Abstract
This study reports on an integrated microfluidic system capable of counting CD4+/CD8+ T lymphocytes from a whole blood sample, which may be further applied for the rapid screening of the human immunodeficiency virus (HIV) infection. This system is composed of a sample incubation module for fluorescence-labeling of the target cells and a micro-fabricated flow cytometry module for cell counting. First, a pneumatically driven, vortex-type micro-mixer has been adopted for the fluorescence-labeling of CD4+/CD8+ T lymphocytes from whole blood. After the labeling process, different laser-excited fluorescent signals are detected and are used for counting of CD4+/CD8+ T lymphocytes as they pass through the detection region of the microflow cytometer. A concentration of 963 cells/μl is counted for cultured CD4+ T lymphocytes with a reference concentration of 1000 cells/μl. The ratio of CD4+/CD8+ T lymphocytes is then calculated. Experimental results show that the results from the microsystem are in agreement with the ones from large-scale flow cytometers. In addition, the entire diagnostic procedure, including the sample incubation and the cell counting, can be automatically performed within 35 min. Therefore, this may become a powerful tool for further biomedical applications, especially for fast screening of HIV infection.
Similar content being viewed by others
1 Introduction
The global HIV infection pandemic HIV infection has been a serious threat to human beings. It may lead to the acquired immunodeficiency syndrome (AIDS) where the immune system fails and causes the body to become susceptible to life-threatening infections (Tsoukas and Bernard 1994). Therefore, there is a great need for a fast and accurate diagnostic method for HIV infection. Briefly, there are several existing methods which can be used for identifying a HIV infection, including (1) a serological diagnosis approach such as western blotting (Guan 2007), enzyme-linked immunosorbent assay (ELISA, Robinson et al. 1990) and an agglutination test (Monzon et al. 1992) either to detect HIV p24, which is a core protein in the HIV particles, to measure anti-HIV antibodies, (2) a molecular diagnosis approach such as real-time polymerase chain reaction (RT PCR) to quantitatively measure the HIV viral load (Lewin et al. 1999), and (3) a cell-based assay to measure CD4 absolute counts or the CD4/CD8 ratio quantified by using flow cytometry (Balakrishnan et al. 2004; Dieye et al. 2005; Strauss et al. 1996). Western blotting, ELISA and an agglutination test could capture HIV surface proteins or anti-HIV antibodies, and therefore, they can be used for fast screening of a HIV infection. However, the sensitivity of these serological diagnosis methods is usually not satisfactory. Besides, the time window for the spread of an AIDS infection can be a serious concern for blood transfusion. Alternatively, a viral load measurement can be accurately performed by using the RT PCR method. However, bulky and costly instruments are usually required, which may be not available for resource-limited regions or in underdeveloped countries. Furthermore, well-trained personnel are required to perform these relatively complicated and lengthy protocols. More importantly, the contamination risk due to the handling of infected samples is a serious issue.
The CD4+ T lymphocyte counts are adopted to identify the HIV infection. The CD4+ T lymphocyte counts are expressed as the absolute number of CD4+ T lymphocytes per micro-liter of blood for adults, and a percentage of total lymphocytes or total T lymphocytes for children. Furthermore, the measurement of the ratio of the CD4+/CD8+ T lymphocytes is also essential to monitor the course of the infection and determine the antiretroviral medications (Tsoukas and Bernard 1994). Therefore, the prognostic and therapeutic implications of the absolute CD4+ T lymphocytes counts and the ratio of the CD4+/CD8+ T lymphocytes are used to form most HIV treatments decisions (Mellors et al. 1997; O’Brien et al. 1996, 1997). However, it is necessary for each HIV-infected patient to perform the CD4+/CD8+ T lymphocyte counts using flow cytometry every 3–6 months. Flow cytometer is a crucial instrument for detecting one type of lymphocyte from another by labeling different fluorescent antibody probes specific for CD4 and other cell surface markers and excited by laser (Balakrishnan et al. 2004; Dieye et al. 2005; Strauss et al. 1996). However, several concerns regarding the use of a large-scale flow cytometer, including the relatively high cost and the relatively high consumption of blood samples and reagents, have made this instrument difficult to use in resource-limited settings. Thus, an inexpensive and user-friendly CD4 diagnostic tool urgently has to been developed (Glencross et al. 2002a, b; Huff 2001). For instance, recently, a CD4 counting device designed for resource-limited settings was reported, in which the capture of leukocytes and imaging of the CD4 subset were carried out on a membrane within a miniaturized flow cell (Rodriguez et al. 2005). However, this device still requires off-line sample preparation, including labeling of the blood samples, and fluorescence-based detection for imaging and counting of target cells.
Microfluidic systems have been a promising tool for clinical diagnostics. They are based on micro-electro-mechanical systems (MEMS) fabrication technologies. Critical functions such as sample preparation, mixing, reaction, transport, separation, and detection of biosamples can be performed on a single chip in an automated manner. The advantages of these microfluidic systems include smaller amounts of required samples and reagents, faster analysis, and higher sensitivity. Also, the functionality and reliability of these microfluidic systems could be significantly enhanced with the integration of other multi-functional components. However, biological samples and reagents usually still use external, automated, large-scale instruments for sample transport. Moreover, intensive human labor is inevitable. To address these problems, microfluidic systems integrated with micro-valves and micro-pumps can be used to automate the entire process (Dittrich and Manz 2006; Dittich et al. 2006; Huh et al. 2005; Lin et al. 2010; Lui et al. 2009; Radisic et al. 2006; Toner and Irimia 2005; Voldman 2006; Wu et al. 2010). With this approach, a compact and automated, microfluidic system is feasible.
Recently, CD4 cell counting devices using microfluidic technology have been reported (Cheng et al. 2007a, b). The microfluidic channels were first functionalized with immobilized anti-CD4 antibodies for isolation of the CD4+ T lymphocytes. Then CD3+/CD4+ T lymphocytes were counted under an optical microscope. In order to avoid using an optical microscope for the counting process, microfluidic chips with lens-less imaging of target CD4+ T lymphocytes were also reported (Moon et al. 2009; Rodriguez et al. 2005). Alternatively, counting the number and the percentage of CD4+ T lymphocytes in a polydimethylsiloxane (PDMS) microchannel were reported recently (Thorslund et al. 2008). Anti-CD4 antibodies were immobilized on one side of a microfluidic chip to capture CD4+ T lymphocytes from whole blood. A charge-coupled-device (CCD) sensor was used to detect these captured cells through an optically transparent chip by lens-less shadow imaging techniques. Another demonstrated approach was to use an optical fluorescence detection scheme with resistive pulse sensing enhanced by a metal-oxide-semiconductor-field-effect-transistor (MOSFET, Wang et al. 2008). When a cell passed the sensing channel, the resistive pulse sensing and fluorescence detection were operated concurrently. The MOSFET recorded all of the cell events, while the fluorescent signals only recorded the cells with a specific fluorescent tag. With this approach, the percentage of the specific cells can be counted. However, the integration of MOSFETs with microfluidic devices is still challenging. Besides, simultaneous CD4+/CD8+ T lymphocyte counts were not yet performed. Recently, four differential leukocyte counts of human blood including neutrophils, eosinophils, lymphocytes, and monocytes by a microflow cytometer were reported (Shi et al. 2010). A two-color laser-induced fluorescence detection scheme was adopted. However, the reagent and the blood sample were still incubated utilizing a conventional bench-top machine.
This study, therefore, reports a new integrated microfluidic system comprising of a micro incubation module and a microflow cytometer module to perform the sample incubation and the CD4+/CD8+ T lymphocyte count. The sample incubation module is comprised of a pneumatically driven, vortex-type micro-mixer (Yang et al. 2009a) to automatically perform the incubation between CD4+/CD8+ T lymphocytes and anti-CD3/CD4/CD8 antibodies, respectively, which increases incubation efficiency and decreases the reaction time. After the incubation process, different laser-induced fluorescence signals are used to measure the CD4+/CD8+ T lymphocyte counts by adopting a micro-fabricated flow cytometry system (Yang et al. 2006). More importantly, the entire process can be performed automatically within a short period of time (35 min). To the best of our knowledge, it is the first integrated device for performing the incubation and cell counting for CD4+/CD8+ T lymphocytes.
2 Experimental
2.1 Chip design and fabrication
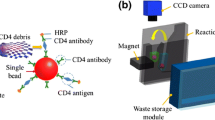
This study reports a new microfluidic system capable of automatic counting the CD4+/CD8+ T lymphocyte by integrating a sample incubation module and a microflow cytometry module on a single chip. Figure 1a schematically illustrates the microfluidic system integrated with two functional modules. The sample incubation module comprised an incubation chamber and a pneumatically driven, vortex-type micro-mixer (Yang et al. 2009a). The micro-mixer consists of three flange-type individual PDMS membranes. Since the air chambers are connected with the air channels, the three membranes are deflected sequentially by the supplied compressed air to generate a vortex-type flow field inside the incubating chamber. Therefore, the mixing procedure between the fluidic samples is rapidly carried out by the vortex-type micromixer. It is used for the incubation process between the CD4+/CD8+ T lymphocytes and the anti-CD4/CD8/CD3 antibodies.
a Schematic illustration of the integrated microfluidic system for counting of CD4+/CD8+ T lymphocytes. The functional components including a sample incubation module and a micro flow cytometry module are integrated on a single chip. b A photograph of the assembled microfluidic system. The width and length of the chip are measured to be 55 and 65 mm, respectively. c A schematic illustration of the optical detection unit
The microflow cytometry module consists of a microfluidic focusing unit for sample flow focusing in the microchannel and an optical detection unit for cell counting. The microfluidic focusing unit in the microflow cytometry module provides the required hydrodynamic forces for flow focusing utilizing three pneumatic micro-pumps (one for sample flow and two for sheath flows, Chang et al. 2007b). The pneumatic micro-pump is also used as the micro-valve to avoid the leakage during the mixing process. In this approach, a pneumatic micro-pump featuring an S-shape air microchannel with a normally closed valve has been adopted. Fluid is driven by the hydrodynamic pressure generated by the peristaltic action of PDMS membranes located at the intersection of the fluidic microchannel and the S-shape air microchannel (Yang et al. 2009b; Wang and Lee 2006). Thus, the CD4+/CD8+ T lymphocytes with the fluorescent-labeled anti-CD3/CD4/CD8 antibodies were driven using the pneumatic micro-pump to flow into the microchannel after the labeling. In addition, the hydrodynamic flow focusing of the sample flow is achieved without using large-scale syringe pumps, and it take only 3 s for establish a steady flow rate for hydrodynamic focusing. With this approach, cells can flow through the detection region downstream in a single file. Therefore, the fluorescent-labeling process of CD4+/CD8+ T lymphocytes from whole blood and the absolute counting of CD4+/CD8+ T lymphocytes can be achieved in an automatic manner by using the integrated microfluidic chip to avoid any contamination risk from handling infected samples.
The proposed microfluidic system is fabricated using MEMS processes. Briefly, a layer of SU-8 negative thick photoresist (PR, MicroChem Corp., MA, USA) is first spun onto a silicon substrate and is subject to a soft bake process at 65°C for 10 min and at 95°C for 30 min. A standard lithography process with an exposure dose of 575 mJ/cm2 is then performed and is followed by a post-exposure bake process at 65°C for 3 min and then at 95°C for 10 min. The SU-8 development process is completed by immersing the exposed substrates into a developer solution (SU-8 Developer, MicroChem Corp) and ultrasonic agitation is used to obtain well-defined SU-8 structures. The depths of all SU-8 templates are measured to be 100 μm. In addition, the width of the S-shape micro-pump and the flow focusing microchannel are 250 and 100 μm, respectively. The dimensions of the PDMS membranes in the micro-mixer are 4500 μm in width and 7500 μm in length. The dimensions of the connecting air channel are 4500 μm in length and 100 μm in width.
Then, the SU-8 template is replicated using a PDMS (Sil-More Industrial Ltd., Sylgard 184A and Sylgard 184B) casting process to form microfluidic structures with inverse images. Another PDMS thin layer with a thickness of 100 μm is formed using a similar process, and then the double-layer PDMS is surface-treated with oxygen plasma and bonded together to form the vortex-type micro-mixer and three S-shape micro-pumps. The two-layer PDMS are finally bonded onto a glass substrate using an oxygen plasma treatment. Figure 1b shows a photograph of the integrated microfluidic system with the sample incubation module and microflow cytometry module after assembly. The dimensions of the integrated microfluidic system are measured to be 65 × 55 mm, respectively.
2.2 Experimental setup and operating procedures
A sample incubation process using the vortex-type micro-mixer is first performed to bind the fluorescent-labeled antibodies with target CD4+/CD8+ T lymphocytes in the human blood. The air chambers of the micro-mixers are placed above the liquid layer. Vortices are induced by the time-phased deflection of neighboring PDMS membranes as the membranes are actuated with compressed air regulated by an electromagnetic valve (EMV, S070M-5BG-32, SMC Inc., Japan) and air compressor (MDR2-1A/11, JUN-AIR Inc., IL, USA). These three flange-type PDMS membranes are moved up and down sequentially by injecting compressed air into the cavities formed between the PDMS structures. The driving frequency of the EMV is regulated utilizing a micro-controller (ATMEGA8353, ATMEL Corp., USA) such that the target CD4+/CD8+ T lymphocytes and the anti-CD3/CD4/CD8 antibodies conjugated with cyanine dyes modified with either a –NO2 group (CyQ for CD3), fluorescein isothiocyanate (FITC for CD4), or R-Phycoerythrin (R-PE for CD8) fluorescent proteins, respectively, can be homogeneously mixed in the sample incubation chamber. The micro-mixer is characterized utilizing a high-speed CCD camera (MC1311, Mikrotron, Germany).
After the incubation process, the CD4+/CD8+ T lymphocytes surface-bound with fluorescent-labeled antibodies are then transported into a microfluidic focusing unit and are detected by an optical detection unit. Three pneumatic micro-pumps are used to provide the required hydrodynamic forces in the microflow cytometry module and are actuated with compressed air regulated by an EMV and an air compressor. In addition, the optical detection unit (as shown in Fig. 1c) consists of one 473 nm solid-state laser diode (MBL5, CNI Corp., China), three 495 nm/535 nm/625 nm long-pass dichroic mirrors (DCLP, Lin Trading Co., Ltd.), three filters (515 ± 30, 575 ± 30, and 675 ± 50 nm, Chroma Technology Corp., USA), and three photo-multiplier tubes (PMTs, R928, Hamamatsu, Japan). The system including optical detection and pneumatically driving units is cheaper and smaller than the conventional machine. A laser source with a 473-nm wavelength is used to excite the fluorescent-labeled antibodies bound on the T lymphocytes when the focused cell sample flows through the optical detection region. Each signal peak indicates the fluorescent intensity of the antibodies conjugated on the CD4+/CD8+ T lymphocytes. The three different optical signals corresponded to the CD3+/CD4+/CD8+ T lymphocytes, respectively.
The entire process including the sample incubation between the anti-CD3/CD4/CD8 and CD4+/CD8+ T lymphocytes, and the CD4+/CD8+ T lymphocyte counting is described as follows. It has been experimentally found that red blood cells (RBCs) may affect the measurement of T lymphocytes. Therefore, the centrifugation procedure was first performed to separate RBCs without lysing for the use of the large sample volume to increase the accuracy of the fluorescence measurement. Then, the 400-μl centrifuged blood without the RBCs and 8-μl anti-CD3/CD4/CD8 antibodies mixture are individually placed into a sample incubation chamber to perform the incubating procedure using the micro-mixer operated at 1 Hz with an applied pressure of 20 psi for 30 min. By using the affinity between the antibodies and the surface antigens of the T lymphocytes, the target CD4+/CD8+ T lymphocytes are specifically incubated with the anti-CD3/CD4/CD8 antibodies.
After the incubation process, the CD4+/CD8+ T lymphocytes surface-bound with fluorescent-labeled antibodies are first focused hydrodynamically by two neighboring sheath flows which are used to squeeze the central sample flow into a narrow stream. At a constant applied air pressure of 20 psi, the flow rates of the sample flow and the sheath flow are measured to be 75 and 150 μl/min, respectively, at an operating frequency of 15 and 25 Hz for EMVs. Then, the CD4+/CD8+ T lymphocytes surface-bound with fluorescent-labeled antibodies individually flow past incident laser beams for optical detection. The different laser-induced fluorescent signals are used to calculate the absolute CD4+/CD8+ T lymphocyte count and the ratio of CD4+/CD8+ T lymphocytes over a period of 5 min. The schematic of the incubating and the counting process is shown in Fig. 2. In this approach, the CD4+ T lymphocytes are counted only when both signals for anti-CD3 and anti-CD4 antibodies are induced at the same time. Similarly, the CD8+ T lymphocytes are also counted when both induced signals for anti-CD3 and anti-CD8 antibodies appear simultaneously. Therefore, the CD4+/CD8+ T lymphocytes absolute count can be accurately monitored in real-time.
2.3 Reagent and sample preparation
CD3 is a specific surface antigen of the T lymphocytes, which is expressed in all T lymphocytes. In addition, CD4 and CD8 are the helper and cytotoxic specific surface antigen for T lymphocytes, respectively (Anderson et al. 1996; Shortman and Wu 1996; Zúñiga-Pflücker and Lenardo 1996). Thus, CD3+/CD4+ and CD3+/CD8+ T lymphocytes are identified as the helper and cytotoxic T lymphocytes, respectively, in this study. In order to capture mature T lymphocyte cells, a mixture of commercial mouse anti-CD3/CD4/CD8 antibodies (Affinity BioReagents™, USA) is used. The anti-CD3/CD4/CD8 antibodies are conjugated with CyQ, FITC, and RP-E fluorescent proteins, respectively, which can be simultaneously excited by a 488-nm laser diode. The emission wavelengths of the FITC, RP-E, and CyQ fluorescent proteins are 520, 576, and 760 nm, respectively. It is possible for excessive fluorescent-labeled antibodies to increase the noise level when measuring the fluorescent signals. To optimize the volume of fluorescent-labeled antibodies, five different volume ratios (2.5:1, 20:1, 50:1, 100:1, and 200:1) for pretreated whole blood (without RBCs) and the anti-CD3/CD4/CD8 antibodies mixture are tested to perform a CD4+/CD8+ T lymphocyte count using the conventional flow cytometer to optimize the operating conditions for sample incubation. A CD4+/CD8+ T lymphocyte count with a volumetric ratio of 50:1 is then experimentally determined to yield optimum signals. Therefore, the T lymphocyte counts are carried out with a biosample/antibody volumetric ratio of 50:1 in this study. It could reduce the cost of the measuring process since the amount of the antibodies can be reduced.
Then, the whole blood samples are also used to count the CD4+/CD8+ T lymphocyte ratio in addition to the cultured CD4+ T lymphocytes. Under informed consent, blood samples have been obtained from healthy donors. Blood is obtained from veins (3 ml) using a needle and a syringe and stored in a 3-ml tube containing K3-ethylenediamine tetra acetic acid (K3EDTA). Before performing sample incubation and the CD4+/CD8+ T lymphocyte counting procedure, the 2-ml blood samples are first centrifuged at 3000 cycles/min (rpm) for 2 min to separate the RBCs to remove the influence of the RBCs during the CD4+/CD8+ T lymphocyte counting process. Then, the pretreated blood with a volume of 400 μl and anti-CD3/CD4/CD8 antibodies mixture with a volume of 8 μl are individually placed into the sample incubation chamber for the incubating procedure. The biosamples are also analyzed utilizing conventional multicolor flow cytometry analysis (FACSAria, Becton, Dickinson and Company, USA) in parallel to calculate the CD4/CD8 ratios.
3 Results and discussion
3.1 Characterization of microfluidic components
3.1.1 Vortex-type micro-mixer
In this study, a pneumatically driven, vortex-type micromixer has been adopted to form the sample incubation module so that efficient mixing can be achieved within a short period of time. The micro-mixer is first characterized utilizing a high-speed CCD. As shown in Fig. 3a. 400-μl of deionized (DI) water and 2-μl of blue ink are first placed in the mixing chamber. Then the micro-mixer is actuated at 1 Hz at an applied pressure of 20 psi. The experimental data reveals that the mixing of the DI water and the blue ink is completed within 1.2 s. Therefore, the mixing procedure with 400-μl sample would be completely achieved using the micro-mixer. In addition, the captured photographs at 0 and 1.2 s are analyzed using digital image processing techniques to evaluate the mixing efficiency. A mixing index (σ) is used to quantify the mixing performance of the micro-mixers, and is defined as follows (Yang et al. 2009a):
a The mixing motion is observed by using a high-speed CCD. b CD4+ T lymphocytes are captured by magnetic beads surface-conjugated with fluorescent-labeled anti-CD3/CD4 antibodies. c The relationship between the pumping rate and the driving frequency of the EMV at applied pressures of 10, 20, and 30 psi, respectively. d The flow of T lymphocytes is focused and squeezed into a narrow stream (about 20 μm wide) by the surrounding sheath flows
where σ(A) is the mixing index with respect to the local normalized concentration (C +) distributed within the area of the incubation chamber (A). \( C_{0}^{ + } \) is the initial condition of the normalization state, and \( C_{\infty }^{ + } \) is the normalized concentration for the completely mixed state (=0.5). The value of σ is set to be 100% while the samples are completely mixed. Conversely, σ is 0% if the samples are completely unmixed. The mixing index is found to increase from 17.08 to 96.74% for this case.
In order to verify that anti-CD3/CD4 antibodies can efficiently capture target cells, magnetic beads surface-conjugated with the anti-CD3/CD4 antibodies are used for capturing the CD4+ T lymphocytes. Figure 3b shows that a CD4+ T lymphocyte is captured by the magnetic beads conjugated with anti-CD3/CD4 antibodies after incubation for 30 min by using the micromixer. This indicates that the anti-CD3/CD4 antibodies can correctly capture the CD4+ T lymphocytes.
3.1.2 S-shape micro-pump
In order to precisely and rapidly transport the reagents and bio-samples, a pneumatic micro-pump previously developed in our group has been modified and is integrated into this microfluidic system (Yang et al. 2009b; Wang and Lee 2006). The pneumatic S-shape micro-pump integrated with a normally closed valve is composed of four PDMS membranes. The normally closed valve of the micro-pump is a PDMS-based floating block structure located inside the liquid channel, which is activated by hydraulic pressure generated by the peristaltic motion of the PDMS membranes. The normally closed micro-valve can efficiently prevent back flow and contamination without external applied power. Furthermore, the pumping rate can be significantly increased by stopping the back flow utilizing this normally closed micro-valve. The relationship between the pumping rate and the driving frequency of the EMV at three different applied pressures of 10, 20, and 30 psi is shown in Fig. 3c. The maximum value of the pumping rate is measured to be 210 μl/min at a driving frequency of 30 Hz but starts to decrease at higher driving frequencies due to the limitation of the frequency response of the entire system. It is observed that the pumping rate also increased with the increasing pneumatic pressure.
Note that three pneumatically driven micro-pumps are adopted for pumping sample and sheath flows. At a constant applied air pressure of 20 psi, the flow rates of the sample flow and the sheath flow are measured to be 75 and 150 μl/min, at an operating frequency of 15 and 25 Hz for EMVs, respectively. As shown in Fig. 3d, the width of the focused sample flow can be as small as 20 μm. This flow focusing assures that cells pass in a single file through the subsequent optical detection region.
3.2 T lymphocyte counting
3.2.1 CD4+ T lymphocyte counting using cultured CD4 cells
Flow cytometry has advanced significantly with the development of both fluorescent dye synthesis and high-speed optical analytical technologies. This powerful platform has become a routine clinical apparatus. In this study, a microflow cytometry module equipped with a 473-nm exciting laser has been adopted for counting of CD4+/CD8+ T lymphocytes. The specificity of target biosamples is verified by using cultured CD4+ T lymphocytes. First, 400 μl of cultured CD4+ T lymphocytes with a concentration of 1000 cells/μl is placed into the incubation chamber and is incubated with an 8 μl mixture of commercial antibodies for 30 min. The incubation is performed by actuating the micromixer at a driving frequency of 1 Hz and at a pressure of 20 psi. Therefore, the nominal concentration of the CD4+ T lymphocytes was 980 cells/μl. Then, the absolute CD4+ T lymphocytes are counted by using the microflow cytometry module. The integrated microfluidic chips may be reusable after thorough rinsing and washing processes. However, these chips were used only once in this work to avoid the contamination issue. Figure 4 shows the experimental results for the optical detection of the CD4+ T lymphocytes in the microflow cytometry module. A threshold line for T lymphocytes labeled with anti-CD3/CD4 antibodies is used to differentiate between signals and noise. For the 400-μl cultured CD4+ T lymphocytes with a concentration of 1000 cells/μl, a subset of the induced signals for anti-CD3 and anti-CD4 antibodies are successfully counted, as shown in Fig. 4a and b, respectively. The 993 and 973 peaks in the induced signals for anti-CD3 and anti-CD4 antibodies, respectively, counted for the 1-μl sample. Thus, only 13 and 7 peaks for anti-CD3 and anti-CD4 antibodies, respectively, are missed. However, the CD4+ T lymphocytes would be counted when both signals of anti-CD3 and anti-CD4 antibodies are simultaneously induced, as shown in Fig. 4c. Thus, a concentration of 963 cells/μl is measured for cultured CD4+ T lymphocytes.
Fluorescent signals collected by a PMT module when CD4+ T lymphocytes with theirs surfaces bound with fluorescent-labeled a anti-CD3 and b anti-CD4 antibodies flow through the optical detection region. c The CD4+ T lymphocytes are counted when both signals for anti-CD3 and anti-CD4 antibodies are induced at the same time
The missing counts could be caused either during the sample incubation procedure or the hydrodynamic flow focusing procedure. The conjugation between the cultured CD4+ T lymphocytes and the anti-CD3/CD4 antibodies may not be 100% complete within the short incubation time even though the optimum incubation time has been experimentally determined to be 30 min in this study. This is because the conjugation may be broken during the mixing procedure. Besides, the fluorescent-label antibodies might also conjugate with the cell debris to increase the fluorescence signal detection. Therefore, the CD4+ T lymphocytes would not be counted since the CD4+ T lymphocytes might conjugate with only anti-CD3 or anti-CD4 antibodies. Furthermore, a two-dimensional hydrodynamic flow focusing has been adopted in this study to squeeze the cultured CD4+ T lymphocytes into a narrow stream. However, the size of the cultured CD4+ T lymphocytes is about 15 μm, which is smaller than the depth of the microchannel (100 μm). Thus, there might be two or more cultured CD4+ T lymphocytes flowing simultaneously through the detection region downstream in the vertical direction. Therefore, reducing the depth of the microchannel or the use of three-dimensional hydrodynamic flow focusing may improve the counting accuracy (Chang et al. 2007a).
3.2.2 T lymphocyte counting from human blood samples
Next, human blood samples collected from seven volunteers, with informed consent, is used to perform the entire procedure which includes sample incubation and the counting of CD4+/CD8+ T lymphocytes utilizing the prototype integrated microfluidic system. During the CD4+/CD8+ T lymphocyte counting procedure, it is observed that the light scattering induced by the RBCs may affect the count. It would be difficult to differentiate the signals from the RBCs and the CD4+ and CD8+ T lymphocytes conjugated with fluorescent-labeled antibodies. Therefore, pretreated blood samples without RBCs are used in this study. Here, the signal peaks are counted when a signal-to-noise (S/N) ratio is greater than 3. The 3000-μl blood samples is first centrifuged at 3000 rpm for 2 min to separate the RBCs prior to performing the diagnostic procedure. Then, the 400-μl of blood samples without RBCs is used to perform the incubation and cell counting procedures by using the prototype microfluidic chip. For comparison, 400-μl of blood samples with RBC separation is also incubated by using a bench-top shaker and are tested by using a large-scale flow cytometer. The fluorescent signals from one pretreated blood sample labeled with anti-CD3/CD4/CD8 antibodies are shown in Fig. 5. Compared to the CD4+/CD8+ T lymphocyte count with whole blood (not shown here), the signal peaks from the anti-CD3/CD4/CD8 antibodies can be easily counted with a threshold S/N ratio of more than 3 for the blood samples without RBCs. However, the background noise signals (2.5–3 mV) for the blood samples without RBCs is higher when compared to the ones for the cultured CD4+ T lymphocytes (0.25–0.5 mV), as shown in Fig. 4, which may be caused by the autofluorescence of cell debris. To improve the signal-to-noise ratio in the fluorescence detection, it is suggested to separate the cell debris from T lymphocytes by integrating the micro-filter into the microfluidic chip in the future. In addition, the optical filter transmitting a narrow band of wavelength could be adopted to block the non-specific wavelength to decrease the background noise.
In addition, Table 1 lists the cell counting data by utilizing the conventional flow cytometer and the integrated microfluidic system. The absolute CD4 and CD8 counts by using the proposed microfluidic chip can be successfully achieved by directly counting the absolute fluorescence signals of the anti-CD3/CD4/CD8 antibodies conjugated with the CD4+/CD8+ T lymphocytes. Thus, this data demonstrates that it is feasible to perform the incubation and to quantify both the absolute CD4 and CD8 counts to evaluate the CD4/CD8 ratio by using the integrated microfluidic chip. For the 400-μl pretreated blood samples without RBCs, the absolute counting of the CD4+/CD8+ T lymphocytes is achieved, as shown in Table 1(a) and (c). Thus, the concentrations of the CD4+/CD8+ T lymphocytes can be calculated (Table 1(b) and (d)). Experimental data also reveal that the CD4/CD8 ratio measured by the integrated microfluidic chip is consistent with the ones measured using the conventional flow cytometry.
In order to quantitatively evaluate the performance of the proposed microfluidic system, comparisons of the CD4/CD8 ratio results obtained between the microfluidic system and the conventional flow cytometer are made based on a Bland–Altman plot (Bland and Altman 1999) and a Passing–Bablok regression analysis (Passing and Bablok 1983). Figure 6a shows the result of the Bland–Altman plot. It indicates that there is no apparent bias for the CD4/CD8 ratio since the differences between these two methods are all within the mean ± 1.96 standard deviation (SD) interval. Moreover, Fig. 6b shows the result from Passing–Bablok regression analysis in which the equation for the regression line is y = 0.8948x + 0.2536. The 95% confidence interval (CI) shows that the slope and the intercept are not significantly different from 1 and 0, respectively, since the slope ranges from 0.2536 to 1.1145 (including 1) and the intercept ranges from −0.2256 to 1.5629 (including 0). These results indicate that the CD4/CD8 ratio determined by the prototype microfluidic chip is in good agreement with the ratio determined by the conventional flow cytometer.
Compared to the existing method which uses a conventional bench-top shaker and a large-scale flow cytometer that requires more than 1 h to complete the assay, the entire process can now be automatically performed within 35 min by using the microfluidic system. More importantly, the cost of the microsystem is much lower than that of the conventional method since the bench-top flow cytometer is relatively expensive and may consume more reagents. Therefore, the developed microfluidic system may provide a promising tool for rapid analysis of immunodeficiency and lymphocytic diseases.
4 Conclusions
This study reports a new integrated microfluidic system comprising of a sample incubation module and a microflow cytometry module to automatically perform the entire process for CD4+/CD8+ T lymphocyte counting. The sample incubation module is formed with a pneumatically driven, vortex-type micromixer to perform the sample incubation between CD4+/CD8+ T lymphocytes and anti-CD3/CD4/CD8 antibodies for increasing incubation efficiency and for decreasing the reaction time. After the incubation procedure, the microflow cytometry module is used for the analysis of CD4+/CD8+ T lymphocytes surface-bounded with fluorescent-labeled antibodies. A concentration of 963 cells/μl is counted for the cultured CD4+ T lymphocytes with a reference concentration of 1000 cells/μl. Human blood samples are then tested. Absolute counting of CD4+/CD8+ T lymphocytes and CD4/CD8 ratio is successfully measured. Comparable results are obtained when compared with the data from a conventional flow cytometer. The entire procedure including sample incubation and cell counting can be finished within 35 min. Therefore, this microsystem may be used for the fast, accurate, and affordable counting of CD4+/CD8+ T lymphocytes in resource-limited settings.
References
Anderson G, Moore NC, Owen JT, Jenkinson EJ (1996) Cellular interactions in thymocyte development. Annu Rev Immunol 14:73–99
Balakrishnan P, Dunne M, Kumarasamy N, Crowe S, Subbulakshmi G, Ganesh AK, Cecelia AJ, Roth P, Mayer KH, Thyagarajan SP, Solomon S (2004) An inexpensive, simple, and manual method of CD4 T-cell quantitation in HIV-infected individuals for use in developing countries. J Acquir Immune Defic Syndr 36:1006–1010
Bland JM, Altman DG (1999) Measuring agreement in method comparison studies. Stat Methods Med Res 8:135–160
Chang CC, Huang ZX, Yang RJ (2007a) Three-dimensional hydrodynamic focusing in two-layer polydimethylsiloxane (PDMS) microchannels. J Micromech Microeng 17:1479–1486
Chang CM, Hsiung SK, Lee GB (2007b) Micro flow cytometer chip integrated with micro-pumps/micro-valves for multi-wavelength cell counting and sorting. Jpn J Appl Phys 46:3126–3134
Cheng X, Irimia D, Dixon M, Sekin K, Demirci U, Zamir L, Tompkins RG, Rodriguez W, Toner M (2007a) A microfluidic device for practical label-free CD4+ T cell counting of HIV-infected subjects. Lab Chip 7:170–178
Cheng X, Irimia D, Dixon M, Ziperstein JC, Demirci U, Zamir L, Tompkins RG, Toner M, Rodriguez W (2007b) A microchip approach for practical label-free CD4+ T-cell counting of HIV-infected subjects in resource-poor settings. J Acquir Immune Defic Syndr 45:257–261
Dieye TN, Verrecken C, Diallo AA, Ordoa P, Diaw PA, Camara M, Karam F, Mboup S, Kestens L (2005) Absolute CD4 T-cell counting in resource-poor settings: direct volumetric measurements versus bead-based clinical flow cytometry instruments. J Acquir Immune Defic Syndr 39:32–37
Dittich PS, Tachikawa K, Manz A (2006) Micro total analysis systems. Latest advancements and trends. Anal Chem 78:3887–3908
Dittrich PS, Manz A (2006) Lab-on-a-chip: microfluidics in drug discovery. Nat Rev Drug Discov 5:210–218
Glencross D, Scott LE, Jani IV, Barnett D, Janossy G (2002a) CD45-assisted PanLeucogating for accurate, cost-effective dual-platform CD4+ T-cell enumeration. Cytometry 50:69–77
Glencross DK, Stevens G, Scott LE, Mendelow BV, Stevens W (2002b) The challenge of laboratory monitoring of HIV. S Afr Med J 92:248
Guan M (2007) Frequency, causes, and new challenges of indeterminate results in western blot confirmatory testing for antibodies to human immunodeficiency virus. Clin Vaccine Immunol 14:649–659
Huff B (2001) Low cost diagnostics. GMHC Treat Issues 15:1–4
Huh D, Gu W, Kamotani Y, Grotberg JB, Takayama S (2005) Microfluidics for flow cytometric analysis of cells and particles. Physiol Meas 26:R73–R98
Lewin SR, Vesanen M, Kostrikis L, Hurley A, Duran M, Zhang L, Ho DD, Markowitz M (1999) Use of real-time PCR and molecular beacons to detect virus replication in human immunodeficiency virus type 1-infected individuals on prolonged effective antiretroviral therapy. J Virol 73:6099–6103
Lin CC, Wang JH, Wu HW, Lee GB (2010) Microfluidic immunoassays. J Assoc Lab Automat 15:253–274
Lui C, Cady NC, Batt CA (2009) Nucleic acid-based detection of bacterial pathogens using integrated microfluidic platform systems. Sensors 9:3713–3744
Mellors JW, Munoz A, Giorgi JV, Margolick JB, Tassoni CJ, Gupta P, Kingsley LA, Todd JA, Saah AJ, Detels R, Phair JP, Rinaldo CR Jr (1997) Plasma viral load and CD4+ lymphocytes as prognostic markers of HIV-1 infection. Ann Intern Med 126:946–954
Monzon OT, Paladin FJE, Dimaandal E, Balis AM, Samson C, Mitchell S (1992) Relevance of antibody content and test format in HIV testing of pooled sera. AIDS 6:43–48
Moon S, Keles HO, Ozcan A, Khademhosseini A, Haeggstrom E, Kuritzkes D, Demirci U (2009) Integrating microfluidics and lensless imaging for point-of-care testing. Biosens Bioelectron 24:3208–3214
O’Brien WA, Hartigan PM, Martin D, Esinhart J, Hill A, Benoit S, Rubin M, Simberkoff MS, Hamilton JD (1996) Changes in plasma HIV-1 RNA and CD4+ lymphocyte counts and the risk of progression to AIDS. N Engl J Med 334:426–431
O’Brien WA, Hartigan PM, Daar ES, Simberkoff MS, Hamilton JD (1997) Changes in plasma HIV RNA levels and CD4+ lymphocyte counts predict both response to antiretroviral therapy and therapeutic failure. Ann Intern Med 126:939–945
Passing H, Bablok W (1983) A new biometrical procedure for testing the equality of measurements from two different analytical methods. Application of linear regression procedures for method comparison studies in clinical chemistry, Part 1. Clin Chem Lab Med 21:709–720
Radisic M, Iyer RK, Murthy SK (2006) Micro- and nanotechnology in cell separation. Int J Nanomedicine 1:3–14
Robinson JE, Holton D, Liu J, McMurdo H, Murciano A, Gohd R (1990) A novel enzyme-linked immunosorbent assay (ELISA) for the detection of antibodies to HIV-1 envelope glycoproteins based on immobilization of rival glycoproteins in microtiter wells coated with concanavalin A. J Immunol Methods 132:63–71
Rodriguez WR, Christodoulides N, Floriano PN, Graham S, Mohanty S, Dixon M, Hsiang M, Peter T, Zavahir S, Thior I, Romanovicz D, Bernard B, Goodey AP, Walker BD, McDevitt JT (2005) A microchip CD4 counting method for HIV monitoring in resource-poor settings. PLoS Med 2:663–672
Shi W, Kasdan HL, Fridge A, Tai YC (2010) Four-part differential leukocyte count using flow cytometer. In: Proceedings of the 23rd International Conference on Micro Electro Mechanical Systems, Hong Kong, China
Shortman K, Wu L (1996) Early T lymphocyte progenitors. Annu Rev Immunol 14:29–47
Strauss K, Hannet I, Engels S, Shiba A, Ward DM, Ullery S, Jinguji MG, Valinsky J, Barnett D, Orfao A, Kestens L (1996) Performance evaluation of the FACSCount system: a dedicated system for clinical cellular analysis. Cytometry 26:52–59
Thorslund S, Larsson R, Bergquist J, Nikolajeff F, Sanchez J (2008) A PDMS-based disposable microfluidic sensor for CD4+ lymphocyte counting. Biomed Microdevices 10:851–857
Toner M, Irimia D (2005) Blood-on-a-chip. Annu Rev Biomed Eng 7:77–103
Tsoukas CM, Bernard NF (1994) Markers predicting progression of human immunodeficiency virus-related disease. Clin Microbiol Rev 7:14–28
Voldman J (2006) Electrical forces for microscale cell manipulation. Annu Rev Biomed Eng 8:425–454
Wang CH, Lee GB (2006) Pneumatic-driven peristaltic micropumps utilizing serpentine-shape channels. J Micromech Microeng 16:341–348
Wang YN, Kang Y, Xu D, Chon CH, Barnett L, Kalams SA, Li D, Li D (2008) On-chip counting the number and the percentage of CD4+ T lymphocytes. Lab Chip 8:309–315
Wu MH, Huang SB, Lee GB (2010) Microfluidic cell culture systems for drug research. Lab Chip 10:939–956
Yang SY, Hsiung SK, Hung YC, Chang CM, Lee GB (2006) A cell counting/sorting system incorporated with a microfabricated flow cytometer chip. Meas Sci Technol 17:2001–2009
Yang SY, Lin JL, Lee GB (2009a) A vortex-type micromixer utilizing pneumatically driven membranes. J Micromech Microeng. doi:10.1088/0960-1317/19/3/035020
Yang YN, Hsiung SK, Lee GB (2009b) A pneumatic micropump incorporated with a normally-closed valve capable of generating a high pumping rate and a high back pressure. Microfluid Nanofluidics 6:823–833
Zúñiga-Pflücker JC, Lenardo MJ (1996) Regulation of thymocyte development from immature progenitors. Curr Opin Immunol 8:215–224
Acknowledgment
This work is funded by the National Science Council under grant NSC-98-2218-E-006-234 and DOH99-TD-B-111-102.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, JH., Wang, CH., Lin, CC. et al. An integrated microfluidic system for counting of CD4+/CD8+ T lymphocytes. Microfluid Nanofluid 10, 531–541 (2011). https://doi.org/10.1007/s10404-010-0687-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10404-010-0687-z