Abstract
Background
AQP2 water channel is critical for urinary concentration in the kidney. Interestingly, AQP2 is abundantly excreted in the urine as extracellular vesicles (EVs), which is known to be a useful biomarker for water-balance disorders although the character of AQP2-enriched EVs is poorly understood including water channel function.
Methods
Human urine EVs were obtained by a differential centrifugation method. AQP2-bearing EVs were isolated by immunoprecipitation with an AQP2-specific antibody, and the proteins in the EVs were analyzed by LC–MS/MS proteomic analysis. Osmotic water permeability (Pf) of the AQP2-rich EVs was measured by a stopped-flow method monitoring scattered light intensity in response to outwardly directed osmotic gradient.
Results
Sequential centrifugation of human urine showed that AQP2 was present predominantly (80%) in low-density EVs (160,000 g), whereas negligible amount in high-density EVs (17,000 g). Proteomic analysis of the AQP2-bearing EVs identified 137 proteins, mostly in the endosome pathway, including the components of ESCRT (endosomal sorting complex required transporter)-I, II, III. Pf value of the 160,000 g EVs was 4.75 ± 0.38 × 10−4 cm s−1 (mean ± SE) with the activation energy of 3.51 kcal mol−1 which was inhibited with 0.3 mM HgCl2 by 63%, suggesting a channel-mediated water transport. Moreover, Pf value showed a significant correlation with the abundance of AQP2 protein in EVs.
Conclusion
Taken together, AQP2 is localized predominantly to urinary exosomes with preserved water channel activities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aquaporin-2 (AQP2) is a key molecule that determines the urine concentrating ability of the kidney and is deeply involved in clinical water-balance disorders such as water retention in heart failure and liver cirrhosis [1, 2]. Thus, in turn, it could serve as a useful biomarker for diagnosis and prognosis of such diseases [3, 4]. Kanno et al. [5] for the first time identified the presence of AQP2 in human urine. They showed that AQP2 is present in the membrane of vesicle-like structure, and the amount of urinary AQP2 is responsive to vasopressin. However, identity and character of such vesicular structure were unclear at that time. In 2004, Pisitkun et al. reported that there are vesicles in the urine whose characteristics are consistent with exosomes and AQP2 is present in those vesicles, resolving the mystery [6].
The exosomes, a subset of extracellular vesicles are derived from the multiple vesicular body and have characters of small size (< 100 nm) and a unique orientation of “cytosolic side inward”. Recent progress in this field shows that urine extracellular vesicles (EVs) are composed of several different subsets of vesicles including exosomes, microvesicles (ectosomes), apoptotic bodies and others [7, 8]. The differences of the subclasses are conceptually clear, but it is practically difficult to differentiate them because they share their characteristics such as sizes, shapes and specific markers [9]. Therefore, more detailed studies on the character of AQP2-rich urine EVs are necessary before applying urine AQP2 for a biomarker of water homeostasis. It is also unknown whether AQP2 in urine EVs preserves its water channel function, and thus has any functional roles in the kidney–urological organs. In this study, we examined the proteome of immunoprecipitated AQP2-bearing EVs and directly measured the osmotic water permeability of AQP2-rich EVs by a stopped-flow method.
Materials and methods
EVs preparation
Urine EVs were prepared from healthy subjects by an ultracentrifugation method [10]. In brief, urine samples were centrifuged at 3000×g for 15 min at 25 °C to remove sediments, cells, and cell debris. Then, the supernatants were centrifuged at 17,000×g for 15 min at 25 °C to remove the larger vesicles (> 100 nm) and high-density membrane fractions. The supernatant was finally ultracentrifuged at 160,000 or 200,000×g for 1 h at 25 °C to collect the smaller (< 100 nm) and low-density membrane fraction. The pellets were suspended in phosphate buffered saline (PBS) for further analysis.
ELISA measurements of urine AQP2 samples
Amount of AQP2 protein in urine and EVs samples were measured by a sandwich enzyme linked immunosorbent assay (ELISA) method as previously reported [11, 12]. The samples were pre-treated with alkali (0.3N NaOH for 20 min) before the assay to disrupt EVs membranes [12, 13]. This procedure is critically necessary because the epitopes of AQP2 antibodies face toward the inside of EVs and cannot react with the antibodies.
Proteomic analysis of AQP2-bearing EVs
AQP2-bearing EVs were obtained by co-immunoprecipitation with AQP2 antibody [5]. Briefly, the urine 160,000 g pellets (see above) were stored at − 30 °C for more than 1 week and freeze–thaw were applied to disrupt EVs membranes [12, 13]. The thawed samples were reacted with AQP2 antibody-coated magnet beads following the manufacturer’s instructions (Dynabeads Co-Immunoprecipitation Kit, Novex, Lifetechnologies, Oslo, Norway). Immunoprecipitated EVs were digested with trypsin in solution. Tryptic peptides were purified by MonoSpin column (GL Sciences, Tokyo, Japan) and analyzed twice by LC–MS/MS (EASY-nanoLC-Fusion Orbitrap, Thermo Fisher Scientific, 115 min gradient method). The proteins were identified by a search engine Mascot (Matrix Science) with following search parameters; peptide mass tolerance: ± 5 ppm, fragment mass tolerance: ± 0.6 Da, max missed cleavages: 2, false discovery rate: <1%, protein database: Uniprot–Swissprot (n = 150,811). Non-labeled quantification was made by normalized spectral index (SIN) values. The identified proteins were annotated by KEGG pathway analysis of DAVID Bioinformatics Resources (NIAID, NIH) [14].
Osmotic water permeability
The osmotic water permeability coefficient (Pf) of EVs was measured by a stopped-flow technique (Stopped Flow Rapid Scan Spectroscopy, RSP-2000, UNISOKU, Osaka). The 160,000×g pellets (see above) were suspended in PBS and the protein concentration of EVs samples was adjusted to 150 µg ml−1 with PBS. The kinetics of volume changes to a rapid inwardly directed osmotic gradient with glycerol were measured by the 90° scattered light intensity of 530 nm at 25 °C until the signal reached a plateau. Pf was calculated using the following equation:
where S/V0 is cell surface-to-volume ratio, Vw is the molar volume of water (18 cm−3 mol−1), (Cin–Cout) is the initial osmotic gradient, d(V/V0)/dt is the initial rate of relative cell volume change determined by the initial slope of light scattering vs. time data upon the osmotic gradient after the calibration between scattered light intensity and cell volume [15, 16]. Mean EVs volume in an isotonic condition was calculated based on mean diameter of EVs which was measured by electron microscope (EM) as described previously [13]. The mean diameter of EVs was 45.9 ± 14.6 nm (mean ± SE, n = 120). To examine the effect of an inhibitor against water channels, HgCl2 was applied to the EVs samples to a final concentration of 0.3 mM 10 min before the Pf measurements. As a negative control, EVs membranes were disrupted by sonication with repeated cycles of on/off 10 s for 5 min on ice. To determine the activation energy (Ea), Pf values were measured at three different temperatures, 4, 25 and 37 °C. Ea was calculated by the slope of the Arrhenius plot as the following equation:
Ea = − [slope × R], where R is the gas constant (1.987 kcal mol−1 K−1). The slope was determined by linear regression analysis [17].
The osmolality of urine samples was measured by a freezing-point osmometer (Micro-Osmometer, Model 210, Fiske, USA). Data were shown as the mean ± SE and statistical differences were determined by non-paired t-test. The CORREL function in Excel (Microsoft ver.15.32) was used to find the correlation coefficient between two variables. p values < 0.05 were considered significant in all statistical analyses.
All healthy normal volunteers who provided urine samples gave written informed consent and the protocol was approved by the Institutional Ethical Committee (Meiji Pharmaceutical University #2609).
Results
Amount of AQP2 in EVs fractions
One of the keys to speculate the nature of AQP-2-rich EVs is to determine the urine centrifugation fractions where AQP2 is enriched. Human urine samples (n = 5) were differentially centrifuged and AQP2 concentration was sequentially measured by ELISA in the original urine, and the each supernatant after 3000, 17,000, and 200,000×g. The mean AQP2 concentration of the urine was 3.32 ± 0.53 ng ml−1 ranging from 1.92 to 4.80 ng ml−1. The AQP2 concentration in the supernatants after various centrifugation procedures decreased slightly by 13.1 and 15.1% after 3000 and 17,000×g centrifugation, respectively (Fig. 1). The minimal decrease of AQP2 concentration from 3000 to 17,000×g indicated that AQP2 was not sedimented in the larger vesicles. On the other hand, AQP2 concentration in the supernatant after 200,000×g was 4.5 ± 4.0% of the urinary value, indicating that the most of AQP2 (80%) in the urine was sedimented in the smaller vesicles, which is consistent with exosomes (Fig. 1). In the separate study, AQP2 concentration in the supernatants after 160,000×g centrifugation was 8.0 ± 2.2% of the urine (n = 4), indicating a similar sedimentation efficacy of AQP2 in 160,000 and 200,000×g centrifugations.
AQP2 concentrations in the original urine and the supernatants after successive centrifugations. Urine samples (n = 5) were successively centrifuged at 3000×g 15 min, 17,000×g 15 min, 200,000×g 60 min and AQP2 concentration was measured in the original urine and supernatants. The AQP2 concentration decreased to 86.9 ± 5.1 and 84.9 ± 8.6% of the original urine after 3000×g and 17,000×g centrifugation, respectively. AQP2 concentration of the supernatant after 200,000×g was 4.5 ± 4.0% of the original urine
Proteomic analysis of EVs immunoprecipitated with AQP2 antibody
AQP2-bearing EVs were separated by co-immunoprecipitation (CO-IP) with an AQP2 antibody from the 160,000 g EVs. Before the CO-IP, these 160,000 g EVs were also analyzed by LC–MS/MS and a total of 1299 proteins were identified. The KEGG pathway analysis showed the prevalence of these proteins in metabolic (12.0%), endocytosis (6.2%), biosynthesis (4.3%), phagosome (3.9%), regulation of actin cytoskeleton (3.7%), and lysosome (2.5%) pathways. These compositions were very similar to the previously deposited database of human urine exosomes (a total of 1160 proteins, Gonzales et al. [18], https://hpcwebapps.cit.nih.gov/ESBL/Database/Exosome/). Thus, our starting materials were human urine so-called “exosome”, although this fraction is known to contain other EVs subclasses.
The MS analysis of the co-immunoprecipitated EVs with our human AQP2 antibody identified 137 proteins. Top 20 of the proteins are shown in a rank order of the normalized spectral index (SIN) in Table 1, and all proteins are listed in the Supplement.
To check whether our CO-IP procedure correctly immunoprecipitated AQP2-bearing EVs, the immuno-localization of these 137 proteins were searched using a public database (The Human Protein Atlas; http://www.proteinatlas.org). Of 137 proteins, 103 proteins are reported to be expressed in kidney collecting ducts by immunohistochemistry, indicating that our CO-IP successfully isolated EVs derived from collecting ducts where AQP2 is selectively expressed. Table 1 also shows the results of this analysis and indicated that 18 out of the top 20 proteins were derived from collecting ducts.
The pathway analysis (KEGG) of the obtained 137 proteins indicated many proteins in the endocytosis pathway (19.1%) followed by MAPK signaling pathway (5.9%) and others (Table 2).
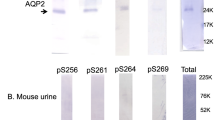
The proteins in endocytosis pathway were components of ESCRT (endosomal sorting complex required transporter); ESCRT-I, II, III, Alix (PDCD61P), TSG101, multivesicular body proteins, heat shock proteins, vacuolar sorting proteins and others. Figure 2 shows the location of these proteins inside the cell, clearly indicating that most of the co-immunoprecipitated EVs were from multivesicular bodies which produce exosomes. On the other hand, none of the proteins reported to be associated microvesicles/ectosomes such as ARF6, VAMP3, TyA, C1q, BSG, β1 integrin and MMP2 [7, 9] were identified.
The intracellular localization of the identified proteins in AQP2-bearing EVs that are annotated as endocytosis pathway by the KEGG analysis. The figure was modified from the data provided KEGG [14]. Gene names shown in red were observed in this analysis
Osmotic water permeability of EVs
The intensity of the scattered light from the 160,000 g EVs was traced after rapid application of inwardly directed 500 mOsm kg−1 H2O osmotic gradient with glycerol. The summated traces (3–13 times) are shown in Fig. 3. The light intensities rapidly increased reflecting the volume decrease of EVs after the rapid osmotic challenge. The calculated Pf value was 4.75 ± 0.38 × 10−4 cm s−1 (n = 17) for the control EVs. The incubation of EVs with 0.3 mM HgCl2, an inhibitor of aquaporins, for 10 min at room temperature before measurements suppressed the Pf by 63% to 1.76 ± 0.39 × 10−4 cm s−1 (n = 5, p < 0.05 compared to the control). When EVs were pre-treated with sonication to mechanically disrupt the membranes, an unchanged stable signal of scattered light was observed, indicating the absence of shape change in the absence of intact membrane (Fig. 3). The activation energy (Ea) value determined from the Arrhenius plot of Pf was 3.51 kcal mol−1 (Fig. 4), a value consistent with the water flow through water channel. In five EVs samples, the relationship between the Pf values and the AQP2 contents was analyzed and a strong positive correlation was observed (r = 0.948, p < 0.014) (Fig. 5a). Moreover, a positive correlation was also observed between the Pf values and the urine osmolality (r = 0.879, p < 0.049) (Fig. 5b). Therefore, we concluded that the observed Pf mostly reflected the activity of AQP2.
Osmotic water permeability of human urine EVs measured by the stopped-flow light scattering technique. Urine sample was centrifuged at 160,000g and suspended in PBS. EVs were subjected to a 500 mM inwardly directed gradient of glycerol and scattered light intensity was recorded (Control). The recording was also made after treatment of 0.3 mM HgCl2 (HgCl2) or membrane disruption by sonication (Sonication). Each trace was a summation of various experiments (4–17)
Arrhenius plot of the temperature dependency of Pf. The activation energy (Ea) was calculated from the slope of the regression line between temperature−1 and natural log of the late constant of osmotic water flow (Ln k). Pf was measured at 4 (n = 4), 25 (n = 17) and 37 °C (n = 5). The Pearson’s correlation coefficient was used to assess the correlation between temperature−1 and Ln
a The relationship between the Pf values and the AQP2 concentrations in the EVs. In each EVs sample (n = 5) Pf was measured by the stopped-flow technique and AQP2 concentration was measured by ELISA. b The relationship between Pf values and the urine osmolality. The Pf values were compared to the osmolality of the original urine from which EVs were prepared.
Discussion
This is the first report on the proteomic analysis of AQP2-bearing urinary EVs. The important, but easily overlooked technical issue is that disruption of vesicle membrane is necessary before CO-IP with AQP2 antibodies. Otherwise, AQP2 antibodies (epitopes face inward vesicles) cannot catch AQP2-bearing vesicles. We stored the EVs samples more than 1 week at − 30 °C and freeze and thaw was applied to accelerate the disruption [12, 13]. Abundant presence of components of ESCRT-I, II, III (Table 2; Fig. 2) strongly indicates that urinary AQP2 vesicles are derived from the late endosome and multivesicular body, which produces exosomes with caveat that ESCRT proteins are also present in microvesicles [19].
Enrichment of AQP2 in the ultracentrifugation (160,000–200,000×g) EVs up to 80% of the urine (Fig. 1) also supports the conclusion that AQP2-rich EVs are exosomes as the smaller vesicles less than 100 nm (exosomes) are usually sedimented in this fraction while the larger vesicles more than 100 nm (microvesicles) and dense membrane vesicles (apoptotic vesicles) are likely sedimented at 17,000×g fraction, although the presence of microvesicles less than 100 nm is known [7]. Wen et al. [20] reported that 96.7% of urine AQP2 was sedimented at 200,000×g in rat urine using semi-quantitative Western blot analysis, although this study did not analyze the 10,000–20,000×g fraction. To quantify urine AQP2, our ELISA should be superior as it is highly sensitive (50 µl sample) without centrifugation or concentration procedures.
This is also the first report on the measurement of the Pf in the EVs. The value obtained (4.75 × 10−4 cm s−1) was much smaller than the values reported for kidney proximal tubule brush border membrane vesicles and erythrocytes (~ 100 × 10−4 cm s−1) [17, 21]. The reasons for this discrepancy can be multifold. First, the size of EVs (diameter; 46 nm) may be too small to measure Pf by light scattering method with rapid and weak signals for volume changes. Second, similarly a larger surface-to-volume ratio of EVs may produce a higher background water permeability to diminish the effect of water channel at the initiation of volume change. Third, a very high content of cholesterol in urine exosomes (63% of total lipid) may have minimized Pf of urine EVs cancelling the water channel activity [22] as a higher cholesterol content in lipid membranes greatly attenuates Pf [23]. Finally, a much lower amount of AQPs in EVs may also be responsible for the low Pf value.
Despite the lower Pf of EVs, however, the Pf of EVs was inhibited by HgCl2, a commonly used inhibitor of AQPs, and completely by their ultrasonic treatment. Furthermore, its activation energy was as low as 3.51 kcal mol−1, which strongly argues for a channel-mediated water transport [24]. Thus, urinary EVs most likely conserve the function of a water channel although their lower Pf values may need further studies.
Among AQP family members, only AQP1, AQP2 and AQP7 have been reported in urine exosomes [18, 25]. As the Pf values of EVs were correlated with the amount of AQP2 in the EVs (Fig. 5a), the observed water channel activity was most likely due to AQP2. Moreover, the Pf values of EVs were also correlated with the urine osmolality (Fig. 5b), which further suggested the involvement of AQP2 as urinary AQP2 excretion is dependent on urine osmolality and vasopressin [11, 25, 26] while the expression of AQP1 is constitutive and not influenced by the urine concentration [20].
Several membrane transport proteins (channels and transporters; such as NCC, NKCC2, SGLT1,2 and ENaC) have been reported to be present in EVs [18, 27]. However, none of them have been examined for their functions directly. In this context, Street et al. [28] reported an indirect result on the function of AQP2 in EVs. They cultured the endogenously AQP2-expressing epithelial cells and showed that the EVs obtained from the medium of vasopressin-stimulated cells induced increased water permeability of the recipient culture cells. The results seemed to be caused by the transfer of preserved water channels from exosomes. However, it is also possible that the transmission of AQP2 mRNA from donor culture cells to be transcribed in the recipient culture cells. Therefore, our direct results of the preserved AQP2 function in EVs will be important to extrapolate to other membrane proteins and will be helpful to speculate the roles of membrane proteins in urinary EVs in the physiology and pathophysiology of the kidney.
References
Sasaki S. Aquaporins 2: from its discovery to molecular structure and medical implications. Mol Aspects Med. 2012;33:535–46.
Radin MJ, Yu MJ, Stoedkilde L, Miller RL, Hoffert JD, Frokiaer J, Pisitkun T, Knepper MA. Aquaporin-2 regulation in health and disease. Vet Clin Pathol. 2012;41:455 – 70.
Imamura T, Kinugawa K. Urine aquaporin-2: a promising marker of response to the arginine vasopressin type-2 antagonist, Tolvaptan in patients with congestive heart failure. Int J Mol Sci. 2016;14:17.
Nakanishi H, Kurosaki M, Hosokawa T, Takahashi Y, Itakura J, Suzuki S, Yasui Y, Tamaki N, Nakakuki N, Takada H, Higuchi M, Komiyama Y, Yoshida T, Takaura K, Hayashi T, Kuwabara K, Sasaki S, Izumi N. Urinary excretion of the water channel aquaporin 2 correlated with the pharmacological effect of tolvaptan in cirrhotic patients with ascites. J Gastroenterol. 2016;51:620–7.
Kanno K, Sasaki S, Hirata Y, Ishikawa S, Fushimi K, Nakanishi S, Bichet DG, Marumo F. Urinary excretion of aquaporin-2 in patients with diabetes insipidus. N Engl J Med. 1995;332:1540–5.
Pisitkun T, Shen RF, Knepper MA. Identification and proteomic profiling of exosomes in human urine. Proc Natl Acad Sci USA. 2004;101:13368–73.
Théry C, Ostrowski M, Segura E. Membrane vesicles as conveyors of immune responses. Nat Rev Immunol. 2009;9:581 – 93.
van der Pol E, Böing AN, Harrison P, Sturk A, Nieuwland R. Classification, functions, and clinical relevance of extracellular vesicles. Pharmacol Rev. 2012;64:676–705.
Cocucci E, Meldolesi J. Ectosomes and exosomes: shedding the confusion between extracellular vesicles. Trends Cell Biol. 2015;25:364–72.
Zhou H, Yuen PS, Pisitkun T, Gonzales PA, Yasuda H, Dear JW, Gross P, Knepper MA, Star RA. Collection, storage, preservation, and normalization of human urinary exosomes for biomarker discovery. Kidney Int. 2006;69:1471–6.
Sasaki S, Ohmoto Y, Mori T, Iwata F, Muraguchi M. Daily variance of urinary excretion of AQP2 determined by sandwich ELISA method. Clin Exp Nephrol. 2012;16:406–10.
Sasaki S, Saijo Y, Ohmoto Y, Iwata F, Koga D, Katsuragi K. Alkali treatment stabilizes fluctuations of urine AQP2 values measured by ELISA. Clin Exp Nephrol. 2016;20:450–5.
Nameta M, Saijo Y, Ohmoto Y, Katsuragi K, Yamamoto K, Yamamoto K, Ishibashi K, Sasaki S. Disruption of membranes of extracellular vesicles is necessary for ELISA determination of urine AQP2: proof of disruption and epitopes of AQP2 antibodies. Int J Mol Sci. 2016;17:1634.
Zhong H, Yang X, Kaplan LM, Molony C, Schadt EE. Integrating pathway analysis and genetics of gene expression for genome-wide association studies. Am J Hum Genet. 2010;86:581–91.
Selser JC, Yeh Y, Baskin RJ. A light-scattering characterization of membrane vesicles. Biophys J. 1976;16:337–56.
Echevarria M, Verkman AS. Optical measurement of osmotic water transport in cultured cells. Role of glucose transporters. J Gen Physiol. 1992;99:573–89.
Meyer MM, Verkman AS. Evidence for water channels in renal proximal tubule cell membranes. J Membr Biol. 1987;96:107–19.
Gonzales PA, Pisitkun T, Hoffert JD, Tchapyjnikov D, Star RA, Kleta R, Wang NS, Knepper MA. Large-scale proteomics and phosphoproteomics of urinary exosomes. J Am Soc Nephrol. 2009;20:363–79.
Nabhan JF, Hu R, Oh RS, Cohen SN, Lu Q. Formation and release of arrestin domain-containing protein 1-mediated microvesicles (ARMMs) at plasma membrane by recruitment of TSG101 protein. Proc Natl Acad Sci USA. 2012;109:4146–51.
Wen H, Frokiaer J, Kwon TH, Nielsen S. Urinary excretion of aquaporin-2 in rat is mediated by a vasopressin-dependent apical pathway. J Am Soc Nephrol. 1999;10:1416–29.
Verkman AS, van Hoek AN, Ma T, Frigeri A, Skach WR, Mitra A, Tamarappoo BK, Farinas J. Water transport across mammalian cell membranes. Am J Physiol. 1996;270:C12–30.
Skotland T, Sandvig K, Llorente A. Lipids in exosomes: current knowledge and the way forward. Prog Lipid Res. 2017;66:30–41.
Finkelstein A, Cass A. Effect of cholesterol on the water permeability of thin lipid membranes. Nature. 1967;216:717–8.
Verkman AS. Mechanisms and regulation of water permeability in renal epithelia. Am J Physiol. 1989;257:C837-C850.
Oshikawa S, Sonoda H, Ikeda M. Aquaporins in urinary extracellular vesicles (exosomes). Int J Mol Sci. 2016;17:E957.
Elliot S, Goldsmith P, Knepper M, Haughey M, Olson B. Urinary excretion of aquaporin-2 in humans: a potential marker of collecting duct responsiveness to vasopressin. J Am Soc Nephrol. 1996;7:403–9.
Isobe K, Mori T, Asano T, Kawaguchi H, Nonoyama S, Kumagai N, Kamada F, Morimoto T, Hayashi M, Sohara E, Rai T, Sasaki S, Uchida S. Development of enzyme-linked immunosorbent assays for urinary thiazide-sensitive Na-Cl cotransporter measurement. Am J Physiol Renal Physiol. 2013;305:F1374–F1381.
Street JM, Birkhoff W, Menzies RI, Webb DJ, Bailey MA, Dear JW. Exosomal transmission of functional aquaporin 2 in kidney cortical collecting duct cells. J Physiol. 2011;589:6119–27.
Acknowledgements
This study was in part supported by a grant-in-aid from the Ministry of Health, Labor and Welfare, Japan, and from the Japan Society for the Promotion of the Science (KAKENHI 15K09301 to S.S. and 15K09302 to K.I.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institution Ethical Committee of Meiji Pharmaceutical University (the approved no. 2609) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10157_2018_1538_MOESM1_ESM.xlsx
Supplement. A list of 137 proteins that were identified in AQP2-bearing EVs. Their SIN values and the presence/absence in collecting duct cells are summarized. NE means “not examined”. (XLSX 15 KB)
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Miyazawa, Y., Mikami, S., Yamamoto, K. et al. AQP2 in human urine is predominantly localized to exosomes with preserved water channel activities. Clin Exp Nephrol 22, 782–788 (2018). https://doi.org/10.1007/s10157-018-1538-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-018-1538-6