Abstract
Background: Treatment of deep endometriosis involving the bowel is controversial. There is limitation of medical treatment. Several surgical techniques are used. All of them are associated with potential intraoperative complications and long-term hazards for the bladder, bowel and sexual function. Objectives: This study seeks to review systematically different types of surgical treatment of bowel endometriosis which include mucosal skinning (shaving), disc excision, and segmental resection. The review includes the number of participants, histology, symptomatology, preoperative assessment, types and access of surgery, complications, hospital stay, length and way of follow up, symptom improvement, recurrence, and effects on fertility. Study strategy: All published articles on surgical treatment of endometriosis (shaving, rectovaginal endometriosis, disc excision, and segmental resection), identified through MEDLINE, EMBASE, CINAHL, and Cochran library during 1970–2011. Grey literatures were searched as well. Selection criteria: The terms ‘endometriosis’, ‘bowel’, surgical, and complications were used. Articles describing 50 patients or more who had bowel surgery for endometriosis were only included. Data collection and analysis: Data did not permit a meaningful meta-analysis. Main results: We analyzed 36 articles after thorough literature search. It described 2,414 of mucosal skinning/rectovaginal endometriosis, 381 of disc excision, and 2,728 of bowel resection for deep endometriosis involving the bowel. The indication for surgery was stated in most of the studies. Histology was confirmed in the majority; however, completeness of the excision was stated in few articles. There is significant improvement of symptoms with all types of surgery. Complications were higher in segmental resection than conservative surgery (shaving and disc excision) especially leakage and fistula formation. The duration of surgery and hospital stay was shorter in conservative surgery unless there were complications or if associated with other surgeries. Fertility outcome was favourable in all. The recurrence and reoperation rate was higher in one study only in the shaving group, but otherwise was comparable to the resection group. Conclusion: There was no difference in the outcome between different types of surgery which indicates that we should adopt the conservative surgery if possible. The heterogeneity of the studies makes it difficult to do any valuable statistical analysis. There should be standardization in clinical trials evaluating bowel surgery for endometriosis.
Similar content being viewed by others
Introduction
Endometriosis is a gynaecological disease defined by histological presence of endometrial glands and stroma outside the uterine cavity, most commonly implanted over visceral and peritoneal surfaces within the female pelvis [1].
Deep endometriosis is defined as adenomyosis externa, mostly presents as a single nodule larger than 1 cm in diameter, in the vesicouterine fold or close to the lower 20 cm of the bowel [2]. It is surgically challenging when involving organs, such as the bowel, bladder, or ureter [3, 4].
Sites of endometriosis affecting the bowel
The term ‘bowel endometriosis’ should be used when endometrial-like glands and stroma infiltrate the bowel wall reaching at least the subserous fat tissue or adjacent to the neurovascular branches (subserous plexus). As initially suggested by Chapron et al. [5], endometriotic foci located on the bowel serosa should be considered peritoneal and not bowel endometriosis. The most frequent location of bowel involvement with endometriosis is the sigmoid colon (over 65 % of the cases), followed by the rectum, the ileum, the appendix, and the caecum [6]. Gastric and transverse colonic diseases are also reported by Remorgida et al. [7].
Why it is important to do this review
Endometriosis generally affects otherwise healthy young women with high expectations of well-being and quality of life. In this population, complications and side effects of surgery are not easily tolerated, and the recurrence of symptoms can be especially frustrating. It is doubtful that the primary surgery, however beautifully and skilfully performed, would remove all viable endometriotic ‘cells’ or microscopic endometriotic lesions invisible to the naked eyes under the laparoscopy and eliminate recurrence altogether. Theoretically, just one single viable cell can, under suitable milieu and conditions, propagate and grow into a colony [8]. Conceivably, recurrence after surgery occurs because of in situ regrowth of residual endometriotic lesions or cells not completely removed in the surgery, growth of microscopic endometriosis undetected at surgery, or the development of de novo lesions, or a combination of these.
Obviously, the recurrence rate varies with the definition of recurrence (subjective feeling of pain or more objective clinical/instrumental measurements), type of endometriosis, methods of surgery or post-operation intervention, if any, disease severity, type of hospital where the surgery is performed, and the skills of the surgeons who performed the surgery, among many known or potential factors that may influence the recurrence risk. Although it is self-evident that the recurrence rate increases as the length of follow-up, occasionally some studies, which involve patients recruited consecutively during a certain time window, only report an ‘overall recurrence rate’, giving few clues to the duration of follow-up. This kind of ‘recurrence rate’ is next to useless when making comparison among studies since it simply means little if anything without specifying the time elapsed since surgery [8].
In the experience of Anaf et al. [9], as well as in the available literature, the presence of a rectovaginal endometriotic nodule is always associated with pelvic pain, dysmenorrhoea, and/or deep dyspareunia [8, 10–13]. However, Fedele et al. [14] followed 88 patients with untreated asymptomatic rectovaginal endometriosis for 1 to 9 years. Pain symptoms and clinical and transrectal ultrasonographic findings were evaluated before and every 6 months after diagnosis. Progression of the disease and appearance of specific symptoms rarely occurred in patients with asymptomatic rectovaginal endometriosis.
Medical management of deep endometriosis (DIE) with colorectal extension (with non-steroidal anti-inflammatory drugs, oral contraceptives, gestogens, antigestogens, or GnRH agonists) is based on suppression of the symptoms, is not curative, and is often associated with significant side effects [15–17]. It is not clear if the medical management approach prevents disease progression, especially in more severe cases of endometriosis with colorectal extension. In addition, discontinuation of this therapy commonly results in recurrence [18].
De Cicco et al. [4] struggled to find good quality studies with accurate reports of the essential information needed to fully appreciate the risks associated with segmental resection for endometriosis. In the studies they reviewed, the majority was retrospective case series, with only four of the 30 studies presented containing more than 100 participants. Indeed, 77 % of the studies included contained fewer than 50 participants .What they do not know from these smaller studies is whether the reported cases reflect the complication rate during the surgeons learning curve. As the major complications rate vary considerably (from 0 % to 48 %), it is likely that the results are heavily influenced by the current experience of the surgeons. It may be the higher morbidity reported in the smaller studies reflects the true situation in units only performing few cases a year. Importantly, there are no reports on fertility rates in women who experienced severe complications, such as faecal peritonitis, which is likely to have resulted in significant adhesive disease.
Paya et al. [19] in their review of surgical treatment of rectovaginal endometriosis concluded that although the studies published to assess the effect of different surgical techniques on the treatment of rectovaginal endometriosis showed a great heterogeneity in their characteristics and methodology, we can say that whenever technically possible, the more conservative techniques, shaving, and discoid intestinal resection would be recommended since they present a lower rate of complications with similar recurrence and greater rates of gestation. In relation to the surgical approach, two main groups can be observed: those who propose a more aggressive approach and tend to defend the systematic intestinal resection under the premise that a more radical approach would be more effective (segmental resection of the rectum and/or sigmoid colon) and those that argue for a more conservative approach basing their argument on the lack of scientific evidence of better results with more radical techniques and the association of these techniques with higher-long-term morbidity and a lower quality of life for patients(shaving of the rectal, disc excision of the anterior rectal wall).
So what advice could we sensibly give women who need to decide on whether they opt for surgical treatment of lower bowel endometriosis? Until we have robust data, it is difficult to provide women with accurate information about the surgical risk. Based on the larger studies in the review by De Cicco et al. [4], we can advise that the chances of having a major surgical complication are probably around 10 % in the bowel resection.
Wright and Ballard [18], continue to remain unclear about the efficacy of rectal surgery for endometriosis.
Yet, in order for women to be able to make an informed choice about whether to have bowel surgery for endometriosis, it is essential that they have accurate information about both the benefits and risks associated with the procedure. We will try in this review to explore the surgical option by looking at large studies.
Methods
We included only the randomized, retrospective or prospective studies with 50 patients or more of bowel surgery for endometriosis which include excision of rectovaginal septum, mucosal skinning, disc excision, and bowel resection. The route of surgery could be laparotomy, laparoscopy, with or without the help of vaginal or transanal approach. The outcome measures include:
-
1.
Significant complications ( anastomotic leaks, stenosis of anastomosis, rectovaginal fistula, vesicovaginal fistula, bowel dysfunction, bladder dysfunction, ureteric injury, haemorrhage necessitating blood transfusion, colostomy, or ileostomy and reoperation).
-
2.
Improvement of symptoms related to endometriosis (pelvic pain, dyspareunia, dyschezia, and dysmenorrhoea). Assessment of improvements can be either clinically, questionnaire, or visual analogue scale. Quality of life after surgery will be looked at as well.
-
3.
Fertility outcome.
We searched the electronic database such as MEDLINE (from 1970 to the end of 2011), CINAHL (from 1981 to the end of 2011), EMBASE (from 1980 to end of 2011), and Cochrane library for relevant studies. The following keywords: endometriosis, bowel, surgical, and complications were searched. The Biotechnology Research Abstracts and all registers included in the meta Register of Controlled Trials (mRCT) were also searched.
Grey literature search was performed using the SIGLE system (System for Information on Grey Literature in Europe). The references of retrieved key articles, together with the proceedings of relevant conferences, were hand-searched to identify other potentially eligible studies for inclusion in the analysis missed by the initial search or any unpublished studies. We also searched the index to thesis. The review will include only the studies published in English.
Study characteristics
-
Setting:
-
Single or multicentre
-
Location
-
Timing and duration
-
-
Size:
-
Number of included women
-
Number of women lost in follow-up
-
Number of women analyzed
-
-
Duration and way of follow-up
-
Type of surgery
-
Duration of surgery
-
Hospital stay
-
Complications
-
Fertility issues
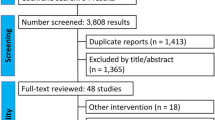
Figure 1 shows the research pathway.
Results
From 1987 to December 2011, 36 articles (5539 patients) were analysed describing 2,414 of mucosal skinning/rectovaginal septum, 381 of disc excision, and 2,728 of bowel resection for deep endometriosis involving the bowel [20–55] (Table 1). There is progressive shift from laparotomy to laparoscopy. Around half of the studies in this review (19 studies) were between 2007 and 2011.
We will use the reference's number for description rather than the authors’ names if required. The case series which deal with shaving only [27, 28, 34, 47], will be named as ‘the shaving group’, and those which discuss the bowel resection only [22, 25, 26, 30, 36, 37, 40, 42, 49, 51] will be named as ‘the resection group’. The rest of the studies will be called 'the mixed group'. There were no clear subdivisions between different types of surgery in the latter group except in these studies [23, 31, 35, 38, 39, 43, 45]. Cases with disc excision in the previous studies within the mixed group were analyzed separately (Fig. 2). Complications rate in this group varied from 0 % to 23 %. Recurrence was only discussed in [23] (3 rectal endometriosis and 7 pelvic endometriosis). Fertility after disc excision was 11 % which was mentioned only in one case series [43].
Types of the studies
There were 15 retrospective and 20 prospective studies in this review. The only randomized study in this systematic review was in study [26]. It was a comparison between laparoscopic assisted and open colorectal resection.
Route of surgery
Laparotomy was the only access of surgery in these studies [21]: (130) [24], (77) [29], (100) [54], and (163). A combination of laparoscopy and laparotomy was the route of surgery in these studies [23, 26, 27, 32, 33, 35, 52, 53, 55]. In the rest of the studies, laparoscopy was the primary access of surgery (23 studies). There were conversions to laparatomy in 103 cases out of 4,946(2.1 %). In the shaving group, all the procedures were laparoscopic. There were 3 conversions out of 1,181 laparoscopies (0.25 %). All the studies in the resection group except [26, 29] (50 % had laparotomy), laparoscopy was the only surgical route. Conversions were done in 35 out of 1,608 laparoscopies (2.2 %) [Table 2].
Histology examination
It was not clearly stated that the specimen removed was sent for histology, in 13 case series [22, 23, 26, 31, 34, 35, 37, 40, 44, 47, 49, 52, 53] out of 36 studies(36 %) [Table 3].
The completeness of the excision was discussed only in 4 articles [25, 29, 36, 53]. It was reported as complete in the last three case series. Darai et al. [25] stated that the completeness of excision was confirmed in 69/70 patients.
Site of the lesion
The rectum (or the rectovaginal septum) was involved in all the studies. The colon (mainly the sigmoid), appendix, and the terminal ileum were also involved in addition to the rectum in some studies to a variable degree.
Symptomatology
Pelvic pain, dysmenorrhoea, dyspareunia, infertility, dyschezia, rectal bleeding, and change of bowel habits are the most common symptoms of endometriosis and the cause of referral. Studies [38, 48, 55] did not mention what the symptoms that the patients were referred with.
Preoperative assessment
It was not mentioned in 3 studies [21, 31, 52] (Table 4). Laparoscopy was used as an initial assessment in these studies [23, 33, 36, 39, 43, 47, 50, 53–55]. Visual analogue was used in four studies as part of the preoperative assessment [40, 41, 46, 51]. Other methods of preoperative assessment included in the study include transvaginal/endorectal ultrasound, colonoscopy/sigmoidoscopy, double contrast barium enema, MRI, and CT scan. CA125 was requested in only one study [42].
Operation time and hospital stay
The shaving group got less operating time (69–178 min) and hospital stay (1.5- 2.8 days), than the resection group (181–390 min) and (3.1–9 days), respectively (Tables 5, 6, and 7).
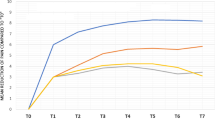
Effect of surgery on symptoms
Pelvic pain
The effect of surgery was not mentioned in these studies [35, 38, 40, 42, 45, 48, 49, 51, 54, 55]. The improvement of pain, either partial or complete varied between 64 % [53] to 97 % [43]. In the shaving group, the improvement was between 88 % and 96 %. In the resection group, there is no comment in these case series [40, 41, 49, 51], while the others [28, 29, 37] showed improvement between 90 % and 96 % or significant improvement [22, 25, 26, 30].
Dysmenorrhea improvement
The effect was not mentioned in these studies [21, 24, 34, 35, 37, 38, 40, 43–45, 47, 49–51, 53–55]. In the other series, the improvement varies between 28 % and 100 %. In the shaving group, it was mentioned in two studies only [27, 28] and the improvement was between 91 % and 100 %.
Rectal bleeding
This was only mentioned in 4 studies [20, 21, 30, 36]. Rectal bleeding disappeared after surgery in 3 studies [20, 21, 36] and remained the same in the fourth [30]. It was not an issue in the shaving group.
Dyspareunia
There was no direct comment on dyspareunia in these studies [24, 34, 35, 38, 40, 45, 47–49, 51–55]. In the other studies, all the patients showed improvement, which was expressed either as percentage (70–100 %), using the score of 10 to compare between the preoperative and postoperative condition, or using the expression of significant improvement. In the shaving group the improvement varies between 91 % and 100 % [28, 29].
Dyschezia
There was no direct comment on dyschezia in these studies [21, 24, 27, 33–35, 37, 38, 40, 41, 43–45, 47–49, 51–55]. Improvement varied between 59 % and 100 %. In the shaving group, the improvement was 91.2 % [28].
Quality of life and way of follow-up
Quality of life score was carried out in these studies [22, 26, 30, 33, 39, 41]. SF-36 health status questionnaire was used in [22, 26, 30]. EQ-5D quality of life score was used in [33]. All these assessments showed significant improvement.
In the shaving group, QOL was not assessed in any study. In the resection group, QOL was assessed in 3 case series [22, 26, 30].
Recurrence of endometriosis and reoperation
Fifteen case series reported recurrence of endometriosis [20]: (4 %) [23], (4.7 %) [26], (5 %) [29], (7.8 %) [32], (30 %) [35], (5 %) [36], (6.6 %) [41], (2–7 %) [42], (8.4 %) [43], (8.4 %) [44], (4.3 %) [47], (50 % in 2nd laparoscopy–67 % in 3rd laparoscopy) [52], (48 %) [53], (15 %), and [54](4.9 %).
Reoperation reported in these series [20]: (2.4 %) [27], (1.2 %) [28], (2.4 %) [32], (25 %) [33], (6 %) [35], (5 %) [20], (4 %) [40], (10.4 %) [41], (9 %) [42], (3.8 %) [43], (21 %) [44], (16 %) [46], (19.4 %) [47], (36 %) [50], (2.3 %) [52], (10 %) [53], (36 %), and (20 %) [54].
The recurrence in the shaving group was 5 % [27], 7.8 % [28], 50–67 % [47], while reoperation rate was 1.2 % [27], 2.4 % [28], and 36 % [47]. In the resection group, the recurrence rate varied between 6.6 % and 8.4 %. The reoperation rate was 3.8 % and 10.4 %.
Follow-up
There were no data on the follow up in 4 studies [38, 48, 54, 55]. In the rest of the studies, there was wide range of duration of follow up which varied between 1 month and 11 years. The follow-up duration in the shaving group [27, 28, 34, 47] varied between 1 year and 11 years. All the patients were followed up in these studies [20–22, 24–26, 28, 29, 31, 34, 37, 40, 41, 45, 49, 51, 53]. In the rest of the studies, the number of patients who were followed up varied between 27 % and 98 %.
Fertility outcome
There were data of the effect of surgery on the fertility in 16 studies (44 %) [21, 24, 25, 28, 32, 34, 36, 37, 41–43, 46, 47, 51, 54] (Table 8). The pregnancy rate was between 11.5 % and 84 %. The success rate includes both cases of spontaneous pregnancy and assisted conception. There were 640 pregnancies in 1,232 women (52 %). In the shaving group [28, 34, 47], the pregnancy rate was 84 %, 57 %, and 74 %, respectively. In the resection group, it was recorded in 5/11 (45 %). The success rate was between 11.5 % and 65 %.
Complications
The intraoperative and postoperative complications of surgery were reported in 34 articles (Table 9). The overall complication rate after surgery was 13.9 % (744/5349). It varied from 1.2 % to 40 %. Leakage occurred in 38/744 cases (5.1 %), fistula 93/744 (12.5 %), bowel obstruction/stricture 55/744 (7.3 %), bladder dysfunction 171/744 (23 %), and bowel dysfunction 55/744 (7.4 %). In the shaving group, the complications rate was 2.8 %. In studies in which segmental resection was the only surgical route [22, 25, 26, 29, 30, 36, 40, 42, 49, 51], the complications rate was 447/1,512 (29.6 %). Keckstein and Weisinger [37] and Tarjanne et al. [52] were excluded as the complications were not discussed (190 patients). The complications include the minors and majors.
Stoma formation
Colostomy or ileostomy can be done prophylactically before bowel resection (Table 10). In some studies, it was done as part of the treatment of complications of bowel surgery. In the shaving group, there was no colostomy or ileostomy in 3 studies [27, 28, 34] and there was no comment in the fourth [47]. In the resection group, there were no data in 2 studies [26, 37] and no stoma in another 2 studies [22, 51]. There were stoma formations in the rest of the studies in the same group [25, 29, 30, 36, 40, 42, 49]. In the disc excision subgroup, there was stoma formation in all of them [23, 31, 35, 38, 39, 44, 45].
Discussion
There is a need for strong and energetic debate to weigh up the benefits and risks of debulking surgery (shaving and disc excision) and radical surgery (bowel resection).
Unfortunately, we have only one randomized trial [26] in this study, comparing laparoscopic versus open colorectal resection for endometriosis. Ideally other randomized studies, one to compare medical and surgical treatment, and the other, to evaluate different types of surgical treatment, are required. To avoid losing large case series, e.g [27, 38], we included 15 retrospective studies (42 %), in spite of the limitations of this type of research.
As we have different types of studies describing varieties of surgeries, with different techniques, done by gynaecologists, surgeons or both, with different ways and time of follow-up, we should interpret the results with caution. De Cicco et al. [4] stated that it would greatly facilitate and permit meta-analysis if journals agreed on the format of reporting and when individual data could be submitted.
All the symptoms significantly improved after surgery. The follow-up in some studies was up to 11 years, and on the other hand, it was just a month in some. It does not look that there is difference between different types of surgery.
Type of surgery
Laparoscopy is taking over from open surgery. It allows accurate diagnosis due to improved visualization of pelvic structures as well as better access to the deep pelvis in cases of rectovaginal septum involvement [53]. Laparoscopy was the only route in the shaving group. The conversion rate in all laparoscopies was quiet low (2.1 %). It is lower in the shaving group (0.25 %) rather than the resection group (2.2 %). This is to add to the advantages of conservative surgery over resection.
Histology confirmation
Histological examination is essential to confirm the diagnosis and to exclude other pathology. Excision should be complete in order to achieve maximal pain relief and minimal recurrence. However, De Cicco [4] stated that there is no data to substantiate this. Histology was reported in 23 studies (64 %) and confirmed in 41–100 % of the specimen. However, there were no data about the completeness of the excision. Absence of clear documentation on the histology is considered as a weakness of the study. Kavallaris et al. [56] noted that a distance of 2 cm between the margin and the main lesion was not sufficient to obtain endometriosis free margins in more than one-third of the patients. Furthermore, margins of the resected bowel specimen were still positive for endometriosis in 6 patients (19 %) after bowel resection was performed in an area with a distance of at least 3 cm from the edges of the palpated lesions, free of any indurations at manual palpation, and free of any serosal or muscular visible endometriosis implant [56]. The same was discussed by Anaf et al. [57, 58] and Roman et al. [59] with a positive margin around 10 %. Neural metastasis hypothesis provides an explanation. This might explains the recurrence of symptoms and endometriosis in segmental resection.
Complications
The overall complication rate after surgery was 13.9 %. In the shaving group, the complications rate was 2.8 % while it was 29.6 % in the resection group. It is obvious that conservative surgery carries low risk. Although most of it was related to bowel surgery, additional surgery, such as ureterolysis, uterosacral ligament resection, and hysterectomy, might contribute as well. Opening of the vagina contributes to the complication, in spite being not always reported. This pleads for the introduction of a systematic protective colostomy in case of concomitant vaginal and rectal resection as already applied in some studies [39]. Additionally, extensive electro coagulation can lead to necrosis of the posterior vaginal cuff with a higher risk for rectovaginal fistulae and abscesses [30].
Pelvic denervation can lead to urine retention, de novo dysuria, and sexual dysfunction. Nerve sparing technique is required, in spite that it is not always possible if there are large nodules with bilateral extension. Care must always be taken to preserve the pelvic autonomic nerves, as they are the pathway for the neurogenic control of rectal, bladder, and sexual arousal function. The identification of the inferior hypogastric nerve and plexus was feasible and performed in acceptable operative time [60]. They believe that a trained laparoscopic surgeon should have a good knowledge not only of the retroperitoneal anatomy, but also of the pelvic neuro-anatomy as this qualification could prohibit long-term bladder and voiding dysfunction.
The shaving technique allows preservation of the nerves by avoiding deep lateral rectal dissection (necessary for recto sigmoid resection). Indeed, lateral dissection is mandatory only in the case of lateral extension of the disease with ureteral involvement and, even in this case, rarely involves dissection of the postero-lateral compartment of the rectum [61]. The case series of Kondo et al. [20] suggests that the major complication rate is likely to be lower in women undergoing a mucosal skinning procedure relative to those having a segmental resection. Women also need to be advised that the complication rate may be higher in units that have relatively little experience of this surgery and, as recommended by the RCOG, the surgeon should quote his/her own complication rate.
Bladder dysfunction constitutes 23 % of the whole complications followed by fistula formation (12.5 %). Anastomotic leakage is a feared complication of colorectal surgery and if unrecognized may be associated with a mortality as high as 39 %. Minor cases may also cause late functional problems [50]. The functional problems are less frequent after a sigmoid than after a rectum resection. As the discoid resection is easier at the level of the rectum, Ret Davalos et al. [62] would suggest an avoidance of resection for lower lesion, if possible. Surgeons should work hard to minimize these serious complications.
Follow-up
The wide variation in the follow-up and the high proportion of the patients who lost in the follow-up are considered to be weakness in this study. There were no follow-up in four studies [38, 48, 54, 55] and very short follow-up (between 1–3 months) in another four studies [31, 40, 45, 49]. All the participants were followed-up in 18 studies only. Study [53] reported at 35 months follow-up that 61 women (36 %) required further surgery for pain. The average time between primary and repeat surgery was 16 months. This explains the value of long-term follow-up. The value of surgery could be overestimated by short follow-up.
Recurrence
It is difficult to distinguish between residual and recurrent disease [63]. Excluding Reich et al. [47], the improvement, recurrence, and reoperation rate are comparable between the two groups, but with higher rate of complications in the resection group.
It is difficult to gauge the proportion of women suffering from pelvic pain due to genuine recurrence of endometriosis and those with postoperative adhesions related to severe complications, such as pelvic abscesses or peritonitis [61]. Resection of deep nodular endometriosis, which is innervated abundantly by sensory C cholinergic and adrenergic nerve fibres, as recently demonstrated [64].
Investigations confirmed high nerve fibre density in deep infiltrating lesions, mainly observed near the intestinal lining. Considering that in bowel resection, the margin are not free in around 10 % [57, 58], it should not be undertaken as first line therapy ,but as secondary-line approach in the case of recurrence with stenosis >80 % after shaving [61].
Paya et al. [19] did a comparative study between different surgeries for rectovaginal endometriosis in four case series (see the table below). All of them are observational studies in which the treatment option was not decided randomly; rather, it was made in terms of clinical criteria or in consensus with the patients. Two studies were part of our systematic analysis [23, 43]. Although some of the outcomes and the way they were assessed are not directly comparable between papers, one can see a tendency that points to a similar symptomatic improvement among the different techniques and a greater rate of surgical complications among the most radical approaches.
The results of the discoid resection analyzed in comparative studies show that the rate of severe complications remains low; the symptomatic improvement stands around 90 %, and the rate of relapse between 5 % and 14 % (Table 11).
More prospective follow-up studies with large sample sizes and clear definitions of endometriosis recurrence (using life table analysis to calculate the cumulative endometriosis recurrence rate) are needed to compare endometriosis recurrence between patient groups receiving different surgical techniques for the treatment of endometriosis with colorectal lesions.
Fertility
The association between endometriosis and infertility is still undefined and there is no consensus on the best treatment options for various clinical conditions [67]. On the basis of three studies [68–70], there seems to be a negative correlation between the stage of endometriosis and the spontaneous cumulative pregnancy rate after surgical removal of endometriosis, but statistical significance was reached only in one study [70].
In our study, we looked at the fertility for women wished to conceive after surgery, either with a documented infertility or not. It was difficult to do a separate analysis of the effect of surgery on infertile women because of the absence of clear documentation or definition of infertility in some studies. Fertility was discussed in 44 % of the studies with a pregnancy rate between 11.5 % and 84 %. The highest was in the shaving group [38].
Rectovaginal endometriosis is a benign condition with limited tendency to progress [32]. In a comparative non randomized study, between resection of rectovaginal endometriosis and expectant treatment, the results did not suggest that excision of rectovaginal plaques improves the incidence of pregnancy and reduces time to conception in women with endometriosis associated infertility [67]. There is no randomized controlled study or met analysis available to answer the question of whether surgical excision of moderate to severe endometriosis enhances pregnancy rate. However, other studies suggest that complete removal of deep infiltrating endometriosis potentially improve fertility [40]. Even in the subfertile population, a good spontaneous pregnancy rate can be achieved after conservative surgery. The spontaneous pregnancy rate in Gordts 2013 study [71] was 50 % in his fertility unit.
If infertility is of primary concern, the lower complication rates and better chance for fertility offered by the less invasive shaving approach justifies initially using this technique [43]. The highest pregnancy rate (84 %) in our study was in study No [28], in which shaving technique was only used. The pregnancy rate in the shaving group (57–84 %) is comparable to that of the resection group (11.5–65 %) [Table 8].
Donnez and Squifflet [28] explained the high pregnancy rate to the following:
-
Lesions are resected without extension or lateral dissection, frequently associated with subsequent adhesions in case of bowel resection.
-
Nodules are not associated with severe peritoneal endometriosis or ovarian endometriomas.
-
Use of the combined technique, when ovarian endometrioma are present, as demonstrated by Donnez et al. [72].
Meuleman et al. [73] stated that the fertility wish of patients with advanced endometriosis with colorectal extension is underestimated in the papers reviewed. The indication of infertility with or without pain is only 22–36 % of all patients included in these papers. Most patients have a combined problem of pain and unfulfilled or uncompleted child wish, which may be formulated by the patient passively (wish for preservation/restoration of fertility during surgery, without well-defined child wish in the near or distant future). Furthermore, it is important to realize that many women with pelvic endometriosis and colorectal extension have been told for many years that they will never become pregnant as a result of their disease. Additionally, before surgery these women are in pain, implying that their first concern is how to stop the pain, rather than a child wish. In these women, child wish may only emerge after a successful removal of the endometriosis and pain reduction.
Life table analysis was used to calculate the cumulative pregnancy rate in only 4 out of 16 (25 %) studies reporting fertility outcome [24, 34, 41, 51]. This is surprising in view of the fact that it has been generally accepted that life table analysis is the best way to calculate fertility outcome while controlling for the duration of follow-up and dropout rate for each patient. Overall, this observation supports the need for prospective follow-up studies with sufficient duration of follow-up and complete follow-up of all operated patients.
Quality of life (QOL)
As we have shown before, there was wide range of methods of follow up to assess the outcome including QOL. SF-36 and EQ-5D were used to measure QOL. The EQ-5D is a short-generic patient-rated questionnaire for subjectively describing and valuing health-related quality of life; it is often used as an outcome measure in both clinical and health care services research. The EQ-5D questionnaire comprises five questions (items) relating to current problems in the dimensions mobility', 'self-care', 'usual activities', 'pain/discomfort', and 'anxiety/depression. Responses in each dimension are divided into three ordinal levels coded (a) no problems, (b) moderate problems, and (c) extreme problems. The SF-36 is composed of 36 questions that estimates a total of 8 domains of physical health (physical functioning, role physical, bodily pain, general health) and mental health (vitality, social functioning, role-emotional, and mental health). It may be applied to individuals 18 years of age up to advanced ages, with different medical conditions, and undergoing different types of treatment.
There were improvement in QOL in the four studies using SF-36 and EQ-5D. Three of them were from the resection group and the other one from the mixed group. The SF-36 questionnaire was applied before and after surgery in Dubernard et al. [30]. These scores were lower after surgery in 11 cases (7.3 %). In two patients, the poorer scores after surgery were a result of the persistence of abdominal pain after treatment, whereas the other patients went on to have some form of clinical complication that did not appear to be directly associated with the laparoscopic intervention alone. Bassi et al. [22] stated that patients reported deterioration both in bowel symptoms and in pain after surgery is attributed to post operative fibrosis. More and large studies with a long-term follow-up using the same validated QOL questionnaire are required to allow comparison between the different surgical techniques used and to confirm the positive impact of each type of surgery on the QOL.
Stoma formation
Obviously, having stoma is very embarrassing to any woman. She should feel that the gain is going to have from surgery is worthwhile, so she can cope with having stoma for some time. No recorded cases of stoma formation were in the shaving group but there were in all the disc excision subgroup and in 7 case series in the resection group. This again emphasizes the value of doing the minimum surgery needed, to get the best outcome at a cheap price.
Conclusion
Implications for practice
Most of the studies documented the clinical outcome for bowel surgery in deep endometriosis regarding postoperative complication rate and relief of symptoms. However, less than 50 % of the studies included data with respect to the recurrence rate, fertility outcome, and quality of life. It is difficult to estimate the actual pregnancy and recurrence rates in some studies because of the short-term follow-up. A patient who has been lost or not included in the follow-up is not necessarily cured, but has possibly moved to another area or turned to another gynaecologist because of the lack of satisfaction or complications.
There was no difference in the outcome between conservative surgery and bowel resection. It is important to make every effort to get the best result from the minimum number of surgical interventions. Precise preoperative diagnosis, advanced laparoscopic surgical skills, and multidisciplinary approaches are considered to be the baseline for successful treatment.
Further studies
We need to have standardization in the clinical trial regarding the methodology, outcome variables, and long-term follow-up. A definition should be used to record postoperative complications, document pelvic pain (dysmenorrheal, dyspareunia, chronic non-menstrual pelvic pain) and assess quality of life, fertility (pregnancy rate), and recurrence rate after surgery for endometriosis. Health professionals are encouraged to report unequivocally and completely in much needed prospective studies with large sample sizes and complete follow up of all patients for a reasonable period of time after surgery [4]. This enables meta-analysis to be done with a reliable conclusion and recommendation.
References
Giudice LC, Kao LC (2004) Endometriosis. Lancet 364:1789–1799
Koninckx PR, Martin DC (2012) Deep endometriosis: a consequence of infiltration or retraction or possibly adenomyosis externa. Fertil Steril 58:924–928
Koninckx PR, Martin D (1994) Treatment of deeply infiltrating endometriosis. Curr Opin Obstet Gynecol 6:231–234
De Cicco C, Corona R, Schonman R, Mailova K, Ussia A, Koninckx PR (2010) Bowel resection for deep endometriosis : a systematic review. BJOG 118:285–291
Chapron C, Fauconnier A, Viera M, Barakat H, Dousset B, Pansini V, Vacher-Lavenu MC, Dubuisson JB (2003) Anatomical distribution of deeply infiltrating endometriosis: surgical implications and proposition for classification. Hum Reprod 18:157–161
Redwine DB (2004) Intestinal endometriosis. In: Redwine DB (ed) Surgical Management of Endometriosis. Taylor & Francis, London, pp 157–173
Remorgida V, Ferrero S, Fulcher E, Ragni N, Martin DC (2007) Bowel endometriosis: presentation, diagnosis, and treatment. Obstet Gynecol Surv 62(7):461–469
Sun-Wei G (2009) Recurrence of endometriosis and its control. Hum Reprod Update 15(4):441–461
Anaf V, Simon PH, El Nakadi L, Fayt I, Buxant F, Simonart T, Peny MO, Noel JC (2000) Relationship between endometriotic foci and nerves in rectovaginal endometriotic nodules. Hum Reprod 15:1744–1750
Cornillie FJ, Oosterlynck J, Lauweryns M, Koninckx PR (1991) Suggestive evidence that endometriosis is a progressive disease, whereas deeply infiltrating endometriosis is associated with pelvic pain. Fertil Steril 55:759–765
Donnez J, Nisolle M, Casanas-Roux F, Bassil S, Anaf V (1995) Rectovaginal septum, endometriosis or adenomyosis:laparoscopic management in a series of 231 patients. Hum Reprod 10:630–635
Clayton RD, Hawe JA, Love JC, Wilkinson N, Garry R (1999) Recurrent pain after hysterectomy and bilateral salpingo-oophorectomy for endometriosis: evaluation of laparoscopic excision of residual excision. Br J Obstet Gynaecol 106(7):740–744
Porpora MG, Koninckx PR, Piazze J, Natili M, Colagrande S, Cosmi EV (1999) Correlation between endometriosis and pelvic pain. J Am Assoc Gynecol Laparosc 6:429–434
Fedele L, Bianchi S, Zanconato G, Raffaelli R, Berlanda N (2004) Is rectovaginal endometriosis a progressive disease? Am J Obstet Gynecol 191:1539–1542
Telimaa S (1988) Danazol and medroxyprogesterone acetate inefficient in the treatment of infertility in endometriosis. Fertil Steril 50:872–875
Marana R, Paielli F, Muzil L, Dell’Acqua S, Mancuso S (1994) GnRH analogs versus expectant management in minimal –mild endometriosis-associated infertility. Acta Eur Fertil 25:37–41
Vercellini P, Crosignani PG, Somigliana E, Berlanda N, Barbara G, Fedele L (2009) Medical treatment for rectovaginal endometriosis : what is the evidence ? Hum Reprod 24:2504–2514
Wright J, Ballard K (2011) The surgical management of rectovaginal endometriosis: plus ca change? BJOG 118(3):274–277
Paya V, Hidalgo-Mora JJ, Diaz-Garcia C, Pellicer A (2011) Surgical treatment of rectovaginal endometriosis with rectal endometriosis. Gynecol Surg 8:269–277
Alvez Pereira RM, Zanatta A, Lima Preti CD, Felipe de Paula FJ, Alvez da Motta EL, Serafini PC (2009) Should the gynaecologist perform laparoscopic bowel resection to treat endometriosis? Results over 7 years in 168 patients. J Minim Invasive Gynecol 16(4):427–429
Bailey HR, Ott MT, Hartendorp P (1994) Aggressive surgical management for advanced colorectal endometriosis. Dis Colon Rectum 37:747–753
Bassi MA, Podgaec S, Antonio D, D'Amico Filho N, Alberto Petta C, Abrao MS (2011) Quality of life after segmental resection of the rectosigmoid by laparoscopy in patients with deep infiltrating endometriosis with bowel involvement. Minim Invasive Gynecol 18:730–733
Brouwer R, Woods RJ (2007) Rectal endometriosis: results of radical excision and review of published work. Aust N Z J Surg 77:562–571
Coronado C, Randolph B, Franklin RR, Valdes CT, Lotez EC (1990) Surgical treatment of symptomatic colorectal endometriosis. Fertil Steril 53(3):411–416
Darai E, Ackerman G, Bazot M, Rouzier R, Dubernard G (2007) Laparoscopic segmental colorectal resection for endometriosis: limits and complications. Surg Endosc 21:1572–1577
Darai E, Dubernard G, Coutant C, Coutan C, Frey C, Rouzier R, Ballester M (2010) Randomized trial of laparoscopically assisted versus open colorectal resection for endometriosis: morbidity, symptoms, quality of life and fertility. Ann Surg 251:1018–1023
Donnez J, Nisolle M, Gillerot S, Smets M, Basil S, Casanas- Roux F (1997) Rectovaginal septum adenomyotic nodules: a series of 500 cases. Br J Obstet Gynaecol 104:1014–1018
Donnez J, Squifflet J (2010) Complications, pregnancy and recurrence in a prospective series of 500 patients operated on by the shaving technique for deep rectovaginal endometriotic nodules. Hum Reprod 25(8):1949–1958
Dousset B, Leconte M, Borghese B, Millischer AE, Roseau G, Akwright S, Chapron C (2010) Complete surgery for low rectal endometriosis. Long term results of a 100- case prospective study. Ann Surg 251:887–895
Dubernard G, Piketty M, Rouzier R, Houry S, Bazot M, Darai E (2006) Quality of life after laparoscopic colorectal resection for endometriosis. Hum Reprod 21(5):1243–1247
Duepree HJ, Senagore AJ, Delaney CP, Marcello P, Brady KM, Falcone T (2002) Laparoscopic resection of deep pelvic endometriosis with rectosigmoid involvement. J Am Coll Surg 195:754–758
Fedele L, Bianchi S, Zanconato G, Bettoni G, Gotsch F (2004) Long-term follow-up after conservative surgery for rectovaginal endometriosis. Am J Obstet Gynecol 190:1020–1024
Ford J, English J, Miles WA, Giannopoulos T (2004) Pain, quality of life and complications following the radical resection of rectovaginal endometriosis. BJOG 111:353–356
Hollett-Caines J, Vilos GA, Penava DA (2003) laparoscopic mobilization of the rectosigmoid and excision of the obliterated cul-de-sac. J Am Assoc Gynecol Laparosc 10(2):190–194
Jatan AK, Solomon MJ, Young J, Cooper M, Pathma-Nathan N (2006) Laparoscopic management of rectal endometriosis. Dis Colon Rectum 49(2):169–174
Kavallaris A, Chalvatzas N, Hornemann A, Banz C, Diedrich K, Agic A (2011) 94 months follow up after laparoscopic assisted vaginal resection of septum rectovaginale and rectosigmoid in women with deep infiltrating endometriosis. Arch Gynecol Obstet 283:1059–1064
Keckstein J, Wiesinger H (2005) Deep endometriosis, including intestinal involvement –the interdisciplinary approach. Minim Invasive Ther Allied Technol 14:160–166
Kondo W, Bourdel N, Tamburro S, Cavoli D, Jardon K, Rabischong B, Botchorishvili R, Pouly JL, Mage G, Canis M (2011) Complications after surgery for deeply infiltrating pelvic endometriosis. BJOG 118:292–298
Maytham G, Dowson H, Levy B, Kent A, Rockall TA (2010) Laparoscopic excision of rectovaginal endometriosis : report of a prospective study and review of the literature. Color Dis 12:1105–1112
Mereu L, Giacomo R, Stefano L, Barbieri F, Zaccoletti R, Fiaccavento A, Stepniewska A, Pontrelli G, Minelli L (2007) Laparoscopic treatment of deep endometriosis with segmental colorectal resection:short term morbidity. Minim Invasive Gynecol 14:463–469
Meuleman C, D'Hoore A, Van Cleynenbreugel B, Berks N, D'Hooghe T (2009) Outcome after mutidisciplinary CO2 laser laparoscopic excision of deep infiltrating colorectal endometriosis. Reprod Biomed Online 18:282–289
Minelli L, Fanfani F, Fagotti A, Rffo G, Ceccaroni M, Mereu L, Landi S, Pomini P, Scambia G (2009) Laparoscopic colorectal resection for bowel endometriosis; feasibility, complications, and clinical outcome. Arch Surg 144(3):234–239
Mohr C, Nezhat FR, Nezhat CH, Seidman DS, Nezhat CR (2005) Fertility consideration in laparoscopic treatment of infiltrative bowel endometriosis. JSLS 9:16–24
Nezhat F, Nezhat C, Pennington E (1992) Laparoscopic treatment of infiltrative rectosigmoid colon and rectovaginal septum by the technique of videolaparoscopy and the CO2 laser. Br J Obstet Gynaecol 99:664–667
Pandis GK, Saridogan E, Windsor AC, Gulumser C, Cohen RG, Cutner AS (2010) Short term outcome of fertility –sparing laparoscopic excision of deeply infiltrating pelvic endometriosis performed in a tertiary centre. Fertil Steril 93:39–45
Redwine DB, Wright JT (2001) Laparoscopic treatment of complete obliteration of the cul-de-sac associated with endometriosis; long term follow up of en bloc resection. Fertil Steril 76:358–365
Reich H, Mc Glynn F, Salvat J (1991) Laparoscopic treatment of Cul-de-sac Obliteration secondary to retrocervical deep fibrotic endometriosis. J Reprod Med 36(7):516–522
Riberiro PA, Rodrigues FC, Kehdi IP, Rossini L, Abdalla HS, Donadio N, Aoki T et al (2006) Laparoscopic resection of intestinal endometriosis : a 5-year experience. J Minim Invasive Gynecol 13:442–446
Ruffo G, Scopelliti M, Scioscia M, Ceccaroni M, Mainardi P, Minelli L (2010) Laparoscopic colorectal resection for deep infiltrating endometriosis:analysis of 436 cases. Surg Endosc 24:63–67
Slack A, Child T, Lindsey I, Kennedy S, Cunningham C, Mortensen N, Koninckx P, Mc Veigh E (2007) Urological and colorectal complications following surgery for rectovaginal endometriosis. BJOG 114:1278–1282
Stepniewska A, Pomini P, Bruni F, Mereu L, Ruffo G, Ceccaroni M, Sciosca M, Guerriero M, Minelli L (2009) Laparoscopic treatment of bowel endometriosis in infertile women. Hum Reprod 24(7):1619–1625
Tarjanne S, Sjoberg J, Heikinheimo O (2010) Radical excision of rectovaginal endometriosis results in high rate of pain relief –results of a long term follow up study. Acta Obstet Gynecol Scand 89:71–77
Varol N, Maher P, Healey M, Woods R, Wood C, Hill D, Lolatgis TJ (2003) Rectal surgery for endometriosis- should we be aggressive? Am Assoc Gynecol Laparosc 10:182–189
Weed JC, Ray JE (1987) Endometriosis of the bowel. Obstet Gynecol 69(5):727–730
Wills H, Reid GD, Cooper MJW, Tsalitas J, Morgan M, Woods RJ (2008) Bowel resection for severe endometriosis: an Australian series of 177 cases. Aust N Z J Obstet Gyaecol 49:415–418
Kavallaris A, Kohler C, Kuhne-Heid SA (2003) Histological extent of rectal invasion by rectovaginal endometriosis. Hum Reprod 18(6):1323–1327
Anaf V, El Nakadi I, Simon P, Van de Stadt J, Fayt L, Simonart T, Noel JC (2004) Preferential infiltration of large bowel endometriosis along the nerves of the colon. Hum Reprod 19(4):996–1002
Anaf V, El Nakadi I, De Moore V, Coppens E, Zalcman M, Noel JC (2009) Anatomic signifcance of a positive barium enema in deep infitrating endometriosisof the large bowel. World J Surg 33:822–827
Roman H, Puscasiu L, Kouteich K, Gromez A, Resch B, Marouteau-Pasquier N, Hochain P, Tuech JJ, Scotte M, Marpeau L (2007) Laparoscopic management of deep endometriosis with rectal affect. Chirurgia 102:421–428
Kavallaris A, Banz C, Chalvatzas N, Hornemann A, Luedders DK, Bohmann M (2011) Laparoscopic nerve-sparing surgery of deep infiltrating endometriosis :description of the technique and patients' outcome. Arch Gynecol Obstet 284:1642–1649
Donnez J, Jadoul P, Colette S, Luyckx M, Squifflet J, Donnez O (2013) Deep rectovaginal endometriotic nodules:perioperative complications from a series of 3298 patients operated on the shaving technique. Gynecol Surg 10(1):31–40
Ret Davalos ML, De Cicco C, D'Hoore A, De Decker B, Koninckx PR (2007) Outcome after rectum or sigmoid resection. A review for gynaecologists. Minim Invasive Gynecol 14(1):33–38
McDonough PG (2001) Are basic assumptions correct-is endometriosis a progressive self destructive disease? Fertil Steril 75:230
Wang G (2009) Rich innervation of deep infiltrating endometriosis. Hum Reprod 24:827–834
Fanfani F, Fagotti A, Gagliardi ML, Ruffo G, Ceccaroni M, Scambia G, Minelli L (2010) Discoid or segmental rectosigmoid resection for deep infiltrating endometriosis : a case–control study. Fertil Steril 94:444–449
Roman H, Loise C, Resch B, Tuech JJ, Hochain P, Leroi AM, Marpeau L (2010) Delayed functional outcomes associated with surgical management of deep rectovaginal endometriosis with rectal involvement :giving patients an informed choice. Hum Reprod 25:890–899
Vercellini P, Pietropaolo G, Giorgi OD, Daguati R, Pasin R, Crosignani PG (2006) Reproductive performance in infertile women with rectovaginal endometriosis: Is surgery worthwhile? Am J Obstet Gynecol 195(5):1303–1310
Adamson GD, Hurd SJ, Pasta DJ, Rodriguez BD (1993) Laparoscopic endometriosis treatment :is it better? Fertil Steril 59:35–44
Guzick DS, Silliman NP, Adamson GD, Buttram VC Jr, Canis M, Malinak LR (1997) Prediction of pregnancy in infertile women based on the American Society for Reproductive Medicine’s revised classification of endometriosis. Fertil Steril 67:822–829
Osuga Y, Koga K, Tsutsumi O, Yano T, Maruyama M, Kugu K (2002) Role of laparoscopy in the treatment of endometriosis associated infertility. Gynecol Obstet Invest 53(Suppl 1):33–39
Gordts S, Puttemans P, Campo R, Valkenburg M, Gordts S (2013) Outcome of conservative surgical treatment of deep infiltrating endometriosis. Gynecol Surg 10:137–141
Donnez J, Lousse JC, Jadoul P, Squifflet J (2010) Laparoscopic management of endometriomas using a combined technique of excisional (cystectomy) and ablative surgery. Fertil Steril 94(1):28–32
Meuleman C, Tomassetti C, D’Hoore A, Van Cleynenbreuguel B, Penninckx F, Vergote I, D'Hooghe T (2011) Surgical treatment of deeply infiltrating endometriosis with colorectal involvement. Hum Reprod Update 17:311–326
Disclosure of interest
The author had no financial interest.
Details of ethical approval
Not required as there was no direct patient intervention.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moustafa, M.M., Elnasharty, M.A.A. Systematic review of the outcome associated with the different surgical treatment of bowel and rectovaginal endometriosis. Gynecol Surg 11, 37–52 (2014). https://doi.org/10.1007/s10397-013-0821-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10397-013-0821-5