Abstract
This multicenter, double-blind study evaluated the effects of three doses of adalimumab in Japanese patients with rheumatoid arthritis (RA). Patients were randomized to placebo (n = 87) or adalimumab 20 mg (n = 87), 40 mg (n = 91), or 80 mg (n = 87) every other week for 24 weeks. The primary efficacy endpoint was the American College of Rheumatology criteria for 20% improvement (ACR20) at Week 24. At Week 24, all adalimumab treatment groups achieved statistically significantly better ACR20 response rates (20 mg: 28.7%, P < 0.05; 40 mg: 44.0%, P < 0.001; and 80 mg: 50.6%, P < 0.001) versus placebo (13.8%), as well as statistically significantly greater ACR50 and ACR70 responses for the two higher adalimumab doses versus placebo. Rates of adverse events were comparable between the adalimumab groups and the placebo group, except for injection-site reactions, which occurred in more adalimumab-treated patients. Adalimumab 20, 40, and 80 mg were safe and effective in Japanese patients; however, the greatest responses occurred with the 40 and 80 mg doses. These results and comparable ACR20 responses in Western patients support adalimumab 40 mg every other week as the appropriate dosage to treat RA in Japanese patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is the most common inflammatory arthritis, estimated to affect between 0.5 and 1.0% of the adult population worldwide [1]. Geographic differences in the incidence of RA in a particular country may be associated with genetic, environmental, or cultural factors [1]. Moreover, differences in ethnicity, medical status, and socioeconomic status may affect response to RA treatment [2].
In Japan, it is estimated that more than 700,000 patients within a population of 120 million have RA [3]. Of those afflicted, 70% are women and 10% are bedridden; the morbidity rate is estimated to be 0.5% [3, 4]. In Japanese patients, RA is an independent risk factor for mortality [5].
In the past decade, the treatment of RA has dramatically changed with the introduction of biologics that target inflammatory cytokines, such as tumor necrosis factor (TNF) [6–8]. Recently, the TNF antagonists infliximab (in combination with methotrexate [MTX]) and etanercept have demonstrated efficacy in Japanese patients with RA [2, 9–11]. Adalimumab is the first fully human monoclonal antibody that binds with high specificity to TNF [12]. Adalimumab has been well established in the treatment of patients with RA in multiple clinical trials conducted in North America [13] and in Europe, [14] both with and without concomitant MTX.
The objective of this study (CHANGE: Clinical investigation in Highly disease-affected rheumatoid Arthritis patients in Japan with Adalimumab applying staNdard and General Evaluation) was to evaluate the safety, efficacy, and pharmacokinetics of three different doses of subcutaneous adalimumab compared with placebo in Japanese patients with RA. In addition, this study was designed as a bridging study to compare efficacy and safety results with those from a previously published study of adalimumab conducted in Western patients with RA [14].
Although adalimumab in Western regions of the world is primarily used in combination with MTX, this study evaluated adalimumab monotherapy and compared the results with the Western study in which adalimumab was also evaluated as monotherapy. Moreover, the combination of adalimumab and MTX was not used in this bridging study because of differences in MTX dosages used in Japan and Western countries. The maximum approved oral MTX dosage in Japan is 8 mg/week, which is much lower than the 15–20 mg/week dosage commonly used in Western countries [2, 8, 15, 16].
Patients and methods
Male and female patients aged 20 years or older were recruited from 68 sites in Japan. Eligible patients met the American College of Rheumatology (ACR) criteria for active RA, had failed treatment with at least one prior disease-modifying antirheumatic drug (DMARD), and had ≥10 swollen joints and ≥12 tender joints (excluding distal interphalangeal joints) at both the screening visit and baseline visit. Patients also had a C-reactive protein (CRP) concentration ≥2 mg/dl.
Patients taking a DMARD, including MTX, must have discontinued DMARDs at least 28 days prior to study drug administration and returned for baseline visit within 42 days. Use of a live vaccine within 3 months; treatment with an investigational biologic, including anti-CD4 antibody, within 6 months; or prior treatment with any TNF antagonist or an alkylating agent was not permitted.
Exclusion criteria included patients with acute inflammatory joint diseases other than RA, active Listeria or tuberculosis, lymphoma, or leukemia, or any malignancy except for successfully treated nonmetastatic basal-cell carcinoma of the skin. Patients with positive serology for anti-human immunodeficiency virus antibody, hepatitis B virus surface antigen, or anti-hepatitis C virus antibody, ongoing or active infection, advanced or poorly controlled diabetes, or central nervous system demyelinating disorders were also excluded.
Patients with positive chest X-ray or strongly positive tuberculin skin test (≥10 mm diameter of erythema and double redness/bullae/necrosis) could not be enrolled. Patients with a positive (≥5 mm of induration), but not strongly positive, tuberculin skin test could be enrolled if receiving prophylactic isoniazid 300 mg daily at least three weeks prior to baseline.
A negative pregnancy test and use of reliable contraception were mandatory for women of childbearing potential. All patients were required to give written informed consent. This study was conducted in compliance with the study protocol, the standards of the Pharmaceutical Affairs Law, the Ministerial ordinance concerning Good Clinical Practice, and all other applicable regulatory requirements.
Study design
This was a Phase II/III, multicenter, double-blind, placebo-controlled trial comparing three different doses of adalimumab given as monotherapy performed from February 2004 through June 2005.
Patient eligibility was determined at screening and at baseline, during the period from 28 to 42 days prior to study drug administration for patients who required a wash-out period for DMARD therapy, and within 42 days prior to study drug administration for all other patients. Patients were randomly assigned in a 1:1:1:1 ratio to four treatment groups: 20 mg adalimumab every other week (eow), 40 mg adalimumab eow, 80 mg adalimumab eow, or placebo eow, administered by subcutaneous injection starting at Week 0 and continuing until Week 22. Study drug was administered by a physician or nurse supervised by an investigator.
Patients who experienced an increase in disease activity or who had less than 10% reduction in tender joint counts (TJC) and swollen joint counts (SJC) compared with baseline after at least eight weeks of treatment stopped study therapy with adalimumab/placebo and were switched to an open-label rescue treatment that could include higher doses of steroids, nonsteroidal antiinflammatory drugs, or conventional DMARDs. Patients completing 24 weeks of treatment, either double-blind or open-label rescue, had the option to enter an open-label extension study to receive 40 mg of adalimumab eow.
Efficacy assessment
The primary efficacy endpoint was ACR20 response rate at Week 24 for the adalimumab 40 and 80 mg groups compared with placebo. The comparison between ACR20 response rates at Week 24 for the adalimumab 20 mg group and the placebo group was a secondary endpoint. The ACR components were evaluated at Weeks 0 (predose), 2, 4, 8, 12, 16, 20, and 24. Additional secondary efficacy endpoints included ACR20 response rate at Week 12; ACR50 and ACR70 response rates at Weeks 12 and 24; individual components of the ACR response (including TJC and SJC) at Weeks 0 (baseline), 12, and 24; and the Health Assessment Questionnaire Disability Index (HAQ DI) at Weeks 0 (baseline), 12, and 24. Morning stiffness was evaluated at Weeks 0 (predose), 2, 4, 8, 12, 16, 20, and 24; and rheumatoid factor (RF) was evaluated at Weeks 0 (predose), 12, and 24. In addition, ACR20 area under the curve (AUC) over the 24-week study period was determined. ACR20 AUC was defined as the sum of the duration that patients achieved an ACR20 response.
Pharmacokinetic analyses
Pharmacokinetic analyses included serum adalimumab concentrations and serum anti-adalimumab antibody (AAA) concentrations, which were determined using a validated enzyme-linked immunosorbent assay (ELISA) based on a double-antigen technique. The lower limit of quantitation for adalimumab and AAA were established at 2.5 and 0.5 ng/mL, respectively, in diluted serum. Because of interference of adalimumab concentrations with the AAA assay, AAA concentrations were analyzed only if the adalimumab concentration was less than 2 μg/mL.
Blood samples for serum adalimumab concentrations were collected at Weeks 0 (immediately prior to dosing), 2, 4, 8, 12, 16, 20, and 24 (or following the last dose) and at the follow-up visit. Blood samples for AAA concentrations were collected at Weeks 0 (immediately prior to dosing), 4, 8, 12, 16, 20, and 24 (or following the last dose) and at the follow-up visit.
Safety assessment
Safety was evaluated on the basis of treatment-emergent adverse events (AEs). Laboratory tests, including hematology tests, clinical chemistry tests, and urinalysis, were conducted at screening; at Weeks 0 (predose), 2, 4, 8, 12, 16, 20, and 24 (or last dose); and at the follow-up visit. Vital signs and physical examinations were also evaluated. Comparisons were made of changes from Week 0 (predose) during treatment for all treatment groups.
Statistical analysis
To detect a difference of 25% in ACR20 response rates between the placebo group and the adalimumab 40 mg group, assuming an ACR response rate of 20% in the placebo arm and 45% in the 40 mg eow arm, a sample size of 74 patients per treatment group was estimated to be required to provide 80% power for a two-sided test (continuity corrected) with an alpha of 0.025. Therefore, taking the exclusion analysis into consideration, a total of 320 subjects (80 subjects per treatment group) needed to be equally allocated to one of the four treatments: 20 mg adalimumab, 40 mg of adalimumab, 80 mg adalimumab, or placebo.
Demographic and baseline characteristics were compared among the four treatment groups using the one-way analysis of variance test for continuous variables and the χ 2 test for categorical variables. All efficacy analyses were primarily performed on the full analysis set population, defined as all randomized patients who received at least one dose of study drug and from whom at least one assessment of efficacy under double-blind medication was available. Unless otherwise specified, statistical significance was set at P = 0.05 (two-sided) for all tests. The effect of study centers was analyzed; however, because there were not enough patients per treatment per center, study center was not adjusted in the statistical analyses.
The primary efficacy endpoint, ACR20 response rate at Week 24, was compared for the placebo group against that of the 40 and 80 mg eow adalimumab groups, using the Pearson χ 2 test. The Hochberg procedure was applied to control for multiplicity of testing. If both P values were less than 0.05, then the individual null hypotheses (no treatment difference between adalimumab and the placebo) were rejected. If one P value did not show significance at 0.05, then the other hypothesis was tested against and adjusted at the 0.025 level. If the test was significant at the adjusted 0.025 level, then the null hypothesis was rejected.
The response rate for ACR20 between the adalimumab 20 mg group and placebo at Week 24 was a secondary endpoint and was compared using the Pearson χ 2 test. For the additional secondary endpoints, ACR20 at Week 12 and ACR50 and ACR70 at Weeks 12 and 24, number of responders and response rates were presented in each group. Improvements in individual components of the ACR response at Week 0 (predose) and at Weeks 12 and 24 were presented as summary statistics for each treatment group, and comparisons between the placebo group and each adalimumab group were performed using analysis of covariance, with baseline values as covariates. For ACR20 AUC, summary statistics by treatment group were presented.
Patients who discontinued the study prior to Week 24 or who moved to the rescue arm following at least eight weeks of treatment were classified as nonresponders. In addition, the last observation carried forward post baseline was conducted for the following analyses: ACR20 response rate at Week 24; ACR50 and ACR70 at Weeks 12 and 24; ACR20 at Week 12; individual components of the ACR response at Weeks 0 (predose), 12, and 24; and ACR20 AUC. The last non-missing visit up to and including the Week-24 assessment for each patient was summarized as the endpoint visit.
All patients who received at least one dose of double-blind study medication were included in the safety analysis. Summary statistics included frequency tabulations and were presented by the Medical Dictionary for Regulatory Activities, version 8.0, preferred term and system organ class for each treatment group.
Results
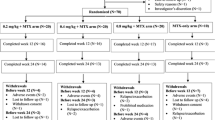
A total of 482 patients were screened and 352 patients met the entry criteria and were randomized to the four treatment groups (placebo, n = 87; adalimumab 20 mg, n = 87; adalimumab 40 mg, n = 91; adalimumab 80 mg, n = 87). A total of 34 (9.7%) of 352 patients discontinued treatment (7, 7, 16, and 4 in the placebo and adalimumab 20, 40, and 80 mg groups, respectively) (Fig. 1). Three of the 34 discontinuations occurred during the rescue period. Discontinuations because of AEs occurred in 4 (4.6%), 5 (5.7%), 12 (13.2%), and 3 (3.4%) patients, in the placebo and adalimumab 20, 40, and 80 mg groups, respectively. Other reasons for early discontinuation included withdrawal of consent, protocol violations, and administrative reasons. A total of 107 patients received rescue medication after ≥8 weeks of double-blind study treatment (45, 26, 17, and 19 in the placebo and adalimumab 20, 40, and 80 mg groups, respectively). The three discontinuations that occurred during the rescue period occurred in one patient each from the original placebo, adalimumab 40 mg, and adalimumab 80 mg groups. A total of 312 (98.1%) of 318 patients who completed the study entered the extension study and 309 patients continued treatment with adalimumab.
Baseline demographics and disease-state characteristics are included in Table 1. For the overall study group, the mean age was 54.9 years, 79.5% of patients were female, the mean weight was 53.7 kg, the mean duration of RA was 9.5 years, and the mean TJC and SJC were 24.4 and 19.6, respectively. Baseline demographics were similar between groups. Baseline disease characteristics were consistent with what is generally observed in patients with RA with moderate to severe disease and were comparable between treatment groups with the following exceptions: the mean of the patient’s global assessment of disease activity for the placebo group (64.6 mm) was lower than those for the adalimumab groups (20 mg: 73.1 mm; 40 mg: 71.2 mm; 80 mg: 75.7 mm; P = 0.003); the mean of HAQ DI for the placebo group (1.39) was lower than those for the adalimumab groups (20 mg: 1.57; 40 mg: 1.64; 80 mg: 1.77; P = 0.010); and the mean CRP for the 20 mg group (4.97 mg/dl) was lower than those for other groups (placebo: 5.86 mg/dl; 40 mg: 6.48 mg/dl; 80 mg: 6.56 mg/dl; P = 0.020).
All patients had previously used one or more DMARDs, and 91.5% (322/352) of the randomized patients had previously used two or more DMARDs. The most common previous DMARDs were MTX (87.2%), salazosulfapyridine (sulfasalazine: 73.9%), and bucillamine (67.6%). More than half (60.5%) of the patients used previous RA treatments other than DMARDs. The most common previous RA treatments other than DMARDs were prednisolone (29.3%), diclofenac (10.8%), and triamcinolone (8.5%).
Primary efficacy: ACR20 at Week 24
At Week 24, adalimumab demonstrated dose-dependent increases in ACR20 response rates and all adalimumab treatment groups achieved statistically significantly higher ACR20 responses (28.7% in the 20 mg group, P < 0.05; 44.0% in the 40 mg group, P < 0.001; and 50.6% in the 80 mg group, P < 0.001) compared with the placebo group (13.8%) (Table 2).
ACR20, ACR50, and ACR70 response rates
Similarly, ACR20 response rates at Week 12 were statistically significantly greater in all adalimumab treatment groups compared with placebo (Table 2). ACR50 and ACR70 responses were statistically significantly greater in all adalimumab treatment groups compared with placebo at Weeks 12 and 24, except for the ACR50 response for the 20 mg group at Week 24 and the ACR70 response for the 20 mg group at Week 12 (Table 2). Overall, the increases in adalimumab ACR20, ACR50, and ACR70 response rates were time dependent (Fig. 2). All adalimumab treatment groups showed ACR20 response rates exceeding 30% at Week 2. For the 40 and 80 mg groups, ACR20 response rates were maintained during the study. However, for the 20 mg group, ACR20 responses fell gradually from Week 16 until the end of the study. In general, ACR50 and ACR70 responses had the tendency to increase with time in each treatment group (Fig. 2).
ACR core components
For both the 40 and 80 mg groups, all individual ACR components showed statistically significant improvement compared with the placebo group (P < 0.05) at Week 24, with the exception of patient’s assessment of pain for the 80 mg group and HAQ DI for the 40 and 80 mg groups (Table 3). For the 20 mg group, there was only significant improvement in SJC compared with the placebo group at Week 24. After adjusting for lower baseline CRP levels in the 20 mg group, results of subgroup analyses found that CRP had a statistically significant relationship to the ACR20 response rate (odds ratio: 0.9); however, its effect on the primary efficacy endpoint evaluation was small. ACR20 response rates in all adalimumab groups with the adjustments were still statistically significantly greater compared with placebo response rates, as achieved without the adjustments.
Morning stiffness
At Week 24, greater percentages of patients in each adalimumab treatment group reported complete resolution of baseline morning stiffness (17.1% in the 20 mg group, 22.9% in the 40 mg group, and 25.0% in the 80 mg group) compared with the placebo group (6.7%). At Week 24, the mean observed duration of morning stiffness compared with baseline decreased by 55.8, 87.6, and 137.0 min in the 20, 40, and 80 mg adalimumab groups, respectively, versus 5.9 min in the placebo group.
RF status
Of the RF-positive patients at baseline, 3.4, 6.0, 9.8, and 6.7% of patients in the placebo and adalimumab 20, 40, and 80 mg groups, respectively, shifted to RF-negative at Week 24, with no significant differences between groups. Of the RF-negative patients at baseline, two patients (one in the placebo group and one in the adalimumab 40 mg group) shifted to RF-positive at Week 24.
Pharmacokinetic analysis
Serum trough concentrations of adalimumab reached a steady state approximately by Week 8 and remained relatively constant through Week 24 (Fig. 3a). Serum adalimumab concentrations were lower in the lower dose groups (20 and 40 mg) compared with the 80 mg group.
a Mean (SD) serum adalimumab concentrations over time. b Distribution (%) of samples with positive serum anti-adalimumab antibody (AAA) concentrations. c Mean (SD) predose serum adalimumab concentrations (μg/mL) over time in Japanese patients with rheumatoid arthritis who completed the 24-week study with every-other-weekly adalimumab treatment stratified by AAA status
The percentages of patients who had at least one AAA-positive serum sample from the start of study drug treatment until 30 days after the last dose were 40.2, 44.0, and 26.4% in the 20, 40, and 80 mg adalimumab groups, respectively. The distribution of serum AAA-positive concentrations is shown in Fig. 3b. The majority of patients who were positive for AAA had relatively low titers. Mean serum adalimumab concentrations over time stratified by AAA status are depicted in Fig. 3c. Concentration-versus-time curves normalized once AAA status was considered.
For ACR20 response rate at Week 24, the AAA-positive patients (14.3, 27.5, and 34.8%) in the adalimumab 20, 40, and 80 mg groups showed lower response rates than AAA-negative patients (38.5, 56.9, and 56.3%), respectively. ACR50 response at Week 24 showed a similar tendency (AAA-positive [5.0–13.0%] and AAA-negative [19.2–39.2%]).
Safety
All patients who received at least one injection of study drug and at least one postbaseline safety evaluation (n = 352) were included in the safety analysis. Overall, 81.6, 92.0, 98.9, and 93.1% of patients in the placebo and the adalimumab 20, 40, and 80 mg groups, respectively, reported at least one treatment-emergent AE during the double-blind study period (Table 4). The number of AEs that occurred in the 40 and 80 mg groups were statistically significantly greater compared with the placebo group (P < 0.05 for both groups) (Table 4). The majority of AEs were mild or moderate in intensity. The most common treatment-emergent AEs across all treatment groups were nasopharyngitis, injection site erythema, anti-dsDNA antibody–positive reaction, and anti–nuclear antibody–positive reaction. Injection-site reaction was reported by a statistically significantly greater percentage of patients in each of the adalimumab treatment groups compared with placebo (Table 4). However, most of these reactions, although reported frequently, were generally mild or moderate in nature and rarely led to discontinuation of treatment. Also, injection-site reactions tended to decrease over time. Three patients in the adalimumab 40 mg group discontinued the study because of injection-site reactions. Severe AEs were reported at similar rates in the adalimumab groups and the placebo group (Table 4).
Infectious AEs were also reported at similar rates in the adalimumab groups and the placebo group. A total of 44 infectious AEs were reported by 36.8% (32/87) of placebo-treated patients and 161 infectious AEs were reported by 40.8% (108/265) of the adalimumab-treated patients. The most common infectious AE, nasopharyngitis, was reported by 15.8% of the patients in all of the adalimumab groups and by 18.4% of placebo-treated patients. The next most common infectious AE, upper respiratory tract infection, was reported by 4.5% of adalimumab-treated patients and by 2.3% of placebo-treated patients. In general, the majority of infectious AEs were mild or moderate in intensity; only five AEs were considered to be severe by the investigator (acute bronchitis and two events of pneumonia in the 20 mg group and infectious bursitis and infectious dacryocystitis in the 40 mg group).
Rates of serious AEs were comparable between the adalimumab groups and the placebo group. Three serious AEs resulted in death in two patients—one patient in the adalimumab 40 mg group died from interstitial lung disease and from lung infection, which was considered possibly related to treatment, and one patient in the adalimumab 80 mg group died from cerebral hemorrhage, which was considered unrelated to treatment. There were no reports of malignancies or tuberculosis in the adalimumab treatment groups. Malignancies were reported in two patients in the placebo group during the double-blind period. There were no clinically relevant differences between treatment groups in physical examination results, vital signs, or laboratory measurements. There were some minor differences in safety profile for AAA-positive patients and AAA-negative patients, but the differences were not clinically important. The most notable difference was the rate of injection-site reactions.
Discussion
In this study of Japanese patients with moderate to severe RA, three adalimumab dosages (20, 40, and 80 mg eow) encompassed the range of effective and well-tolerated dosages shown in previous clinical studies of adalimumab in North America, Australia, and Europe. [13, 14, 17–19] For the primary efficacy endpoint—ACR20 response rates at Week 24—the adalimumab 20, 40, and 80 mg groups showed dose-dependent improvement and were statistically significantly greater than that seen in placebo-treated patients. In each adalimumab dosage group, the percentage of patients achieving an ACR 20 response increased from Week 1 through Week 12 and continued at that level through Week 24.
The results of this bridging study in Japanese patients were intended to be compared with data from a similar study in Western patients with RA conducted in Europe, Australia, and Canada [14]. Similar study designs allow for comparisons between the two study populations. Both studies were multicenter, double-blind, placebo-controlled, randomized trials. This study in Japanese patients is a Phase II/III study, which included 352 Japanese patients, and the Western study was a Phase III study, which included 544 patients (98.2% white). Both studies included patients with RA who had an inadequate response to one or more DMARDs and TJC ≥ 12, SJC ≥ 10, and CRP ≥ 2 mg/dl. This Japanese study evaluated adalimumab 20, 40, and 80 mg eow; whereas the Western study evaluated adalimumab 20 and 40 mg eow and 20 and 40 mg weekly. The 80 mg eow dosage in Japanese patients can be roughly compared with the 40 mg weekly dosage in Western patients, achieving a similar dosage over time.
It was not practical to dose adalimumab weekly in this study conducted in Japanese patients as in the Western study, because it is generally not standard procedure for patients in Japan to self-inject their subcutaneous medications; therefore, weekly visits to receive their study drug would be inconvenient. Baseline demographics and disease characteristics were comparable, except for weight and height, which were lower in Japanese patients, as expected; TJC was also lower in Japanese patients, but not SJC.
The primary efficacy endpoints were similar—ACR20 at Week 24 (Japanese) and ACR20 at Week 26 (Western). The results of both studies found comparable ACR response rates supporting 40 mg eow as the appropriate standard dose (Fig. 4). ACR20 response rates were 19.1, 35.8, 46.0, and 53.4% in the placebo group and the adalimumab 20, 40, and 40 mg/week groups, respectively, in Western patients. Similarly, ACR20 responses were 13.8, 28.7, 44.0, and 50.6% in the placebo group and the adalimumab 20, 40, and 80 mg eow groups, respectively, in Japanese patients. Serum trough concentrations of adalimumab in both Japanese and Western patients were almost constant after Week 8. However, mean steady-state serum concentrations of adalimumab in Japanese patients were lower compared with Western patients in the 40 mg group and slightly lower in the 20 mg group. There was a similar influence of AAAs on efficacy in both studies, with lower ACR20 response rates in AAA-positive patients than in AAA-negative patients, although the positivity for AAA was higher in our study compared with the Western study (40.2 [20 mg] to 44% [40 mg] versus approximate 12%) [14]. The reason for the higher percentage of AAA positivity among Japanese versus Western patients is unknown. Many of the positive samples showed low concentrations of AAA (Fig. 3b), which may explain why the overall ACR response rates are still very comparable. We could also theorize that, at some time within the 2-week dosing interval, adalimumab concentrations were sufficiently high to produce the comparable efficacy results seen in this study. Because only trough (predose) samples were tested for adalimumab concentrations, we cannot evaluate the validity of this theory within the context of this study. Increased positivity for AAA in this study can be ascribed to monotherapy of adalimumab, as concomitant usage of MTX is known to significantly decrease the incidence of anti-human chimeric antibody against infliximab [16]. The lower incidence of AAA in the 80 mg group (26.4%) in this study compared with the 20 and 40 mg groups may be explained by the higher dose of adalimumab potentially inhibiting AAA production. Moreover, the sample size in this study is smaller than the overall population of RA patients (N = 1062) in which a 5% incidence of AAA has been reported [12]. Further study of the clinical importance of AAA development is warranted.
The safety profiles of adalimumab in the two studies were similar. Minor differences in safety were reported, most notably injection-site reaction, which was reported at greater percentages in Japanese patients in all adalimumab groups (67/265; 25.3%) compared with all adalimumab dose groups in Western patients (46/434; 10.6%). Almost all injection-site reactions were considered mild in intensity and were easily manageable with conservative medical treatment.
Conclusions
Adalimumab 20, 40, and 80 mg eow led to significant improvement in signs and symptoms of RA in Japanese patients with moderate to severe RA. The greatest treatment responses occurred with the 40 and 80 mg adalimumab doses. Repeated doses of adalimumab 20, 40, and 80 mg were generally well-tolerated in Japanese patients. At the suggested adalimumab dosage in foreign countries (40 mg eow), similar efficacy, safety, and pharmacokinetic study results were obtained with Japanese patients with RA compared with results in Western patients. Only minor differences in the safety profile between all three adalimumab groups and the placebo group were reported in Japanese patients compared with Western patients, the most notable of which is injection-site reaction. Therefore, comparable ACR response rates and safety data support adalimumab 40 mg eow being the appropriate standard dosage to treat RA in Japanese patients.
Disclosure statement
N. Miyasaka is affiliated with Abbott Japan and Eisai.
References
Kvien TK. Epidemiology and burden of illness of rheumatoid arthritis. Pharmacoeconomics. 2004;22 Suppl 1:1–12.
Miyasaka N, Takeuchi T, Eguchi K. Official Japanese guidelines for the use of infliximab for rheumatoid arthritis. Mod Rheumatol. 2005;15:4–8.
Shiokawa Y. International conference for the bone and joint decade. Rheumatic diseases at the dawn of the millennium. J Rheumatol. 2003;30 Suppl 67:1–2.
Mugitani M. International conference for the bone and joint decade. Bone and joint diseases around the world. Japan: strategy for rheumatic disease control. J Rheumatol. 2003;30 Suppl 67:47.
Hakoda M, Oiwa H, Kasagi F, Masunari N, Yamada M, Suzuki G, et al. Mortality of rheumatoid arthritis in Japan: a longitudinal cohort study. Ann Rheum Dis. 2005;64:1451–5.
Elliott MJ, Maini RN, Feldmann M, Kalden JR, Antoni C, Smolen JS, et al. Randomised double-blind comparison of chimeric monoclonal antibody to tumour necrosis factor alpha (cA2) versus placebo in rheumatoid arthritis. Lancet 1994;344:1105–10.
Moreland LW, Baumgartner SW, Schiff MH, Tindall EA, Fleischmann RM, Weaver AL, et al. Treatment of rheumatoid arthritis with a recombinant human tumor necrosis factor receptor (p75)-Fc fusion protein. N Engl J Med. 1997;337:141–7.
Weinblatt ME, Keystone EC, Furst DE, Moreland LW, Weisman MH, Birbara CA, et al. Adalimumab, a fully human anti-tumor necrosis factor α monoclonal antibody, for the treatment of rheumatoid arthritis in patients taking concomitant methotrexate. Arthritis Rheum. 2003;48:35–45.
Abe T, Takeuchi T, Miyasaka N, Hashimoto H, Kondo H, Ichikawa Y, et al. A multicenter, double-blind, randomized, placebo controlled trial of infliximab combined with low dose methotrexate in Japanese patients with rheumatoid arthritis. J Rheumatol. 2006;33:37–44.
Yamanaka H, Tanaka Y, Sekiguchi N, Inoue E, Saito K, Kameda H, et al. Retrospective clinical study on the notable efficacy and related factors of infliximab therapy in a rheumatoid arthritis management group in Japan (RECONFIRM). Mod Rheumatol. 2007;17:28–32.
Miyasaka N, Takeuchi T, Eguchi K. Guidelines for the proper use of etanercept in Japan. Mod Rheumatol. 2006;16:63–7.
Prescribing Information, Humira. Abbott Laboratories, North Chicago, IL. Feb, 2007.
Furst DE, Schiff MH, Fleischmann RM, Strand V, Birbara CA, Compagnone D, et al. Adalimumab, a fully human anti tumor necrosis factor-alpha monoclonal antibody, and concomitant standard antirheumatic therapy for the treatment of rheumatoid arthritis: results of STAR (Safety Trial of Adalimumab in Rheumatoid Arthritis). J Rheumatol. 2003;30:2563–71.
Van de Putte LBA, Atkins C, Malaise M, Sany J, Russell AS, van Riel PLCM, et al. Efficacy and safety of adalimumab as monotherapy in patients with rheumatoid arthritis for whom previous disease modifying antirheumatic drug treatment has failed. Ann Rheum Dis. 2004;63:508–16.
Kashiwazaki S, Ichikawa Y, Sugawara S, et al. Determination of the clinical optimal dose of L-377 (methotrexate capsule) for the treatment of rheumatoid arthritis (in Japanese). Jpn J Inflamm. 1996;16:437–58.
Maini R, St. Clair EW, Breedveld F, Furst D, Kalden J, Weisman M, et al. Infliximab (chimeric anti–tumor necrosis factor alpha monoclonal antibody) versus placebo in rheumatoid arthritis patients receiving concomitant methotrexate: a randomized phase II trial. ATTRACT Study Group. Lancet. 1999;354:1932–9.
Burmester GR, Mariette X, Montecucco C, Monteagudo-Sáez I, Malaise M, Tzioufas AG, et al. Adalimumab alone and in combination with disease-modifying antirheumatic drugs for the treatment of rheumatoid arthritis in clinical practice: the research in active rheumatoid arthritis (ReAct) trial. Ann Rheum Dis. 2007;66:732–9.
Breedveld FC, Weisman MH, Kavanaugh AF, Cohen SB, Pavelka K, van Vollenhoven R, et al. The PREMIER study: a multicenter, randomized, double-blind clinical trial of combination therapy with adalimumab plus methotrexate versus methotrexate alone or adalimumab alone in patients with early, aggressive rheumatoid arthritis who had not had previous methotrexate treatment. Arthritis Rheum. 2006;54:26–37.
Schiff MH, Burmester GR, Kent JD, Pangan AL, Kupper H, Fitzpatrick SB, et al. Safety analyses of adalimumab (HUMIRA®) in global clinical trials and US postmarketing surveillance of patients with rheumatoid arthritis. Ann Rheum Dis. 2006;65:889–94.
Acknowledgments
This study was sponsored by Abbott Japan Co., Ltd., Osaka, Japan, and Eisai Co., Ltd., Tokyo, Japan. The authors would like to thank Michelle L. Metelo, PharmD, for her editorial assistance in the writing of this manuscript.
Author information
Authors and Affiliations
Consortia
Corresponding author
Appendices
The CHANGE study investigators
Koji Taneichi (Kitami Red Cross Hospital), Tatsuya Atsumi (Hokkaido University), Hiroki Takahashi (Sapporo Medical University), Masaya Mukai (Sapporo City General Hospital), Katsunori Onishi (Sapporo Social Insurance Hospital), Takeshi Sasaki (Tohoku University), Tomomasa Izumiyama, Akira Hatakeyama (Tohoku Rousai Hospital), Shuji Ota (Hitachi Ltd. Taga General Hospital), Takayuki Sumida (Tsukuba University), Yoshihisa Nojima (Gunma University), Seiji Minoda (Jichi Medical School), Itsuo Iwamoto, Noriaki Nakagawa (Chiba University), Ryutaro Matsumura (National Hospital Organization Chiba-East Hospital), Toshihide Mimura (Saitama Medical University), Tsutomu Takeuchi (Saitama Medical Center), Takeshi Kuroda (Niigata University), Akira Murasawa (Niigata Prefectural Rheumatic Center; Niigata Senami Hospital), Tadamasa Hanyu (Nagaoka Red Cross Hospital), Kazuhiko Yamamoto (Tokyo University), Toshihiro Nanki (Tokyo Medical and Dental University), Michito Hirakata (Keio University), Hiroshi Hashimoto, Ken Yamaji (Juntendo University), Naoyuki Kamatani (Tokyo Women’s Medical University), Hirotsugu Ide, Tsuyoshi Kasamatsu (Showa University), Shigemasa Sawada (Nihon University School of Medicine, Nerima Hikarigaoka Hospital), Takashi Yamada (Metropolitan Ohtsuka Hospital), Sigeko Inokuma (Metropolitan Komagome Hospital), Yoshiaki Kuga (Metropolitan Bokutoh Hospital), Hajime Yamagata (National Hospital Organization Murayama Medical Center), Yasuo Osone (Kawasaki Municipal Hospital), Shoichi Ozaki (St. Marianna University School of Medicine), Isao Hirose (Showa University Fujigaoka Rehabilitation Hospital), Shohei Nagaoka (Yokohama Minami Mutual Aid Association Hospital), Testuo Nishikawa (Yokohama Rousai Hospital), Shigeto Toma (National Hospital Organization Sagamihara National Hospital), Hirobumi Kondo (Kitasato University), Yasuo Suzuki (Tokai University), Taro Karahashi (Fujieda Municipal General Hospital), Seiji Tsuboi (Shizuoka Kosei Hospital), Toshiaki Miyamoto (Seirei Hamamatsu General Hospital), Shigeyuki Wakitani (Shinshu University), Toshihisa Kanamono (Nagano Red Cross Hospital), Eiji Sugiyama (Toyama Medical and Pharmaceutical University Hospital), Satoshi Nakazaki (Kamiaraya Clinic; Kanazawa Rehabilitation Hospital), Kazunori Sugimoto (Fukui General Hospital), Tetsuo Tsuji (Fukui Onsen Hospital), Naoki Ishiguro (Nagoya University), Masami Tsukamoto (National Hospital Orgnization Nagoya Medical Center), Shunji Yoshida (Fujita Health University), Takeshi Oguchi (Anjo Kosei Hospital), Takao Fujii (Kyoto University), Yutaka Kawahito (Kyoto Prefectural University), Toshiro Tanaka (Osaka University), Yukihiko Saeki (National Hospital Organization Osaka-Minami Medical Center), Shunichi Kumagai (Kobe University), Hajime Sano (Hyogo College of Medicine), Tsukasa Matsubara (Matsubara Mayflower Hospital), Masahiro Yamamura (Okayama University), Yasuhiko Yoshinaga, Akira Okamoto (National Hospital Organization Minami-Okayama Medical Center), Kenji Tani (Tokushima University), Sanpei Nakata (Matsuyama Red Cross Hospital), Kiyoshi Takasugi (Dohgo Spa Hospital), Takeshi Otsuka, Hitoshi Nakajima (Kyushu University), Eiichi Suematsu (National Hospital Organization Kyushu Medical Center), Takaaki Fukuda (Kurume University Medical Center), Katsumi Eguchi (Nagasaki University), Kazuyoshi Saito (University of Occupational and Environmental Health), Takemasa Matsuda (Kagoshima Red Cross Hospital).
Martin Kaul, MD, of Abbott GmbH & Co. KG is a co-author on this manuscript.
The committee for evaluation of efficacy and safety
Kimimasa Nakabayashi (Kyorin University), Yasuyuki Yoshizawa (Tokyo Medical and Dental University), and Takashi Harada (Tokyo Women’s Medical University Medical Center East).
Central respiratory evaluation members for chest X-ray
Yasuyuki Yoshizawa, Syuji Miyake, Naohiko Inase, Yutaka Usui, Takeshi Umino, Yuuki Sumi, Susumu Isogai, and Nobuyuki Koyama (Tokyo Medical and Dental University).
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Miyasaka, N., The CHANGE Study Investigators. Clinical investigation in highly disease-affected rheumatoid arthritis patients in Japan with adalimumab applying standard and general evaluation: the CHANGE study. Mod Rheumatol 18, 252–262 (2008). https://doi.org/10.1007/s10165-008-0045-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10165-008-0045-0