Abstract
Aim
The purpose of this systematic review was to evaluate robust interventions across seven eating practice outcomes and to consider potential modifiers, including parental involvement, intervention setting, and quality of food practice evaluation.
Methods
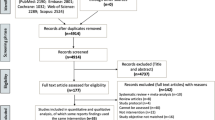
The search procedure reflected Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Web of Science, PsychInfo, PubMed, and Elton B. Stephens Company (EBSCO) (2004–2019) were searched for studies that aimed to change children’s (2 to 12 years old) diet (one or more eating practice components: fruit, vegetables, whole grains, lower saturated fat, lower sugar-sweetened beverages (SSBs), intake of dairy, diet quality). Of 2316 papers, 22 met inclusion criteria.
Results
Fruits (n = 12) and vegetables (n = 15) were the most frequent outcomes. Half of fruit-targeted, two-thirds of vegetable-targeted, half of fruit/vegetable-targeted, eight of nine SSB-targeted, and one of two whole grain-targeted outcomes showed significant improvements. The actual food intake change was modest in most cases. Eighteen interventions included parents, although the four that did not also reported significant outcomes. Most studies were conducted in schools, early childcare, or after-school programs (n = 13) with significant improvements in most settings. Only about half of the studies involving children < 10 years used proxy reporting/direct observation. Eight studies included no reliability, validity, or citation for the method of dietary measurement.
Conclusion
Robust studies continue to focus on one or two foods, parental involvement may be beneficial depending on the intervention, and more research is needed to establish best practices across all settings.
Similar content being viewed by others
Introduction
Healthy eating throughout childhood is important to a child’s growth and development (Bartleman 2019). However, there is no simple definition of “healthy eating.” The 2020 U.S. Dietary Guidelines for Americans (DGA) recommends a healthy dietary pattern that can be achieved by including vegetables, fruits, grains of which half are whole grains, low-fat or fat-free dairy, protein, and oils while limiting added sugars, saturated fats, and sodium (U.S. Department of Agriculture and U.S. Department of Health and Human Services 2020). These guidelines are similar to the World Health Organization’s (2018) key facts on a healthy diet.
Lower quality or less healthful diets in childhood have been associated with chronic ill health in adulthood, such as cardiovascular diseases, metabolic syndrome, and diabetes (Langley-Evans 2015) and breast and colorectal cancers (Clarke and Joshu 2017), as well as obesity (Freedman et al. 2007). Because the eating habits of children may also continue through adult life, establishing healthy eating habits early is important to build the foundation of health throughout life and prevent future chronic conditions. For instance, evidence demonstrates that most children (84%) with a body mass index (BMI) in the 95th to 99th percentiles as children become obese adults (Freedman et al. 2007). Additionally, unhealthy diets are significantly associated with poorer mental health in children and adolescents (O’Neil et al. 2014).
Interventions to improve children’s diets have often focused on one to three food groups or food types. For example, a systematic review of interventions within a school setting targeted fruit and vegetable (F&V) intake and concluded that these interventions had a moderate effect on fruit intake and minimal effect on vegetable intake (Evans et al. 2012). Another systematic review of school environment policies’ effects on children’s sugar-sweetened beverage (SSB) intake reported that three of four SSB studies were effective (Micha et al. 2018). One systematic review focusing on dairy or calcium intake in preschoolers concluded that the results of the interventions were variable (Srbely et al. 2019). Clearly, a broader review of interventions to improve children’s diet, including various food groups and settings, is needed to reflect where there are strengths vs. weaknesses for research and practical considerations.
The settings of interventions for changing children’s food intake vary. While many interventions for children are school-based, others are home-based, clinic-based, or online. In a systematic review of interventions for children that included school environmental policies, direct provision policies had a modest effect on fruit intake and a slight impact on vegetable intake (Micha et al. 2018). Another systematic review focused on gardening-based interventions to improve children’s (2 to 15 years) F&V intake and reported a small but positive impact (Savoie-Roskos et al. 2017). However, all the above reviews included non-controlled interventions and quasi-experimental designs, and the included studies were not required to be powered in primary outcomes. One systematic review focused on elements of the home environment and the child’s F&V intake, concluding that study results varied, but access, availability, and parental input or modeling may be important (Ong et al. 2017). It remains unclear whether the setting of the intervention has an important impact.
Adding to the complexity is the role of parents. Parents can be an important component of changing and molding a child’s dietary practice, by modeling food intake, providing food, or demonstrating certain parental behaviors that could promote or deter food intake. Hingle et al. 2010 reported that of 1774 identified articles, 24 met their review criteria. Nine studies reported improvement in the diet outcomes measured, ten reported mixed results, and five showed no effect. They did not find enough studies that compared the effects of having and not having parental involvement to determine the impact of parents’ involvement on the outcome. Hingle’s review did not therefore comment on the extent of parental involvement needed to improve dietary intake.
In addition, how the food intake is measured must be considered, although it rarely is. Dietary intake studies are highly dependent on how intake is measured. Direct weighing is considered the most accurate method for measuring plate waste, and thus food intake (Martins et al. 2014). However, because this can be costly and time-consuming, observation of food eaten has often been used and is considered valid and reliable with trained observers (Baxter 2009). Observation has been shown to be more valid and reliable than dietary recall methods by children (Baxter 2009). Although food records, diaries, and logs have limitations such as high respondent burden, changing usual food intake, and underreporting, this method is often considered to provide a more accurate estimation of intake than recall methods (Magarey et al. 2011). In children younger than 10 years, a parent or proxy report is recommended for food intake recalls (Magarey et al. 2011). The 24-h recall should use a standardized technique such as a 5-pass or 3-pass protocol (Montgomery et al. 2005). To the authors’ knowledge, no systematic reviews have addressed the issue of measuring food.
To expand the literature, this systematic review examines the outcomes of interventions to improve the eating habits of children in terms of the DGA, namely intake of fruit, vegetables, whole grains, lower saturated fat, lower SSBs, and intake of dairy (U.S. Department of Agriculture and U.S. Department of Health and Human Services 2020). It also reports the frequency and degree of parental involvement, the environment of the intervention, and the quality of dietary intake tools used.
Methods
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, in particular the 27 items included in the 2009 checklist (Ottawa Hospital Research Institute 2009).
Data sources
The Web of Science, PsychInfo, PubMed, and EBSCO were searched using the terms “child” AND “nutrition intervention” AND one of the following terms individually and/or in combination: whole grains, dairy, fruit, vegetables, F&V, SSBs, sugar beverages, saturated fat, parent (parental intervention), and diet quality (according to the Healthy Eating Index [HEI]) between 2004 and 2019.
Inclusion/exclusion criteria
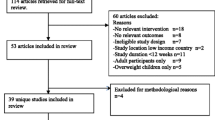
To be included, articles had to be published between 2004 and 2019, have food intake as an outcome, and be randomized controlled studies where the intervention occurred with children aged two to 12 years. Exclusion criteria were as follows: non-intervention; non-English; not powered on the outcome of interest. Studies including only children with overweight or obesity and weight as primary outcomes were excluded as these interventions could be more treatment-oriented rather than prevention-oriented. Studies that included children younger than two or older than 12 were only included if the data for the specified age group were available or if the mean age (± SD) of children actually enrolled fell within the age range.
Data extraction
Four investigators independently performed an initial screening of the identified papers based on titles and abstracts (Fig. 1). Full-text papers were obtained from 216 articles and reviewed independently by two researchers. Of these, 195 were excluded for not fitting the inclusion criteria and due to exclusion criteria, leaving 22 in the review. The data extracted included information on the population targeted, tools to measure food intake, whether the study was powered on the outcomes of interest, quality assessment data, intervention dosage information, parental involvement information, study setting, and outcome results. The primary reporting of outcomes was the difference in means of dietary intake based on DGA components.
Study quality assessment
Articles were evaluated for quality by two investigators using the Academy of Nutrition and Dietetics Evidence Analysis Library’s (EAL) quality criteria checklist, giving articles a quality rating of positive, negative, or neutral (Academy of Nutrition and Dietetics 2019). The EAL quality checklist includes four relevance questions and ten validity questions, including those addressing potential bias, comparability of groups, handling of withdrawals, blinding, validity of measurement tools, statistical analyses, and potential bias because of funding.
Dietary data evaluation
Since dietary intake studies are highly dependent on how intake is measured, an analysis of these methods was also conducted, considering aspects of validity and reliability. In view of the hierarchy of estimation of food intake, validity was scored as follows: weighing food: 4; observation of food intake: 3; food logs, diaries, or records: 2; and 24-h recalls or food frequencies: 1, whereby the higher the score, the more valid the method. The reliability of the food estimation method was evaluated based on the amount of information provided in the paper and was scored as follows: no references for the instrument or procedure and no reliability statistics: 0; references for the instrument or procedure: 1; references plus statistics for instrument reliability: 2, whereby again, the higher the score, the more reliable the method.
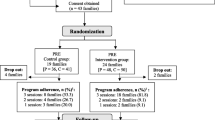
Parental involvement
The included studies varied greatly in terms of the degree of parental involvement. Therefore, a post hoc evaluation was made concerning the level of parental involvement in terms of high, medium, or low. This evaluation was conducted independently by three investigators and then discussed until consensus was reached. Low involvement was defined as indirect parental engagement, such as newsletters sent home via email by the school staff or handed over to the participating children by the program staff; medium parental involvement reflected additional interaction, such as through a website or specific home activities; high parental involvement included program staff making home visits with parents, and individual or group counseling or classes outside the home. These classifications reflect a modification based on van der Kruk et al.’s work (van der Kruk et al. 2013).
Results
Study characteristics
Studies were conducted in Australia (n = 3) (Wolfenden et al. 2014; Wyse et al. 2012; Yoong et al. 2019); Brazil (n = 1) (Sichieri et al. 2009); Finland (n = 1) (Rasanen et al. 2004); Israel (n = 1) (Kaufman-Shriqui et al. 2016); Italy (n = 1) (Panunzio et al. 2011); the Netherlands (n = 1) ([van de Gaar et al. 2014); the United Kingdom (n = 4) (Anderson et al. 2005; Anez et al. 2013; Kipping et al. 2014; McGowan et al. 2013); and the United States (n = 10) (Arredondo et al. 2018; Cravener et al. 2015; Cullen et al. 2015; Larsen et al. 2015; Lumeng et al. 2017; Muth et al. 2008; Nezami et al. 2018; Thompson et al. 2015; Williams et al. 2014; Wright et al. 2012). The total number of participants across these studies was 10,129, ranging from n = 24 (Cravener et al. 2015) to n = 1576 (Cullen et al. 2015). Thirteen were conducted in childcare centers, schools or after-school programs (Anderson et al. 2005; Cullen et al. 2015; Kaufman-Shriqui et al. 2016; Kipping et al. 2014; Larsen et al. 2015; Lumeng et al. 2017; Muth et al. 2008; Panunzio et al. 2011; Sichieri et al. 2009; van de Gaar et al. 2014; Williams et al. 2014; Wright et al. 2012; Yoong et al. 2019) and nine were home-based [Anez et al. 2013; Arredondo et al. 2018; Cravener et al. 2015; McGowan et al. 2013; Nezami et al. 2018; Rasanen et al. 2004; Thompson et al. 2015; Wolfenden et al. 2014; Wyse et al. 2012). Three had more than two intervention arms (Anez et al. 2013; Lumeng et al. 2017; Thompson et al. 2015). Five collected data at a follow-up time (Arredondo et al. 2018; Larsen et al. 2015; Nezami et al. 2018; Thompson et al. 2015; Wolfenden et al. 2014). Most (n = 18) received a positive quality evaluation, with the remaining four receiving neutral ratings (Arredondo et al. 2018; Lumeng et al. 2017; Nezami et al. 2018; Yoong et al. 2019).
The intervention dosages varied greatly, as did the extent to which methods were reported. The longest study covered two years of counseling (Rasanen et al. 2004). Four studies spanned the academic year (Anderson et al. 2005; Lumeng et al. 2017; Muth et al. 2008; van de Gaar et al. 2014); seven studies lasted between 3 and 7 months (Arredondo et al. 2018; Cullen et al. 2015; Muth et al. 2008; Nezami et al. 2018; Panunzio et al. 2011; Sichieri et al. 2009; Yoong et al. 2019); and six studies lasted 4 to 10 weeks (Cravener et al. 2015; Kaufman-Shriqui et al. 2016; Larsen et al. 2015; McGowan et al. 2013; Williams et al. 2014; Wright et al. 2012). The shortest study lasted 12 days (Anez et al. 2013), while another consisted of four 30-min phone calls with data collected at 2 and 6 months post-intervention (Wyse et al. 2012), and a third was a follow-up of the intervention, with data collected at 12 and 18 months post-intervention (Wolfenden et al. 2014).
Eight interventions focused on one food group (Anez et al. 2013; Cravener et al. 2015; Kipping et al. 2014; Nezami et al. 2018; Rasanen et al. 2004; Sichieri et al. 2009; van de Gaar et al. 2014; Wyse et al. 2012), and another eight focused on two food groups (Anderson et al. 2005; Cullen et al. 2015; Kaufman-Shriqui et al. 2016; Larsen et al. 2015; Panunzio et al. 2011; Williams et al. 2014; Wolfenden et al. 2014; Wright et al. 2012), while six included three food groups (Arredondo et al. 2018; Lumeng et al. 2017; McGowan et al. 2013; Muth et al. 2008; Thompson et al. 2015; Yoong et al. 2019). No pattern was discerned in the number of food groups targeted and significant findings.
Food intake outcomes
Of the 22 studies that met the inclusion criteria, 12 had fruit intake as an outcome variable (Anderson et al. 2005; Arredondo et al. 2018; Cullen et al. 2015; Larsen et al. 2015; Lumeng et al. 2017; McGowan et al. 2013; Panunzio et al. 2011; Thompson et al. 2015; Williams et al. 2014; Wolfenden et al. 2014; Wright et al. 2012; Yoong et al. 2019); 15 included vegetable intake (Anderson et al. 2005; Anez et al. 2013; Arredondo et al. 2018; Cravener et al. 2015; Cullen et al. 2015; Kaufman-Shriqui et al. 2016; Larsen et al. 2015; Lumeng et al. 2017; McGowan et al. 2013; Panunzio et al. 2011; Thompson et al. 2015; Williams et al. 2014; Wolfenden et al. 2014; Wright et al. 2012; Yoong et al. 2019); six included F&V (Anderson et al. 2005; Kipping et al. 2014; Muth et al. 2008; Thompson et al. 2015; Williams et al. 2014; Wyse et al. 2012); two included whole grains (Muth et al. 2008; Yoong et al. 2019); one included saturated fat (Rasanen et al. 2004); nine included SSB (Arredondo et al. 2018; Kaufman-Shriqui et al. 2016; Larsen et al. 2015; Lumeng et al. 2017; McGowan et al. 2013; Muth et al. 2008; Nezami et al. 2018; Sichieri et al. 2009; van de Gaar et al. 2014); and one included dairy intake (Yoong et al. 2019) (Table 1). All studies except one (Kipping et al. 2014) reported significant results, but not all outcomes measured in a study may have had significant improvements. In the studies with some (but not all) significant outcomes, the non-significant results occurred with seven fruit outcomes (Arredondo et al. 2018; Cullen et al. 2015; Larsen et al. 2015; Lumeng et al. 2017; Thompson et al. 2015; Williams et al. 2014; Yoong et al. 2019); five vegetable outcomes (Anderson et al. 2005; Arredondo et al. 2018; Larsen et al. 2015; Lumeng et al. 2017; Thompson et al. 2015); three F&V outcomes (Anderson et al. 2005; Kipping et al. 2014; Williams et al. 2014); one whole grain outcome (Muth et al. 2008); and two SSB outcomes (Muth et al. 2008; van de Gaar et al. 2014). Overall, six of 12 fruit-targeted (Anderson et al. 2005; Cullen et al. 2015; McGowan et al. 2013; Panunzio et al. 2011; Wolfenden et al. 2014; Wright et al. 2012), 10 of 15 vegetable-targeted (Anez et al. 2013; Cravener et al. 2015; Cullen et al. 2015; Kaufman-Shriqui et al. 2016; McGowan et al. 2013; Panunzio et al. 2011; Williams et al. 2014; Wolfenden et al. 2014; Wright et al. 2012; Yoong et al. 2019), three of six F&V-targeted (Muth et al. 2008; Thompson et al. 2015; Wyse et al. 2012), eight of nine SSB-targeted (Arredondo et al. 2018; Kaufman-Shriqui et al. 2016; Larsen et al. 2015; Lumeng et al. 2017; McGowan et al. 2013; Nezami et al. 2018; Sichieri et al. 2009; van de Gaar et al. 2014), and one of two whole grain-targeted outcomes (Yoong et al. 2019) showed significant improvements. Dairy intake was not significantly improved, but diet quality was in the study by Yoong et al. (2019).
Within the six statistically significant fruit-targeted outcome studies (Anderson et al. 2005; Cullen et al. 2015; McGowan et al. 2013; Panunzio et al. 2011; Wolfenden et al. 2014; Wright et al. 2012), the largest change was in the study by Anderson et al. (2005), with the intervention participants increasing their consumption by 183 g vs. 107 g in the control group (one serving being approximately 80 g). The study by Wright et al. (2012) reported an increase of 2.0 servings for the intervention vs. a decrease of 0.4 servings for the control group. The study by Anderson et al. 2005 was conducted in school with tastings, education, and parental newsletters over a period of 9 months, whereas Wright et al.’s 2012 study constituted 6 weeks of 90-min nutrition and physical activity instruction after school with parents.
Within the ten statistically significant vegetable-focused studies (Anez et al. 2013; Cravener et al. 2015; Cullen et al. 2015; Kaufman-Shriqui et al. 2016; McGowan et al. 2013; Panunzio et al. 2011; Williams et al. 2014; Wolfenden et al. 2014; Wright et al. 2012; Yoong et al. 2019), the largest difference between intervention and control groups was reported in Wright et al.’s study (2012) as 1.5 vs. 0.4 servings. Within the three significant F&V-targeted studies (Muth et al. 2008; Thompson et al. 2015; Wyse et al. 2012), the largest improvement was in the Wyse et al. study (17 vs 15.4 F&V score) (2012). The summed score reflected intake and variety over the previous seven days. Of the eight studies with significant changes in SSB, the results were represented across a wide variety of denominators (e.g., ml/day, l/day, servings/day, percentage bringing SSB to school, mean change in servings/day) (Arredondo et al. 2018; Kaufman-Shriqui et al. 2016; Larsen et al. 2015; Lumeng et al. 2017; McGowan et al. 2013; Nezami et al. 2018; Sichieri et al. 2009; van de Gaar et al. 2014).
Parental involvement
Within the 22 studies, 18 included parents in some way in the intervention. The four studies that did not include parents were Anez et al. (2013), Cullen et al. (2015), Sichieri et al. (2009), and Yoong et al. (2019). All four reported positive significant results: improved vegetable intake in preschoolers (Anez et al. 2013); improved fruit intake in elementary school students (p < 0.001), and improved fruit (p < 0.001) and vegetable (p < 0.05) intake in intermediate school students (Cullen et al. 2015); decreased SSB in 9-to-12-year-old fourth graders (p = 0.03; n = 435, intervention group; n = 608, control group) (Sichieri et al. 2009); and increased vegetable intake (p < 0.001) and whole grains (p < 0.01) (but not dairy) in preschoolers (Yoong et al. 2019). One study used food exposure methods directly (Anez et al. 2013) while two used school menu changes to increase healthy food offerings (Cullen et al. 2015; Yoong et al. 2019).
Of the 18 studies with parental involvement, five were categorized as low parental involvement (Anderson et al. 2005; Kipping et al. 2014; Larsen et al. 2015; Muth et al. 2008; van de Gaar et al. 2014). In all but one study, where parents were invited to water-themed activities at school or in the community (van de Gaar et al. 2014), the interventions with parents consisted of homework or a brochure being sent home. Two studies with low parental involvement evaluated fruit intake, with one reporting significant results post-intervention (Anderson et al. 2005), while the other reported no significant difference at post-intervention (Larsen et al. 2015). In this study, there was a significant difference between intervention and control groups at follow-up, but both groups’ fruit intake declined, with the intervention declining less than the control (Larsen et al. 2015). There were no statistically significant results for vegetable intake in the two studies with low parental involvement that measured vegetable intake (Anderson et al. 2005; Larsen et al. 2015). Two of the studies that evaluated F&V combined reported non-significant results (Anderson et al. 2005; Kipping et al. 2014) while one reported significant results of adjusted mean differences of 0.9 servings (Muth et al. 2008). One study that included whole grains and SSB had non-significant results (Muth et al. 2008). Another study that focused on SSB had some significant reports among multiple measures of SSB intake (van de Gaar et al. 2014), while yet another had significant results post-intervention, but not at follow-up (Larsen et al. 2015).
There were two studies categorized as medium or medium-to-high parental involvement (Thompson et al. 2015; Wright et al. 2012). While Thompson et al. (2015) reported significant improvements only when F&V were combined and not separately for F&V intakes, Wright et al. (2012) reported significant improvements in both individual fruit and vegetable intake and did not combine them. The study resulted in significant increases at the 12-month follow-up in F&V intakes after a 6-week, daily 90-min after-school program coupled with a home-level program covering a variety of diet and physical activity topics.
There were 11 studies that were categorized as having high parental involvement (Arredondo et al. 2018; Cravener et al. 2015; Kaufman-Shriqui et al. 2016; Lumeng et al. 2017; McGowan et al. 2013; Nezami et al. 2018; Panunzio et al. 2011; Rasanen et al. 2004; Williams et al. 2014; Wolfenden et al. 2014; Wyse et al. 2012). Of note is the generally younger age, with eight studies targeted at children younger than seven years (Cravener et al. 2015; Kaufman-Shriqui et al. 2016; Lumeng et al. 2017; McGowan et al. 2013; Nezami et al. 2018; Williams et al. 2014; Wolfenden et al. 2014; Wyse et al. 2012). Of those that measured fruit intake (Arredondo et al. 2018; Lumeng et al. 2017; McGowan et al. 2013; Panunzio et al. 2011; Williams et al. 2014; Wolfenden et al. 2014), three reported significant increases [McGowan et al. 2013; Panunzio et al. 2011; Wolfenden et al. 2014). Eight studies included vegetable intake (Arredondo et al. 2018; Cravener et al. 2015; Kaufman-Shriqui et al. 2016; Lumeng et al. 2017; McGowan et al. 2013; Panunzio et al. 2011; Williams et al. 2014; Wolfenden et al. 2014), with six having significant results (Cravener et al. 2015; Kaufman-Shriqui et al. 2016; McGowan et al. 2013; Panunzio et al. 2011; Williams et al. 2014; Wolfenden et al. 2014). Two studies measured F&V intake combined (Williams et al. 2014; Wyse et al. 2012), with one reporting significant results (Wyse et al. 2012). Whole grains were not included in any of the high parental involvement studies. Only one study included saturated fat and found that saturated fat intake was 11.1% of calories for the intervention group as compared to 13.4% for the control group (p < 0.001) (Rasanen et al. 2004).
To summarize, of the four studies with no parental involvement, all reported statistically significant changes in healthy eating variables (Anez et al. 2013; Cullen et al. 2015; Sichieri et al. 2009; Yoong et al. 2019). These were driven by food exposure or school menu changes in three of the four studies. For the five studies with low parental involvement (Anderson et al. 2005; Kipping et al. 2014; Larsen et al. 2015; Muth et al. 2008; van de Gaar et al. 2014), most results were non-significant: Anderson et al. for vegetables and F&V (Anderson et al. 2005); Kipping et al. for F&V (2014); Larsen et al. for F&V at post-intervention (Larsen et al. 2015); Muth et al. for whole grains and SSB (Muth et al. 2008); and van der Gaar et al. for some measurements of SSB (van de Gaar et al. 2014). Regarding the two studies with medium or medium–high involvement, F&V intakes were not always improved (Thompson et al. 2015; Wright et al. 2012). Within the 11 studies with high parental involvement, there were more significantly improved results than in other levels of parental involvement (Arredondo et al. 2018; Cravener et al. 2015; Kaufman-Shriqui et al. 2016; Lumeng et al. 2017; McGowan et al. 2013; Nezami et al. 2018; Panunzio et al. 2011; Rasanen et al. 2004; Williams et al. 2014; Wolfenden et al. 2014; Wyse et al. 2012).
Study setting
Thirteen studies were in the school or early childcare setting (Anderson et al. 2005; Anez et al. 2013; Cullen et al. 2015; Kaufman-Shriqui et al. 2016; Kipping et al. 2014; Larsen et al. 2015; Lumeng et al. 2017; Muth et al. 2008; Panunzio et al. 2011; Sichieri et al. 2009; van de Gaar et al. 2014; Williams et al. 2014; Wright et al. 2012; Yoong et al. 2019). All but one (Kipping et al. 2014) reported some significant findings. Four of eight studies with a fruit outcome reported significant improvements in fruit intake (Anderson et al. 2005; Cullen et al. 2015; Panunzio et al. 2011; Wright et al. 2012). Seven of 10 studies with a vegetable outcome reported significant positive results (Anez et al. 2013; Cullen et al. 2015; Kaufman-Shriqui et al. 2016; Panunzio et al. 2011; Williams et al. 2014; Wright et al. 2012; Yoong et al. 2019). All but one (Muth et al. 2008) of the nine studies with the SSB outcome had positive results (Arredondo et al. 2018; Kaufman-Shriqui et al. 2016; Larsen et al. 2015; Lumeng et al. 2017; McGowan et al. 2013; Nezami et al. 2018; Sichieri et al. 2009; van de Gaar et al. 2014). Three studies were home-based (Arredondo et al. 2018; Cravener et al. 2015; McGowan et al. 2013). McGowan et al. (2013) reported significant improvements in fruit, vegetables, and SSB intake. Cravener et al. (2015) reported improvements in SSB intake, and Arrendondo et al. (2018) reported non-significant findings for F&V, but a significant impact on SSBs. One study was conducted at a clinic (Rasanen et al. 2004), two had online components (Nezami et al. 2018; Thompson et al. 2015), and two were conducted by phone (Wolfenden et al. 2014; Wyse et al. 2012). Rasanen et al.’s (2004) clinic-based study focused on changing saturated fat intake and reported positive results. The online study by Thompson et al. (2015) did not report significant findings for fruit or vegetables but did for SSBs. Nezami et al. (2018) included one group meeting followed by online content and reported significant improvement in SSB intake. Outcomes for both telephone interventions reported significant increases, in fruit and vegetables individually (Wolfenden et al. 2014) or F&V combined (Wyse et al. 2012).
Dietary data evaluation
There were two studies that scored “4” on validity since they weighed food (Anez et al. 2013; Cravener et al. 2015). Three studies scored a “3” because they observed intake (Cullen et al. 2015; Lumeng et al. 2017; van de Gaar et al. 2014). Three studies scored “2” as they used food logs or records (Anderson et al. 2005; Panunzio et al. 2011; Rasanen et al. 2004), and 14 scored “1” as they used recalls or food frequencies (Arredondo et al. 2018; Kaufman-Shriqui et al. 2016; Kipping et al. 2014; Larsen et al. 2015; McGowan et al. 2013; Muth et al. 2008; Nezami et al. 2018; Sichieri et al. 2009; Thompson et al 2015; Williams et al. 2014; Wolfenden et al. 2014; Wright et al. 2012; Wyse et al. 2012; Yoong et al. 2019).
Of the 21 studies involving children under 10 years of age, nine used proxy reporting (Kaufman-Shriqui et al. 2016; Lumeng et al. 2017; McGowan et al. 2013; Nezami et al. 2018; Rasanen et al. 2004; Williams et al. 2014; Wolfenden et al. 2014; Wyse et al. 2012; Yoong et al. 2019) as recommended (Magarey et al. 2011). Direct observation and/or food weight was used in four others (Anez et al. 2013; Cravener et al. 2015; Kaufman-Shriqui et al. 2016; van de Gaar et al. 2014). The tools used to collect dietary information included student-completed diaries or food recalls with student interviews (Anderson et al. 2005), student-completed recalls with supervision (Kipping et al. 2014; Muth et al. 2008; Panunzio et al. 2011), student self-reports (Arredondo et al. 2018; Larsen et al. 2015; Sichieri et al. 2009; Wright et al. 2012), and student interviews (Thompson et al. 2015).
Four studies scored “2” for reliability as they included instrument reliability statistics in the paper (Anderson et al. 2005; Cullen et al. 2015; Panunzio et al. 2011; Rasanen et al. 2004). All four reported statistically significant changes in their outcome variables. Ten studies scored a “1,” having a reference cited for the measurement tool or procedure (Arredondo et al. 2018; Kaufman-Shriqui et al. 2016; Kipping et al. 2014; Larsen et al. 2015; Lumeng et al. 2017; Muth et al. 2008; Panunzio et al. 2011; Thompson et al. 2015; Williams et al. 2014; Yoong et al. 2019). Eight papers included neither reliability statistics nor a reference for their means of measuring intake (Anderson et al. 2005; Anez et al. 2013; Cravener et al. 2015; McGowan et al. 2013; Nezami et al. 2018; Rasanen et al. 2004; Sichieri et al. 2009; van de Gaar et al. 2014).
Discussion
The results of this review suggest that most included interventions aimed to improve two to three dietary outcomes as opposed to addressing the total child diet quality. The most common outcomes addressed included intake of fruit, vegetables, F&V combined, and SSBs. While the studies included in this review were more likely to show dietary improvements in their results as the degree of parental involvement increased, we also found that interventions directly exposing children to F&V could be successful, even without parental involvement. Interventions in varied settings, including school, at home, clinic-based, and online programs, reported significant findings. The non-school studies included in this review incorporated a parental component.
Dietary improvement goals for all studies in this review were limited to dietary components which may increase the probability of positive outcomes, possibly because of more focused interventions. A systematic review by Murimi et al. (2017) reported that nutrition education interventions focusing on three or fewer objectives were more likely to have positive results, although the included studies were with adults rather than children. Most studies in the current review included F&V intake improvement in their objectives. One systematic review and meta-analysis of strategies to improve vegetable intake in children aged 2 to 5 years concluded that repeated exposure was most likely to have a positive effect (Nekitsing et al. 2017). This is similar to findings of the current review in which three (Anez et al. 2013; Cravener et al. 2015; Cullen et al. 2015 of the four studies (Anderson et al. 2005; Anez et al. 2013; Cravener et al. 2015; Cullen et al. 2015) involving repeated vegetable exposure resulted in significant positive outcomes. Cullen et al. (2015) found increased vegetable intake in younger and older children in an intervention where they were to select one fruit and two vegetables vs. the control group where they were to select a total of three F&V. This study also reported greater intake of fruits in older, but not among younger, children. Another systematic review that included parent-targeted home-based interventions to increase F&V intake in children 2 to 12 years old also found that taste exposure increased vegetable intake (Touyz et al. 2018). In the present review, the one study where this was not found included a vegetable soup or starter once a week and a daily choice of salad and a cooked vegetable, among other educational or promotional strategies for a school-based intervention for children aged 6 to 7 and 10 to 11 years (Anderson et al. 2005). With this exception, the current review is consistent with that of DeCosta et al. (2007) who concluded from a review of experimental research in changing children’s dietary practice that making F&V available and accessible to children led to increased intake. These authors note that very few studies have been conducted in this area, and they included only six in their review, primarily with F&V in schools.
Nine studies included an objective to reduce SSB intake (Arredondo et al. 2018; Kaufman-Shriqui et al. 2016; Larsen et al. 2015; Lumeng et al. 2017; McGowan et al. 2013; Muth et al. 2008; Nezami et al. 2018; Sichieri et al. 2009; van de Gaar et al. 2014), and eight reported significant outcomes (Arredondo et al. 2018; Kaufman-Shriqui et al. 2016; Larsen et al. 2015; Lumeng et al. 2017; McGowan et al. 2013; Nezami et al. 2018; Sichieri et al. 2009; van de Gaar et al. 2014). One systematic review and meta-analysis of strategies to reduce SSB in children aged 4 to 16 years concluded that educational and behavioral interventions were modestly successful (Abdel Rahman et al. 2018). Another systematic review and meta-analysis to reduce SSB and/or increase water intake in children and adults concluded that behavioral interventions were successful in reducing SSB in children and adolescents, but not adults (Vargas-Garcia et al. 2017). While Abdel Rahman et al. (2018) included only randomized controlled trials as the current review did, Vargas-Garcia et al. (2017) included other study designs as well. However, Abdel Rahman et al. did not omit studies that also focused on obesity reduction as the current review did. Nevertheless, these two systematic reviews, as well as the current review, found many interventions to reduce SSB in children successfully using a variety of intervention approaches such as social marketing, school lessons, parental newsletters, and text messages. Therefore, the intervention approach to reducing SSB intake does not seem to be a critical element. Comparable systematic reviews of interventions to increase whole grains or dairy, improve diet quality, or reduce saturated fat intake in children and adolescents were not found.
Studies in this review where both parental involvement was high or where food was provided without parental involvement were likely to result in dietary improvement. Studies involving parents included school, community, and clinic settings. The level of parental involvement ranged from a simple handout sent home to multiple sessions providing parents with nutrition education. In high parent involvement studies, all reported some statistically significant improvements in dietary practices (Arredondo et al. 2018; Cravener et al. 2015; Kaufman-Shriqui et al. 2016; Lumeng et al. 2017; McGowan et al. 2013; Nezami et al. 2018; Panunzio et al. 2011; Rasanen et al. 2004; Williams et al. 2014; Wolfenden et al. 2014; Wyse et al. 2012). Yee et al. (2017) point out that restrictive guidance by parents might be more effective in unhealthy behaviors, such as intake of SSB, but their review revealed a variety of results, with eight of 33 studies reporting higher intake of unhealthy food with restrictive guidance, and 16 reporting lower intake. It is unknown whether modeling or restrictive guidance techniques were embedded in the interventions of the current review. An umbrella review of systematic reviews and meta-analyses of diet and physical activity interventions to reduce the obesity risk of children aged 3 to 12 concluded that parental involvement in interventions was beneficial to child weight outcomes, but it was not possible to define best practices for parental involvement type or duration (Tomayko et al. 2021). The current review supports these conclusions relative to diet. Another systematic review, which included non-randomized controlled studies and did not mention the power of the studies, reported that most interventions for nutrition education of children included parents, whether the intervention had positive outcomes or not (Murimi et al. 2018). Because the quality of these included studies may not have been as high as in the present study, comparisons cannot be drawn, however.
A systematic review of interventions targeting F&V intake of children within the school setting by Evans et al. concluded that these interventions had a moderate effect on fruit intake and minimal effect on vegetable intake (Evans et al. 2012). However, of the 13 studies in a school or early childcare setting in the present review, four (Anderson et al. 2005; Cullen et al. 2015; Panunzio et al. 2011; Wright et al. 2012) of eight (Anderson et al. 2005; Cullen et al. 2015; Larsen et al. 2015; Lumeng et al. 2017; Panunzio et al. 2011; Williams et al. 2014; Wright et al. 2012; Yoong et al. 2019) reported significant improvements in fruit intake. For those with vegetable intake outcomes, seven (Anez et al. 2013; Cullen et al. 2015; Kaufman-Shriqui et al. 2016; Panunzio et al. 2011; Williams et al. 2014; Wright et al. 2012; Yoong et al. 2019) of 10 studies (Anderson et al. 2005; Anez et al. 2013; Cullen et al. 2015; Kaufman-Shriqui et al. 2016; Larsen et al. 2015; Lumeng et al. 2017; Panunzio et al. 2011; Williams et al. 2014; Wright et al. 2012; Yoong et al. 2019) reported significant results. Most (eight out of nine) of the school-based interventions with SSB in the present study had positive results. This is in agreement with a systematic review of school environment policy effects on children’s intake that reported three of four SSB studies were effective (Micha et al. 2018). It may be that the studies in the current review had less of a chance to report non-significant results because all were powered on the variable of interest. Thus, the setting may be less important than a well-designed, powered intervention.
A systematic review describing the food intake assessment methodologies in child and adolescent obesity prevention interventions evaluated those methods on seven components that included validity, data collection quality, and food database description. Authors reported that 15 of the 31 studies were rated as poor, with most limitations in reporting of validity and instrument quality (Burrows et al. 2012). These results are similar to the current review, where eight of the 22 studies included neither reliability information nor a citation to support the use of the instrument. In the present review, three studies used food diaries (Anderson et al. 2005; Panunzio et al. 2011; Rasanen et al. 2004), in contrast to the review by Burrows et al. (2012), where food records or diaries were most commonly used. As noted in the Burrows et al. 2012 review, the choice of assessment technique should be framed by the research method and child’s age, and include information both for replication purposes and quality evaluation.
A strength of this systematic review is that only the highest-quality studies were included: RCTs that were powered on the outcomes of interest. This is in contrast to other systematic reviews included in this discussion (Murimi et al. 2017; Murimi et al. 2018; Nekitsing et al. 2017; Touyz et al. 2018; Vargas-Garcia et al. 2017; Yee et al. 2017). This review also provides a substantially broader perspective by evaluating studies across several food groups and multiple intervention settings, and assessing the degree of parental involvement as well as dietary evaluation methods. However, this systematic review must also acknowledge some limitations. The search strategies may have unintentionally excluded papers not indexed in the databases used. Non-published studies with negative results may alter the results of this review, as could including only English articles. The authors excluded those studies focused on overweight or obese children as this was not the aim of the project. Although behavioral theory use may have an effect on outcomes (Diep et al. 2014), this aspect of the interventions was not evaluated. In addition, details of implementation, fidelity, and process evaluation were not included as part of the systematic review since they were not explicitly available in most papers.
It must also be acknowledged that the studies assessed in this systematic review utilized a variety of factors that make direct comparisons difficult. These variations included the child’s age, study setting, duration of intervention, degree of parent involvement, and methods for evaluating intake. To address one of these differences, parental involvement was classified to examine diverse outcomes among various levels of involvement.
In addition, multiple methods were used to assess dietary intake with varying levels of validity and reliability. To address these variations, we classified the validity of intake assessment methods, with food weighing considered the most valid, and recalls and food frequency questionnaires least valid. Comparing child reports of intake in some studies to the parent or proxy reporting in others adds to concerns with the evaluation, with the varied methods of assessment complicating the interpretation of results. Finally, the review included studies published between 2004–2019, and interventions published prior to or after this time may have changed the results.
Conclusion
The current review adds to the literature by reporting that most vegetable and SSB interventions and about half of the fruit-targeted interventions were successful in demonstrating improvement in intake using a variety of interventions. Most studies with higher parental involvement were successful in affecting positive dietary change, but those without parental involvement also reported positive outcomes if they included food offerings. While schools were the most frequent setting, positive outcomes were also reported with online and clinic- and home-based interventions. As many studies did not provide details on food intake assessment, the inclusion of such information would help advance the science of achieving positive change in children’s diets. With a scarcity of studies targeting multiple components of diet beyond F&V and SSB, further research focused on overall diet quality and components such as whole grains seems warranted.
References
Abdel Rahman A, Jomaa L, Kahale LA et al (2018) Effectiveness of behavioral interventions to reduce the intake of sugar-sweetened beverages in children and adolescents: a systematic review and meta-analysis. Nutr Rev 76(2):88–107. https://doi.org/10.1093/nutrit/nux061
Academy of Nutrition and Dietetics (2019) Evidence analysis manual: steps in the Academy evidence analysis process. https://www.andeal.org/evidenceanalysis-manual. Accessed Nov 2022
Anderson AS, Porteous LE, Foster E et al (2005) The impact of a school-based nutrition education intervention on dietary intake and cognitive and attitudinal variables relating to fruits and vegetables. Pub Health Nutr 8:650–656. https://doi.org/10.1079/phn2004721
Añez E, Remington A, Wardle J et al (2013) The impact of instrumental feeding on children’s responses to taste exposure. J Hum Nutri Diet 26:415–420. https://doi.org/10.1111/jhn.12028
Arredondo EM, Ayala GX, Soto S et al (2018) Latina mothers as agents of change in children’s eating habits: findings from the randomized controlled trial Entre Familia: Reflejos de Salud. In J Behav Nutr Phys Act 15(1):95. https://doi.org/10.1186/s12966-018-0714-0
Bartleman J (2019) Infant and Child Nutrition. Medicine 47(3):195–198. https://doi.org/10.1016/j.mpmed.2018.12.002
Baxter SD (2009) Cognitive processes in children’s dietary recall insight from methodological studies. Eur J Clin Nutr 63(1):S19–S32. https://doi.org/10.1038/ejcn.2008.61
Burrows T, Golley RK, Khambalia A et al (2012) The quality of dietary intake methodology and reporting in child and adolescent obesity intervention trials: a systematic review. Obes Rev 13(12):1125–1138. https://doi.org/10.1111/j.1467-789X.2012.01022.x
Clarke MA, Joshu CE (2017) Early life exposures and adult cancer risk. Epidemiol Rev 39(1):11–27. https://doi.org/10.1093/epirev/mxx004
Cravener TL, Schlechter H, Loeb KL et al (2015) Feeding strategies derived from behavioral economics and psychology can increase vegetable intake in children as part of a home-based intervention: results of a pilot study. J Acad Nutr Diet 115:1798–1807. https://doi.org/10.1016/j.jand.2015.03.024
Cullen KW, Chen TA, Dave JM et al (2015) Differential improvements in student fruit and vegetable selection and consumption in response to the new National School Lunch Program regulations: a pilot study. J Acad Nutr Diet 115:743–750. https://doi.org/10.1016/j.jand.2014.10.021
DeCosta P, Moller P, Bom Frøst M et al (2007) Changing children’s eating behavior – a review of experimental research. Appetite 113:327–357. https://doi.org/10.1016/j.appet.2017.03.004
Diep CS, Chen TA, Davies VF et al (2014) Influence of behavioral theory on fruit and vegetable intervention effectiveness among children: a meta-analysis. J Nutr Educ Behav 46(6):506–546. https://doi.org/10.1016/j.jneb.2014.05.012
Evans CE, Christian MS, Cleghorn CL et al (2012) Systematic review and meta-analysis of school-based interventions to improve daily fruit and vegetable intake in children aged 5 to 12 y. Am J Clin Nutr 96(4):889–901. https://doi.org/10.3945/ajcn.111.030270
Freedman DS, Mei Z, Srinivasan SR et al (2007) Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr 150(1):12–17. https://doi.org/10.1016/j.jpeds.2006.08.042
Hingle MD, O’Connor TM, Dave JM et al (2010) Parental involvement in interventions to improve child dietary intake: a systematic review. Prev Med 51(2):103–111. https://doi.org/10.1016/j.ypmed.2010.04.014
Kaufman-Shriqui V, Fraser D, Friger M et al (2016) Effect of a school-based intervention on nutritional knowledge and habits of low-socioeconomic school children in Israel: a cluster-randomized controlled trial. Nutrients 8(4):234. https://doi.org/10.3390/nu8040234
Kipping RR, Howe LD, Jago R et al (2014) Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: active for life year 5 (AFLY5) school-based cluster randomized controlled trial. Br Med 348:g3256. https://doi.org/10.1136/bmj.g3256
Langley-Evans SC (2015) Nutrition in early life and the programming of adult disease: a review. J Hum Nutr Diet 28(Suppl 1):1–14. https://doi.org/10.1111/jhn.12212
Larsen AL, Robertson T, Dunton G (2015) Re-aim analysis of a randomized school-based nutrition intervention among fourth-grade classrooms in California. Trans Behav Med 5:315–326. https://doi.org/10.1007/s13142-015-0311-6
Lumeng JC, Miller AL, Horodynski MA et al (2017) Improving self-regulation for obesity prevention in head start: a randomized controlled trial. Pediatrics 139(5):e20162047. https://doi.org/10.1542/peds.2016-2047
Magarey A, Watson J, Golley RK et al (2011) Assessing dietary intake in children and adolescents: considerations and recommendations for obesity research. Int J Pediatr Obes 6(1):2–11. https://doi.org/10.3109/17477161003728469
Martins ML, Cunha LM, Rodrigues SSP et al (2014) Determination of plate waste in primary school lunches by weighing and visual estimation methods: a validation study. Waste Manage 34(8):1362–1368. https://doi.org/10.1016/j.wasman.2014.03.020
McGowan L, Cooke LJ, Gardner B et al (2013) Healthy feeding habits: efficacy results from a cluster-randomized, controlled exploratory trial of a novel, habit-based intervention with parents. Am J Clin Nutr 98:769–777. https://doi.org/10.3945/ajcn.112.052159
Micha R, Karageorgou D, Bakogianni I et al (2018) Effectiveness of school food environment policies on children’s dietary behaviors: a systematic review and meta-analysis. PLoS ONE 13(3):e0194555. https://doi.org/10.1371/journal.pone.0194555
Montgomery C, Reilly JJ, Jackson DM et al (2005) Validation of energy intake by 24-hour multiple pass recall: comparison with total energy expenditure in children aged 5–7 years. Br J Nutr 93(5):671–676. https://doi.org/10.1079/bjn20051405
Murimi MW, Kanyi M, Mupfudze T et al (2017) Factors influencing efficacy of nutrition education interventions: a systematic review. J Nutr Educ Behav 49(2):142–165. https://doi.org/10.1016/j.jneb.2016.09.003
Murimi MW, Moyeda-Carabaza AF, Nguyen B et al (2018) Factors that contribute to effective nutrition education interventions in children: a systematic review. Nutr Rev 76(8):553–580. https://doi.org/10.1093/nutrit/nuy020
Muth ND, Chatterjee A, Williams D et al (2008) Making an IMPACT: effect of a school-based pilot intervention. N C Med J 69:432–440
Nekitsing C, Blundell-Birtill P, Cockroft JE et al (2017) Systematic review and meta-analysis of strategies to increase vegetable consumption in preschool children aged 2–5 years. Appetite 127:138–154. https://doi.org/10.1016/j.appet.2018.04.019
Nezami BT, Ward DS, Lytle LA et al (2018) A mHealth randomized controlled trial to reduce sugar-sweetened beverage intake in preschool-aged children. Pediatr Obes 13(11):668–676. https://doi.org/10.1111/ijpo.12258
O’Neil A, Quirl SE, Housden S et al (2014) Relationship between diet and mental health in children and adolescents: a systematic review. Am J Public Health 104(10):e31-42. https://doi.org/10.2105/AJPH.2014.302110
Ong JX, Ullah S, Magarey A, Miller J, Leslie E (2017) Relationship between the home environment and fruit and vegetable consumption in children aged 6–12 years: a systematic review. Pub Health Nutr 20(3):464–480. https://doi.org/10.1017/S1368980016002883
Ottawa Hospital Research Institute (2009) PRISMA checklist http://www.prisma-statement.org/documents/PRISMA%202009%20checklist.pdf. Accessed Nov 2021
Panunzio MF, Caporizzi R, Antoniciello A et al (2011) Training the teachers for improving primary schoolchildren’s fruit and vegetables intake: a randomized controlled trial. Ann Ig 23:249–260
Rasanen M, Niinikoski H, Keskinen S et al (2004) Impact of nutrition counselling on nutrition knowledge and nutrient intake of 7-to 9-y-old children in an atherosclerosis prevention project. Eur J Clin Nutr 58:162–172. https://doi.org/10.1038/sj.ejcn.1601763
Savoie-Roskos MR, Wengreen H, Durward C (2017) Increasing fruit and vegetable intake among children and youth through gardening-based interventions: a systematic review. J Acad Nutr Diet 117(2):240–250. https://doi.org/10.1016/j.jand.2016.10.014
Sichieri R, Paula Trotte A, de Souza RA et al (2009) School randomised trial on prevention of excessive weight gain by discouraging students from drinking sodas. Pub Health Nutr 12:197–202. https://doi.org/10.1017/S1368980008002644
Srbely V, Janjua I, Buchholz AC, Newton G (2019) Interventions aimed at increasing dairy and/or calcium consumption of preschool-aged children: a systematic literature review. Nutrients 11(4):714. https://doi.org/10.3390/nu11040714
Thompson D, Bhatt R, Vazquez I et al (2015) Creating action plans in a serious video game increases and maintains child fruit-vegetable intake: a randomized controlled trial. Int J Behav Nutr Phys Act 12:39. https://doi.org/10.1186/s12966-015-0199-z
Tomayko EJ, Tovar A, Fitzgerald N et al (2021) Parent involvement in diet or physical activity interventions to treat or prevent childhood obesity: an umbrella review. Nutrients 13(9):3227. https://doi.org/10.3390/nu13093227
Touyz LM, Wakefield CE, Grech AM et al (2018) Parent-targeted home-based interventions for increasing fruit and vegetable intake in children: a systematic review and meta-analysis. Nutr Rev 76(3):154–173. https://doi.org/10.1093/nutrit/nux066
U.S. Department of Agriculture and U.S. Department of Health and Human Services (2020) Dietary Guidelines for Americans, 2020–2025. 9th Edition. https://www.dietaryguidelines.gov/. Accessed 1 Dec 2023
van de Gaar VM, Jansen W, van Grieken A et al (2014) Effects of an intervention aimed at reducing the intake of sugar-sweetened beverages in primary school children: a controlled trial. Int J Behav Nutr Phys Act 11:98. https://doi.org/10.1186/s12966-014-0098-8
van der Kruk JJ, Kortekaas F, Lucas C, Jager-Wittenaar H (2013) Obesity: a systematic review on parental involvement in long-term European childhood weight control interventions with a nutritional focus. Obes Rev 14(9):745–760. https://doi.org/10.1111/obr.12046
Vargas-Garcia EJ, Evans CEL, Prestwich A et al (2017) Interventions to reduce consumption of sugar-sweetened beverages or increase water intake: evidence from a systematic review and meta-analysis. Obes Rev 18(11):1350–1363. https://doi.org/10.1111/obr.12580
Williams PA, Cates SC, Blitstein JL et al (2014) Nutrition-education program improves preschoolers’ at-home diet: a group randomized trial. J Acad Nutr Diet 114:1001–1008. https://doi.org/10.1016/j.jand.2014.01.015
Wolfenden L, Wyse R, Campbell E et al (2014) Randomized controlled trial of a telephone-based intervention for child fruit and vegetable intake: long-term follow-up. Am J Clin Nutr 99:543–550. https://doi.org/10.3945/ajcn.113.071738
World Health Organization. Healthy Diet (2018) https://www.who.int/news-room/fact-sheets/detail/healthy-diet. Accessed Jan 2020
Wright K, Norris K, Newman-Giger J et al (2012) Improving healthy dietary behaviors, nutrition knowledge, and self-efficacy among underserved school children with parent and community involvement. Child Obes 8:347–356. https://doi.org/10.1089/chi.2012.0045
Wyse R, Wolfenden L, Campbell E et al (2012) A cluster randomized controlled trial of a telephone-based parent intervention to increase preschoolers’ fruit and vegetable consumption. Am J Clin Nutr 96:102–110. https://doi.org/10.3945/ajcn.111.030585
Yee AZ, Lwin MO, Ho SS (2017) The influence of parental practices on child promotive and preventive food consumption behaviors: a systematic review and meta-analysis. Int J Behav Nutr Phys Act 14(1):47. https://doi.org/10.1186/s12966-017-0501-3
Yoong SL, Grady A, Seward K et al (2019) The impact of a childcare food service intervention on child dietary intake in care: an exploratory cluster randomized controlled trial. Am J Health Promot 33(7):991–1001. https://doi.org/10.1177/0890117119837461
Funding
Partial funding from the USDA/NIFA Multistate Research Project W2005: “Parenting, energy dynamics, and lifestyle determinants of childhood obesity: New directions in prevention.”
Author information
Authors and Affiliations
Contributions
Conceptualization, N.F., R.I., J.K., and K.C-N; methodology, N.F., R.I., J.K., and K.C-N; software, K.D., H.M., N.F., F.D., R.I., J.K., and K.C-N; validation, K.D., H.M., N.F., F.D., J.K., and K.C-N.; formal analysis, K.D., H.M., N.F., F.D., R.I., J.K., and K.C-N; investigation, K.D., H.M., N.F., F.D., R.I., J.K., and K.C-N; resources, N.F., F.D., R.I., J.K., and K.C-N; data curation, K.D., H.M., N.F., F.D., R.I., J.K., and K.C-N.; writing—original draft preparation, K.D., H.M., N.F., F.D., J.K., and K.C-N.; writing—review and editing, K.D., H.M., N.F., F.D., R.I., J.K., and K.C-N; visualization, N.F., R.I., J.K., and K.C-N; supervision, J.K., and K.C-N.; project administration, J.K., and K.C-N.; funding acquisition, J.K., and K.C-N. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
All authors have reviewed and approved the manuscript for publication consideration.
Conflicts of interest
The authors declare that they no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Muzaffar, H., Difilipo, K.N., Fitzgerald, N. et al. A systematic review of interventions to improve the diet of children. J Public Health (Berl.) (2024). https://doi.org/10.1007/s10389-024-02258-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10389-024-02258-3