Abstract
Aneurysms with a major diameter > 25 mm are defined as giant intracranial aneurysms (GIAs). Different clinical, pathological, and radiological factors were revealed as playing a role in choosing the best strategy between surgical and endovascular approaches. Despite the improvement of both techniques, the efficacy and safety of these different management are still debated. We evaluated the differences in clinical and radiological outcomes of GIAs treated with surgical and endovascular techniques in a large retrospective mono-centric study. We compared aneurysm location, clinical, morphological features, treatment outcome, and complications on the ground of treatment technique. The final cohort consisted of 162 patients. All the patients were assigned on the ground of the type of eligible treatment: surgical (118 patients) and endovascular procedure (44 patients). The different treatment strategies were made through a multidisciplinary selection whereas clinical parameters, location, and morphologic features of the aneurysm were considered. The surgical group manifested a greater reduction in performance levels and neurological status in the post-operative phases than the endovascular group (p < 0.01) with a higher incidence of complications (p = 0.012) in contrast to a lower recurrence rate (p > 0.01). There is no significant difference in post-operative mortality and survival between surgical and endovascular groups. The surgical group manifested a higher incidence of complications after treatment. The endovascular group has a better post-operative outcome, but a higher risk of recurrence and the necessity of further treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Giant intracranial aneurysms (GIA) are vascular lesions whose diameter is greater than 25 mm 1. This uncommon type of lesion represent 5% of all cerebral aneurysms and most frequently involve females in the fifth and seventh decade of life [1, 2]. The natural history of GIAs is characterized by progressive growth, thrombosis, and a high risk of rupture [3, 4]. Clinical presentation of GIA is heterogeneous: 65–85% of patients present with mass effect-related symptoms, 25–35% with subarachnoid hemorrhages (SAHs), ischemic symptoms or stroke, and seizures [5]. If left untreated, mortality rates in patients harboring GIA are around 68–100% at 2 years [6], with an annual risk of rupture around 8–10% [7–11].
These high mortality rates support the indication to treat patients with GIAs to exclude the lesion from the circulation while preserving distal blood flow [12]; although high risks in treatment are recognized, prognostic factors are not precisely known, and there are no specific treatment recommendations for this particular subtype of aneurysm.
Several clinical, pathological, and radiological factors have been assumed to choose the best therapeutic strategy between the surgical and endovascular approaches for GIAs.
From a surgical perspective, different old and new micro neurosurgical techniques are available. We just know a general surgical mortality rate for the treatment of both ruptured and unruptured GIAs that varies between 6 and 22% [10–12].
On the other hand, despite the improvement of endovascular techniques, the efficacy and safety of reconstructive and deconstructive techniques are still not well defined. The appropriateness of treatment is decided on a case-by-case basis considering the high risk of complications and/or recurrence (re-canalization) of the aneurysm [2].
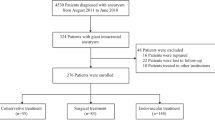
We performed an institutional retrospective review of all patients undergoing treatment for GIA between January 1990 and December 2018 at the Department of Human Neuroscience, Neurosurgical and Neuroradiological Units of Sapienza University in Rome, Italy. The study illustrates our experience with the therapeutic management of GIAs by reporting intra-procedural and delayed complication rates and anatomic and clinical outcomes, concerning treatment modality and vascular characteristics, and highlighting the main elements to consider when considering deciding how to treat this uncommon type of aneurysm.
Methods
Patient selection and eligibility
We evaluated all patients with radiological diagnoses of GIA referred to our departments. All patients included in this study met the inclusion and exclusion criteria reported in Table 1; we collected patient demographics, clinical debut, rupture and configuration of GIAs, treatment modality, and outcome. Digital subtraction angiography (DSA), magnetic resonance imaging (MRI), computed tomographic (CT) and computed tomography angiography (CTA), and outpatient clinical data were analyzed independently by a neuroradiologist (M.I) and a neurosurgeon (F.P.).
We retrieved morphological aneurysm characteristics based on vascular origin of the GIA, neck dimension and characteristics, the dome shape and presence of thrombosis.
Patients underwent to a pre-operative protocol of study imaging and selection data reported in repository data of this manuscript.
Clinical follow-up was performed by interventional neuroradiologists (M.I. and C.C.) and neurosurgeons (D.A. and F.P.), depending on the treatment technique. Clinical letters and telephonic questionnaires were used to determine pre-and post-operative functional status, surgical status, and complication rates.
Treatment
The goal of the procedures was to exclude the aneurysm from the brain circulation and decompress the nervous structures involved by the dome.
The decision of whether treatment with a micro-neurosurgical rather than endovascular approach was tailored for any patients after a multidisciplinary evaluation with a neuro-interventional radiologist and a neuro-anaesthesiologist considering different variables: aneurysm’s location and morphology of dome and neck, pre-existing pathologies, clinical status (based on Hunt Hess, HH scale and ASA physical status classification system, ASA score), symptoms, and patient’s preference. In general, the patient was not considered eligible to undergo a microsurgical approach in case of massive SAH (with HH grading of 4–5), anesthesiological solid contraindication, and involvement of subtentorial compartments.
Surgical procedure
In the surgical cohort (group A), the primary treatment strategy was direct aneurysm neck clipping before thrombectomy, clip reconstruction, or combination with a revascularization surgery. Indirect aneurysm occlusion was performed as an alternative treatment strategy when direct neck clipping was not achievable.
Direct aneurysm clipping was defined as feasible after pre-operative imaging evaluation based on a wide neck or high calcified/absence of a proper neck. We also considered the relationship between the neck and efferent vessels and the location, shape, and fusiform parent artery dilatation. Another essential step for surgical strategy is the tolerance of the balloon occlusion test (BOT). BOT consisted of mechanical occlusion of the cervical portion of the ICA performing clinical observation, and electroencephalographic registration for 30 min. The test was immediately suspended when any neurologic deficit or EEG abnormality was detected.
Three different indirect surgical strategies were performed: (1) trapping of the GIA by distal and proximal occlusion when good collateral blood supply existed in wide-neck GIAs; for those without enough collaterals, a combined revascularization/clipping strategy was performed; (2) proximal occlusion of the cervical ICA if the BOT was tolerated without symptoms; if not, a combined revascularization/clipping strategy was performed; (3) bypass strategy alone. The bypass strategy included the external carotid artery-to-ICA (ECA-ICA) bypass or intracranial internal carotid artery bypass (ICA-ICA). Preferentially GIAs without a recognized neck were submitted to bypass. Only the patients who did not tolerate the pre-operative BOT underwent an ECA-ICA bypass with a spontaneous or an angiographic closure of the ICA within 2 weeks after surgery (staged revascularization) [13, 14].
Exceptions in our series are strongly dependent on intraoperative flowmetry after its introduction in 2001 and the use of a post-operative occlusion test of the ICA.
The staged revascularization strategy included a post-operative occlusion test of the ICA to evaluate the patency of the graft. It confirmed the clinical adaptation of the patient to the new intracranial hemodynamic condition. For all the patients treated microsurgically after 1997, BOT was performed intraoperatively, closing in order the ICA, ECA, and common carotid artery for 15 min during EEG recording to evaluate if the use of the ECA (BOT non-tolerated) or the ICA (BOT tolerated) as donor’s vessel. In the case of ECA-ICA bypass, the ICA was closed intraoperatively after verifying graft patency with intraoperative angiography (single-stage combined revascularization) until 2001 or intraoperative flowmeter (transonic system, Inc., Ithaca, NY) from 2001. In any surgically treated case, intraoperative electrophysiological monitoring (PESS and PEM) was routinely used, intraoperative Doppler ultrasonography, and indo-cyanine green (ICG) fluorescence.
Endovascular procedure
Endovascular treatment of giant cerebral aneurysms has changed significantly during the last decades as many new technological advances were introduced:
Vessel sacrifice with balloon test occlusion
Proximal occlusion of GIAs via endovascular parent vessel sacrifice is feasible when appropriate collateral circulation exists proved by BOT. To avoid recurrences, it is essential to have complete occlusion of the neck of the aneurysm to exclude the possibility of recanalization through collaterals activation, like in posterior communicating artery aneurysms. However, patients who pass BOT still have a 5–25% risk of ischemic stroke after parent vessel sacrifice secondary to hemodynamic and thromboembolic causes [15]. We generally recommend the vessel sacrifice for an older patient who tolerates BOT and compressive symptoms well.
Coil-assisted embolization
Coil embolization alone for unrupted GIAs is no longer an acceptable strategy for their management. This technique is associated with significantly high re-treatment rates. Re-canalization is highest in the setting of wide residual aneurysm necks, mainly due to coils compaction, growing residual aneurysm neck, and refilling fundus [16, 17]. Moreover, the necessity of dual antiplatelet therapy limits the use of these devices in the acute setting. We reserved treatment with coiling alone to the few patients (6 patients, 13.6%) with severe contraindication to surgery but who displayed a good health status without SAH, with supratentorial GIA with the presence of neck in the absence of apparent thrombosis. Coil embolization was assisted by a vascular reconstruction device, such as Neuroform Atlas Stent (Stryker Neurovascular, Fremont, California, USA) or Low-profile Visualised Intraluminal Support (LVIS; Microvention, Tustin, California, USA); these were designed to augment coil embolizations of wide-neck aneurysms. Both LVIS Jr and Neuroform Atlas stents provide low-profile advantages with delivery through a 0.017-inch microcatheter. Open cells stent could be used in a Y- or X-stent configuration to maximize the coils packing density.
Flow diversion embolization
In this series, the Pipeline Embolisation Device (PED; Medtronic Neurovascular, Irvine, California, USA), Silk (Balt, Montmercy, France), The Flow Re-Direction Endoluminal Device (FRED, Microvention, Tustin, California, USA), and Derivo flow diverter (Acandis Pforzheim Germany) were used. They have been used alone or in combination with coiling. This is to minimize the risk of post-procedural aneurysmal rupture. All the patients treated with flow diverter (FD) receive 5 days of dual antiplatelet therapy before the intervention. The necessity of dual antiplatelet therapy limits the use of these devices in the acute setting.
We usually provide a staged treatment for ruptured GIAs with SAH, coiling in the acute phase, and flow diverter treatment following recovery from SAH. This plan is safe and effective, as demonstrated in a recent series [18], where no cases of re-bleeding occurred during the interval between coiling and flow diversion. Carotid or vertebral artery occlusion in the acute phase of SAH cannot be recommended because vasospasm may develop, and ischemic events may be aggravated by diminished reserve capacity after occlusion of the artery.
Statistical methods
The sample was analyzed with SPSS version 18. A comparison between ordinal and nominal variables was made with the ANOVA test, and a comparison between two nominal variables was created with the Chi2 test. Pre-operative and post-operative study outcomes were examined with analysis of variance and repeated measures general linear models adjusted for age and sex. Analyses were based on 2-sided tests with values of p < 0.05 considered significant with Bonferroni correction when appropriate. Data reported in the study have been completely anonymized. No treatment randomization has been performed. This work is part of a retrospective arm of a study approved by our institution’s ethics committee with number IRB 6168 Prot. 0935/2020. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration. This article does not contain any studies with animals performed by any of the authors. Informed consent was obtained from all individual participants included in the study.
Results
The clinical, radiographic characteristics, treatment methods, and outcomes of our GIAs series are summarised in Tables 2, 3, 4. The final cohort consisted of 162 patients (Table 2). Of these patients, 99 were females (61.1%) and 63 males (38.9%). The sample age showed a normal distribution after applying the Lilliefors correction with a mean age of 49.53 years old (median 51, SD 14.07); the treatment modality was for 118 patients (72.8%) a surgery, and 44 (27.2%) performed an operative DSA.
Analysis of groups
All the patients who met the inclusion mentioned above and exclusion criteria were assigned on the ground of treatment: surgical or endovascular procedure (respectively group A and group B). Group A consisted of 118 patients (mean age: 47.87 years, range 18–72); group B consisted of 44 patients (mean age 53.98 years, range 10–86). The average age was found to be comparable between the two test groups. The morphological and clinical characteristics of the two different groups analyzed are presented in Table 3.
The choice to treat a GIA by the endovascular route rather than transcranial surgery was made through a multidisciplinary discussion. In contrast, clinical parameters, location, and morphologic features of the aneurysm were considered. We recognized that the endovascular strategy was the best treatment modality for posterior circulation GIAs, selected in the most of cases as first choice.
The second factor on which the choice was based was the clinical parameters: GIA with acute clinical onset as symptomatology related to endocranial hypertension, ESA (28 pts (23.7%) vs. 5 pts (11.4%), p = 0.06), seizure (12 pts (10.2%) vs. 0% p = 0.02), and ischemia (17 pts (14.4%) vs. 0%, p = 0.03) with pre-operative MRS more impaired (p = 0.01) from the functional and performance point of view, were more frequently selected for endovascular treatment (details in Table 3).
In anterior healthy GIAs, aneurysms with unidentifiable necks, with necks less than 4 mm in size, or calcified necks were more frequently selected for surgery (p = 0.01).
The presence of endoaneurysmal thrombosis appears to be no significantly distributed among the selected procedures (group A, < 50% = 34–28.8%; > 50% = 2–1.7; no thrombosis = 84–71.2% group B, < 50% = 12–27.3%; > 50% = 2–4.5%; no thrombosis = 32–72.7% p = 0.51 p = 0.3 p = 0.51 respectively). This variable was taking in account for the selection of appropriate endovascular treatment.
Angiographic and clinical outcomes
In general, there is a significant correlation between survival and the location of GIAs. More favorable localizations are identified for aneurysms originating from MCA, AcoA, and carotid bifurcation (p = 0.01, Fig. 1).
The bar graph of the ANOVA study shows the outcome difference on the ground of GIA’s aneurysm site. The bars show the percentages of cases in which a better clinical outcome was obtained, showing a significant difference in patients in which the GIA was localized at the MCA, the bifurcation of ICA, and at the AcoA complex
Observing the prospective outcome in patients shows that there is no significant difference in post-operative mortality (in the first 24–48 h) between the two groups (p = 0.73); in the individual outcome measures, it seems there is higher mortality found in the first 30 days after the procedure in the endovascular group; at the last evaluation, the difference in overall survival is not significant (p = 0.616, Fig. 2A).
Group A manifested a more significant reduction in performance levels and neurological status in the post-operative phases than group B (p < 0.001); this finding is confirmed in part by the higher incidence of complications at the last evaluation (respectively p = 0.01 and p = 0.02 Fig. 2B) in the surgical series than in the endovascular series.
From an outcome perspective, it is interesting to note the presence of a lower rate of aneurysm recurrence (intended as re-canalization of dome) in the surgical group compared with the endovascular group (p < 0.01 Fig. 3).
Analyzing the different rates of recurrence, complications, and mortality, no significant differences were found in other treatment modalities in group B (p = 0.1, ANOVA study).
The same findings were retrieved for group A with the difference that a high rate of late complications is present in GIAs treated with bypass without differences in mortality rate (p < 0.01, ANOVA study). Data of outcome are summarized in Table 4.
Based on the best results obtained in consideration of the variables that were deemed most important for the choice of treatment that in the results we set forth, we finally designed a treatment algorithm (Fig. 4).
Discussion
The treatment of GIAs represents a significant challenge among vascular lesions. Although the continuous improvement of neurosurgical and endovascular techniques, no treatment is considered a gold standard [19]. If indeed by now the endovascular procedure is becoming the first choice of treatment for most intracranial aneurysms, the same cannot be said for GIAs [20]. We show an adequate and comparable result between the two strategies, with an acceptable percentage of survival and complication rate (6.8% of mortality and an mRS < 2 in 79.7% of patients after 3 months) reported in the largest published series [21–23], for the surgical group, and comparable results for the endovascular group (6.8% of mortality and an mRS < 2 in 86.4% of patients after 3 months), where different series [24–27] show a rate of mortality and morbidity between 3.8% and 9%.
In literature, few studies of GIAs compare the outcomes of the two different treatment strategies; in some collections [11, 23, 28–30], it is argued that a different rate of complications and obliteration rates among reconstructive techniques for each strategy. On other hand, designing treatment strategies for GIAs is difficult as evidence of large clinical trials is lacking [31–33].
In our series, we did not find significant prognostic differences between approaches. The most evident difference lies in a different total number of complete occlusion between the two strategies in front of the same good outcomes.
Given these promising results in terms of outcome between the two groups, we tried to analyze the variables taken into account to choose the most appropriate treatment.
According to the current epidemiology [31, 32], we found GIAs located more frequently in the anterior circulation. Here we have recognized that, regardless of treatment modality, there is a significant difference in outcome concerning the aneurysm site, where localizations such as MCA, AcoA, and the supraclinoid portion carotid artery pose a lower risk of mortality. We confirmed [33, 34] that when GIAs appear in the posterior circulation, the complications are more severe, and they have a worse outcome [35] since the brainstem has a functional role in the control of essential body functions such as breathing, swallowing, heart rate, blood pressure, and consciousness [8]. The anatomic locations of GIAs adjacent to the brainstem increase the difficulty of surgical treatment, and patients with this localization are more frequently selected for endovascular intervention in our series, where its evaluation was posed as the first factor evaluated.
Patient factors (age, comorbidity, clinical condition) [36], pathological factors (aneurysm location, morphology) [31], and team experience [5] play a crucial role in the decision-making for GIAs.
In addition to size, we recognized that what makes these lesions so complex is the morphology of the aneurysm, the presence of intraluminal thrombus, calcifications of the aneurysmal wall, and the presence or absence of collateral vessels, and location [37].
About morphological type of aneurysm, three major conformations have been described: saccular, fusiform, and serpentine/dissected. Saccular GIAs are thought to develop from smaller saccular aneurismatic lesions due to wall remodeling caused by high hemodynamic stress and blood flow that could increase the risk of intra-operative rupture when assumed a serpentine or dissected conformation [2]. For these reasons, the endovascular approach is generally preferred for dissected GIAs. We have placed the location and morphology of the aneurysmal wall as the foremost factors for treatment choice because they respond best to endovascular treatment regardless of the patient’s clinical characteristics at diagnosis. The clinical and neurological status are among the first variables to consider when making the diagnosis of a non-dissected supratentorial GIA. We suggest to consider surgery as the first choice in case of good health conditions of patients with good HH grades. In surgery, new techniques are available today, although direct occlusion with clipping is the technique of choice [21], reporting percentages of occlusion of 100% [9] and decompression of surrounding parenchyma. There are different methods for clipping, such as tandem or parallel clipping, combined clipping using a fenestrated and straight clip, and dome clipping. In some cases, temporary trapping, thrombectomy, or clip reconstruction may be required, especially with wide-necked aneurysms [25, 26, 38]. Based on our experience, the most critical surgical factor for the technical decision is the characteristics of the neck: in the case of an absent or small channel (defined as < 4 mm [39, 40]) or in surgical cases of fusiform aneurysms, the first alternative technique taken into consideration is the bypass (that can be high-flow extracranial-intracranial bypass, low-flow bypass with superficial temporal artery or reimplantation/reanastomosis [31, 41], based on BOT).
Suppose there is a calcified aneurysm or a thrombus in the neck or perforating vessels arising from the dome, in that case, other alternative techniques can be used, such as wrapping, trapping, and aneurysmectomy. BOT should precede the procedure in which there are parent vessels sacrificed [42–45].
Considering the endovascular perspective, the introduction of FD devices has revolutionized the management of giant, wide-necked, or dissecting/fusiform intracranial aneurysms [25, 46]. FD shows a higher obliteration rate than stent-assisted coiling in unruptured supratentorial GIAs, whereas coiling alone should be preferred for posterior circulation and ruptured lesions with a wide neck.
Among coiling techniques [25, 47, 48], it has been shown that the results obtained with coiling alone or stent-assisted coil are not as effective due to the risk of re-canalization and migration of coils [49, 50]. However, there is a slight difference in the percentage of re-habitation in our series. Furthermore, in various cases, combining FD with coil embolization should accelerate the aneurysmal sac’s thrombosis, which suggests that these two techniques should be considered complementary rather than competitive [24].
In conclusion, according to the literature (advanced by recent meta-analysis and series [22]), we can affirm that although the endovascular approach is nowadays considered a well-accepted technique even for GIAs, microsurgery shows advantages that make it still the first-line treatment in most cases [9, 10, 17, 51]. For their essential mass effect, the goal of therapy is both the occlusion of the aneurysmal sac and the reduction of this effect on the brain [52, 53], which makes endovascular treatment unacceptable in most cases. In contrast, some authors believe that given the risks associated with microsurgery and the less-invasive endovascular approach, the latter should be applied [38, 54,55,56,57,58].
Limitations and further study
Our study has several limitations; the study was a retrospective study over a long period, which might include some confounding factors, such as patient selection and treatment technique bias. GIAs is a rare disease, and collecting a large case series presupposed a review of cases spanning almost three decades. In the early 1990s, endovascular treatments were less frequent and not equipped with current technology. Another limitation is that being a single-center study, surgical indications, procedures, and peri-operative patient management may vary according to institutional guidelines and experience.
Conclusion
The mortality rate is comparable between the endovascular and surgical groups regarding the treatment of GIAs. Both endovascular and surgical treatment could be safe and effective and lead to favorable outcomes for GIAs. Endovascularly treated patients have a better post-operative outcome and a lower rate of complications but a higher risk of recurrence and necessity of further treatment. Despite the improvement of the various techniques, the efficacy and safety are still unclear, and the appropriateness of the treatment is decided case by case, preferring high-risk patients, posterior location, or dissecant GIAs for the endovascular procedure and healthy, young, supratentorial, and wide neck GIAs for surgery.
Abbreviations
- GIA:
-
Giant intracranial aneurysms
- SAHs:
-
Subarachnoid hemorrhages
- EC-IC:
-
External carotid-intracranial carotid bypass
- FD:
-
Flow diverters
- MRI:
-
Magnetic resonance imaging
- ICA:
-
Internal carotid artery
- VBS:
-
Vertebrobasilar system
- CTA:
-
Computed tomography angiography
- MCA:
-
Middle cerebral artery
- ACA-ACoA:
-
Anterior cerebral-anterior communicating
- BTO:
-
Balloon test occlusion
- TIA:
-
Transitory ischemic attach
- FD:
-
Flow diverter
References
Scozzafava J, Sutherland G (2011) Giant intracranial aneurysm. CMAJ 183(9):E604. https://doi.org/10.1503/cmaj.080184
Parkinson RJ, Eddleman CS, Batjer HH, Bendok BR (2006) Giant intracranial aneurysms: endovascular challenges. Neurosurgery 59(5 Suppl 3):S103-12. https://doi.org/10.1227/01.NEU.0000237410.32115.C9 (discussion S3-13)
Briganti F, Leone G, Napoli M, Lauriola W, Florio F, Maiuri F (2015) Early fatal hemorrhage after endovascular treatment of a giant aneurysm with flow diverter device and coils. Clin Neuroradiol 25:201–205. https://doi.org/10.1007/s00062-014-0310-x
Blanc R, Weill A, Piotin M, Ross IB, Moret J (2001) Delayed stroke secondary to increasing mass effect after endovascular treatment of a giant aneurysm by parent vessel occlusion. AJNR Am J Neuroradiol 22:1841–1843
Lonjon M, Pennes F, Sedat J, Bataille B (2015) Epidemiology, genetic, natural history and clinical presentation of giant cerebral aneurysms. Neurochirurgie 61(6):361–365. https://doi.org/10.1016/j.neuchi.2015.08.003
Choi IS, David C (2003) Giant intracranial aneurysms: development, clinical presentation and treatment. Eur J Radiol 46(3):178–194
Wiebers DO, Whisnant JP, Huston J 3rd et al (2003) Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 362(9378):103–110
Ota N et al (2018) Evaluation of microsurgery for managing giant or complex cerebral aneurysms: a retrospective study. World Neurosurgery 115:e190–e199
Chalouhi N et al (2014) Microsurgical clipping of large and giant cerebral aneurysms: a single-center contemporary experience. J Clin Neurosci 21(8):1424–1427
Morita A et al (2012) The natural course of unruptured cerebral aneurysms in a Japanese cohort. N Engl J Med 366(26):2474–2482
Dengler J, Rüfenacht D, Meyer B, Rohde V, Endres M, Lenga P, Uttinger K, Rücker V, Wostrack M, Kursumovic A, Hong B, Mielke D, Schmidt NO, Burkhardt JK, Bijlenga P, Boccardi E, Cognard C, Heuschmann PU, Vajkoczy P, Giant Intracranial Aneurysm Study Group (2019) Giant intracranial aneurysms: natural history and 1-year case fatality after endovascular or surgical treatment. J Neurosurg. 134(1):49–57
Lawton MT, Spetzler RF (1995) Surgical management of giant intracranial aneurysms: experience with 171 patients. Clin Neurosurg 42:245–266
Pescatori L, Tropeano MP, Santoro A (2018) Complex aneurysm: the unpredictable pathological entity. Acta Neurochir Suppl 129:61–70. https://doi.org/10.1007/978-3-319-73739-3_9
Cantore G, Santoro A, Guidetti G, Delfinis CP, Colonnese C, Passacantilli E (2008) Surgical treatment of giant intracranial aneurysms: current viewpoint. Neurosurgery. 63(4 Suppl 2):279–89. https://doi.org/10.1227/01.NEU.0000313122.58694.91 (discussion 289-90)
Arambepola PK, McEvoy SD, Bulsara KR (2010) De novo aneurysm formation after carotid artery occlusion for cerebral aneurysms. Skull Base 20(6):405–408. https://doi.org/10.1055/s-0030-1253578
Hasan DM, Nadareyshvili AI, Hoppe AL, Mahaney KB, Kung DK, Raghavan ML (2012) Cerebral aneurysm sac growth as the etiology of recurrence after successful coil embolization. Stroke 43(3):866–868. https://doi.org/10.1161/STROKEAHA.111.637827
Bendok BR, Parkinson RJ, Hage ZA, Adel JG, Gounis MJ (2007) The effect of vascular reconstruction device-assisted coiling on packing density, effective neck coverage, and angiographic outcome: an in vitro study. Neurosurgery. 61(4):835–40. https://doi.org/10.1227/01.NEU.0000298913.24625.26 (discussion 840-1)
Brinjikji W, Piano M, Fang S, Pero G, Kallmes DF, Quilici L, Valvassori L, Lozupone E, Cloft HJ, Boccardi E, Lanzino G (2016) Treatment of ruptured complex and large/giant ruptured cerebral aneurysms by acute coiling followed by staged flow diversion. J Neurosurg 125(1):120–127. https://doi.org/10.3171/2015.6.JNS151038
Nurminen V, Lehecka M, Chakrabarty A, Kivisaari R, Lehto H, Niemelä M, Hernesniemi J (2014) Anatomy and morphology of giant aneurysms–angiographic study of 125 consecutive cases. Acta Neurochir (Wien) 156(1):1–10. https://doi.org/10.1007/s00701-013-1933-4
- Misra BK (2015) Treatment of giant intracranial aneurysms: what is the best option? Neurology India
Sharma BS, Gupta A, Ahmad FU, Suri A, Mehta VS (2008) Surgical management of giant intracranial aneurysms. Clin Neurol Neurosurg 110(7):674–681
Dengler J, Maldaner N, Gläsker S, Endres M, Wagner M, Malzahn U, Heuschmann PU, Vajkoczy P, Giant Intracranial Aneurysm Study Group (2016) Outcome of surgical or endovascular treatment of giant intracranial aneurysms, with emphasis on age, aneurysm location, and unruptured aneuryms–a systematic review and meta-analysis. Cerebrovasc Dis 41(3–4):187–98. https://doi.org/10.1159/000443485
Sughrue ME, Saloner D, Rayz VL, Lawton MT (2011) Giant intracranial aneurysms: evolution of management in a contemporary surgical series. Neurosurgery 69(6):1261–1271
Peschillo S et al (2017) Endovascular treatment of large and giant carotid aneurysms with flow-diverter stents alone or in combination with coils: a multicenter experience and long-term follow-up. Operative Neurosurgery 13(4):492–502
Liu JM et al (2018) Parent artery reconstruction for large or giant cerebral aneurysms using the tubridge flow diverter: a multicenter, randomized, controlled clinical trial (PARAT). Am J Neuroradiol 39(5):807–816
Adeeb N et al (2017) Pipeline embolization device in treatment of 50 unruptured large and giant aneurysms. World Neurosurgery 105:232–237
Kallmes DF et al (2015) International retrospective study of the pipeline embolization device: a multicenter aneurysm treatment study. Am J Neuroradiol 36(1):108–115
Jahromi BS et al (2008) Clinical and angiographic outcome after endovascular management of giant intracranial aneurysms. Neurosurgery 63(4):662–675
Liang F et al (2019) Predictors of periprocedural complications and angiographic outcomes of endovascular therapy for large and giant intracranial posterior circulation aneurysms. World Neurosurgery 125:e378–e384
- Wang J et al (2019) Corrigendum: application of the pipeline embolization device for giant vertebrobasilar dissecting aneurysms in pediatric patients. Frontiers in Neurology 10
Sousa A, Sousa Filho J, Dellaretti Filho M (2015) Treatment of giant intracranial aneurysms: a review based on experience from 286 cases. Arquivos Brasileiros de Neurocirurgia: Brazilian Neurosurgery 34(04):295–303
Sekhlar LN et al (2016) Microsurgery of giant intracranial aneurysms. Atlas Neurosurg Techniques I:301–321
Johnson AK et al (2015) Complication analysis in nitinol stent-assisted embolization of 486 intracranial aneurysms. J Neurosurg 123(2):453–459
- Nanda, A., Sonig, A., Banerjee, A. D. & Javalkar, V. K (2014) Microsurgical management of giant intracranial aneurysms: a single surgeon experience from Louisiana State University, Shreveport. World Neurosurgery
Cagnazzo F et al (2018) Endovascular treatment of very large and giant intracranial aneurysms: Comparison between reconstructive and deconstructive techniques - a meta-analysis. Am J Neuroradiol 39(5):852–858
Lawton MT et al (2003) Combined microsurgical and endovascular management of complex intracranial aneurysms. Neurosurgery 52(2):263–275
- Hanel RA, Spetzler RF (2008) Surgical treatment of complex intracranial aneurysms. Neurosurgery 62 (6 SUPPL)
Lubicz B et al (2007) Endovascular treatment of intracranial aneurysms as the first thérapeutic option. J Neuroradiol 34(4):250–259
Yasargil MG (1984) Pathological considerations. In: Yasargil MG (ed) Microneurosurgery. Thieme Verlag, Stuttgart, pp 280–281
Fernandez Zubillaga A, Guglielmi G, Viñuela F, Duckwiler GR (1994) Endovascular occlusion of intracranial aneurysms with electrically detachable coils: correlation of aneurysm neck size and treatment results. AJNR Am J Neuroradiol 15(5):815–820
Jafar JJ et al (2002) Treatment of giant intracranial aneurysms with saphenous vein extracranial-to-intracranial bypass grafting: indications, operative technique, and results in 29 patients. Neurosurgery 51(1):138–146
Hassan T, Sultan AE, Elwany MN (2011) Evaluation of balloon occlusion test for giant brain aneurysms under local anaesthesia. Neuroradiol J 24(5):735–742
Linskey ME et al (1994) Stroke risk after abrupt internal carotid artery sacrifice: accuracy of preoperative assessment with balloon test occlusion and stable xenon-enhanced CT. Am J Neuroradiol 15(5):829–843
Mattingly T et al (2013) Visual outcomes for surgical treatment of large and giant carotid ophthalmic segment aneurysms: a case series utilizing retrograde suction decompression (the ‘Dallas technique’). Clinical article. J Neurosurg 118(5):937–946
Batjer HH, Kopitnik TA, Giller CA, Samson DS (1994) Surgery for paraclinoidal carotid artery aneurysms. J Neurosurg 80(4):650–658
Jiang B, Paff M, Colby GP, Coon AL, Lin LM (2016) Cerebral aneurysm treatment: modern neurovascular techniques. Stroke Vasc Neurol 1(3):93–100. https://doi.org/10.1136/svn-2016-000027
Dmytriw AA et al (2019) On flow diversion: the changing landscape of intracerebral aneurysm management. American Journal of Neuroradiolog 40:591–600
Zhou Y et al (2014) A novel flow-diverting device (tubridge) for the treatment of 28 large or giant intracranial aneurysms: a single-center experience. Am J Neuroradiol 35(12):2326–2333
Wang B, Gao BL, Xu GP, Xiang C, Liu XS (2015) Endovascular embolization is applicable for large and giant intracranial aneurysms: experience in one center with long-term angiographic follow-up. Acta Radiol 56(1):105–113
Bracard S et al (2016) Traitement endovasculaire des anévrismes géants. Neurochirurgie 62(1):25–29
- Balaji A et al (2019) A retrospective study in microsurgical procedures of large and giant intracranial aneurysms: an outcome analysis. World Neurosurgery X 2
Maldaner N et al (2015) Changes in volume of giant intracranial aneurysms treated by surgical strategies other than direct clipping. Acta Neurochir 157(7):1117–1123
Cantore G et al (2008) Surgical treatment of giant intracranial aneurysms: current viewpoint. Operative Neurosurgery 63:279–290
Molyneux AJ et al (2005) International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet 366(9488):809–817
Luzzi S, Gragnaniello C, Giotta Lucifero A, Del Maestro M, Galzio R (2020) Surgical management of giant intracranial aneurysms: overall results of a large series. World Neurosurg 144:e119–e137. https://doi.org/10.1016/j.wneu.2020.08.004
Campos JK, Ball BZ, Cheaney Ii B, Sweidan AJ, Hasjim BJ, Hsu FPK, Wang AS, Lin LM (2020) Multimodal management of giant cerebral aneurysms: review of literature and case presentation. Stroke Vasc Neurol 5(1):22–28. https://doi.org/10.1136/svn-2019-000304
Whittle IR, Dorsch NW, Besser M (1982) Spontaneous thrombosis in giant intracranial aneurysms. J Neurol Neurosurg Psychiatry 45(11):1040–1047. https://doi.org/10.1136/jnnp.45.11.1040
Kato Y et al (2003) Surgical strategies for treatment of giant or large intracranial aneurysms: our experience with 139 cases. Minimally invasive neurosurgery 46(6):339–343
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
Antonio Santoro: surgical operator, conceptualization, supervising; Daniele Armocida: writing, analysis, data curation; Francesco Paglia: data collection, review of literature; Marta Iacobucci: neuro-radiological operator, writing, data collection; Luigi Valentino Berra: surgical operator, revising, writing; Luca D’Angelo: surgical operator, revising; Carlo Cirelli: neuro-radiological operator, writing; Giulio Guidetti: neuro-radiological operator, supervising; Francesco Biraschi: neuro-radiological operator, writing, data collection, conceptualization; Giampaolo Cantore: surgical operator, conceptualization.
Corresponding author
Ethics declarations
Ethics approval
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Num. IRB 6168 Prot. 0935/2020.
Consent for publication
Informed consent was obtained from all subjects involved in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Santoro, A., Armocida, D., Paglia, F. et al. Treatment of giant intracranial aneurysms: long-term outcomes in surgical versus endovascular management. Neurosurg Rev 45, 3759–3770 (2022). https://doi.org/10.1007/s10143-022-01884-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-022-01884-3