question on intimacy showed low loadings on Factor 2 which could be due to differently worded unipolar response scales (e.g., completely and an extreme amount) and culture as older adults are sensitive to topics about intimacy and may not express their true feelings when interviewed (Wang et al. 2006). Similarly, it is suggested that the same unipolar response scale is used and replace Q13 with “To what extent are you satisfied with your intimate relationships in your life?”. Future studies using exploratory factor analysis could be conducted to assess whether replacements could improve factor loadings on these items. Future research using exploratory factor analysis and CFA could explore revising low factor loading items to improve factor loadings.
The WHOQOL-AGE showed good internal consistency, consistent with the original development papers and previous two validation studies (Caballero et al. 2013; Lin et al. 2020; Santos et al. 2018). Convergent validity was demonstrated by moderate-to-large positive correlations between QOL and related constructs (e.g., satisfaction with life and social connectedness). This was in line with previous research (Dorji et al. 2017; Mei et al. 2021; Yang and Srinivasan 2016). The current findings also provide preliminary evidence of discriminant validity for the WHOQOL-AGE, demonstrated by low correlations between QOL and an unrelated construct (e.g., compassion) (Campbell & Fiske 1959). Consistent with the literature (Caballero et al. 2013; Özcan & Eser 2020), the WHOQOL-AGE discriminated between healthy individuals and individuals with at least one chronic medical condition, showing adequate known-groups validity, although the effect size of the difference between groups was relatively small (Cohen’s d = 0.31) as compared to previous studies (Caballero et al. 2013; Özcan & Eser 2020); one possible reason for such small effect size could be that the current sample was relatively younger (Mage = 67.19 years) and more physically independent as compared to those previous studies, and their chronic condition may still be in the early stages to influence their QOL. Future studies may further investigate whether the WHOQOL-AGE applied in Singapore is sensitive in detecting intervention effects and other variables (e.g., dependency) that were previously found to decrease QOL in older adults (Lobo et al. 2014; Tobiasz-Adamczyk et al. 2017).
It needs to be acknowledged that participants in this study were predominantly of Chinese descent (94.3%) community-dwelling older adults living in the central-west region of Singapore. This was similar to the ethnic distribution reported by the Department of Statistics, Singapore (2017), for the Anak Bukit Area of Singapore. However, the ethnic distribution of the older adult sample in this study (see Table 2) was slightly different from the total ethnic distribution of older adults in Singapore, whereby 74.07% residents were Chinese, 13.36%% were Malay, 9.23% were Indians, and 3.33% belonged to the others group (Department of Statistics 2010). While findings can be generalized to neighborhoods with similar ethnic proportions, it may be difficult to generalize to the general older adult population in Singapore, or clinical populations. In addition, the present study did not assess multigroup invariance and test–retest reliability of the WHOQOL-AGE; hence, further support is needed to evaluate its reproducibility, stability and construct validity. Future research could further conduct measurement invariance testing across different conditions as previously invariance was supported in Taiwan on across gender, education levels and living settings (Lin et al. 2020). As only the English version of WHOQOL-AGE was used in this study, future research could test for structural invariance across language and evaluate the validity of translated versions.
In conclusion, the present study demonstrated promising psychometric properties of the WHOQOL-AGE using a Singapore older adult sample. Findings from this study supplement current literature as the data fitted a bifactor model and showed adequate internal consistency, convergent and discriminant validity, and known groups validity. WHOQOL-AGE may provide healthcare professional and researchers a valid tool to assess QOL for older adults, especially in community settings or when time is limited. With further research, the WHOQOL-AGE can be used to evaluate intervention effects, assess community needs and inform treatment planning in Singapore and other Asian populations.
References
Aw S, Koh GCH, Tan CS, Wong ML, Vrijhoef HJM, Harding SC, Geronimo MAB, Hildon ZJL (2019) Theory and design of the community for successful ageing (ComSA) program in Singapore: connecting biopsychosocial health and quality of life experiences of older adults. BMC Geriatr 19(1):254. https://doi.org/10.1186/s12877-019-1277-x
Balogun SA, Balogun R, Philbrick J, Abdel-Rahman E (2017) Quality of life, perceptions, and health aatisfaction of older adults with end-stage renal disease: a systematic review. J Am Geriatr Soc 65(4):777–785. https://doi.org/10.1111/jgs.14659
Bengtsson T, Keilman N (2019) Old and new perspectives on mortality forecasting. Springer
Bentler PM (1990) Comparative fit indexes in structural models. PsyB 107(2):238–246. https://doi.org/10.1037/0033-2909.107.2.238
Bowling A, Hankins M, Windle G, Bilotta C, Grant R (2012) A short measure of quality of life in older age: the performance of the brief Older People’s Quality of Life questionnaire (OPQOL-brief). Arch Gerontol Geriatr 56(1):181–187. https://doi.org/10.1016/j.archger.2012.08.012
Brown TA (2015) Confirmatory factor analysis for applied research. Guilford Publications, New York
Browne MW, Cudeck R (1992) Alternative ways of assessing model fit. Sociol Methods Res 21(2):230–258. https://doi.org/10.1177/0049124192021002005
Bulamu NB, Kaambwa B, Ratcliffe J (2015) A systematic review of instruments for measuring outcomes in economic evaluation within aged care. Health Qual Life Outcomes 13(1):179. https://doi.org/10.1186/s12955-015-0372-8
Burnham KP, Anderson DR (2002) Model selection and multimodel inference : a practical information-theoretic approach, 2nd edn. Springer, New York
Caballero FF, Marta M, Power M, Chatterji S, Tobiasz-Adamczyk B, Koskinen S, Leonardi M, Olaya B, Haro JM, Ayuso-Mateos JL (2013) Validation of an instrument to evaluate quality of life in the aging population: WHOQOL-AGE. Health Qual Life Outcomes 11:177. https://doi.org/10.1186/1477-7525-11-177
Campbell DT, Fiske DW (1959) Convergent and discriminant validation by the multitrait-multimethod matrix. PsyB 56(2):81–105. https://doi.org/10.1037/h0046016
Chung OKJ, Li HCW, Chiu SY, Ho KY, Lopez V (2015) Sustainability of an integrated adventure-based training and health education program to enhance quality of life among Chinese childhood cancer survivors: a randomized controlled trial. Cancer Nurs 38(5):366–374. https://doi.org/10.1097/ncc.0000000000000211
Cimarolli VR, Jopp DS (2014) Sensory impairments and their associations with functional disability in a sample of the oldest-old. Qual Life Res 23(7):1977–1984. https://doi.org/10.1007/s11136-014-0657-0
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Lawrence Erlbaum Associates, Hillsdale, New Jersey
Department of Statistics S (2010) Census of population: statistical release 2
Department of Statistics S (2017) Population trends
Diener E, Emmons RA, Larsen RJ, Griffin S (1985) The satisfaction with life scale. J Pers Assess 49(1):71–75. https://doi.org/10.1207/s15327752jpa4901_13
Dorji N, Dunne MP, Seib C, Deb S (2017) Quality of life among senior citizens in Bhutan: associations with adverse life experiences, chronic diseases, spirituality, and social connectedness. Asia Pac J Public Health 29(1):35–46. https://doi.org/10.1177/1010539516685609
Fang J, Power M, Lin Y, Zhang J, Hao Y, Chatterji S (2012) Development of short versions for the WHOQOL-OLD module. Gerontologist 52(1):66–78. https://doi.org/10.1093/geront/gnr085
Fernandez-Mayoralas G, Giraldez-Garcia C, Forjaz MJ, Rojo-Perez F, Martinez-Martin P, Prieto-Flores M-E (2012) Design, measures and sample characteristics of the CadeViMa-Spain survey on quality of life in community-dwelling older adults. Int Psychogeriatr 24(3):425–438. https://doi.org/10.1017/s1041610211002018
Gabriel Z, Bowling ANN (2004) Quality of life from the perspectives of older people. Ageing Soc 24(5):675–691. https://doi.org/10.1017/s0144686x03001582
Haraldstad K, Wahl A, Andenæs R, Andersen JR, Andersen MH, Beisland E, Borge CR, Engebretsen E, Eisemann M, Halvorsrud L, Hanssen TA, Haugstvedt A, Haugland T, Johansen VA, Larsen MH, Løvereide L, Løyland B, Kvarme LG, Moons P, Norekvål TM, Ribu L, Rohde GE, Urstad KH, Helseth S (2019) A systematic review of quality of life research in medicine and health sciences. Qual Life Res 28(10):2641–2650. https://doi.org/10.1007/s11136-019-02214-9
Hawthorne G (2006) Measuring social isolation in older adults: development and initial validation of the friendship scale. Soc Indic Res 77(3):521–548. https://doi.org/10.1007/s11205-005-7746-y
Hawthorne G (2008) Perceived social isolation in a community sample: its prevalence and correlates with aspects of peoples’ lives. Soc Psychiatry Psychiatr Epidemiol 43(2):140–150. https://doi.org/10.1007/s00127-007-0279-8
Hickey A, O’Hanlon A, McGee H (2010) Quality of life in community-dwelling older people in Ireland. Null 31(3–4):135–150. https://doi.org/10.1080/03033910.2010.10446331
Homans NC, Metselaar RM, Dingemanse JG, van der Schroeff MP, Brocaar MP, Wieringa MH, Baatenburg de Jong RJ, Hofman A, Goedegebure A (2017) Prevalence of age-related hearing loss, including sex differences, in older adults in a large cohort study. Laryngoscope 127(3):725–730. https://doi.org/10.1002/lary.26150
Hu L-t, Bentler PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model 6(1):1–55. https://doi.org/10.1080/10705519909540118
Kalfoss M, Halvorsrud L (2009) Important issues to quality of life among norwegian older adults: an exploratory study. Open Nurs J 3:45–55. https://doi.org/10.2174/1874434600903010045
Kaplan RM, Saccuzzo DP (2017) Psychological testing: principles, applications, and issues. Nelson Education, Toronto
Klainin-Yobas P, Kowitlawakul Y, Lopez V, Tang CT, Hoek KE, Gan GL, Lei F, Rawtaer I, Mahendran R (2019) The effects of mindfulness and health education programs on the emotional state and cognitive function of elderly individuals with mild cognitive impairment: a randomized controlled trial. J Clin Neurosci 68:211–217. https://doi.org/10.1016/j.jocn.2019.05.031
Kline RB (2011) Principles and practice of structural equation modeling, Principles and practice of structural equation modeling, 3rd edn. Guilford Press, New York
Kyu HH, Abate D, Abate KH, Abay SM et al (2018) Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet 392(10159):1859–1922. https://doi.org/10.1016/S0140-6736(18)32335-3
Lee RZY, Yu J, Rawtaer I, Allen PF, Bao Z, Feng L, Feng Q, Lee JK, Lim CT, Ling LH, Thang LL, Naing T, Wang DY, Yap KZ, Kua E, Mahendran R (2020) CHI study: protocol for an observational cohort study on ageing and mental health in community-dwelling older adults. BMJ Open 10:e035003. https://doi.org/10.1136/bmjopen-2019-035003
Lin C-Y, Wang J-D, Liu L-F (2020) Can we apply WHOQOL-AGE to Asian population? Verifying its factor structure and psychometric properties in a convenience sample from Taiwan. Front Public Health 8:575374. https://doi.org/10.3389/fpubh.2020.575374
Liu R, Wu S, Hao Y, Gu J, Fang J, Cai N, Zhang J (2013) The Chinese version of the world health organization quality of life instrument-older adults module (WHOQOL-OLD): psychometric evaluation. Health Qual Life Outcomes 11(1):156–156. https://doi.org/10.1186/1477-7525-11-156
Llewellyn AM, Skevington SM (2016) Evaluating a new methodology for providing individualized feedback in healthcare on quality of life and its importance, using the WHOQOL-BREF in a community population. Qual Life Res 25(3):605–614. https://doi.org/10.1007/s11136-015-1132-2
Lobo AdJS, Santos L, Gomes S (2014) Level of dependency and quality of life of elderly. Rev Bras Enferm 67(6):913–919. https://doi.org/10.1590/0034-7167.2014670608
Makai P, Brouwer WBF, Koopmanschap MA, Stolk EA, Nieboer AP (2014) Quality of life instruments for economic evaluations in health and social care for older people: a systematic review. Soc Sci Med 102:83–93. https://doi.org/10.1016/j.socscimed.2013.11.050
Martins D, Nicholas NA, Shaheen M, Jones L, Norris K (2013) The development and evaluation of a compassion scale. J Health Care Poor Underserved 24(3):1235–1246. https://doi.org/10.1353/hpu.2013.0148
Mei S, Qin Z, Yang Y, Gao T, Ren H, Hu Y, Cao R, Liang L, Li C, Tong Q (2021) Influence of life satisfaction on quality of life: mediating roles of depression and anxiety among cardiovascular disease patients. Clin Nurs Res 30(2):215–224. https://doi.org/10.1177/1054773820947984
Milte CM, Walker R, Luszcz MA, Lancsar E, Kaambwa B, Ratcliffe J (2014) How important is health status in defining quality of life for older people? An exploratory study of the views of older South Australians. Appl Health Econ Health Policy 12(1):73–84. https://doi.org/10.1007/s40258-013-0068-3
Morrison TG, Morrison MA, McCutcheon JM (2017) Best practice recommendations for using structural equation modelling in psychological research. Psychology 8(09):1326
National Council of Social S (2017) Understanding quality of life of seniors
Özcan C, Eser E (2020) Validation of the Turkish version of the WHOQOL-AGE and a proposed alternative scale structure. Tjgeri 23(2):157–168. https://doi.org/10.31086/tjgeri.2020.150
Park N, Peterson C, Ruch W (2009) Orientations to happiness and life satisfaction in twenty-seven nations. J Posit Psychol 4(4):273–279. https://doi.org/10.1080/17439760902933690
Paschoal SMP, Jacob Filho W, Litvoc J (2008) Development of elderly quality of life index - EQoLI: item reduction and distribution into dimensions. Clinics 63(2):179–188. https://doi.org/10.1590/s1807-59322008000200005
Pequeno NPF, Cabral NLdA, Marchioni DM, Lima SCVC, Lyra CdO (2020) Quality of life assessment instruments for adults: a systematic review of population-based studies. Health Qual Life Outcomes 18(1):208. https://doi.org/10.1186/s12955-020-01347-7
Petersen RC (2004) Mild cognitive impairment as a diagnostic entity. J Intern Med 256(3):183–194. https://doi.org/10.1111/j.1365-2796.2004.01388.x
Power M, Quinn K, Schmidt S (2005) Development of the WHOQOL-Old module. Qual Life Res 14(10):2197–2214. https://doi.org/10.1007/s11136-005-7380-9
Purba FD, Hunfeld J, Fitriana TS, Iskandarsyah A, Sadarjoen S, Busschbach J, Passchier J (2018) Living in uncertainty due to floods and pollution: the health status and quality of life of people living on an unhealthy riverbank. BMC Public Health 18(1):782–782. https://doi.org/10.1186/s12889-018-5706-0
Reise SP, Moore TM, Haviland MG (2010) Bifactor models and rotations: exploring the extent to which multidimensional data yield univocal scale scores. J Pers Assess 92(6):544–559. https://doi.org/10.1080/00223891.2010.496477
Rosseel Y (2012) Lavaan: an R package for structural equation modeling. J Stat Softw 48(2):1–36
Santos D, Abad FJ, Miret M, Chatterji S, Olaya B, Zawisza K, Koskinen S, Leonardi M, Haro JM, Ayuso-Mateos JL, Caballero FF (2018) Measurement invariance of the WHOQOL-AGE questionnaire across three European countries. Qual Life Res 27(4):1015–1025. https://doi.org/10.1007/s11136-017-1737-8
Schermelleh-Engel K, Moosbrugger H, Müller H (2003) Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Methods Psychol Res 8(2):23–74
Schmidt S, Mühlan H, Power M (2006) The EUROHIS-QOL 8-item index: psychometric results of a cross-cultural field study. Eur J Public Health 16(4):420–428. https://doi.org/10.1093/eurpub/cki155
Schreiber JB, Nora A, Stage FK, Barlow EA, King J (2006) Reporting structural equation modeling and confirmatory factor analysis results: a review. J Educ Res 99(6):323–338. https://doi.org/10.3200/joer.99.6.323-338
Shorey S, Kua EH, Tam W, Chan V, Goh YS, Lim HM, Lim LHK, Tian CS, Mahendran R (2021) “Where-there-is-no-psychiatrist integrated personal therapy” among community-dwelling older adults: a randomized pilot study. Int J Environ Res Public Health 18(18):9514
Shrestha S, Stanley MA, Wilson NL, Cully JA, Kunik ME, Novy DM, Rhoades HM, Amspoker AB (2015) Predictors of change in quality of life in older adults with generalized anxiety disorder. Int Psychogeriatr 27(7):1207–1215. https://doi.org/10.1017/s1041610214002567
Siew S, Mahendran R, Yu J (2021) Directional effects of social isolation and quality of life on anxiety levels among community-dwelling older adults during a COVID-19 lockdown. Am J Geriat Psychiat. https://doi.org/10.1016/j.jagp.2021.03.012
Skevington SM, Lotfy M, O’Connell KA (2004) The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial A Report from the WHOQOL Group. Qual Life Res 13(2):299–310. https://doi.org/10.1023/b:Qure.0000018486.91360.00
Suárez L, Tay B, Abdullah F (2018) Psychometric properties of the World Health Organization WHOQOL-BREF quality of life assessment in Singapore. Qual Life Res 27(11):2945–2952. https://doi.org/10.1007/s11136-018-1947-8
The WG (1994) The development of the World Health Organization quality of life assessment instrument (the WHOQOL). In: Orley J, Kuyken W (eds) Quality of life assessment: international perspectives. Springer, Berlin, pp 41–60
The WG (1998) Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med 28(3):551–558. https://doi.org/10.1017/s0033291798006667
Tobiasz-Adamczyk B, Galas A, Zawisza K, Chatterji S, Haro JM, Ayuso-Mateos JL, Koskinen S, Leonardi M (2017) Gender-related differences in the multi-pathway effect of social determinants on quality of life in older age—The COURAGE in Europe project. Qual Life Res 26(7):1865–1878. https://doi.org/10.1007/s11136-017-1530-8
Vera-Villarroel P, Alfonso Urzúa M, Pavez P, Celis-Atenas K, Silva J (2012) Evaluation of subjective well-being: analysis of the satisfaction with life scale in chilean population. Univ Psychol 11(3):719–727. https://doi.org/10.11144/javeriana.upsy11-3.eswa
Wang B, Gao H, Liu X (2006) A Study on applicability of WHOQOL-OLD module in Chinese elderly patients with prostatic hyperplasia. Chin J Nurs 41:687–690
Ware JE, Snow KK, Kosinski M, Gandek B (1993) Health survey manual and interpretation guide. The Health Institute, New England Medical Center, Boston, MA
Yang C, Srinivasan P (2016) Life satisfaction and the pursuit of happiness on Twitter. PLoS ONE 11(3):e0150881–e0150881. https://doi.org/10.1371/journal.pone.0150881
Yu J, Rawtaer I, Fam J, Feng L, Kua E-H, Mahendran R (2020) The individualized prediction of cognitive test scores in mild cognitive impairment using structural and functional connectivity features. Neuroimage 223:117310–117310. https://doi.org/10.1016/j.neuroimage.2020.117310
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
R.M. is the principal investigator. R.M. initiated and conducted the study with a team of researchers (including R.Z.Y.L.). R.M., L.S. and R.Z.Y.L. contributed to the study conception and design. Data analysis was performed by R.Z.Y.L. in consultation with W.F.Z.Y., L.S. and R.Z.Y.L. prepared the first draft of the manuscript. R.M. and W.F.Z.Y. revised the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors have no relevant financial or nonfinancial interests or conflict of interests to disclose.
Additional information
Responsible Editor: Matthias Kliegel.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, R.Z.Y., Yang, W.F.Z., Mahendran, R. et al. Psychometric properties of the World Health Organization WHOQOL-AGE Scale in Singapore. Eur J Ageing 21, 10 (2024). https://doi.org/10.1007/s10433-024-00803-3
Accepted:
Published:
DOI: https://doi.org/10.1007/s10433-024-00803-3