Abstract
Drowning diagnosis is a complicated process in the autopsy, even with the assistance of autopsy imaging and the on-site information from where the body was found. Previous studies have developed well-performed deep learning (DL) models for drowning diagnosis. However, the validity of the DL models was not assessed, raising doubts about whether the learned features accurately represented the medical findings observed by human experts. In this paper, we assessed the medical validity of DL models that had achieved high classification performance for drowning diagnosis. This retrospective study included autopsy cases aged 8–91 years who underwent postmortem computed tomography between 2012 and 2021 (153 drowning and 160 non-drowning cases). We first trained three deep learning models from a previous work and generated saliency maps that highlight important features in the input. To assess the validity of models, pixel-level annotations were created by four radiological technologists and further quantitatively compared with the saliency maps. All the three models demonstrated high classification performance with areas under the receiver operating characteristic curves of 0.94, 0.97, and 0.98, respectively. On the other hand, the assessment results revealed unexpected inconsistency between annotations and models’ saliency maps. In fact, each model had, respectively, around 30%, 40%, and 80% of irrelevant areas in the saliency maps, suggesting the predictions of the DL models might be unreliable. The result alerts us in the careful assessment of DL tools, even those with high classification performance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Drowning is one of the leading causes of unnatural death worldwide, according to the World Health Organization [1]. In forensic medicine, drowning diagnosis via autopsy is difficult because of its nonspecific pathophysiology [2, 3]. The difficulties mainly arise from the absence of a single pathognomonic sign or test. Drowning may present a wide range of clinical and radiological manifestations, further complicated by variables such as water conditions, drowning scenarios, and the postmortem interval. Thus, it is crucial to notice that drowning diagnosis is based on sum of all the nonspecific findings and exclusion of other causes of death.
Autopsy imaging, such as postmortem computed tomography (PMCT), has been introduced to aid in the drowning diagnosis [4]. However, there is a shortage of forensic pathologists who can interpret imaging scans. Considering the above challenges, deep learning-based computer-aided diagnosis systems have been developed to assist forensic pathologists. Previous studies [5,6,7] have demonstrated the feasibility of deep learning (DL) models for drowning diagnosis using PMCT. These models have achieved high classification accuracy, but the validity of the models remains unknown. Certain research has raised concerns about the potential unreliability of DL models. For instance, some DL-based classification models for COVID-19 screening might generate predictions founded on irrelevant image features sourced from different data sources [8].
To prove the validity of the models, most studies [9,10,11,12,13] have made efforts to provide visual explanations for model predictions using visualization methods like Grad-CAM [14]. Although such visualization can provide insight into the attention of a model by highlighting the important areas on the input images [15, 16], these studies only use it for visual verification and did not carry out any assessment. Some studies had assessed the visual explanations of classification models with the ground truth, but they only conducted hit-or-miss evaluation [17, 18]. Given the inherent black-box nature of DL models, it becomes crucial to assess the validity of these models, which is to determine whether the areas to which the model assigns attention (which form the basis for its predictions) align with human observations.
In this study, we evaluated the validity of DL models for drowning diagnosis by examining the consistency level between model attention (saliency maps) and human observation (manual annotations). Three DL models that had reached the state of the art in a related work of drowning diagnosis [17] were first trained on an in-house PMCT dataset to generate saliency maps. Four annotators independently annotated lung features related to drowning on the dataset. The saliency maps and annotations were then compared and analyzed. Finally, we discussed potential problems and future work.
Materials and Methods
The review board of our institute approved this retrospective study and waived the requirement for informed consent (IRB No. 2021–1-495).
Study Sample and Scan Protocol
There were 2610 bodies that underwent pre-autopsy screening and autopsy at the study institution at Tohoku University from June 2012 to January 2021. Cases that were no later than 2 days after death and underwent drug screens and diatom tests were eligible for inclusion (n = 359). We further excluded 46 cases that were without helical scan or with damage to the thoracic cavity and obtained a study sample of 313 cases, including 153 drowning cases and 160 non-drowning cases, as shown in Fig. 1. Causes of non-drowning death include cardiovascular disease (n = 54), asphyxia other than drowning (n = 19), infection (n = 16), intoxication (n = 14), trauma (n = 14), alcoholic and diabetic ketoacidosis (n = 13), and others (n = 30).
The autopsy diagnosis was based on a comprehensive assessment including PMCT, on-site police investigation, and forensic autopsy. Each case (anonymized) had a free-text autopsy report from a forensic pathologist with 35 years of experience and a free-text radiology report from a board-certified radiologist with 20 years of experience (and 14 years of PMCT interpretation experience) and a radiological technologist who had 14 years of PMCT imaging experience. Both reports had achieved an agreement in the final diagnosis. Due to the particularity of autopsy images, we did not conduct external validation because it is difficult to obtain reliable dissection-proved autopsy imaging data.
PMCT scanning was performed on a multi-channel scanner (Canon Medical Systems, Japan). We obtained high-resolution (HR) chest scans of the lung with protocol of 135 kVp, 190–250 mAs, M-sized field of view (FOV), and 1.0-mm slices (size 512 × 512 pixels) every 30 mm through the chest in a four-row multi-slice mode and processed with lung kernel settings. Following the HR-CT scanning, volumetric helical scans were obtained from the head to the proximal femurs at 120 kVp with variable mAs, a beam pitch of 0.875, LL-sized FOV, and 2.0-mm collimation. The volumetric data allowed reconstruction of whole lung images from 2.0-mm slices, also with lung kernel settings.
Model Architecture and Training
The models are based on AlexNet [19], VGG16 [20], and Inception-ResNet-V2 (InResV2) [21] and have 4 M, 15 M, and 56 M parameters, respectively. The original layers on top of the last convolutional block of AlexNet and VGG16 were replaced by a global average pooling (GAP) layer, two smaller fully connected (FC) layers, and a softmax layer. The 313 PMCT cases were randomly split into training and test set at a ratio of around 85%:15%, and all models were trained from scratch. The loss function was binary cross-entropy, and the optimizer was Adam with a learning rate of 1e − 5 and a decay rate of 1e − 6. To determine whether the training was done, early stopping was applied if the validation loss was no longer decreasing in ten epochs.
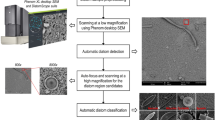
In terms of the model input, we adopted the method mentioned in [17], which can produce better classification and visualization results. To be more specific, a single 2D image only offers information in the transverse plane, resulting in the loss of 3D anatomical details, while 3D volumetric input requires 3D models, resulting in much more parameters to be fitted. Since PMCT data were obtained with a protocol of a four-row multi-slice mode (four 1.0-mm slices every 30 mm), we can pick out images of a case with the same interval and concatenate them vertically or horizontally to embed 3D information into a 2D image, as shown in Fig. 2. The area under the receiver operating characteristic curve (AUC), accuracy, sensitivity, and specificity were used to evaluate the models.
The input of the models [17]. PMCT images with the same interval were concatenated into one 2D image, which was used as an input of the models
Saliency Maps
For most of the papers that generated visual explanation to model predictions, the major saliency methods can be summed up into two kinds: perturbation-based [22, 23] and gradient-based methods [14, 15, 24, 25]. Perturbation-based methods are intuitive and simple to implement but are also time consuming, and gradient-based methods could be of low quality and noisy or show false confidence in visualization results due to the global pooling operation and the gradient vanishing issue in models [16, 26]. Following this discover, Wang et al. proposed a novel gradient-free method named Score-CAM [27], which bridges the gap between perturbation-based and gradient-based methods. In this study, we adopted the Score-CAM to generate saliency maps and compared them with annotations, as shown in Fig. 3. A warmer color (red) in the saliency maps represents a stronger model attention (higher activation).
A simple illustration of a model and its visualization. Models take PMCT images as the input and classify them into non-drowning and drowning. Then, saliency maps are then calculated using the weights of models and further projected to the input to get visualization results. A warmer color in the saliency maps represents a stronger model attention
Human Annotations
To evaluate the saliency maps, four annotators (radiological technologists with over 1 year of clinical experience) used an annotation tool (Labelme, v5.1.1) [28] to annotate 150 images selected at the same interval from the 25 drowning test cases, and finally, we obtained 600 annotation maps. To ensure the quality and validity of the annotations, we invited the experienced radiological technologist (14 years of PMCT imaging experience) as an annotation supervisor and made some rules.
The rules are as below:
-
1)
Annotate features that are associated with drowning according to the reports: consolidation and opacity (granular opacity, ground-glass opacity, edema-like opacity, etc.) in lungs, airway with fluid or solid (only above the carina of trachea), and pleural effusion. Note that we did not distinguish them in the evaluation because the models were for binary classification.
-
2)
Follow both the autopsy and radiology reports and ensure coherency among continuous images.
-
3)
Empty annotation is allowed if features are not significant.
The annotation process referred to the two-phase annotation process of a benchmark dataset called LIDC/IDRI [29] and was organized as below:
-
1)
In the initial blinded-read phase, four annotators independently annotated PMCT scans. Then, the annotation supervisor blindly reviewed and gave comments on each annotation.
-
2)
In the second unblinded-read phase, annotators independently revised their annotations according to the comments.
By following this two-phase process, we aimed to enhance the accuracy of the annotations. Instead of averaging or fusing annotations to achieve an agreement, we kept the differences to evaluate the DL models with the real-world variability of image interpretation.
Validity Assessment
Intersection over union (IoU) was used to measure the consistency between annotations and saliency maps. Two IoU-derived metrics [30], namely Saliency Cover (SC) and Ground Truth Cover (GC), were used to describe the how saliency maps and annotations cover each other. Let S represent saliency maps and G represent annotations, then the metrics can be denoted as:
All metrics range from 0 to 1, with 1 indicating a perfect match between the predicted saliency map (S) and the ground truth (G). IoU, or Jaccard index, measures the overlap between S and G. SC assesses how much of S aligns with G, while GC evaluates how much of G is covered by S. In essence, SC reflects precision, representing the true saliency among all predictions, and GC implies sensitivity, indicating the true saliency among all ground truth annotations.
To decide whether the saliency maps are consistent with annotation, we adopted a default threshold of 0.5 for IoU, as also used in many other benchmark tasks [31, 32]. An example of annotations and saliency maps are shown in Fig. 4. Annotations are binary masks, while saliency maps have continuous pixel values, so in addition to the original saliency maps So, we applied Otsu thresholding [33] to obtain highly activated saliency maps Sh to see the discriminative areas.
Statistics Analysis
Dunn’s test was used for comparison of two groups and Kruskal–Wallis H test for three or more groups, with P < 0.05 for significance. AUC, accuracy, sensitivity, and specificity of the models were described by means with 95% CIs using nonparametric bootstrapping. Considering the asymmetric distributions of IoU, SC, and GC, they were described by medians with interquartile ranges (IQRs). All analysis was performed using Python (v3.9.10, with SciPy v1.9.3 and scikit-learn v1.2.0; Python Software Foundation).
Results
Characteristics of the Study Sample
The study sample is described in Fig. 1 and Table 1. There were 359 cases from 2012 to 2021 that met our inclusion criteria; 46 were excluded due to lacking helical scans or having damage to the thoracic cavities. A total of 313 PMCT cases contained 153 drowning cases (128 for training and 25 for test) and 160 non-drowning cases (135 for training and 25 for test). There was no significant difference between the age of training set and test set according to Dunn’s test (P > 0.05).
Classification Performance of DL Models
The receiver operating characteristic (ROC) curves and the classification performance of models are summarized in Fig. 5 and Table 2. As can be observed, the three models had achieved high AUC, accuracy, sensitivity, and specificity. VGG16 achieved almost the same performance as InResV2, but with a simpler architecture and fewer parameters. This suggests that the improvement from using deeper models on small dataset is limited.
Human Annotations
Unlike risk assessment or diagnosis results, analyzing variability in annotations is challenging because such pixel-level annotations are unstructured data with nonuniform shapes, quantities, and positions. The intraobserver variability was not applicable because of the second unblinded-read phase in the annotation process. To show the interobserver variability among four annotators (A1–A4), we used the area of each annotation map as an index, which was simple but efficient. For the annotation area of each image, A2, A3, and A4 showed no difference (P = 0.20, Kruskal–Wallis H test), but they were significantly different from A1 (P < 0.001, Kruskal–Wallis H test). However, we did not exclude A1’s annotations because there is no specific criterion for the interobserver variability, especially for image interpretation [34]. In addition, the radiologists approved all annotations as “annotations made by different individuals may not be precise but could be correct.”
Validity Assessment
IoU measures the consistency level between the human annotations and the saliency maps; SC and GC describe how much saliency and annotation was covered by each other, respectively. We used the overall medians of IoU, SC, and GC between four annotators and saliency maps in the following unless otherwise noted.
Table 3 summarized the detailed statistical descriptions calculated on the original saliency maps So. Both IoU and SC of A1 were significantly smaller than A2, A3, and A4 (all P < 0.001, Dunn’s test). AlexNet exhibited moderate consistency (IoU of 0.48, SC/GC of 0.66/0.67), with approximately 33% of human annotations not covered and 34% of the saliency maps containing irrelevant information. VGG16 displayed poor consistency with a high GC of 0.90 and low IoU/SC of 0.34/0.37, mainly as a superset of annotations, encompassing over 60% irrelevant content. InResV2 had low IoU/SC of 0.14/0.14, with a GC of 1 indicating complete annotation coverage but producing coarse-grained maps that extended to the entire annotation area.
Similarly, Table 4 showed the results on the highly activated saliency maps Sh. Both IoU and SC of A1 were significantly smaller than A2, A3, and A4 (all P < 0.001, Dunn’s test). AlexNet showed poor consistency with a high SC of 0.80 but low IoU/GC of 0.19/0.20, primarily representing a subset of annotations, covering only 20%. VGG16 also displayed poor consistency, with a decrease in GC (from 0.90 to 0.36) and an increase in SC (from 0.37 to 0.62), resulting in a slight IoU change (from 0.34 to 0.29) due to the removal of a substantial irrelevant portion after thresholding. InResV2 had a decrease in GC to 0.63 after thresholding and low IoU/SC of 0.17/0.19, indicating poor consistency in its highly activated saliency maps.
For a better view, we also presented the overall medians of the IoU, SC, and GC scores using bar plot. It can be observed that So of the models exhibited varying levels of consistency with the annotations in Fig. 6a. In the highly activated saliency maps Sh (Fig. 6b), there were shifts in the patterns, which was mainly caused by reduced irrelevant information after thresholding.
In summary, we found significant inconsistency between the human annotations and the saliency maps of the models. Additionally, models with higher classification performance showed more inconsistency, possibly due to overfitting on the small-scale dataset.
To illustrate the inconsistency between model attention and human annotations, we showed a true positive cases and a false negative case of VGG16. In Fig. 7a, there is a notable inconsistency between the saliency maps and their corresponding annotations. While most annotators marked the areas with pleural effusion, the model did not effectively capture this feature, resulting in a lack of response. In the false negative case depicted in Fig. 7b, the model’s prediction was primarily based on the identification of dry airways and airway-like cavities, while it ignored the presence of fluid-filled airways and pleural effusion. This might be attributed to the fact that dry airways possess well-defined edges that can be more easily detected by computer vision, leading the model to regard them as feature-rich objects. In contrast, the fluid-filled airways and pleural effusion can resemble blood vessels and tissues and are therefore more difficult to distinguish. Furthermore, we observed variations among annotators’ interpretations: one annotator omitted the lung area, while all others included it in their annotations.
Examples of saliency maps (top rows) and corresponding overlapped annotations (bottom rows) are provided for a true positive case (a) and a false negative case (b). The red arrows highlight the region of pleural effusion that the model overlooked. Warmer colors indicate higher activation in the saliency maps and stronger agreement among annotators
Discussion
In this study, we trained three DL classification models for drowning diagnosis, and obtained high AUCs of 0.94 (95% CI: 0.93, 0.95), 0.97 (95% CI: 0.96, 0.98), and 0.98 (95% CI: 0.97, 0.99), respectively. To evaluate the validity of these models, we measured the consistency level between the saliency maps of models and human annotations. Unexpectedly, the best IoU scores were only 0.52, 0.38, and 0.20, respectively, with 30%, 40%, and 80% of the areas in the saliency maps being irrelevant according to the SC and GC scores. To our surprise, the models with higher classification performance had higher inconsistency compared to the human annotations, which may indicate overfitting due to the excessive parameters of the models.
One challenge we faced in this study is interobserver variability, which is especially prevalent in image interpretation tasks that rely on subjective perception. For example, when one person annotates a cat image, he or she may mark the cat’s face, while another may mark the entire profile, and both approaches may be considered correct. In medical imaging, where images may contain ambiguous features, this variability may be even more pronounced. Our results show that the total area of annotations from one of the annotators (A1) was significantly smaller than that of the other annotators (P < 0.001, Kruskal–Wallis H test), resulting in smaller scores of IoU and SC, as all metrics were calculated based on the area of annotations and saliency maps. This highlights the significant impact that ground truth annotations can have on the training and evaluation of models.
Some possible solutions to this challenge are as follows. First, keeping a detailed record of the annotation process could help identify and correct errors or biases that may have occurred. Second, having an expert supervise and review the annotation process can help improve the accuracy and quality of the annotations, as was employed in this study. Finally, crowdsourcing could be an effective approach to obtain high-quality annotations. For example, a collaborative framework [35] has been proposed to engage medical students and pathologists in producing quality labels for cell nuclei, without sacrificing diversity. By collecting a larger number of annotations from multiple annotators, we can mitigate the bias and variability in the training and evaluation of our models.
There are some limitations in this study. First, we could not find a forensic pathologist who can interpret radiological images to make annotations directly, which is one of the motivations for developing the CAD system. To ensure the credibility of the annotations, we adopted a two-phase annotation process, referred to the autopsy and radiology reports during annotation, and revised the annotations according to the comments of the experienced radiologist. The second issue is an inherent problem in the evaluation method. We used IoU and its derivatives SC and GC to measure the similarity and inclusive relation between annotations and saliency maps. IoU is a common and suitable metric for detection and segmentation tasks because the outputs of models, e.g., bounding boxes and segmented maps, are designed to be as close as possible to the annotations. However, the original outputs of a classification model are numbers corresponding to numerical labels, not annotation maps, which leads to a significant difference in area between saliency maps and annotations. In fact, the area of So was 2.92 to 3.97 times that of the annotations, while Sh was only 0.60 to 0.82 times that of the annotations. Consequently, even if all saliency maps and annotations overlap perfectly, we can only have a maximum IoU score of around 0.35 for So and 0.82 for Sh, not 1, so do the SC and GC. Although it seems improper to evaluate classification models using these metrics, there is no criterion for such evaluation, especially for image interpretation.
To address these problems, the validity of classification models needs further research, possibly by combining deep learning with detailed human expertise, as is common in detection/segmentation tasks. It is worth noting that interobserver variability can be observed among annotators, which may affect the evaluation results. Therefore, the annotation process and evaluation metrics should be carefully considered. Our future work will focus on developing deeply supervised methods to improve the validity of our models and alleviate the negative impact of interobserver variability on evaluation results.
Conclusion
Three DL models were trained for drowning diagnosis and achieved high classification performance. However, the saliency maps generated from these models showed inconsistency attention with human annotations, suggesting that the models may be unreliable from the perspective of medical image diagnosis, or the annotations were subjective and prone to biases. The result alerts us in the careful assessment of DL tools, even those with high classification performance.
Data Availability
Data are accessible from the corresponding author by request, subject to approval from the institutional review board.
References
Status of drowning in South-East Asia: Country reports. World Health Organization (WHO). https://www.who.int/publications/i/item/9789290210115. Accessed December 15, 2022.
Vander Plaetsen S, De Letter E, Piette M, Van Parys G, Casselman JW, Verstraete K: Post-mortem evaluation of drowning with whole body CT. Forensic science international 249:35-41. https://doi.org/https://doi.org/10.1016/j.forsciint.2015.01.008, Apr 1, 2015.
Christe A, Aghayev E, Jackowski C, Thali MJ, Vock P: Drowning—post-mortem imaging findings by computed tomography. European radiology 18:283-290, 2008.
Usui A, Kawasumi Y, Funayama M, Saito H: Postmortem lung features in drowning cases on computed tomography. Japanese journal of radiology 32:414-420, 2014.
Homma N, Zhang X, Qureshi A, Konno T, Kawasumi Y, Usui A, Funayama M, Bukovsky I, Ichiji K, Sugita N, Yoshizawa M: A deep learning aided drowning diagnosis for forensic investigations using post-mortem lung CT images. In 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society, pp.1262–1265. https://doi.org/10.1109/EMBC44109.2020.9175731, Jul 20, 2020.
Zeng Y, Zhang X, Kawasumi Y, Usui A, Ichiji K, Funayama M, Homma N: Deep learning-based interpretable computer-aided diagnosis of drowning for forensic radiology. In 2021 60th Annual Conference of the Society of Instrument and Control Engineers of Japan, pp. 820–824, Sep 8, 2021.
Ogawara T, Usui A, Homma N, Funayama M: Diagnosing drowning in postmortem CT images using artificial intelligence. The Tohoku Journal of Experimental Medicine 259(1): 65-75, 2023.
Sadre R, Sundaram B, Majumdar S, Ushizima D: Validating deep learning inference during chest X-ray classification for COVID-19 screening. Scientific reports 11(1):16075, 2021.
Bae J, Yu S, Oh J, Kim TH, Chung JH, Byun H, Yoon MS, Ahn C, Lee DK: External validation of deep learning algorithm for detecting and visualizing femoral neck fracture including displaced and non-displaced fracture on plain X-ray. Journal of Digital Imaging 34(5):1099-109, 2021.
Singh V, Danda V, Gorniak R, Flanders A, Lakhani P: Assessment of critical feeding tube malpositions on radiographs using deep learning. Journal of digital imaging 32:651-655, 2019.
Erten M, Tuncer I, Barua PD, Yildirim K, Dogan S, Tuncer T, Tan RS, Fujita H, Acharya UR: Automated urine cell image classification model using chaotic mixer deep feature extraction. Journal of Digital Imaging 2:1-2, 2023.
Qiu S, Joshi PS, Miller MI, Xue C, Zhou X, Karjadi C, Chang GH, Joshi AS, Dwyer B, Zhu S, Kaku M: Development and validation of an interpretable deep learning framework for Alzheimer’s disease classification. Brain 143(6):1920-1933, 2020.
Liu H, Li L, Wormstone IM, Qiao C, Zhang C, Liu P, Li S, Wang H, Mou D, Pang R, Yang D: Development and validation of a deep learning system to detect glaucomatous optic neuropathy using fundus photographs. JAMA ophthalmology 137(12):1353-1360, 2019.
Selvaraju RR, Cogswell M, Das A, Vedantam R, Parikh D, Batra D: Grad-cam: Visual explanations from deep networks via gradient-based localization. Proceedings of the IEEE international conference on computer vision, pp. 618–626. https://doi.org/10.48550/arXiv.1610.02391, 2017.
Zeiler MD, Fergus R. Visualizing and understanding convolutional networks. Proceedings of Computer Vision–ECCV, pp. 818–833, September 6–12, 2014.
Singh A, Sengupta S, Lakshminarayanan V. Explainable deep learning models in medical image analysis. Journal of Imaging 6(6), 52, 2020.
Zeng Y, Zhang X, Kawasumi Y, Usui A, Ichiji K, Funayama M, Homma N: A 2.5D deep learning-based method for drowning diagnosis using post-mortem computed tomography. IEEE Journal of Biomedical and Health Informatics 27(2):1026–1035, 2023.
Arun N, Gaw N, Singh P, Chang K, Aggarwal M, Chen B, Hoebel K, Gupta S, Patel J, Gidwani M, Adebayo J: Assessing the trustworthiness of saliency maps for localizing abnormalities in medical imaging. Radiology: Artificial Intelligence 3(6): e200267, 2021.
Krizhevsky A, Sutskever I, Hinton GE: Imagenet classification with deep convolutional neural networks. Communications of the ACM 60(6): 84-90, 2017.
Simonyan K, Zisserman A: Very deep convolutional networks for large-scale image recognition. arXiv preprint arXiv:1409.1556, Sep 4, 2014.
Szegedy C, Ioffe A, Vanhoucke V, Alemi AA: Inception-v4, inception-resnet and the impact of residual connections on learning. Thirty-first AAAI conference on artificial intelligence, pp. 4278–4284, 2017.
Ribeiro MT, Singh S, Guestrin C: Why should I trust you?" Explaining the predictions of any classifier: Proceedings of the 22nd ACM SIGKDD international conference on knowledge discovery and data mining, pp.1135–1144, 2016.
Lundberg SM, Lee SI: A unified approach to interpreting model predictions. Advances in neural information processing systems (NIPS) 30, 2017.
Springenberg JT, Dosovitskiy A, Brox T, Riedmiller M: Striving for simplicity: The all convolutional net. arXiv preprint arXiv:1412.6806, Dec 21, 2014
Chattopadhay A, Sarkar A, Howlader P, Balasubramanian VN: Grad-cam++: Generalized gradient-based visual explanations for deep convolutional networks. IEEE winter conference on applications of computer vision (WACV),pp. 839–847, 2018.
Reyes M, Meier R, Pereira S, Silva CA, Dahlweid FM, Tengg-Kobligk HV, Summers RM, Wiest R: On the interpretability of artificial intelligence in radiology: challenges and opportunities. Radiology: artificial intelligence 27;2(3):e190043, 2020.
Wang H, Wang Z, Du M, Yang F, Zhang Z, Ding S, Mardziel P, Hu X: Score-CAM: Score-weighted visual explanations for convolutional neural networks. Proceedings of the IEEE/CVF conference on computer vision and pattern recognition workshops, pp. 24–33, 2020.
Wada K. Labelme: Image Polygonal Annotation with Python. https://github.com/wkentaro/labelme
Armato III SG, McLennan G, Bidaut L, McNitt‐Gray MF, Meyer CR, Reeves AP, Zhao B, Aberle DR, Henschke CI, Hoffman EA, Kazerooni EA: The lung image database consortium (LIDC) and image database resource initiative (IDRI): a completed reference database of lung nodules on CT scans. Medical physics 38(2): 915-931, 2011.
Boggust A, Hoover B, Satyanarayan A, Strobelt H: Shared interest: Measuring human-AI alignment to identify recurring patterns in model behavior. Proceedings of the CHI Conference on Human Factors in Computing Systems, pp. 1–17, 2022.
Hoiem D, Chodpathumwan Y, Dai Q: Diagnosing error in object detectors. In European conference on computer vision, pp. 340–353, Oct 7, 2012.
Redmon J, Divvala S, Girshick R, Farhadi A: You only look once: Unified, real-time object detection. In Proceedings of the IEEE conference on computer vision and pattern recognition, pp. 779–788. 2016.
Otsu N. A threshold selection method from gray-level histograms. IEEE transactions on systems, man, and cybernetics 9(1): 62-66, 1979.
Hausman NL, Javed N, Bednar MK, Guell M, Schaller E, Nevill RE, Kahng S: Interobserver consistency: A preliminary investigation into how much is enough? Journal of applied behavior analysis 55(2): 357-368, 2022.
Amgad M, Atteya LA, Hussein H, Mohammed KH, Hafiz E, Elsebaie MA, Alhusseiny AM, AlMoslemany MA, Elmatboly AM, Pappalardo PA, Sakr RA: NuCLS: A scalable crowdsourcing approach and dataset for nucleus classification and segmentation in breast cancer. Giga Science 11: 1-12, 2022.
Acknowledgements
We would like to thank the radiological technologists Hamabe H, Shinohara Y, Awaji I, and Ishii M for their contribution and great efforts in the radiology reports and the annotations.
Funding
This work was supported by Autopsy imaging Center, Tohoku University Graduate School of Medicine, and JSPS KAKENHI Grant Numbers JP18K19892, JP19H04479, and JP20K08012.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Usui A and Funayama M. Model training and data analysis were performed by Zeng Y and Zhang X. The first draft of the manuscript was written by Zeng Y, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The review board of Tohoku University Graduate School of Medicine approved this retrospective study (IRB No. 2021–1-495).
Consent to Participate
The requirement for informed consent was waived by Tohoku University Graduate School of Medicine. All methods and procedures were carried out in accordance with the Declaration of Helsinki.
Consent for Publication
This manuscript has not been published or presented elsewhere in part or in entirety and is not under consideration by another journal. We have read and understood your journal’s policies, and we believe that neither the manuscript nor the study violates any of these.
Competing Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zeng, Y., Zhang, X., Wang, J. et al. Inconsistency between Human Observation and Deep Learning Models: Assessing Validity of Postmortem Computed Tomography Diagnosis of Drowning. J Digit Imaging. Inform. med. 37, 1–10 (2024). https://doi.org/10.1007/s10278-024-00974-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10278-024-00974-6