Abstract
Purpose
Cardiovascular reactivity to the cold pressor test (CPT) is considered to be a marker for apparent and potential hypertension. We aimed to elucidate the association between the changes in wave intensity (WI) during CPT and hypertension.
Methods
We recruited 85 volunteers, 33 of whom were hypertensive and 52 normotensive. Using ultrasonic equipment during CPT, we measured carotid arterial WI, which is defined in terms of blood pressure and velocity in the carotid artery.
Results
The peak WI (W1) increased during CPT in 70.6% of hypertensive individuals, but decreased in 72.6% of normotensive individuals. The chi-square (χ2) test showed that the association between the direction of change in W1 (increase or decrease) and the blood pressure (hypertensive or normotensive) was very strong (P < 0.0001).
Conclusion
Direction of change in W1 during CPT is a clear marker to discriminate cardiovascular reactivity that does not vary depending on each investigator’s subjective point of view.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypertensive persons are considered to be hyper-reactive to CPT. A widely accepted indicator for reactivity is the amount of increase in systolic blood pressure [1, 2]. However, the threshold value to discriminate between hyper-reactive and normo-reactive subjects varies with the investigator. Wave intensity (WI) is a hemodynamic index that can be used to evaluate the working condition of the heart interacting with the arterial system. It can be defined at any site in the circulatory system in terms of blood velocity and blood pressure, and provides integrated information [3]. We suppose that WI has the ability to discriminate between hyper-reactors and normo-reactors more clearly. To evaluate this supposition, we measured WI in hypertensive and normotensive subjects during CPT.
Materials and methods
Subjects
Subjects who had a blood pressure lower than 130/80 mmHg were categorized as normotensive. We recruited 52 normotensive subjects (Norm) from among students and staff at Himeji Dokkyo University, Himeji, Japan. We recruited 33 hypertensive subjects (HT) from among outpatients who were diagnosed as hypertensive at Sakakibara Heart Institute, Tokyo, Japan. All subjects had no abnormal ECGs and had normal echocardiographic findings. Baseline characteristics of the subjects are shown in Table 1.
Methods
Wave intensity
Wave intensity (WI) is a hemodynamic index, which is defined as
at any site in the circulatory system, where dP/dt and dU/dt are the derivatives of blood pressure (P) and velocity (U) with respect to time, respectively [3]. We developed a real-time measurement system for carotid arterial WI that simultaneously measured carotid arterial blood flow velocity and diameter. This system was incorporated in ultrasonic diagnostic equipment (SSD-6500; Aloka, Tokyo, Japan), which had a color Doppler system for blood flow velocity measurements and an echo-tracking subsystem for diameter change measurements. Using systolic and diastolic pressure measured with a cuff-type manometer applied to the upper arm, we calibrated the maximum and minimum values of a diameter change waveform and used it as a surrogate for a blood pressure waveform. We reported the details and reproducibility of this system elsewhere [3, 4].
Cold pressor test (CPT)
Each subject was asked to lie in a supine position for 10 min in a quiet room maintained at a temperature of 25℃ (resting state). Blood pressure readings were obtained during this period; the last of these measurements was used for calibrating the diameter change waveform, which is the surrogate for a blood pressure waveform. Then, the subject was asked to immerse one hand to just above the wrist for 2 min in ice water that was being kept at 0–1 °C. During the period of ice water immersion, blood pressure, blood velocity, and WI were obtained from the carotid artery, and ECG was also recorded (Fig. 1).
Representative recordings of blood pressure (BP), blood flow velocity (U), and calculated wave intensity (WI) in the common carotid artery, and electrocardiogram (ECG) obtained from a normal subject. WI in a normal subject shows two sharp positive peaks during a cardiac cycle, wave 1 and wave 2, and the ejection period is divided into three phases (initial (E), mid (M), and late ejection (L)) by the two waves
Statistical analyses
Data were expressed as percent change, normalized to the index value in the resting state. Comparisons between HT and Norm groups were performed by two-way ANOVA, followed by Bonferroni test. The relationship between gender (male, female) and classification of blood pressure (HT, Norm) was analyzed by the χ2 test. The relationship between classification of %change in W1 (increase, decrease) and classification of blood pressure (HT, Norm) was also analyzed by the χ2 test. The relationship between %change in W1 (%W1) and age and the relationship between %W1 and arterial stiffness were analyzed by linear regression.
Results
During CPT, systolic blood pressure, diastolic blood pressure, and heart rate increased significantly in both HT and Norm. Carotid arterial stroke volume did not change in either HT or Norm. Systolic carotid arterial diameter increased significantly in both HT and Norm. Diastolic carotid arterial diameter did not change in HT, but it increased significantly in Norm. The maximum velocity in the carotid artery did not change in HT, but it decreased significantly in Norm. W1 increased significantly in HT. On the other hand, W1 decreased significantly in Norm (Table 2).
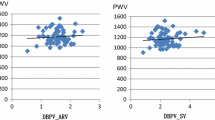
Figure 2 shows the linear regression lines of %W1 during CPT on age. The slope of the regression line for Norm deviates significantly from zero (r = 0.58, P = 0.0001) (Fig. 2, left), while the slope of the regression line for HT does not deviate significantly from zero (r = – 0.19, P = 0.30) (Fig. 2, right).
To define arterial stiffness, we used the stiffness parameter β, which is considered to be independent of pressure. Figure 3 shows the linear regression lines of %W1 during CPT on β before CPT (resting). The slope of the regression line for Norm does not deviate significantly from zero (r = 0.16, P = 0.23), while the slope of the regression line for HT deviates significantly from zero (r = 0.57, P = 0.0007).
Table 3 is the contingency table in which the subjects were classified with respect to the direction of changes in W1 (increase or decrease) and with respect to blood pressure (HT or Norm). The χ2 test was used to determine differences in proportions. The association between the direction of change in W1 and the blood pressure was very strong (P < 0.0001).
Discussion
Hypertensive persons are considered to be hyper-reactive to the CPT, and hyper-reactivity to the CPT in normotensive persons is hypothesized to be a marker for future hypertension [1, 2]. However, the mechanism of future development of hypertension in subjects who show an excessive response to the CPT is not established. The current study was not designed to test this hypothesis, but rather aimed to define ‘cardiovascular reactivity’ without ambiguity. A widely accepted indicator for reactivity is the amount of increase in blood pressure. However, the threshold value to discriminate between hyper-reactive and normo-reactive subjects varies with the investigator. The difference in the changes in the maximum carotid arterial blood velocity between HT and Norm, i.e., no change in HT and decrease in Norm, can be a discriminator. The decrease in the maximum velocity is partly explained as follows: carotid arterial stroke volume did not change during CPT, while systolic carotid arterial diameter increased significantly, which caused a reduction in blood velocity. However, systolic carotid arterial diameter increased in HT, as well. Therefore, this reasoning is inconsistent.
We consider that an index comprised of multiple variables would be more informative than blood pressure alone or velocity alone. We evaluated WI, which is defined in terms of both blood pressure and velocity. Changes in WI during CPT were two directional, i.e., increase or decrease. The association between the direction of change in W1 (increase or decrease) and blood pressure (HT or Norm) was very strong (P < 0.0001) (Table 3). The maximum WI during a cardiac cycle (W1) strongly correlates with left ventricular Max dP/dt, an index of cardiac contractility [3, 5,6,7]. Therefore, in other words, cardiac contractility increases during CPT in HT, but decreases in Norm.
Scatter diagrams for the relationship between %W1 and age show that there is a tendency for higher age (say age > 60) to be associated with positive values of %W1 both in Fig. 2 left and right. Actually, the difference between the mean values of %W1 in the HT and Norm groups is not significant for age > 60. However, in the figure for the Norm group, the slope of the regression line is significantly positive (r = 0.58, P < 0.0001), while in the figure for the HT group, the slope of the regression line is negative but does not deviate significantly from zero (r = –0.19, P = 0.30). Thus, %W1 has a tendency to be negative for lower age in the Norm group, while it has no significant association with age in the HT group.
However, the age ranges of the Norm group and HT group are different (20–80 vs 50–80). To examine whether the above-mentioned tendencies are also observed over the common age range of 50–80, we compared the regression line of %W1 on age for the Norm group and that for the HT group in this age range (Fig. 4). The regression line for the Norm group does not deviate significantly from zero (r = 0.354, P = 0.164). That for the HT group also does not deviate from zero (r = – 0.304, P = 0.091). Therefore, as far as the age range of 50–80 is concerned, the associations between % W1 and age are not significant in either the Norm or HT group.
We also evaluated the effects of stiffness parameter β of the carotid artery before CPT on %W1 during CPT (Fig. 3). In Norm, the amount of %W1 during CPT is not associated with β. In HT, however, the amount of %W1 is associated with β. The effects of the above confounding factors on changes in W1 are not consistent. Thus, the mechanisms underlying the two-way changes in cardiac contractility during CPT are largely unknown. Nevertheless, this property of cardiac contractility, i.e., decrease or increase, is a clear marker to discriminate cardiovascular reactivity, which does not vary depending on each investigator’s subjective point of view.
Limitations
We did not discuss the ability of hyper-reactivity to CPT for predicting future hypertension since we had no data concerning this issue. Our study was limited by the small sample size. Information about smoking status, diabetes mellitus, dyslipidemia, and obesity was not reported, which might have affected the multivariate analyses of factors in relation to the reactions to CPT. Therefore, our findings must be considered to be preliminary until they are replicated by other large studies that are able to show whether there is really no association between these factors and reaction to CPT.
Conclusion
Wave intensity, an index of ventriculo-arterial interaction, increases in hypertensive subjects, but decreases in normotensive subjects during the cold pressor test. Direction of change in W1 during CPT is a marker without ambiguity.
Change history
05 March 2021
A Correction to this paper has been published: https://doi.org/10.1007/s10396-021-01084-4
References
Wood DLSS, Elveback LR, Schirger A. Cold pressor test as a predictor of hypertension. Hypertension. 1984;6:6.
Menkes MS, Matthews KA, Krantz DS, et al. Cardiovascular reactivity to the cold pressor test as a predictor of hypertension. Hypertension. 1989;14:524–30.
Sugawara M, Niki K, Ohte N, et al. Clinical usefulness of wave intensity analysis. Med Biol Eng Comput. 2009;47:197–206.
Niki K, Sugawara M, Chang D, et al. A new noninvasive measurement system for wave intensity: evaluation of carotid arterial wave intensity and reproducibility. Heart Vessels. 2002;17:12–21.
Ramsey MW, Sugawara M. Arterial wave intensity and ventriculoarterial interaction. Heart Vessels. 1997;12:128–34.
Jones CJ, Sugawara M, Kondoh Y, et al. Compression and expansion wavefront travel in canine ascending aortic flow: wave intensity analysis. Heart Vessels. 2002;16:91–8.
Ohte N, Narita H, Sugawara M, et al. Clinical usefulness of carotid arterial wave intensity in assessing left ventricular systolic and early diastolic performance. Heart Vessels. 2003;18:107–11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Research ethics
Study procedures were approved separately by the Ethical Committees of Himeji Dokkyo University and Sakakibara Heart Institute, and were in accordance with the latest revision of the Declaration of Helsinki. Informed consent was obtained from all subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Tanaka, M., Sugawara, M., Niki, K. et al. Wave intensity, an index of ventriculo-arterial interaction, increases in hypertensive subjects but decreases in normotensive subjects during the cold pressor test. J Med Ultrasonics 48, 199–203 (2021). https://doi.org/10.1007/s10396-020-01077-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-020-01077-9