Abstract
Background
Globally, artificial intelligence (AI) is expanding in healthcare and public health and AI education for students in these fields will be essential. It is therefore important that future public health professionals are aware of opportunities and challenges linked to AI.
Aim
The aim of the study was to assess the perceptions and attitudes regarding AI among one such group of future public health professionals – Postgraduate Diploma in Public Health students – in South Africa.
Methods
An online survey was sent to students enrolled for the Postgraduate Diploma in Public Health programme from 13 June 2022 to 17 June 2022.
Results
Six hundred and eighteen respondents completed an online survey (81.5% response rate). Generally, respondents thought AI would be capable of performing various tasks that did not provide direct care to individuals. Most (69%) agreed that introduction of AI could reduce job availability in public health fields. Respondents agreed that AI in public health could raise ethical (84%), social (77%) and health equity (77%) challenges. Relatively few respondents (52%) thought they were being adequately trained to work alongside AI tools, and the majority (76%) felt training of AI competencies should begin at an undergraduate level.
Conclusion
Respondents expect AI to eventually carry out specific functions in public health and had reservations that AI may cause ethical challenges and increase unemployment in the country. Further exploration is needed regarding the perceptions about AI and its integration into the health system and the implications for undergraduate and postgraduate curricula.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Artificial intelligence (AI) is the use of software technology designed to perform multiple decision-making tasks (Vinuesa et al. 2020). There are different branches of AI that are aimed to enable computers to learn without being programmed, thus improving the computers’ performance to execute tasks (Samuel 1959; Mitchel 1997). The term AI was established as early as 1956 (Schmidt-Erfurth et al. 2018), and similar concepts such as machine learning (ML) and deep learning (DL) were also conceptualised during that time (Dhande 2020).
AI is commonly used in the business and marketing sectors (De Bruyn et al. 2020; Di Vaio et al. 2020; Dimitrieska et al. 2018; Dirican 2015; Loureiro et al. 2021), and is used in the health sector in a number of ways for diagnostic tools, HIV research, and in clinical monitoring (Aguiar et al. 2016; Go et al. 2018; Schmidt-Erfurth et al. 2018; Sinisi et al. 2007). In low-to-middle income countries, the main focus of AI interventions has been on health issues such as tuberculosis (Aguiar et al. 2016; Jaeger et al. 2018; Lopes and Valiati 2017), malaria (Andrade et al. 2010; Go et al. 2018), non-infectious diseases in children and infants, and cervical cancer (Schwalbe and Wahl 2020). Although research concerning AI in public health in Africa is growing, AI applications in public health and medical studies are more prominent in countries such as China, the United States of America and in Europe (Bellinger et al. 2017; Cisse 2018; Ferrein and Meyer 2012). The introduction of AI and its application in healthcare and public health have the potential to improve clinical decision-making and efficiency in managing large clinical datasets (Oakden-Rayner 2020; Rajkomar et al. 2019; Topol 2019).
The use of AI in South Africa is increasing, and several studies show the use of AI application in healthcare and medical studies and its potential benefits (Dlamini et al. 2020; Kim et al. 2019; Madahana et al. 2022; Mbunge et al. 2022; van Heerden and Young 2020). Additionally, ML has also been used as a prediction tool in the provision of healthcare services and placements of healthcare workers (Moyo et al. 2018). The extent and implementation of AI and ML in epidemiology, in an African context, is in the early stages leaving room for exploration (Liyanage et al. 2019).
In the post-coronavirus era there has been an increased interest in the use of AI to derive meaningful information from the large amount of health information that is produced (Manteghinejad and Javanmard 2021). As useful as the applications of AI in healthcare and public health are, little is known regarding the preparedness of those who will be expected to use these applications. Few studies have been done to assess the attitudes and perceptions of those who are studying to work in public health regarding the use of AI in their work (Emmert-Streib et al. 2020; Liyanage et al. 2019; Mehta et al. 2021). Generally, there are certain misperceptions and attitudes around AI and its general potential (Albarrán Lozano et al. 2021; Emmert-Streib et al. 2020). In South Africa, these perceptions of AI in public health have not been explored. Therefore, the aim of this study was to assess the perceptions and attitudes regarding AI in public health among one of the largest programmes in South Africa, i.e. students registered for the online Postgraduate Diploma in Public Health at the University of Pretoria.
Methods
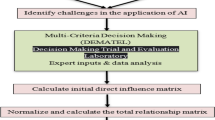
A cross-sectional survey was conducted. The data collection was done over five days from 13 June 2022 to 17 June 2022. The questionnaire was adapted from a Canadian study that explored the same topic among medical students (Mehta et al. 2021).
The questionnaire was created in Qualtrics before an online invitation was sent to students who were attending an online module. Consent from the students was obtained through the first page of the survey.
The questionnaire had three designated sections: (A) demographics of the respondents that included the gender, age, residence, the interaction with computer science and AI; (B) basic knowledge of AI terminology, including AI, ML, DL, neural networks (NN) and an algorithm; and (C) perceptions of AI in public health. This last section was separated into four subsections, namely the perceptions of AI and task performance at individual primary care, health systems and population, perceptions of AI and impact on public health careers, perceptions of AI and ethics and perceptions of AI and public health education.
The data from Qualtrics was exported to a Microsoft Excel spreadsheet before being imported to STATA 15, where all demographic and statistical analysis were performed.
The scaled questions regarding perceptions and attitudes are reported in percentages. Content analysis was used to analyse the open-ended responses obtained from the questionnaires. Chi-square tests were applied to assess the correlations between sections B and C and the demographic information captured in section A.
Results
Demographics
There were 758 responses received, and 618 questionnaires were completed in full with no missing values (81.5% response rate). Most of the respondents (82%) were female, 17.9% were male, and less than 1% chose not to indicate their gender (Table 1). The majority of the respondents were younger than 40 years old. Most of the respondents (83.5%) did not have any computer science background. Less than 15% of respondents had attended or viewed AI related talks or lectures.
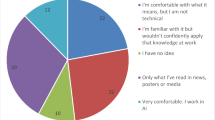
Knowledge of AI terminology
Respondents’ understanding of general terminology varied among the different terms. The majority (77.9%) of the respondents at least agreed that they understood what artificial intelligence is and 51.4% similarly agreed that they understood machine learning. Other terms such as neural networks, deep learning and algorithms that are associated with/related to deeper knowledge of artificial intelligence, were unknown to most of the respondents (Supplementary Table 1).
Perceptions of AI and task performance
Table 2 shows how likely respondents thought AI could perform tasks at an individual patient care level. Respondents thought it at least likely that AI could perform administrative, diagnostic and prognostic task, e.g. the vast majority thought AI would be likely to read and interpret diagnostic imaging (89.1%). However, respondents did not think it likely the AI would be able to perform tasks that involved direct care to patients. Only 28% of respondents thought AI could provide empathetic care and only 26% felt that it could perform psychiatric/personal counselling.
Respondents who thought it likely for AI to provide preventative health recommendations (31.1%) and read and interpret diagnostic imaging (29.7%), felt that this would be possible in the next 5 to 10 years. Overall, respondents thought AI performance of other tasks would be possible within 11 to 25 years. Details of expected time respondents perceived AI to eventually perform a specific task at an individual health level can be found in Supplementary Table 2.
The majority of respondents thought it possible for AI to perform tasks at a health systems level (Table 3). Among those who thought it likely, approximately 29% responded that AI could be able to perform most of these tasks within the next 5 to 10 years (Supplementary Table 3).
Table 3 also shows that respondents also thought it likely that AI could perform tasks at a population health level, with 61.9% thinking it likely that AI could conduct population health surveillance and outbreak prevention. However, of the respondents who thought it likely for AI to perform tasks at a population level, approximately 30% thought that this could occur within 11 to 25 years (Supplementary Table 3).
Perceptions of AI and impact on public health careers
Respondents thought that AI would not only reduce job availability to them (77%) but the number of jobs in public health in general (69.4%). This reality did seem to influence the consideration of the specialty as the majority (53.8%) were unsure or at least agreed that this would be the case (Supplementary Table 4).
Perceptions of AI and ethics
Respondents strongly agreed or agreed that AI in public health would introduce new ethical (84.9%), social (77.4%) and health equity (77.2%) challenges. When asked if respondents thought the South African healthcare system was currently well prepared to deal with challenges related to AI, 78.6% disagreed or strongly disagreed (Table 4).
Perceptions of AI and public health education
A small majority (52.9%) of respondents agreed that their current public health education was adequately preparing them to work alongside AI and there was very strong support (91.4%) for the inclusion of AI in public health training (Supplementary Table 5). This inclusion could start at an undergraduate level (76 %).
An analysis of the open-ended responses was done. These responses were non-compulsory open-ended questions on whether they had any comments or concerns about AI in public health.
There were 327 free text responses to the question ‘Do you have any comments on the topic of AI in public health?’ Examples of some of the responses are highlighted in Table 5.
Respondents were also asked to give a general reflection on AI within their department in the next five years. There were 418 responses. Some examples of the responses are highlighted in supplementary Table 6.
Chi-square of independence tests were performed to assess whether gender, age group, highest qualification obtained, background in computer science and attendance of AI talks or lectures had any effect on the perceptions on AI in public health. The female respondents showed better understanding of terms such as ML (p = 0.0003), NN (p = 0.01) and an algorithm (p = 0.01) than the male respondents. Respondents who had a background in computer sciences showed better understanding of ML (p = 0.0003), NN (p = 0.01), DL (p = 0.001) and an algorithm (p = 0.01). Respondents who had not attended AI talks or lectures showed less understanding of all AI terminology (p < 0.05). Generally, demographic factors such as age, gender and highest qualification did not significantly influence respondents perception on whether AI could eventually perform a specific task at an individual level (p > 0.05). However, in some instances, respondents who had a background in computer science and attended AI talks/lectures thought AI was more likely to perform some individual tasks. Demographic factors did not significantly influence the respondents’ perceptions on whether AI could eventually perform a specific task at health systems or population health levels (p > 0.05).
Similarly, the demographic factors did not significantly influence the way respondents’ perceived AI impact on public health careers or ethical challenges from AI (p > 0.05). There was one exception from the latter where all demographic factors showed to influence respondents perceptions on whether ‘The South African healthcare system is currently well prepared to deal with challenges related to AI (p < 0.05)’. Respondents who had a background in computer science (p = 0.04) and attended AI talk/lectures (p = 0.01) felt that their public health education was not adequately preparing them for working alongside AI tools. However, these demographic factors did not significantly influence the perceptions of other questions asked in this section.
Discussion
The aim of this study was to assess the perceptions and attitudes regarding AI in public health among postgraduate public health students at one university in South Africa.
The survey respondents were mainly female, which is a reflection of the demographic profile of the student population. In some health studies, there is often a slightly larger female population involved (Stai et al. 2020; Tiyuri et al. 2018) unless the study is male specific (Dada et al. 2020); otherwise, the gender balance is often dependent on the country and career of interest in which the study is taking place (Yüzbaşıoğlu 2021). The majority of the respondents in this study were in the 25 to 40-year-old age group, which is a common age group of online postgraduate students (Dada et al. 2020; Fernandez et al. 2014; Tiyuri et al. 2018). Similar to the Mehta et al. (2021) study, the majority of the respondents in this study did not have any background in computers or had been exposed to AI lectures or talks. The respondents’ lack of exposure to AI lectures or talks is evident in their responses regarding familiarity with AI terminology. Their lack of familiarity with terms such as deep learning and neural networks is similar to what was reported in a Canadian cohort (Mehta et al. 2021).
Respondents were confident that AI would be able to carry out many tasks at different levels of public health. These identified tasks were tasks that could not provide direct care to patients, such as empathetic care or counselling. Respondents felt that administrative, diagnostic and prognosis tasks were better suited for AI advancements in public health. Mehta et al. (2021) also found that their participants were more confident the AI would be able to perform ‘objective’ tasks such as diagnosis, prognosis, interpreting imaging and formulating prescriptions as compared to tasks requiring more person-centred skills, personal counselling and providing empathetic care. Gender, age, level of qualification, a background in computer science and the attendance of AI talks or lectures did not show to have a significant impact on the perceptions made by respondents. However, Stai et al. (2020) found that age made a significant difference in participants’ perception of AI’s ability to perform certain tasks such as surgery. A meta-analysis done by Hauk et al. (2018) found it was a misconception that younger generations would be more likely to engage in advancing technology, but rather technology is better taken up by how easy it is to use rather than the age of the individual. The findings of this study seems to echo the latter sentiment as age did not impact the respondents’ perceptions of AI’s ability to perform certain tasks in public health.
Some issues were raised about AI affecting job availability at an individual and general level in public health. The general perception was that AI would increase unemployment. In similar studies conducted in Canada, Spain and Turkey, the perception that the use of AI would reduce the number of jobs was also recorded as a concern (Albarrán Lozano et al. 2021; Mehta et al. 2021; Yüzbaşıoğlu 2021). Unemployment in South Africa is a general concern as the current unemployment rate is close to 30% (Marire 2022; Mazorodze and Nsiah 2020). This high unemployment rate could be the reason why respondents focused on this aspect. The concern about job availability after the introduction of AI in public health could also be a result of fear of possible redundancy of certain jobs in public health. Because AI can run certain repetitive tasks and leave the more challenging tasks for healthcare professionals, there is a concern that this would then change or reduce their roles in the workplace (Chen et al. 2021; Tursunbayeva and Renkema 2022). In spite of the positive benefits AI in healthcare and public health may promote, the concern of job replacement and job loss is a prominent issue. Another reason why perceptions of AI may be taken negatively, could revert back to the misconceptions around the topic. AI can be thought to be a type of technology that allows computers to think, but that is not the case (Emmert-Streib et al. 2020; Liu and Bressler 2020). While AI is a part of computer science, the findings showed that having a background in computer science or attending AI talks or lectures did not influence the perceptions of the effects of AI in public health careers.
A rise in ethical challenges was also highlighted as an issue that could result from introducing AI into public health. Respondents perceived that the introduction of AI would raise ethical, social and health equity issues. Concerns about hacking of private information was also raised. Patient and hospital information is a very sensitive matter in health and there is already difficulty in acquiring such data (Reisman 2017). There is therefore a legitimate concern about data being shared and liability should patient information be wrongfully accessed (Petersson et al. 2022; Reisman 2017). Although this was not highlighted in the study findings, it is an interesting factor to consider when assessing possible ethical issues around AI in public health.
Health equity was another concern highlighted by the respondents, specifically concerning how AI implementation could increase the gap between lower- and upper-income groups. This concern is valid due to the current, severe socio-economic disparities in South Africa (Gordon et al. 2020; Mutyambizi et al. 2019; Rispel 2016; Wilson 2011). In contrast to this concern, some research has found that the use of AI technologies is optimistic and could be a means for developing nations’ abilities to address their health disparities (Akpanudo 2022; Marcus et al. 2020; Owoyemi et al. 2020; Vinuesa et al. 2020). Respondents overwhelmingly agreed that the South African healthcare system was currently not prepared to handle AI-related challenges. The health department has been reported to have mismanaged funds and experiences a shortage of healthcare facilities and staff to meet the demand of the population (Aikman 2019). These shortcomings were highlighted during the recent Covid-19 pandemic that further strained the healthcare system (Mokhele et al. 2022; Taylor et al. 2021). The manner in which the pandemic was handled could be a reason why a large proportion of respondents do not feel confident that AI-related challenges would be dealt with by the current healthcare system.
Gender, age, having a background in computer science and attending an AI talk or lecture showed a significant association with the ethical challenges of AI and the country’s readiness to address these challenges that may arise. Similar studies did not look at the associations of the demographics and AI and ethics (Mehta et al. 2021; Yüzbaşıoğlu 2021; Stai et al. 2020). However some did find that in general, female respondents had more positive perceptions towards AI in dentistry (Yüzbaşıoğlu 2021) and the publics’ opinion of AI in surgery (Stai et al. 2020). Although these findings were similar to this, the distribution of female to male respondents was quite disproportional.
The majority of respondents agreed that being introduced to AI competencies should be done early in undergraduate training. Due to the ‘newness’ of the topic of AI, people may be very unsure about it but may be willing to learn more (Mehta et al. 2021; Yüzbaşıoğlu 2021). Although with current misconceptions, people may have no interest at all to learn more on the topic (Albarrán Lozano et al. 2021). A lot of effort needs to be done to restructure the misconceptions on AI, reducing the popularity and marketing definition of AI and inform its useful scientific capabilities (Emmert-Streib et al. 2020; Cukurova et al. 2020). Whilst AI may be perceived as a complex concept, curricular content for AI in public health and medicine can be structured around basic understanding of AI concepts, limitations, and relevant ethical and legal implications (Davenport and Kalakota 2019; Kolachalama and Garg 2018; McCoy et al. 2020; Mehta et al. 2021). This educational strategy could better prepare public health students to accept and understand AI.
The main strength to the study is that it is the first study conducted at a South Africa university to address the subject of AI in public health. The study addressed one of the nine strategic interventions of the National Digital Health Strategy for South Africa (2019–2024), namely ‘to develop enhanced digital health technical capacity and skilled workforce for digital technology support and implementation’ (Department of health 2019). The findings of this study provide baseline information as a foundation for similar studies to be done at other South African tertiary institutions. A study limitation is that this study explored the topic among one group of students at one university and therefore the findings are not generalisable.
The study provides an argument for an introductory AI course in undergraduate and/or postgraduate health professions and public health. This introduction can encourage further AI research by public health professionals in the country as there are no current courses offered within public health curricula that offer AI and ML. However, the introduction of AI in public health education is limited by the lack of expertise on the subject. Although AI in computer science is more available, constructing a more ‘user friendly’ curriculum for public health students will still need more time to implement and need a balanced contribution from both computer science and public health to make it fit for purpose. It is therefore recommended that this is an area for future joint curriculum development and research collaboration that needs exploration.
Conclusion
In conclusion, this survey brought out a variety of views shared among future public health professionals. There was a general assumption about AI entering public health and performing particular tasks at different health levels. However, there was a general consensus that AI had the potential to increase unemployment and ethical challenges in the field. These concerns could be attributed to existing high unemployment rates and mistrust in the government in South Africa. Overall, this study does create a baseline for more extensive in-depth studies to be done within an African context. It is recommended that further studies be done that include participants from more and different programmes within health faculties in different settings. This could lead to a better educational strategy that integrates the understanding and application of AI into the health system and the implications for undergraduate and postgraduate curricula. This could result in an increase in the use of AI in South African public health research.
Data availability
The data will be available upon reasonable request from the authors.
References
Aguiar FS, Torres RC, Pinto JV, Kritski AL, Seixas JM, Mello FC (2016) Development of two artificial neural network models to support the diagnosis of pulmonary tuberculosis in hospitalized patients in Rio de Janeiro, Brazil. Med Biol Eng Comput 54(11):1751–1759
Aikman N (2019) The crisis within the South African healthcare system: a multifactorial disorder. S Afr J Bioeth Law 12(2):52–56
Akpanudo S (2022) Application of artificial intelligence systems to improve healthcare delivery in Africa. Prim Health Care 12(1):1–4
Albarrán Lozano I, Molina JM, Gijón C (2021) Perception of artificial intelligence in Spain. Telemat Inform 63:101672
Andrade BB, Reis-Filho A, Barros AM, Souza-Neto SM, Nogueira LL, Fukutani KF, Camargo EP, Camargo LM, Barral A, Duarte A, Barral-Netto M (2010) Towards a precise test for malaria diagnosis in the Brazilian Amazon: comparison among field microscopy, a rapid diagnostic test, nested PCR, and a computational expert system based on artificial neural networks. Malar J 9(1):1–11
Bellinger C, Mohomed Jabbar MS, Zaïane O, Osornio-Vargas A (2017) A systematic review of data mining and machine learning for air pollution epidemiology. BMC Public Health 17(1):1–9
Chen Y, Stavropoulou C, Narasinkan R, Baker A, Scarbrough H (2021) Professionals’ responses to the introduction of AI innovations in radiology and their implications for future adoption: a qualitative study. BMC Health Services Res 21(1):1–9
Cisse M (2018) Look to Africa to advance artificial intelligence. Nature 562(7728):461
Cukurova M, Luckin R, Kent C (2020) Impact of an artificial intelligence research frame on the perceived credibility of educational research evidence. Int J Artif Intell Educ 30(2):205–235. https://doi.org/10.1007/s40593-019-00188-w
Dada SO, Oyewole OE, Desmennu AT (2020) Knowledge as determinant of healthy-eating among male postgraduate public health students in a Nigerian tertiary institution. Int Q Commun Health Educ 42(1):103–114
Davenport T, Kalakota R (2019) The potential for artificial intelligence in healthcare. Future Healthc J 6(2):94–98
De Bruyn A, Viswanathan V, Beh YS, Brock JK, Von Wangenheim F (2020) Artificial intelligence and marketing: pitfalls and opportunities. J Interact Mark 51(1):91–105
Department of Health (2019) National Digital Health Strategy for South Africa (2019-2024), 978-1-920585-31-0, Pretoria, South Africa
Dhande M (2020) What is the difference between AI, machine learning and deep learning? Geospatial World. https://www.geospatialworld.net/blogs/difference-between-ai%EF%BB%BF-machine-learning-and-deep-learning/
Di Vaio A, Palladino R, Hassan R, Escobar O (2020) Artificial intelligence and business models in the sustainable development goals perspective: a systematic literature review. J Bus Res 21:283–314
Dimitrieska S, Stankovska A, Efremova T (2018) Artificial intelligence and marketing. Entrepreneurship 6(2):298–304
Dirican C (2015) The impacts of robotics, artificial intelligence on business and economics. Procedia Soc Behav Sci 195:564–573
Dlamini Z, Francies FZ, Hull R, Marima R (2020) Artificial intelligence (AI) and big data in cancer and precision oncology. Comput Struct Biotechnol J 18:2300–2311
Emmert-Streib F, Yli-Harja O, Dehmer M (2020) Artificial intelligence: a clarification of misconceptions, myths and desired status. Front Artif Intell 3:524339
Fernandez RS, Tran DT, Ramjan L, Ho C, Gill B (2014) Comparison of four teaching methods on evidence-based practice skills of postgraduate nursing students. Nurse Educ Today 34(1):61–66
Ferrein A, Meyer T (2012) A brief overview of artificial intelligence in South Africa. AI Magazine 33(1):99–103
Go T, Kim JH, Byeon H, Lee SJ (2018) Machine learning-based in-line holographic sensing of unstained malaria-infected red blood cells. J Biophotonics 11(9):e201800101
Gordon T, Booysen F, Mbonigaba J (2020) Socio-economic inequalities in the multiple dimensions of access to healthcare: the case of South Africa. BMC Public Health 20(1):1–13
Hauk N, Hüffmeier J, Krumm S (2018) Ready to be a silver surfer? A meta-analysis on the relationship between chronological age and technology acceptance. Comput Hum Behav 84:304–319
Jaeger S, Juarez-Espinosa OH, Candemir S, Poostchi M, Yang F, Kim L, Ding M, Folio LR, Antani S, Gabrielian A, Hurt D, Rosenthal A, Thoma G (2018) Detecting drug-resistant tuberculosis in chest radiographs. Int J Comput Assist Radiol Surg 13(12):1915–1925
Kim MC, Okada K, Ryner AM, Amza A, Tadesse Z, Cotter SY, Gaynor BD, Keenan JD, Lietman TM, Porco TC (2019) Sensitivity and specificity of computer vision classification of eyelid photographs for programmatic trachoma assessment. Plos One 14(2):e0210463
Kolachalama VB, Garg PS (2018) Machine learning and medical education. NPJ Digit Med 1(1):1–3
Liu TYA, Bressler NM (2020) Controversies in artificial intelligence. Curr Opin Ophthalmol 31(5):324–328
Liyanage H, Liaw ST, Jonnagaddala J, Schreiber R, Kuziemsky C, Terry AL, de Lusignan S (2019) Artificial intelligence in primary health care: perceptions, issues, and challenges. Yearb Med Inform 28(1):41–46
Lopes UK, Valiati JF (2017) Pre-trained convolutional neural networks as feature extractors for tuberculosis detection. Comput Biol Med 89:135–143
Loureiro SMC, Guerreiro J, Tussyadiah I (2021) Artificial intelligence in business: state of the art and future research agenda. J Bus Res 129:911–926
Madahana M, Khoza-Shangase K, Moroe N, Mayombo D, Nyandoro O, Ekoru J (2022) A proposed artificial intelligence-based real-time speech-to-text to sign language translator for South African official languages for the COVID-19 era and beyond: in pursuit of solutions for the hearing impaired. S Afr J Commun Disord 69(2):915
Manteghinejad A, Javanmard S (2021) Challenges and opportunities of digital health in a post-COVID19 world. J Res Med Sci 26(1):11
Marcus JL, Sewell WC, Balzer LB, Krakower DS (2020) Artificial intelligence and machine learning for HIV prevention: emerging approaches to ending the epidemic. Curr HIV/AIDS Rep 17(3):171–179
Marire J (2022) Relationship between fiscal deficits and unemployment in South Africa. J Financ Econ 15(1):12
Mazorodze BT, Nsiah C (2020) Youth unemployment and murder crimes in KwaZulu-Natal, South Africa. Cogent Econ Finance 8(1):1799480
Mbunge E, Batani J, Gaobotse G, Muchemwa B (2022) Virtual healthcare services and digital health technologies deployed during coronavirus disease 2019 (COVID-19) pandemic in South Africa: a systematic review. Glob Health J. https://doi.org/10.1016/j.glohj.2022.03.001
McCoy LG, Nagaraj S, Morgado F, Harish V, Das S, Celi LA (2020) What do medical students actually need to know about artificial intelligence? NPJ Digit Med 3(1):1–3
Mehta N, Harish V, Bilimoria K, Morgado F, Ginsburg S, Law M, Das S (2021) Knowledge and attitudes on artificial intelligence in healthcare: a provincial survey study of medical students. MedEdPublish 10(1). https://doi.org/10.1101/2021.01.14.21249830.
Mitchel TM (1997) Machine learning, 1st edn. McGraw-Hill, New York
Mokhele T, Manyaapelo T, Sifunda S, Dukhi N, Sewpaul R, Naidoo I, Mabaso M, Moshabela M, Reddy P (2022) Factors influencing healthcare workers’ perception of South African health system capability for managing COVID-19 pandemic. Open Public Health J 15(1)
Moyo S, Doan TN, Yun JA, Tshuma N (2018) Application of machine learning models in predicting length of stay among healthcare workers in underserved communities in South Africa. Hum Resour Health 16(1):68
Mutyambizi C, Booysen F, Stokes A, Pavlova M, Groot W (2019) Lifestyle and socio-economic inequalities in diabetes prevalence in South Africa: a decomposition analysis. Plos One 14(1):e0211208
Oakden-Rayner L (2020) Exploring large-scale public medical image datasets. Acad Radiol 27(1):106–112
Owoyemi A, Owoyemi J, Osiyemi A, Boyd A (2020) Artificial intelligence for healthcare in Africa. Front Digit Health 2:6
Petersson L, Larsson I, Nygren JM, Nilsen P, Neher M, Reed JE, Tyskbo D, Svedberg P (2022) Challenges to implementing artificial intelligence in healthcare: a qualitative interview study with healthcare leaders in Sweden. BMC Health Serv Res 22(1):850
Rajkomar A, Dean J, Kohane I (2019) Machine learning in medicine. N Engl J Med 380(14):1347–1358
Reisman M (2017) EHRs: the challenge of making electronic data usable and interoperable. Pharmacol Ther 42(9):572–575
Rispel L (2016) Analysing the progress and fault lines of health sector transformation in South Africa. S Afr Health Rev 2016(1):17–23
Samuel AL (1959) Studies in machine learning using the game of checkers. IBM J Res Dev 3(3):210–229
Schmidt-Erfurth U, Sadeghipour A, Gerendas BS, Waldstein SM, Bogunović H (2018) Artificial intelligence in retina. Prog Retin Eye Res 67:1–29
Schwalbe N, Wahl B (2020) Artificial intelligence and the future of global health. Lancet 395(10236):1579–1586
Sinisi SE, Polley EC, Petersen ML, Rhee SY, van der Laan MJ (2007) Super learning: an application to the prediction of HIV-1 drug resistance. Stat Appl Genet Mol Biol 6:Article7
Stai B, Heller N, McSweeney S, Rickman J, Blake P, Vasdev R, Edgerton Z, Tejpaul R, Peterson M, Rosenberg J, Kalapara A, Regmi S, Papanikolopoulos N, Weight C (2020) Public perceptions of artificial intelligence and robotics in medicine. J Endourol 34(10):1041–1048
Taylor A, Feuvre DL, Taylor B (2021) COVID-19: The South African experience. Interv Neurol 27(1_suppl):50–53. https://doi.org/10.1177/15910199211035905
Tiyuri A, Saberi B, Miri M, Shahrestanaki E, Bayat BB, Salehiniya H (2018) Research self-efficacy and its relationship with academic performance in postgraduate students of Tehran University of Medical Sciences in 2016. J Educ Health Promot 7
Topol EJ (2019) High-performance medicine: the convergence of human and artificial intelligence. Nat Med 25(1):44–56
Tursunbayeva A, Renkema M (2022) Artificial intelligence in health-care: implications for the job design of healthcare professionals. Asia Pac J Hum Resour. https://doi.org/10.1111/1744-7941.12325
van Heerden A, Young S (2020) Use of social media big data as a novel HIV surveillance tool in South Africa. Plos One 15(10):e0239304
Vinuesa R, Azizpour H, Leite I, Balaam M, Dignum V, Domisch S, Felländer A, Langhans SD, Tegmark M, Fuso Nerini F (2020) The role of artificial intelligence in achieving the Sustainable Development Goals. Nat Commun 11(1):233
Wilson F (2011) Historical roots of inequality in South Africa. Econ Hist Dev Reg 26(1):1–15
Yüzbaşıoğlu E (2021) Attitudes and perceptions of dental students towards artificial intelligence. J Dent Educ 85(1):60–68
Funding
Open access funding provided by University of Pretoria.
Author information
Authors and Affiliations
Contributions
The study conception and design was conceptualised by JW. All authors were involved in the material preparation. Data collection was performed by SMP, MvV and JWol. Data analysis was performed by NSM. The first draft of the manuscript was written by NSM and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics
This study was approved by the Faculty of Health Sciences Research Ethics Committee at the University of Pretoria (171/2022).
Consent to participate
Consent to participate in the study was acquired prior to taking the survey. No identifying information was included in the findings.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 47 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mwase, N.S., Patrick, S.M., Wolvaardt, J. et al. Public health practice and artificial intelligence: views of future professionals. J Public Health (Berl.) (2023). https://doi.org/10.1007/s10389-023-02127-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10389-023-02127-5