Abstract
Objectives
Renal blood flow (RBF) is controlled by a number of physiological factors that can contribute to the variability of its measurement. The purpose of this review is to assess the changes in RBF in response to a wide range of physiological confounders and derive practical recommendations on patient preparation and interpretation of RBF measurements with MRI.
Methods
A comprehensive search was conducted to include articles reporting on physiological variations of renal perfusion, blood and/or plasma flow in healthy humans.
Results
A total of 24 potential confounders were identified from the literature search and categorized into non-modifiable and modifiable factors. The non-modifiable factors include variables related to the demographics of a population (e.g. age, sex, and race) which cannot be manipulated but should be considered when interpreting RBF values between subjects. The modifiable factors include different activities (e.g. food/fluid intake, exercise training and medication use) that can be standardized in the study design. For each of the modifiable factors, evidence-based recommendations are provided to control for them in an RBF-measurement.
Conclusion
Future studies aiming to measure RBF are encouraged to follow a rigorous study design, that takes into account these recommendations for controlling the factors that can influence RBF results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal blood flow (RBF) has an important role in providing high capillary pressure to drive glomerular filtration and maintain oxygen supply to meet the demands of renal metabolism. A well-recognized feature of the renal circulation is its ability to maintain RBF at a relatively constant level as a result of autoregulation [1]. This mechanism is essential for preserving body fluid balance and protecting the glomerular capillaries from an increase in blood pressure. Renal autoregulation does not imply that RBF is unchangeable, as RBF is known to change remarkably with daily activities [2, 3]. This is because the kidney actively participates in blood pressure regulation [4] through baroreceptor reflex and the release of vasoactive agents [5] which ultimately modulate renal haemodynamics.
Alterations in renal microcirculation play a critical role in the pathophysiological mechanisms of renal disease [6]. Measurement of RBF is therefore considered an important biomarker in the evaluation of renal function. However, a significant problem in the interpretation of RBF is the large heterogeneity of normal reported values due to combination of measurement error and inherent physiological changes of RBF [7]. While it is difficult to distinguish between the two effects, understanding and quantifying potential physiological factors can promote standardization and reduce variability in RBF measurements. Such standardization is essential to ensure that disease-related changes are not confounded by physiological events.
Recently, a consensus-based project has outlined a number of technical recommendations to improve the standardization of renal biomarkers such as RBF, perfusion and blood oxygen level dependent (BOLD) magnetic resonance imaging (MRI) [8,9,10]. The results highlighted a lack of consensus among experts concerning aspects of patient preparation due to incomplete understanding of the impact of physiological variability.
The aim of this review is to develop a practical reference for the preparation and interpretation of RBF values. For this purpose, a literature review was conducted to identify and assess a wide range of factors that can contribute to the variability in RBF in heathy humans. Based on brief discussion of the variability in the applied techniques and a comprehensive analysis of the physiological variability in the literature, evidence-based recommendations will be formulated for future studies aiming to achieve a more standardized approach for RBF quantification.
Materials and methods
Scope
Different biomarkers quantify the amount of blood delivered to the kidney. Renal blood flow (RBF, expressed in mL/min) measures the delivery of blood at the macrovascular level, whereas tissue perfusion (expressed in mL/min/100 mL) measures delivery to the capillaries at the microvascular level. Measurements of RBF are often indexed to body surface area (BSA) and presented per 1.73 m2, thereby providing comparable estimates between different populations.
Different methods are available to measure RBF [Clearance technique, Radionuclide scintigraphy, Doppler ultrasound (US), and Phase contrast MRI (PC)], or perfusion [Positron emission tomography (PET), Dynamic contrast enhanced (DCE) and Arterial spin labelling (ASL)]. Reference values tend to be dependent on the measurement methodology used and are summarized in Table 1. All these methods are considered in this review, assuming that relative changes under influence of confounders are comparable even if absolute values are not. Analysis of this review was based on RBF (mL/min) with renal perfusion studies only interpreted in the results section.
Literature search and selection
An initial exploratory search was performed using Pubmed, Ovid MEDLINE and Web of Science databases with the terms physiological, biological, variability and ‘renal circulation’. Articles obtained from this search were used to determine a list of physiological factors that cause changes in RBF. The identified factors focussed both on normal physiological changes that cause within- or between-subject variation in RBF. Each identified factor was searched individually to include studies up to June 2021. The search terms used for each influencing factor are provided in Table 2. Reference lists from acquired articles were also searched for inclusion of relevant studies. English, full-text articles reporting perfusion, blood and/or plasma flow in adult human subjects were included in this review.
Data synthesis
The magnitude of change was determined for each factor as the absolute (mL/min) and relative (%) difference of baseline RBF values. Results are presented as mean (and range) of absolute and relative change in RBF across studies. Since renal dysfunction can modulate the renal response to some physiological factors, only studies reporting on subjects with normal kidney function were included in the analysis. When RPF was reported, a conversion to RBF was made assuming a haematocrit value of 42% known from the literature [11], except where haematocrit was reported in the original study.
Results
The search terms yielded a total of 6987 articles, after removing duplicates. Following abstract and title screening and assessing for eligibility, 215 full-text articles were reviewed. A total of 162 original studies were summarized and included in this review; of which 110 studies reported quantitative measurement for the absolute and/or relative change. These studies investigated the effect of 24 potential factors on renal circulation.
The factors were divided into non-modifiable and modifiable. Non-modifiable factors essentially compromise the demographic characteristics of a population, such as age, sex, and race. While these factors cannot be manipulated in an experiment, acknowledging their impact on the measured RBF means that researchers can account for those in the study design or data analysis. The modifiable factors include a range of activities which can be controlled for in an experiment. Figure 1 shows the absolute change in RBF obtained from each study for all identified factors. The estimated absolute and relative change in RBF average across studies were summarized in Table 3 and presented in Fig. 2.
Non-modifiable factors
Age
The kidney undergoes multiple changes with advanced age, including reduced renal function [12], decreased kidney size, and alterations in blood flow. Changes in RBF with normal ageing are well-documented and have been reported using different methods. Davies and Shock [13] were one of the first to report the decline in resting RBF in adults after the age of 40. In this study, baseline measurements using clearance methods were compared in male subjects aged between 20 and 90 years old. Differences in RBF were observed between age groups for each decade with the largest reduction (53%) between the youngest and the oldest groups from a mean of 1170 to 433 mL/min. This observation has consistently been reported by other investigators using PAH clearance [14,15,16,17], 99mTc-MAG3 scintigraphy [18] and similarly using PC-MRI [19, 20]. Renal cortical perfusion estimated with ASL and DCE showed lower values in the older adults and negative association with advanced age [20,21,22]. Collectively, RBF was found to decrease after the age of 40 by − 10% each decade with an average decline of − 85 mL/min per decade (range from − 49 to − 106 mL/min) between different studies [13, 16, 19]. The effect of age is important and should therefore be considered when interpreting RBF between subjects of different age groups.
Sex
The total RBF in women was found to be − 20% (range − 16 to − 23%) lower than men by an average of − 243 mL/min (range − 187 to − 385 mL/min) [16, 19, 23,24,25]. The effect of gender on the renal haemodynamics appears to be driven by the protective action of oestrogen in women during reproductive age [26]. As a result, an interaction between age and gender was demonstrated, where gender-related differences were found to disappear after the age of 60 [16, 19]. The gender effect on RBF can also be secondary to the difference in body size and kidney volume between men and women [27]. The findings reported by Berg [23] suggest no differences when the measurement was indexed to 1.73 m2 BSA. While it remains unclear whether there is a truly physiological difference, the gender effect appears to be important and should be considered.
Race
Race has long been considered a critical variable in the estimation of glomerular filtration rate (eGFR). The misuse of race in the assessment of renal function is subject to an ongoing debate [28], and a replacement of current eGFR equations is under evaluation [29]. However, studies investigating racial differences for RBF are limited. Using PAH clearance, RPF of African Americans was found to be 16% lower than age-matched Caucasians when participants followed a high-salt diet [30]. The difference in RPF between the two groups disappeared when switching to a low-salt diet in a subsequent study [31]. These data suggest an underlying physiological difference between the two ethnic groups, which involve a blunted renal response to angiotensin-II receptor antagonist in the kidneys of African Americans [32]. There is also some evidence pointing towards the involvement of genetic factors, whereby specific gene variants appear to be associated with RPF variations in individuals of African descent [33]. Future studies on sufficiently large population and including other racial groups are necessary to better understand how race, social and genetic factors interact to affect kidney function.
Body mass index
The effect of body mass index (BMI) on renal haemodynamics is not specific to obesity or being overweight as it appears across wide BMI ranges. Comparing lean (BMI: 18–25 kg/m2) and overweight subjects (BMI: 25–35 kg/m2), with normal kidney function, showed a marked positive correlation with renal circulation [25, 34], and an increase in RBF on average by 20% (range 13–31%) with higher BMI [34,35,36]. The relation between BMI and RBF persists even when adjusted for age and sex [37, 38]. A reduction in RBF with weight loss following bariatric surgery has also been reported [39, 40]. However, renal perfusion measured using 15O-H2O PET in both cortex and medulla was not affected by changes in weight between normal and obese [40]. Of note, correcting RBF for body dimensions (expressed per 1.73 m2 BSA) was found to be negatively associated with BMI [37, 38, 41]. Indexing for height has been suggested as an alternative approach [42], in which the association with RBF was found to be eradicated and therefore, make the measurement more comparable between individuals. However, this alternative way of indexing was not widely adopted as it would lead to the same error as BSA in populations of variable height measurements. Overall, the effect of BMI is apparent and should be considered when comparing RBF between subjects with variable body dimensions.
Pregnancy and menses
Major changes in RBF were noted during pregnancy, which can occur as early as the sixth gestational week [43]. Serial studies using PAH clearance performed on pregnant women showed substantial increase in RBF during the first trimester by an average of 514 mL/min (range 434–625 mL/min) [44,45,46,47] reaching maximal level at ~ 12 gestational week [43]. Although a marked reduction in RBF is expected during the third trimester − 308 mL/min (range − 631 to − 117 mL/min), the value remains to be 30% (range 14–61%) higher than the measurement obtained from non-pregnant women [44,45,46,47]. Women investigated before pregnancy and after delivery showed no difference between measurements [45], indicating a return to normal values after childbirth [47].
Similar changes in RBF, but at smaller effect 8% (range 7–10%), were noted during the menstrual cycle [48]. In the luteal phase of the menstrual cycle, RBF measured using PAH clearance was found to increase on average by 77 mL/min (range 58–95 mL/min) [49]. This small variation in RBF was not detected in some studies using the same clearance method [50, 51].
Taken together, changes in RBF during normal pregnancy are substantial and if not considered can be confounded with hyperaemia. The impact of the menstrual cycle on RBF appears to be relatively small but controlling for this effect can inform a rigorous study design. In any case, querying information regarding menstrual health and history for female participants should be considered.
Modifiable factors
Circadian cycle
A typical circadian cycle of renal haemodynamics exhibits a sinusoidal course [52], with peak and trough observed at late daytime wakefulness and night-time sleep, respectively [53]. Using the clearance technique, the average amplitude of change in RPF with day-night cycle was found to be 35% (range 25–52%) [52, 54,55,56]. A similar pattern was observed in global renal perfusion values, measured with ASL, which is more pronounced in the cortex than medulla [56]. In one study, no change in RPF was found when subjects were maintained at bed rest throughout the experiment [57], suggesting that circadian fluctuation of the renal circulation can be driven by behavioural stimulant such as changes in activity, food and fluid consumption during the day [58]. Nevertheless, the effect of circadian rhythms has been found to be persistent when identical meals were taken at regular intervals throughout the 24 h [3]. In line with these data, acquiring RBF measurement during a fixed time of the day should be considered to minimize the influences of daily cycle.
Food intake
Food intake is accompanied by profound cardiovascular changes in which hormonal and nervous systems are engaged to promote the digestion, absorption, and storage of nutrients in the body. Postprandial change in renal circulation is evident and depends on the size and macronutrient content of the meal.
The intake of high-energy fatty meal (142 g fat) was associated with a modest but sustained increase in RBF measured with PC-MRI of 23% after 20 min [59]. No change in RBF was observed after ingestion of mixed meal high in carbohydrate (> 90 g) in 1 h [60] or 4 h duration [61] using ultrasound.
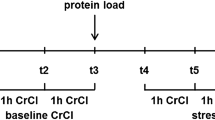
After the ingestion of high protein meal, RBF measured with PAH clearance was found to increase by an average of 260 mL/min (range 150–390 mL/min) with peak values achieved 60–120 min postprandially [62,63,64,65,66,67]. The test meal used in these trials contained 80–90 g (1.2 g/kg) of different types of animal protein (including lean meat or dairy products) [64, 67]. Reducing the amount of protein (0.55 g/kg) appears to be associated with smaller renal response [68]. Two studies looked at RBF changes using PAH clearance in response to vegetarian protein, but the results are not aligned. One study showed no acute changes in RPF after consuming 80 g soy protein meal compared to meat meal in healthy subjects [69]. Another showed 14% increase in RPF values 90 min after intake of 77 g soy protein [70]. Given the small number of participants in both studies (n ≤ 10), it is difficult to conclude whether or not plant-based protein will elicit short-term changes in renal haemodynamics. The inconsistency between findings could be attributed to differences in the follow-up duration between studies, or heterogeneity in the soy protein supplement and the amino acid composition.
Studies investigating the chronic response of protein diet showed similar results to single-meal protein experiments. High protein diet (2.0 g/kg/day) was found to increase RPF compared to low protein diet (0.5 g/kg/day) when consumed for period of 6 days [71] or 3 weeks [72] in the adult kidney, but not in the elderly [73]. Switching from animal to vegetable-based protein diet for a period of 3 weeks was associated with lower resting RPF in healthy subjects [69, 74].
A trend towards higher RBF in individuals following high sodium diet (> 200 mmol/day or 11.7 g/day) compared to low sodium diet (50–70 mmol/day or 3–4 g/day) for period of 5–7 days was described in some [75,76,77], but not all studies [78, 79]. While PAH clearance was applied in all studies, the discrepancy might be explained by the amount of water intake which is known to enhance renal sodium excretion and hence modify the RAS-activity expected from a low sodium diet [80].
Since meal consumption is often associated with RBF changes, fasting before the study is commonly used. Low baseline RBF value was observed in some studies [63, 81, 82] in which the authors have attributed to overnight fasting, but no empirical study has yet sufficiently addressed this point. While awaiting further insight from future studies on the matter, a preliminary conclusion can be reached from the literature synthesis as to stress the importance of controlling food intake prior to RBF measurement.
Fluid intake/hydration
Water loading (20 mL/kg) induced a 10% increase in total RBF measured using PC-MRI [83], but no changes were observed in perfusion values of the cortex and medulla estimated using ASL [84]. In both studies, the renal response was evaluated relative to fasting conditions (i.e. fluid restriction). Comparing different hydration levels (high: 24 mL/kg vs. low: 3 mL/kg) using PAH clearance showed contradictory results. One study reported no change in RPF with different degree of water loading [85], while another found lower RPF (− 13%) in the higher hydration regimen [81]. Sampling error associated with the use of different methods for urine collection (spontaneous voiding [85] versus bladder catheterization [81]) imply that these findings should be interpreted with caution. A study conducted using 131I-hippuran scintigraphy showed that hydration did not affect the measurement of RBF, despite large inter-individual differences in RBF response [86]. The authors concluded that hydration can be advantageous as it aids rapid transport of radioactivity, and therefore peak activity can be achieved at an earlier time.
While the magnitude and direction of change in response to hydration status remains elusive, it can be inferred that acute physiological changes in RBF may appear in cases of sub-optimal or excessive hydration. There is no evidence against the regular intake of water which is in line with the recent consensus recommendation for PC-MRI [9].
Smoking, caffeine, and alcoholic consumption
Cigarette smoking has a profound systemic vasoconstriction effect associated with increased sympathetic stimulation and these responses are specific to nicotine component of the cigarettes. Chewing nicotine gum (4 mg) was associated with acute reduction (− 15%) in RPF in non-smokers [87, 88]. Habitual smokers, however, showed impaired renal response following active smoking (2–3 mg nicotine) [89], suggesting the development of nicotine tolerance in these individuals compared to non-smokers [87]. Comparing chronic smokers and non-smokers showed a lower RPF (− 23%) in the smoking group [90], and steeper decline in RPF with age in smoking male subjects [91].
Few studies have looked at the effect of caffeine and alcohol consumption, despite their well-known diuretic effect. One study using PAH clearance found no change in RPF after consuming beer (666 mL) or water containing 2.7% alcohol [92]. Similarly, caffeine intake had no acute effect on PAH clearance when consumed in doses less than 400 mg [93, 94]. There were no reports concerning the impact of regular (chronic) consumption of alcohol, caffeine, or other recreational drugs on RBF in humans.
At present, the limited data on the potential effect on RBF, preclude restricting the acute use of nicotine, alcohol, or caffeine substances. Future studies are required to confirm these findings. Nevertheless, querying the habitual use of these substances should be considered to support the interpretation of RBF results [90].
Exercise
The renovascular adjustments to exercise training occur in response to the increased sympathetic neural outflow, resulting in blood flow being directed away from the kidneys [95]. Using PAH clearance, a substantial decline − 40% (range − 26 to − 58%) in RBF − 450 mL/min (− 279 to − 759 mL/min) was reported immediately following dynamic exercise [96,97,98,99,100]. Similar response was observed in renal perfusion of the cortex [101,102,103] and medulla [103], measured using PET [101, 102] and MRI [103], following static handgrip exercise. A return to near pre-exercise RBF value can appear 30–60 min after completion of the dynamic exercise bouts [2, 104], with full-recovery reported at 2-h post-activity [105]. In older adults, changes in RBF during exercise is lower [106, 107] and recover at slower rate [106, 108]. Studies investigating the effect of variable level of exercise training showed minimal RBF response with low exercise intensity [99, 100, 109, 110]. The degree of RBF reduction can also be related to other factors such as exercise duration [100], ambient temperature [97, 99, 107], and hydration level [111].
Difference in resting RBF measurements between sedentary and well-trained young individuals was noted in a cross-sectional study [107]. Nevertheless, no effect on RBF was found when subjects underwent a sustained exercise training program for 4 weeks [107] or 6 months [112].
The transient change in RBF post-exercise might be confounded with reduced renal function. Hence, heavy physical activity should be restricted on the day of RBF measurement.
High altitudes
Exposure to high altitude is associated with an elevation in haemoglobin concentration and a redistribution of RBF which serve to restore normal blood oxygenation as a consequence of acute hypoxia. RBF measured with PAH clearance [113,114,115] or Doppler ultrasound [116] showed a reduction of − 17% (range − 10 to − 23%) in response to short-term (1–7 days) exposure to high altitude (range 3500–6500 m). The reduction in RBF is maintained during prolonged stay (> 60 days) [115] but was not detected with shorter exposure time (6 h) using Doppler US [117]. Natives living at high altitude have also been found to have − 28% lower RBF values when compared with sea level residents [118, 119]. While the impact of altitude adaptation might be less relevant in single-centre studies, it should be considered when comparing data that involve individuals residing at high-altitude environment.
Mental activity
The renal response to acute mental stress is characterized by a rapid and transient vasoconstriction stimulated by sympathoadrenal excitation. Cortical [120] and total RBF [121,122,123] was found to decrease − 19% (range − 6 to − 33%) in response to solving stressful mental arithmetic [123] or the Stroop colour-word tests [120,121,122]. Alterations in RBF were observed at 2 min of mental stress [120] which would gradually return to baseline at 1 h [122]. The reduction in RBF can be negatively associated with the increment in systolic blood pressure during mental stress [123]. In the elderly, mental stress results on more pronounced and prolonged reduction in RBF [124]. Similar changes were noted in renal circulation following emotional stress induced by the discussion of sensitive personal topics [125]. In addition, individuals annoyed by environmental noise were found to have 10% lower RBF compared to non-noise-annoyed individuals [126].
These data support that anxiety, tenseness, and annoyance are factors that should be considered (and possibly controlled) when measuring RBF. Ensuring the participant feels comfortable before and during the scan can be achieved by thorough explanation of the procedure. Since the MRI scanner environment can be an obvious source of apprehension to some participants (i.e. claustrophobia), it is advised to record for such effects which would aid the interpretation of results. In addition, capturing information on individual’s feelings (i.e. anxiety and depression) should provide additional comparative data between subjects.
Thermal stress
Exposure to thermal stress causes a redistribution of RBF where the kidney acts to maintain internal body temperature by activating the sympathetic outflow. Reduced RBF measured with PAH clearance − 31% (range − 26 to − 38%) was reported in response to increased body temperature + 0.5 to + 2 °C following exposure to hot environment (50 °C dry bulb) [97], or passive heating induced with water-perfused suits [127,128,129]. RBF reduction was only minimal when subjects were exposed at a milder air temperature (36 °C) [99], or internal body temperature rose by 0.4 °C [99, 130]. Sustained heat exposure (i.e. heat acclimation) at 30 °C for period of 4 days had no measurable effect on baseline RBF [131]. The cooling effect provoke similar renal response. One study using ASL reported reduced renal perfusion in the cortex but not in the medulla when participant’s feet were covered with ice packs at 1 °C for 2 min [132]. This effect has similarly been observed on ultrasound measured renal blood velocity and resistance index [133,134,135]. The pattern that emerges from these studies is that changes in body temperature is associated with large RBF fluctuation. Measurement of body temperature should therefore be obtained, and the study can be delayed in case of fever.
Medication use
Extensive research has been performed to investigate the alterations of renal circulation in response to a wide range of pharmacological treatments. In this section, an emphasis will be given to the use of commonly prescribed medications that have been studied in normal human subjects.
Nonsteroidal anti-inflammatory drugs (NSAID) can inhibit prostaglandin synthesis, thereby causing important alterations in renal function. Studies on normal subjects have reported variable RBF response of selective and non-selective NSAIDs.
The oral administration of indomethacin (50 mg) was found to acutely reduce RPF − 16% (range − 10 to − 23%) measured using PAH clearance in young normotensive subjects who were maintained on sodium balance [136,137,138]. However, the short-term intake of indomethacin for period of 3–7 days resulted on preserved RPF both in young [139,140,141] and elderly subjects [142].
Under conditions of severe salt depletion, single oral dose of celecoxib (400 mg) resulted on a transient drop in RPF measured with PAH clearance within 1 h [143], but no changes were observed in the same study when a lower dose (200 mg) was used. This reduction in RPF with the higher dose of celecoxib (400 mg) was not observed in a separate study performed on subjects with minimal salt depletion [144].
A daily dose of diclofenac (50 mg) used for period of 2–3 days had no alteration in RPF measured using standard PAH clearance both in young [145] and older patients without impaired renal function [146]. Similarly, using ASL no changes in renal perfusion were detected after single oral dose (50 mg) or short-term tropical application (3 days) of diclofenac [147]. However, a significant reduction in renal perfusion was reported, in the same study, in sub-group of subjects with high plasma diclofenac level after oral intake only.
Previous studies that have investigated the effect of ibuprofen (400–800 mg) on renal circulations reported no significant changes in RPF after acute [137, 148], short-term (3 days) [141] or sustained (14 days) [149] administration in salt-replete subjects. Similarly, therapeutic doses of etodolac (300 mg) [149], paracetamol (500 mg) [140], Aspirin (975 mg) [137, 150], diflunisal (500 mg) [137], naproxen (500 mg) [143] or ketoprofen (50 mg) [139] for short-term did not affect RPF in healthy young subjects.
These data indicate that various NSAIDs have different effects on RBF in normal individuals. It can also be inferred that the changes in RBF are more pronounced during acute oral use, rather than the repeated use of NSAIDs, possibly due to counterregulatory mechanism operating in the human kidney. In addition, the specific effect of NSAIDs can be confounded by the state of sodium intake, with more pronounced effect expected during sodium-restriction [151]. Taken together, participants can be advised to avoid NSAIDs before RBF measurement, and recent use of NSAIDs should be documented.
The use of oral contraceptive pills (OCP) is known to be associated with increased RAS activity, but their impact on renal hemodynamic has been controversial. An earlier study reported reduction in renal perfusion by an average of − 25%, estimated from the disappearance curve of radioactive xenon, in normotensive women using a variety of combined oestrogen-progestogen drugs for long-term (> 6 months) [152]. Similar, though minor, differences were observed when comparing baseline RBF between OCP users (30 ± 5 µg ethynyl-oestradiol) and non-users in some [153, 154], but not all studies [155, 156] using PAH clearance. The progestational and androgenic activity in the OCP has been found to be associated with enhanced angiotensin-dependent control of the renal circulation [157]. The discontinuation of OCP for period of 6 months had no measurable effect on baseline RBF [155]. These data suggest that the regular use of OCP should be documented when measuring RBF in women.
Renin-angiotensin system (RAS) inhibitors, reduce the formation of angiotensin-II, which results on reduced systemic and renal vascular resistance and favourable renal vasodilator effect. Different classes of RAS inhibitors have been studied previously namely, angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARB) and direct renin inhibitors. In spite of differences in their mechanism of actions, the acute administration of these agents has been found to increase RBF to variable degree.
In healthy subjects, the acute administration of Captopril (25 mg) caused marked rise in RPF (range 14–24%) [148, 158] with peak values reported at 3–4 h [158]. Two ascending doses of Ramipril (2.5 mg and 10 mg) administrated on separate days resulted on similar increase in RBF, with an estimated change of 18% reported with the highest dose during 3.75–4.75 h period [159]. Treatment with Enalapril (20 mg) caused modest increase in RPF (range 10–13%) at 2–4 h [160, 161], but maximal vasodilation was noted 6 h after drug intake [160].
Studies using drugs of the ARB class showed similar renal hemodynamic effect to those using ACE inhibitor [162]. In healthy, salt depleted subjects, single oral dose of Eprosartan (200 mg) increased baseline RPF by 20% at 3.75 h post-administration [163]. In the same study, the lowest Eprosartan dose sufficient to cause significant renal vasodilation was determined to be < 10 mg, whereas the near-maximal vasodilator response was achieved with a dose of 100 mg. In similar laboratory sittings, escalating doses of Candesartan caused progressive increase in RPF with peak response (24%) achieved with a dose of 16 mg during 4 h after administration [164]. Studies using Valsartan (80 mg) [160] or Losartan (50 mg) [165] on healthy subjects showed relatively small increase in RBF (range 8–11%) during 3–4 h after acute administration.
One study looked at the effect of direct renin inhibitor, Aliskiren, and found marked dose-related renal vasodilation [166]. Under conditions of salt-depletion, a change from baseline RPF values of 16%, 22% and 30% were reported in repones to acute aliskiren doses of 75 mg, 150 mg, and 300 mg, respectively. In addition, baseline RPF remained significantly increased after each aliskiren dose when repeated measurements were performed 48 h post-drug intake [166].
Calcium channel blockers represent another class of drugs that have been associated with a preferential vasodilation effect on afferent arterioles. Normal subjects receiving two separate doses of felodipine (5 mg and 20 mg) showed major changes in RBF acutely, with maximum estimated change of 40% reported with the higher dose [159]. On the other hand, the acute use of Nifedipine (10 mg) caused minimal vasodilation in baseline RPF value [158]. This considerable variability in the renal hemodynamic effects among calcium antagonists, might be related to differences in the intrinsic actions of the agents studied.
Beta blockers suppress cardiac output and inhibit mediated vasodilation, both effects could result in reduced RBF. However, previous studies reported conflicting results which make the effect of beta blockers difficult to interpret. One study using PAH clearance showed the anticipated reduction in RBF (-11%) in the first hour following oral intake of metoprolol (100 mg) or pindolol (10 mg) in hypertensive patients with normal kidney function [167]. An opposite trend was reported in response to the same dose of metoprolol in a separate study performed on healthy volunteers. No changes in baseline RBF were reported following 10 days treatment with metoprolol (200 mg) compared to placebo [168].
In general, anti-hypertensive medications represent potent modulators of RBF. Patients with prescribed anti-hypertensive treatments (RAS inhibitors, calcium channel blockers, beta blockers) can be advised to withdraw acute use of drugs before RBF measurement where possible.
Diuretics can affect renal haemodynamics through their actions as an inhibitor of sodium-reabsorption in the ascending loop of Henle. One study, using PAH clearance, compared the effect of oral intake of four different loop diuretics on healthy volunteers and reported no alteration in RPF in response to piretanide (6 mg) or bumetanide (1 mg), whereas ethacrynic acid (100 mg) and furosemide (40 mg) induced reduction in RPF by − 23% and − 7%, respectively [169]. Variable effects have been found in response to the acute parenteral administration of furosemide in healthy volunteers. Two studies, using PAH clearance, reported transient increase in RPF in the first 20 min after furosemide (20 mg) injection [141, 170]. Other studies applying PAH clearance [171] or PC-MRI [103] reported no alteration in RBF post-furosemide injection. Regional perfusion in the cortex and medulla, estimated using ASL, have been found to decrease post-furosemide injection [172].
While the inconsistency between findings makes the net effect of loop diuretics difficult to conclude, omitting diuretic drugs in the morning before RBF measurement should be considered where possible.
Discussion
This review has evaluated the magnitude and direction of change of several influencing factors on RBF with the goal to formulate evidence-based recommendations. The results obtained from the literature support the need for a rigorous study design to enable more efficient quantification of RBF. Despite some large variability in the reported magnitude of change, the direction of change was mostly aligned between studies. It must be noted that measurement error is inevitable and constitute an additional source of variability, even if a gold-standard method was used.
Standardization is a pivotal initial phase in biomarker validation. Ongoing efforts for standardisation of renal MRI seek to establish consistent and reliable measurement protocols [8,9,10]. The work presented in this review paper supplement existing recommendations with additional evidence-based information and could promote an alignment of opinions in future revisions of the consensus. A wide range of influencing factors was found to cause changes in RBF. In the recently published technical recommendations for PC-MRI, the panel has advised against restricted diet and hydration (i.e. fasting), instead scans are recommended to be performed in the normal hydration state while avoiding salty- and protein rich meals [9]. Although there is a dispute on the acute effect of water loading, hydration is undeniably a standard procedure used in clearance studies to maintain urine flow at constant rate. At present, the provided evidence supports the relevance of normal hydration before RBF measurements. With respect to food intake, our recommendation is less clear-cut, and calls for future research in this matter.
Depending on the influencing factor, RBF can decrease by a mean of 130 mL/min or increase by 250 mL/min. Differences of this magnitude have an important clinical implication and can be confounded with disease characteristics. For instance, patients with benign hypertension show reduced RBF compared to controls subjects [173]. An effect of similar magnitude and direction can be observed post exercise or in response to heat exposure. By contrast, newly diagnosed diabetes is characterized by higher RBF than in normal subjects [174, 175]. An effect of similar pattern can be observed in response to protein meal in healthy subjects [67].
Considering the data presented in this review, we propose evidence-based recommendations to provide future researchers a means to interpret and possibly correct for the influencing factors. While the review primarily aimed at assessing RBF and perfusion, the proposed recommendation might also apply to other techniques such as renal BOLD MRI. The specific recommendations are summarized in Table 3, and include all factors, even those only minimally contributing to the variability. The physiological confounders were arranged into three separate categories in relation to the stage where they should be considered. Since it may not be feasible to control for all modifiable in clinical practice, it can be advised to acquire information using questionnaire. For instance, providing a standardized meal before conducting the exam can ensure reducing the influence of certain type of food on RBF, but may also cause financial and practical constrains. An alternative option would be to ask participants to keep a record of their last meal, which can be referred to in case of unusual measurement. While current evidence in the literature showed preserved RBF in response to acute use of caffeine, nicotine and alcoholic products, more studies would be helpful to support this conclusion. Our recommendation to withdraw acute medications was based on current preparation worked in a clinical trial [176]. However, whether this acute cessation of treatment has an impact on renal haemodynamics was not studied before. Similarly, little is known about the acute use of some novel medications, notably sodium–glucose cotransporter 2 (SGLT2) inhibitors and glucagon-like peptide 1 (GLP-1) receptor agonists. These medications have been found to contribute to improved renal outcomes [177], and more comprehensive investigation into their acute influence on RBF is needed to understand their potential implications. As a general rule, obtaining additional information regarding individual habits, and/or prescribed medications can be considered for a rigorous study design. These factors can then be used as covariates in the statistical analysis model to enable better interpretation of RBF measurement.
Limitations
One limitation of this review arises from the inclusion of studies using various techniques to measure RBF in response to each influencing factor. The unit of RBF was inconsistently reported in the literature, where normalization to BSA was used in some but not all studies. For the analysis of this review, RBF was assessed in absolute units (i.e. mL/min) as correcting to BSA is a potential confounder and therefore can obscure some of the variation between individuals of different body dimensions. It must therefore be emphasized that the magnitude of change in absolute units presented in this review should not be used to correct for such effects but rather as an estimation of the effect size. A detailed discussion of the underlying physiological mechanism affecting an individual confounding factor would enable better understanding of the reported results, but this was not the main objective of the current review.
Conclusions
The variability in RBF in response to physiological factors is an important consideration in the development of an efficient study design to assess the renal hemodynamic. In this review, the effect of several influencing factors was assessed in order to provide an evidence-based recommendation. Future studies aiming to measure RBF are encouraged to follow a rigorous study design, which takes into account the factors that can influence RBF results. In addition, some gaps in the scientific literature were highlighted that represent exciting opportunities for future exploration to expand our understanding of kidney physiology and more importantly, promote well-controlled quantitative assessment.
Data availability
Data sharing is not applicable to this review article as no new data were created or analyzed in this study.
References
Cupples WA, Braam B (2007) Assessment of renal autoregulation. Am J Physiol Renal Physiol 292:F1105–F1123
Pricher MP, Holowatz LA, Williams JT, Lockwood JM, Halliwill JR (2004) Regional hemodynamics during postexercise hypotension. I. Splanchnic and renal circulations. J Appl Physiol (1985) 97:2065–2070
Koopman MG, Koomen GCM, Krediet RT, de Moor EAM, Hoek FJ, Arisz L (1989) Circadian rhythm of glomerular filtration rate in normal individuals. Clin Sci 77:105–111
Persson PB (2002) Renal blood flow autoregulation in blood pressure control. Curr Opin Nephrol Hypertens 11:67–72
Barrett CJ, Navakatikyan MA, Malpas SC (2001) Long-term control of renal blood flow: what is the role of the renal nerves? Am J Physiol Regul Integr Comp Physiol 280:R1534–R1545
Prasad PV, Li L-P, Thacker JM, Li W, Hack B, Kohn O, Sprague SM (2019) Cortical perfusion and tubular function as evaluated by magnetic resonance imaging correlates with annual loss in renal function in moderate chronic kidney disease. Am J Nephrol 49:114–124
Hockings P, Saeed N, Simms R, Smith N, Hall MG, Waterton JC, Sourbron S (2020) MRI biomarkers. In: Seiberlich N, Gulani V, Calamante F, Campbell-Washburn A, Doneva M, Hu HH, Sourbron S (eds) Quant magn reson imag, 1st edn. Elsevier Academic Press, London, p Iiii–Ixxxvi
Nery F, Buchanan CE, Harteveld AA, Odudu A, Bane O, Cox EF, Derlin K, Gach HM, Golay X, Gutberlet M, Laustsen C, Ljimani A, Madhuranthakam AJ, Pedrosa I, Prasad PV, Robson PM, Sharma K, Sourbron S, Taso M, Thomas DL, Wang DJJ, Zhang JL, Alsop DC, Fain SB, Francis ST, Fernández-Seara MA (2020) Consensus-based technical recommendations for clinical translation of renal ASL MRI. MAGMA 33:141–161
de Boer A, Villa G, Bane O, Bock M, Cox EF, Dekkers IA, Eckerbom P, Fernández-Seara MA, Francis ST, Haddock B, Hall ME, Hall Barrientos P, Hermann I, Hockings PD, Lamb HJ, Laustsen C, Lim RP, Morris DM, Ringgaard S, Serai SD, Sharma K, Sourbron S, Takehara Y, Wentland AL, Wolf M, Zöllner FG, Nery F, Caroli A (2020) Consensus-based technical recommendations for clinical translation of renal phase contrast MRI. J Magn Reson Imaging 55:323–335
Bane O, Mendichovszky IA, Milani B, Dekkers IA, Deux J-F, Eckerbom P, Grenier N, Hall ME, Inoue T, Laustsen C (2020) Consensus-based technical recommendations for clinical translation of renal BOLD MRI. MAGMA 33:199–215
Miao G, Qingsheng Y, Zhiyuan R, Hongxian Z, Yanfang Z, Shuyan Y (2002) Reference value of presenile human hematocrit and geographical factors. J Clin Lab Anal 16:26–29
Baba M, Shimbo T, Horio M, Ando M, Yasuda Y, Komatsu Y, Masuda K, Matsuo S, Maruyama S (2015) Longitudinal study of the decline in renal function in healthy subjects. PLoS ONE 10:e0129036
Davies DF, Shock N (1950) Age changes in glomerular filtration rate, effective renal plasma flow, and tubular excretory capacity in adult males. J Clin Invest 29:496–507
Olbrich O, Ferguson MH, Robson JS, Stewart CP (1950) Renal functions in aged subjects. Edinb Med J 57:117
Hoang K, Tan JC, Derby G, Blouch KL, Masek M, Ma I, Lemley KV, Myers BD (2003) Determinants of glomerular hypofiltration in aging humans. Kidney Int 64:1417–1424
Czarkowska-Paczek B, Wyczalkowska-Tomasik A, Paczek L (2018) Laboratory blood test results beyond normal ranges could not be attributed to healthy aging. Medicine 97:e11414
Bäck SE, Ljungberg B, Nilsson-Ehle I, Borgå O, Nilsson-Ehle P (1989) Age dependence of renal function: clearance of iohexol and p-amino hippurate in healthy males. Scand J Clin Lab Invest 49:641–646
Lin W-Y, Changlai S-P, Kao C-H (1998) Normal ranges of renal physiological parameters for technetium-99m mercaptoacetyltriglycine and the influence of age and sex using a camera-based method. Urol Int 60:11–16
Bax L, Bakker CJG, Klein WM, Blanken N, Beutler JJ, Mali WPTRM (2005) Renal blood flow measurements with use of phase-contrast magnetic resonance imaging: normal values and reproducibility. J Vasc Interv Radiol 16:807–814
Cox EF, Buchanan CE, Bradley CR, Prestwich B, Mahmoud H, Taal M, Selby NM, Francis ST (2017) Multiparametric renal magnetic resonance imaging: validation, interventions, and alterations in chronic kidney disease. Front Physiol 8:696
Dujardin M, Sourbron S, Luypaert R, Verbeelen D, Stadnik T (2005) Quantification of renal perfusion and function on a voxel-by-voxel basis: a feasibility study. Magn Reson Med 54:841–849
Shimizu K, Kosaka N, Fujiwara Y, Matsuda T, Yamamoto T, Tsuchida T, Tsuchiyama K, Oyama N, Kimura H (2017) Arterial transit time-corrected renal blood flow measurement with pulsed continuous arterial spin labeling MR imaging. Magn Reson Med Sci 16:38–44
Berg UB (2006) Differences in decline in GFR with age between males and females. Reference data on clearances of inulin and PAH in potential kidney donors. Nephrol Dialy Transplant 21:2577–2582
Toering TJ, Van Der Graaf AM, Visser FW, Buikema H, Navis G, Faas MM, Lely AT (2015) Gender differences in response to acute and chronic angiotensin II infusion: a translational approach. Physiol Rep 3:e12434
Eckerbom P, Hansell P, Cox E, Buchanan C, Weis J, Palm F, Francis S, Liss P (2019) Multiparametric assessment of renal physiology in healthy volunteers using noninvasive magnetic resonance imaging. Am J Physiol Renal Physiol 316:F693–F702
Miller JA, Anacta LA, Cattran DC (1999) Impact of gender on the renal response to angiotensin II. Kidney Int 55:278–285
Kalucki SA, Lardi C, Garessus J, Kfoury A, Grabherr S, Burnier M, Pruijm M (2020) Reference values and sex differences in absolute and relative kidney size. A Swiss autopsy study. BMC Nephrol 21:289
Levey AS, Tighiouart H, Titan SM, Inker LA (2020) Estimation of glomerular filtration rate with vs. without including patient race. JAMA Intern Med 180:793–795
Delgado C, Baweja M, Burrows NR, Crews DC, Eneanya ND, Gadegbeku CA, Inker LA, Mendu ML, Miller WG, Moxey-Mims MM, Roberts GV, St. Peter WL, Warfield C, Powe NR (2021) Reassessing the inclusion of race in diagnosing kidney diseases: an interim report from the NKF-ASN task force. J Am Soc Nephrol 32:1305 LP – 1317
Price DA, Fisher ND, Osei SY, Lansang MC, Hollenberg NK (2001) Renal perfusion and function in healthy African Americans. Kidney Int 59:1037–1043
Price DA, Fisher NDL, Lansang MC, Stevanovic R, Williams GH, Hollenberg NK (2002) Renal perfusion in blacks: alterations caused by insuppressibility of intrarenal renin with salt. Hypertension 40:186–189
Forman JP, Price DA, Stevanovic R, Fisher ND (2007) Racial differences in renal vascular response to angiotensin blockade with captopril or candesartan. J Hypertens 25:877–882
Bochud M, Eap CB, Maillard M, Johnson T, Vollenweider P, Bovet P, Elston RC, Bergmann S, Beckmann JS, Waterworth DM, Mooser V, Gabriel A, Burnier M (2008) Association of ABCB1 genetic variants with renal function in Africans and in Caucasians. BMC Med Genomics 1:21
Ribstein J, du Cailar G, Mimran A (1995) Combined renal effects of overweight and hypertension. Hypertension 26:610–615
Chagnac A, Weinstein T, Korzets A, Ramadan E, Hirsch J, Gafter U (2000) Glomerular hemodynamics in severe obesity. Am J Physiol Renal Physiol 278:F817–F822
Wuerzner G, Pruijm M, Maillard M, Bovet P, Renaud C, Burnier M, Bochud M (2010) Marked association between obesity and glomerular hyperfiltration: a cross-sectional study in an African population. Am J Kidney Dis 56:303–312
Bosma RJ, van der Heide JJH, Oosterop EJ, de Jong PE, Navis G (2004) Body mass index is associated with altered renal hemodynamics in non-obese healthy subjects. Kidney Int 65:259–265
Kwakernaak AJ, Zelle DM, Bakker SJL, Navis G (2013) Central body fat distribution associates with unfavorable renal hemodynamics independent of body mass index. J Am Soc Nephrol 24:987–994
Chagnac A, Weinstein T, Herman M, Hirsh J, Gafter U, Ori Y (2003) The effects of weight loss on renal function in patients with severe obesity. J Amer Soc Nephrol 14:1480–1486
Rebelos E, Dadson P, Oikonen V, Iida H, Hannukainen JC, Iozzo P, Ferrannini E, Nuutila P (2019) Renal hemodynamics and fatty acid uptake: effects of obesity and weight loss. Amer J Physiol Endo Metabol 317:E871–E878
Anastasio P, Spitali L, Frangiosa A, Molino D, Stellato D, Cirillo E, Pollastro RM, Capodicasa L, Sepe J, Federico P, Gaspare De Santo N (2000) Glomerular filtration rate in severely overweight normotensive humans. Am J Kidney Dis 35:1144–1148
Schmieder RE, Beil AH, Weihprecht H, Messerli FH (1995) How should renal hemodynamic data be indexed in obesity? J Am Soc Nephrol 5:1709–1713
Chapman AB, Abraham WT, Zamudio S, Coffin C, Merouani A, Young D, Johnson A, Osorio F, Goldberg C, Moore LG (1998) Temporal relationships between hormonal and hemodynamic changes in early human pregnancy. Kidney Int 54:2056–2063
Sims EAH, Krantz KE (1958) Serial studies of renal function during pregnancy and the puerperium in normal women. J Clin Invest 37:1764–1774
Dunlop W (1981) Serial changes in renal haemodynamics during normal human pregnancy. BJOG 88:1–9
de Alvarez RR (1958) Renal glomerulotubular mechanisms during normal pregnancy: I. Glomerular filtration rate, renal plasma flow, and creatinine clearance. Am J Obstet Gynecol 75:931–944
Roberts M, Lindheimer MD, Davison JM (1996) Altered glomerular permselectivity to neutral dextrans and heteroporous membrane modeling in human pregnancy. Am J Physiol 270:F338–F343
Brøchner-Mortensen J, Paaby P, Fjeldborg P, Raffn K, Larsen CE, Møller-Petersen J (1987) Renal haemodynamics and extracellular homeostasis during the menstrual cycle. Scand J Clin Lab Invest 47:829–835
Chapman AB, Zamudio S, Woodmansee W, Merouani A, Osorio F, Johnson A, Moore LG, Dahms T, Coffin C, Abraham WT, Schrier RW (1997) Systemic and renal hemodynamic changes in the luteal phase of the menstrual cycle mimic early pregnancy. Am J Physiol 273:F777–F782
van Beek E, Houben A, van Es P, Willekes C, Korten E, de Leeuw PD, Peeters L (1996) Peripheral haemodynamics and renal function in relation to the menstrual cycle. Clin Sci 91(2):163–168
Chidambaram M, Duncan JA, Lai VS, Cattran DC, Floras JS, Scholey JW, Miller JA (2002) Variation in the renin angiotensin system throughout the normal menstrual cycle. J Amr Soc Nephrol 13:446–452
Koopman MG, Koomen GC, van Acker BA, Arisz L (1994) Urinary sodium excretion in patients with nephrotic syndrome, and its circadian variation. Q J Med 87:109–117
Wesson LGJ (1964) Electrolyte excretion in relation to diurnal cycles of renal function. Medicine 43:547–592
Wesson LGJ, Lauler DP (1961) Diurnal cycle of glomerular filtration rate and sodium and chloride excretion during responses to altered salt and water balance in man. J Clin Invest 40:1967–1977
Voogel AJ, Koopman MG, Hart AA, van Montfrans GA, Arisz L (2001) Circadian rhythms in systemic hemodynamics and renal function in healthy subjects and patients with nephrotic syndrome. Kidney Int 59:1873–1880
Eckerbom P, Hansell P, Cox E, Buchanan C, Weis J, Palm F, Francis S, Liss P (2020) Circadian variation in renal blood flow and kidney function in healthy volunteers monitored with noninvasive magnetic resonance imaging. Am J Physiol Renal Physiol 319:F966–F978
Sirota JH, Baldwin DS, Villarreal H (1950) Diurnal variations of renal function in man. J Clin Invest 29:187–192
Steinmetz PR, Eisinger RP (1966) Influence of posture and diurnal rhythm on the renal excretion of acid: observations in normal and adrenalectomized subjects. Metabolism 15:76–87
Hauser JA, Muthurangu V, Steeden JA, Taylor AM, Jones A (2016) Comprehensive assessment of the global and regional vascular responses to food ingestion in humans using novel rapid MRI. Am J Physiol Regul Integr Comp Physiol 310:R541–R545
Muller AF, Fullwood L, Hawkins M, Cowley AJ (1992) The integrated response of the cardiovascular system to food. Digestion 52:184–193
Avasthi PS, Greene ER, Voyles WF (1987) Noninvasive Doppler assessment of human postprandial renal blood flow and cardiac output. Amer J Physiol Renal Physiol 252:F1167–F1174
Bosch JP, Lew S, Glabman S, Lauer A (1986) Renal hemodynamic changes in humans: response to protein loading in normal and diseased kidneys. Am J Med 81:809–815
Hostetter TH (1986) Human renal response to meat meal. Am J Physiol 250:F613–F618
Swainson CP, Walker RJ (1989) Renal haemodynamic and hormonal responses to a mixed high-protein meal in normal men. Nephrol Dial Transpl 4:683–690
Braendle E, Kindler J, Sieberth HG (1990) Effects of an acute protein load in comparison to an acute load of essential amino acids on glomerular filtration rate, renal plasma flow, urinary albumin excretion and nitrogen excretion. Nephrol Dial Transpl 5:572–578
Krishna GG, Newell G, Miller E, Heeger P, Smith R, Polansky M, Kapoor S, Hoeldtke R (1988) Protein-induced glomerular hyperfiltration: role of hormonal factors. Kidney Int 33:578–583
Simon AH, Lima PR, Almerinda M, Alves VF, Bottini PV, de Faria JB (1998) Renal haemodynamic responses to a chicken or beef meal in normal individuals. Nephrol Dial Transpl 13:2261–2264
Rodríguez-Iturbe B, Herrera J, García R (1988) Relationship between glomerular filtration rate and renal blood flow at different levels of protein-induced hyperfiltration in man. Clin Sci 74:11–15
Kontessis P, Jones S, Dodds R, Trevisan R, Nosadini R, Fioretto P, Borsato M, Sacerdoti D, Viberti G (1990) Renal, metabolic and hormonal responses to ingestion of animal and vegetable proteins. Kidney Int 38:136–144
Deibert P, Lutz L, Konig D, Zitta S, Meinitzer A, Vitolins MZ, Becker G, Berg A (2011) Acute effect of a soy protein-rich meal-replacement application on renal parameters in patients with the metabolic syndrome. Asia Pac J Clin Nutr 20:527–534
ten Dam M, van Kamp GJ, Kok A, Meuwissen SGM, Donker AJM, ten Kate RW (1991) The effect of acute and chronic protein loading on urinary pepsinogen A excretion. Nephron 59:239–243
Viberti G, Bognetti E, Wiseman MJ, Dodds R, Gross JL, Keen H (1987) Effect of protein-restricted diet on renal response to a meat meal in humans. Am J Physiol Renal Physiol 253:F388–F393
Fancourt GJ, Asokan VS, Bennett SC, Walls J, Castleden CM (1992) The effects of dopamine and a low protein diet on glomerular filtration rate and renal plasma flow in the aged kidney. Eur J Clin Pharmacol 42:375–378
Kitazato H, Fujita H, Shimotomai T, Kagaya E, Narita T, Kakei M, Ito S (2002) Effects of chronic intake of vegetable protein added to animal or fish protein on renal hemodynamics. Nephron 90:31–36
Hollenberg NK, Chenitz WR, Adams DF, Williams GH (1974) Reciprocal influence of salt intake on adrenal glomerulosa and renal vascular responses to angiotensin II in normal man. J Clin Invest 54:34–42
Luik PT, Hoogenberg K, Van Der Kleij FGH, Beusekamp BJ, Kerstens MN, De Jong PE, Dullaart RPF, Navis GJ (2002) Short-term moderate sodium restriction induces relative hyperfiltration in normotensive normoalbuminuric Type I diabetes mellitus. Diabetologia 45:535–541
Pruijm M, Hofmann L, Maillard M, Tremblay S, Glatz N, Wuerzner G, Burnier M, Vogt B (2010) Effect of sodium loading/depletion on renal oxygenation in young normotensive and hypertensive men. Hypertension 55:1116–1122
Burnier M, Rutschmann B, Nussberger J, Versaggi J, Shahinfar S, Waeber B, Brunner HR (1993) Salt-dependent renal effects of an angiotensin II antagonist in healthy subjects. Hypertension 22:339–347
Miller JA (1997) Renal responses to sodium restriction in patients with early diabetes mellitus. J Am Soc Nephrol 8:749–755
Burnier M, Pechère-Bertschi A, Nussberger J, Waeber B, Brunner HR (1995) Studies of the renal effects of angiotensin II receptor blockade: the confounding factor of acute water loading on the action of vasoactive systems. Am J Kidney Dis 26:108–115
Anastasio P, Cirillo M, Spitali L, Frangiosa A, Pollastro RM, De Santo NG (2001) Level of hydration and renal function in healthy humans. Kidney Int 60:748–756
Alhummiany BA, Shelley D, Saysell M, Olaru M, Kühn B, Buckley DL, Bailey J, Wroe K, Coupland C, Mansfield MW (2022) Bias and precision in magnetic resonance imaging-based estimates of renal blood flow: assessment by triangulation. J Magn Reson Imag 55:1241–1250
Thelwall PE, Taylor R, Marshall SM (2011) Non-invasive investigation of kidney disease in type 1 diabetes by magnetic resonance imaging. Diabetologia 54:2421–2429
Li L-P, Tan H, Thacker JM, Li W, Zhou Y, Kohn O, Sprague SM, Prasad PV (2017) Evaluation of renal blood flow in chronic kidney disease using arterial spin labeling perfusion magnetic resonance imaging. Kidney Int Rep 2:36–43
Boer WH, Koomans HA, Dorhout Mees EJ (1988) Renal lithium handling during water loading and subsequent d-DAVP-induced anti-diuresis. Eur J Clin Invest 18:273–278
Razzak MA, Botti RE, MacIntyre WJ (1969) Interrelationship between hydration, urine flow, renal blood flow and the radiohippuran renogram. J Nuc Med 10:672–675
Halimi JM, Philippon C, Mimran A (1998) Contrasting renal effects of nicotine in smokers and non-smokers. Nephrol Dial Transpl 13:940–944
Halimi JM, Mimran A (2000) Systemic and renal effect of nicotine in non-smokers: influence of vitamin C. J Hypertens 18:1665–1669
Ritz E, Benck U, Franek E, Keller C, Seyfarth M, Clorius J (1998) Effects of smoking on renal hemodynamics in healthy volunteers and in patients with glomerular disease. J Am Soc Nephrol 9:1798–1804
Gambaro G, Verlato F, Budakovic A, Casara D, Saladini G, Del Prete D, Bertaglia G, Masiero M, Checchetto S, Baggio B (1998) Renal impairment in chronic cigarette smokers. J Am Soc Nephrol 9:562–567
Guberina H, Baumann M, Bruck H, Feldkamp T, Nürnberger J, Kribben A, Philipp T, Witzke O, Sotiropoulos G, Mitchell A (2013) Associations of smoking with alterations in renal hemodynamics may depend on sex-investigations in potential kidney donors. Kidney Blood Press Res 37:611–621
Jan EK, Josephson B (1953) On the influence of beer and a purine derivative on the renal clearance of creatinine, inulin and pnrn-amino-hippuric acid (PAH). Acta Physiol Scand 28:347–354
Passmore AP, Kondowe GB, Johnston GD (1987) Renal and cardiovascular effects of caffeine: a dose–response study. Clin Sci 72:749–756
Shirley DG, Walter SJ, Noormohamed FH (2002) Natriuretic effect of caffeine: assessment of segmental sodium reabsorption in humans. Clin Sci 103:461–466
Drew RC (2017) Baroreflex and neurovascular responses to skeletal muscle mechanoreflex activation in humans: an exercise in integrative physiology. Am J Physiol Regul Integr Compar Physiol 313:R654–R659
Aas K, Blegen E (1949) The renal blood flow and the glomerular filtration rate in congestive heart failure and some other clinical conditions. Scand J Clin Lab Invest 1:22–32
Radigan LR, Robinson S (1949) Effects of environmental heat stress and exercise on renal blood flow and filtration rate. J Appl Physiol 2:185–191
Haywood GA, Counihan PJ, Sneddon JF, Jennison SH, Bashir Y, McKenna WJ (1993) Increased renal and forearm vasoconstriction in response to exercise after heart transplantation. Br Heart J 70:247 LP – 251
Kenney W, Ho C (1995) Age alters regional distribution of blood flow during moderate-intensity exercise. J Appl Physiol 79:1112–1119
Chapman CB, Henschel A, Minckler J, Forsgren A, Keys A (1948) The effect of exercise on renal plasma flow in normal male subjects. J Clin Invest 27:639–644
Middlekauff HR, Nitzsche EU, Nguyen AH, Hoh CK, Gibbs GG (1997) Modulation of renal cortical blood flow during static exercise in humans. Circ Res 80:62–68
Middlekauff HR, Nitzsche EU, Hoh CK, Hamilton MA, Fonarow GC, Hage A, Moriguchi JD (2000) Exaggerated renal vasoconstriction during exercise in heart failure patients. Circulation 101:784–789
Haddock BT, Francis ST, Larsson HBW, Andersen UB (2018) Assessment of perfusion and oxygenation of the human renal cortex and medulla by quantitative MRI during handgrip exercise. J Am Soc Nephrol 29:2510–2517
Suzuki M, Sudoh M, Matsubara S, Kawakami K, Shiota M, Ikawa S (1996) Changes in renal blood flow measured by radionuclide angiography following exhausting exercise in humans. Eur J Appl Physiol Occup Physiol 74:1–7
Baker J, Cotter JD, Gerrard DF, Bell ML, Walker RJ (2005) Effects of indomethacin and celecoxib on renal function in athletes. Med Sci Sports Exerc 37:712–717
Kenney WL, Zappe DH (1994) Effect of age on renal blood flow during exercise. Aging Clin Exp Res 6:293–302
Ho CW, Beard JL, Farrell PA, Minson CT, Kenney WL (1997) Age, fitness, and regional blood flow during exercise in the heat. J Appl Physiol 82:1126–1135
Farquhar WB, Kenney WL (1999) Age and renal prostaglandin inhibition during exercise and heat stress. J Appl Physiol (1985) 86:1936–1943
Kawakami S, Yasuno T, Matsuda T, Fujimi K, Ito A, Yoshimura S, Uehara Y, Tanaka H, Saito T, Higaki Y (2018) Association between exercise intensity and renal blood flow evaluated using ultrasound echo. Clin Exp Nephrol 22:1061–1068
Bucht H, Ek J, Eliasch H, Holmgren A, Josephson B, Werkö L (1953) The effect of exercise in the recumbent position on the renal circulation and sodium excretion in normal individuals. Acta Physiol Scand 28:95–100
Nagashima K, Wu JC, Kavouras SA, Mack GW (2001) Increased renal tubular sodium reabsorption during exercise-induced hypervolemia in humans. J Appl Physiol 91:1229–1236
Dengel DR, Brown MD, Reynolds TH, Supiano MA (2006) Effect of aerobic exercise training on renal responses to sodium in hypertensives. Med Sci Sports Exerc 38:217–222
Olsen NV, Hansen JM, Kanstrup IL, Richalet JP, Leyssac PP (1993) Renal hemodynamics, tubular function, and response to low-dose dopamine during acute hypoxia in humans. J Appl Physiol 74:2166–2173
Richalet JP, Souberbielle JC, Antezana AM, Dechaux M, Le Trong JL, Bienvenu A, Daniel F, Blanchot C, Zittoun J (1994) Control of erythropoiesis in humans during prolonged exposure to the altitude of 6542 m. Am J Physiol Regul Integr Compar Physiol 266:R756–R764
Singh MV, Salhan AK, Rawal SB, Tyagi AK, Kumar N, Verma SS, Selvamurthy W (2003) Blood gases, hematology, and renal blood flow during prolonged mountain sojourns at 3500 and 5800 m. Aviat Space Environ Med 74:533–536
Steele AR, Tymko MM, Meah VL, Simpson LL, Gasho C, Dawkins TG, Villafuerte FC, Ainslie PN, Stembridge M, Moore JP, Steinback CD (2020) Global REACH 2018: renal oxygen delivery is maintained during early acclimatization to 4330 m. Am J Physiol Renal Physiol 319:F1081–F1089
Ge R-L, Witkowski S, Zhang Y, Alfrey C, Sivieri M, Karlsen T, Resaland GK, Harber M, Stray-Gundersen J, Levine BD (2002) Determinants of erythropoietin release in response to short-term hypobaric hypoxia. J Appl Physiol 92:2361–2367
Lozano R, Monge CC (1965) Renal function in high-altitude natives and in natives with chronic mountain sickness. J Appl Physiol 20:1026–1027
Anand IS, Chandrashekhar Y, Rao SK, Malhotra RM, Ferrari R, Chandana J, Ramesh B, Shetty KJ, Boparai MS (1993) Body fluid compartments, renal blood flow, and hormones at 6000 m in normal subjects. J Appl Physiol 74:1234–1239
Middlekauff HR, Nguyen AH, Negrao CE, Nitzsche EU, Hoh CK, Natterson BA, Hamilton MA, Fonarow GC, Hage A, Moriguchi JD (1997) Impact of acute mental stress on sympathetic nerve activity and regional blood flow in advanced heart failure: implications for “triggering” adverse cardiac events. Circulation 96:1835–1842
Tidgren B, Hjemdahl P (1989) Renal responses to mental stress and epinephrine in humans. Am J Physiol 257:F682–F689
Castellani S, Ungar A, La Cava G, Cantini C, Stefanile C, Camaiti A, Messeri G, Coppo M, Vallotti B, Di Serio C, Brocchi A, Masotti G (1997) Renal adaptation to stress: a possible role of endothelin release and prostaglandin modulation in the human subject. J Lab Clin Med 129:462–469
Schmieder RE, Rüddel H, Schächinger H, Bruns J, Schulte W (1993) Renal hemodynamics and cardiovascular reactivity in the prehypertensive stage. Behav Med (Washington) 19:5–12
Castellani S, Ungar A, Cantini C, La Cava G, Di Serio C, Altobelli A, Vallotti B, Pellegri M, Brocchi A, Camaiti A, Coppo M, Meldolesi U, Messeri G, Masotti G (1998) Excessive vasoconstriction after stress by the aging kidney: inadequate prostaglandin modulation of increased endothelin activity. J Lab Clin Med 132:186–194
Pfeiffer JBJ, Wolff HG, Winter OS (1950) Studies in renal circulation during periods of life stress and accompanying emotional reactions in subjects with and without essential hypertension; observations on the role of neural activity in regulation of renal blood flow. J Clin Invest 29:1227–1242
Kannenkeril D, Jung S, Ott C, Striepe K, Kolwelter J, Schmieder RE, Bosch A (2021) Association of noise annoyance with measured renal hemodynamic changes. Kidney Blood Press Res 46:323–330
Minson CT, Wladkowski SL, Pawelczyk JA, Kenney WL (1999) Age, splanchnic vasoconstriction, and heat stress during tilting. Am J Physiol 276:R203–R212
Minson CT, Wladkowski SL, Cardell AF, Pawelczyk JA, Kenney WL (1998) Age alters the cardiovascular response to direct passive heating. J Appl Physiol (1985) 84:1323–1332
Rowell LB, Brengelmann GL, Blackmon JR, Murray JA (1970) Redistribution of blood flow during sustained high skin temperature in resting man. J Appl Physiol 28:415–420
Smith JH, Robinson S, Pearcy M (1952) Renal responses to exercise, heat and dehydration. J Appl Physiol 4:659–665
Zappe DH, Bell GW, Swartzentruber H, Wideman RF, Kenney WL (1996) Age and regulation of fluid and electrolyte balance during repeated exercise sessions. Am J Physiol 270:R71–R79
Kannenkeril D, Janka R, Bosch A, Jung S, Kolwelter J, Striepe K, Ott C, Martirosian P, Schiffer M, Uder M, Schmieder RE (2021) Detection of changes in renal blood flow using arterial spin labeling MRI. Am J Nephrol 52:69–75
Schlader ZJ, Chapman CL, Benati JM, Gideon EA, Vargas NT, Lema PC, Johnson BD (2019) Renal hemodynamics during sympathetic activation following aerobic and anaerobic exercise. Front Physiol 9:1928
Patel HM, Mast JL, Sinoway LI, Muller MD (2013) Effect of healthy aging on renal vascular responses to local cooling and apnea. J Appl Physiol 115:90–96
Wilson TE, Sauder CL, Kearney ML, Kuipers NT, Leuenberger UA, Monahan KD, Ray CA (2007) Skin-surface cooling elicits peripheral and visceral vasoconstriction in humans. J Appl Physiol 103:1257–1262
Toto RD, AdamsHuet B, Fenves AZ, Mitchell HC, Mulcahy W, Smith RD (1996) Effect of ramipril on blood pressure and protein excretion rate in normotensive nondiabetic patients with proteinuria. Am J Kidney Dis 28:832–840
Bergamo RR, Cominelli F, Kopple JD, Zipser RD (1989) Comparative acute effects of aspirin, diflunisal, ibuprofen and indomethacin on renal function in healthy man. Am J Nephrol 9:460–463
Nielsen CB, Sørensen SS, Pedersen EB (1994) Effects of indomethacin on renal function in normotensive patients with chronic glomerulonephritis with preserved renal function. Scand J Clin Lab Invest 54:523–529
Toto RD, Anderson SA, Brown-Cartwright D, Kokko JP, Brater DC (1986) Effects of acute and chronic dosing of NSAIDs in patients with renal insufficiency. Kidney Int 30:760–768
Prescott LF, Mattison P, Menzies DG, Manson LM (1990) The comparative effects of paracetamol and indomethacin on renal function in healthy female volunteers. Br J Clin Pharmacol 29:403–412
Passmore AP, Copeland S, Johnston GD (1989) A comparison of the effects of ibuprofen and indomethacin upon renal haemodynamics and electrolyte excretion in the presence and absence of frusemide. Br J Clin Pharmacol 27:483–490
Asokan A, Fancourt GJ, Bennett SE, Castleden CM (1992) Renal prostaglandins, effective renal plasma flow and glomerular filtration rate in healthy elderly subjects. Age Ageing 21:39–42
Rossat J, Maillard M, Nussberger J, Brunner HR, Burnier M (1999) Renal effects of selective cyclooxygenase-2 inhibition in normotensive salt-depleted subjects. Clin Pharmacol Ther 66:76–84
Kistler T, Ambühl PM (2001) Renal safety of combined cyclooxygenase 2 (COX-2) inhibitor and angiotensin II receptor blocker administration in mild volume depletion. Swiss Med Wkly 131:193–198
Farker K, Nassr N, Huck F, Zerle G, Rosenkranz B, Schmieder G, Hoffmann A (1995) Dipyrone and diclofenac do not influence creatinine-clearance, inulin-clearance or PAH-clearance in healthy male volunteers. Int J Clin Pharmacol Ther 33:125–130
Farker K, Merkel U, Schweer H, Haerting J, Madani SF, Eggers R, Muller UA, Seyberth HW, Hoffmann A (2002) Effects of short-term treatment with diclofenac–colestyramine on renal function and urinary prostanoid excretion in patients with type-2 diabetes. Eur J Clin Pharmacol 58:85–91
Hellms S, Gueler F, Gutberlet M, Schebb NH, Rund K, Kielstein JT, VoChieu V, Rauhut S, Greite R, Martirosian P, Haller H, Wacker F, Derlin K (2019) Single-dose diclofenac in healthy volunteers can cause decrease in renal perfusion measured by functional magnetic resonance imaging. J Pharm Pharmacol 71:1262–1270
Allon M, Pasque CB, Rodriguez M (1990) Interaction of captopril and ibuprofen on glomerular and tubular function in humans. Am J Physiol Renal Physiol 259:F233–F238
Svendsen KB, Bech JN, Sorensen TB, Pedersen EB (2000) A comparison of the effects of etodolac and ibuprofen on renal haemodynamics, tubular function, renin, vasopressin and urinary excretion of albumin and alpha-glutathione-S-transferase in healthy subjects: a placebo-controlled cross-over study. Eur J Clin Pharmacol 56:383–388
Muther RS, Potter DM, Bennett WM (1981) Aspirin-induced depression of glomerular filtration rate in normal humans: role of sodium balance. Ann Intern Med 94:317–321
Kramer HJ, Stinnesbeck B, Klautke G, Kipnowski J, Klingmueller D, Glaenzer K, Duesing R (1985) Interaction of renal prostaglandins with the renin-angiotensin and renal adrenergic nervous systems in healthy subjects during dietary changes in sodium intake. Clin Sci 68:387–393
Hollenberg NK, Williams GH, Burger B, Chenitz W, Hoosmand I, Adams DF (1976) Renal blood flow and its response to angiotensin II. An interaction between oral contraceptive agents, sodium intake, and the renin-angiotensin system in healthy young women. Circ Res 38:35–40
Cherney DZI, Scholey JW, Cattran DC, Kang AK, Zimpelmann J, Kennedy C, Lai V, Burns KD, Miller JA (2007) The effect of oral contraceptives on the nitric oxide system and renal function. Am J Physiol Renal Physiol 293:F1539–F1544
Kang AK, Duncan JA, Cattran DC, Floras JS, Lai V, Scholey JW, Miller JA (2001) Effect of oral contraceptives on the renin angiotensin system and renal function. Am J Physiol Regul Integr Compar Physiol 280:R807–R813
Ribstein J, Halimi JM, du Cailar G, Mimran A (1999) Renal characteristics and effect of angiotensin suppression in oral contraceptive users. Hypertension 33:90–95
Ahmed SB, Hovind P, Parving H-H, Rossing P, Price DA, Laffel LM, Lansang MC, Stevanovic R, Fisher NDL, Hollenberg NK (2005) Oral contraceptives, angiotensin-dependent renal vasoconstriction, and risk of diabetic nephropathy. Diabetes Care 28:1988–1994
Sarna MA, Hollenberg NK, Seely EW, Ahmed SB (2009) Oral contraceptive progestins and angiotensin-dependent control of the renal circulation in humans. J Hum Hypertens 23:407–414
Böhler J, Becker A, Reetze-Bonorden P, Woitas R, Keller E, Schollmeyer P (1993) Effect of antihypertensive drugs on glomerular hyperfiltration and renal haemodynamics. Comparison of captopril with nifedipine, metoprolol and celiprolol. Eur J Clin Pharmacol 44(Suppl 1):S57-61
Hasselgren B, Edgar B, Johnsson G, Rönn O (1993) The acute haemodynamic and renal effects of oral felodipine and ramipril in healthy subjects. Eur J Clin Pharmacol 45:327–332
Fricker AF, Nussberger J, Meilenbrock S, Brunner HR, Burnier M (1998) Effect of indomethacin on the renal response to angiotensin II receptor blockade in healthy subjects. Kidney Int 54:2089–2097
Vos PF, Boer P, Koomans HA (1993) Effects of enalapril on renal sodium handling in healthy subjects on low, intermediate, and high sodium intake. J Cardiovasc Pharmacol 22:27–32
Lansang MC, Price DA, Laffel LMB, Osei SY, Fisher NDL, Erani D, Hollenberg NK (2001) Renal vascular responses to captopril and to candesartan in patients with type 1 diabetes mellitus. Kidney Int 59:1432–1438
Price DA, DeOliveira JM, Fisher NDL, Hollenberg NK (1997) Renal hemodynamic response to an angiotensin II antagonist, eprosartan, in healthy men. Hypertension 30:240–246
Lansang MC, Osei SY, Price DA, Fisher NDL, Hollenberg NK (2000) Renal hemodynamic and hormonal responses to the angiotensin II antagonist candesartan. Hypertension 36:834–838
Duranteau J, Pussard E, Berdeaux A, Giudicelli JF (1995) Effects of the angiotensin type I receptor antagonist, losartan, on systemic and regional vascular responses to lower body negative pressure in healthy volunteers. Br J Clin Pharmacol 40:431–438
Fisher NDL, Danser AHJ, Nussberger J, Dole WP, Hollenberg NK (2008) Renal and hormonal responses to direct renin inhibition with aliskiren in healthy humans. Circulation 117:3199–3205
Koch G, Fransson L, Karlegärd L, Kothari P (1989) Responses of glomerular filtration, renal blood flow and salt-water handling to acute cardioselective and non-selective β-adrenoceptor blockade in essential hypertension. Eur J Clin Pharmacol 36:343–345
Wuerzner G, Chiolero A, Maillard M, Nussberger J, Burnier M (2005) Metoprolol prevents sodium retention induced by lower body negative pressure in healthy men. Kidney Int 68:688–694
McNabb WR, Noormohamed FH, Brooks BA, Lant AF (1984) Renal actions of piretanide and three other “loop” diuretics. Clin Pharmacol Ther 35:328–337
Passmore AP, Copeland S, Johnston GD (1990) The effects of ibuprofen and indomethacin on renal function in the presence and absence of frusemide in healthy volunteers on a restricted sodium diet. Br J Clin Pharmacol 29:311–319
Freudenthaler S, Benohr P, Grenz A, Selzer T, Schmidt T, Morike K, Osswald H, Gleiter CH (2003) Do alterations of endogenous angiotensin II levels regulate erythropoietin production in humans? Br J Clin Pharmacol 56:378–387
Wang J, Zhang Y, Yang X, Wang X, Zhang J, Fang J, Jiang X (2012) Hemodynamic effects of furosemide on renal perfusion as evaluated by ASL-MRI. Acad Radiol 19:1194–1200
Reubi FC, Weidmann P, Hodler J, Cottier PT (1978) Changes in renal function in essential hypertension. Am J Med 64:556–563
Nelson RG, Bennett PH, Beck GJ, Tan M, Knowler WC, Mitch WE, Hirschman GH, Myers BD (1996) Development and progression of renal disease in Pima Indians with non-insulin-dependent diabetes mellitus. Diabetic Renal Disease Study Group. N Engl J Med 335:1636–1642
Mogensen CE (1971) Glomerular filtration rate and renal plasma flow in short-term and long-term juvenile diabetes mellitus. Scand J Clin Lab Invest 28:91–100
Gooding KM, Lienczewski C, Papale M, Koivuviita N, Maziarz M, Dutius Andersson A-M, Sharma K, Pontrelli P, Garcia Hernandez A, Bailey J, Tobin K, Saunavaara V, Zetterqvist A, Shelley D, Teh I, Ball C, Puppala S, Ibberson M, Karihaloo A, Metsärinne K, Banks R, Gilmour PS, Mansfield M, Gilchrist M, de Zeeuw D, Heerspink HJL, Nuutila P, Kretzler M, Wellberry-Smith M, Gesualdo L, Andress D, Grenier N, Shore AC, Gomez MF, Sourbron S (2020) Prognostic imaging biomarkers for diabetic kidney disease (iBEAt): study protocol. BMC Nephrol 21:1–11
Lee MMY, Gillis KA, Brooksbank KJM, Allwood-Spiers S, Hall Barrientos P, Wetherall K, Roditi G, AlHummiany B, Berry C, Campbell RT (2022) Effect of empagliflozin on kidney biochemical and imaging outcomes in patients with type 2 diabetes, or prediabetes, and heart failure with reduced ejection fraction (SUGAR-DM-HF). Circulation 146:364–367
Goldring W, Chasis H, Ranges HA, Smith HW (1940) Relations of effective renal blood flow and glomerular filtration to tubular excretory mass in normal man. J Clin Invest 19:739–750
Bolomey AA, Michie AJ, Michie C, Breed ES, Schreiner GE, Lauson HD (1949) Simultaneous measurement of effective renal blood flow and cardiac output in resting normal subjects and patients with essential hypertension. J Clin Invest 28:10–17
Esteves FP, Taylor A, Manatunga A, Folks RD, Krishnan M, Garcia EV (2006) 99mTc-MAG3 renography: normal values for MAG3 clearance and curve parameters, excretory parameters, and residual urine volume. Am J Roentgenol 187:W610–W617
Greene ER, Venters MD, Avasthi PS, Conn RL, Jahnke RW (1981) Noninvasive characterization of renal artery blood flow. Kidney Int 20:523–529
Nitzsche EU, Choi Y, Killion D, Hoh CK, Hawkins RA, Rosenthal JT, Buxton DB, Huang SC, Phelps ME, Schelbert HR (1993) Quantification and parametric imaging of renal cortical blood flow in vivo based on Patlak graphical analysis. Kidney Int 44:985–996
Normand G, Lemoine S, Le Bars D, Merida I, Irace Z, Troalen T, Costes N, Juillard L (2019) PET [11C]acetate is also a perfusion tracer for kidney evaluation purposes. Nucl Med Biol 76–77:10–14
Wu W-C, Su M-Y, Chang C-C, Tseng W-YI, Liu K-L (2011) Renal perfusion 3-T MR imaging: a comparative study of arterial spin labeling and dynamic contrast-enhanced techniques. Radiology 261:845–853
Eikefjord E, Andersen E, Hodneland E, Hanson EA, Sourbron S, Svarstad E, Lundervold A, Rorvik JT (2017) Dynamic contrast-enhanced MRI measurement of renal function in healthy participants. Acta Radiol 58:748–757
Naeije R, Fiasse A, Carlier E, Opsomer M, Leeman M (1993) Systemic and renal haemodynamic effects of angiotensin converting enzyme inhibition by zabicipril in young and in old normal men. Eur J Clin Pharmacol 44:35–39
Acknowledgements
BA is funded by Taibah University, Saudi Arabia. KS, KKS and SPS are supported by the BEAT-DKD project funded by the Innovative Medicines Initiative 2 Joint Undertaking under grant agreement No 115974. This Joint Undertaking receives support from the European Union’s Horizon 2020 research and innovation programme and EFPIA with JDRF.
Author information
Authors and Affiliations
Contributions
BA performed the literature search, analysis, and writing the first draft of the manuscript. KS, DLB, KKS, and SPS commented on later versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alhummiany, B., Sharma, K., Buckley, D.L. et al. Physiological confounders of renal blood flow measurement. Magn Reson Mater Phy (2023). https://doi.org/10.1007/s10334-023-01126-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10334-023-01126-7