Abstract
Background
Giant intracranial aneurysms are rare and heterogeneous lesions with complex vascular anatomy. The aim of this retrospective study was to provide a comprehensive description of the anatomical features of giant aneurysms.
Methods
We identified 125 patients with 129 giant aneurysms (≥25 mm) who were treated between 1987 and 2007 at the Department of Neurosurgery of Helsinki University Central Hospital (HUCH). All the imaging studies and medical records were reviewed for relevant information.
Results
The distribution of the giant aneurysms among regions was as follows: internal carotid artery (ICA) 39 %, middle cerebral artery (MCA) 32 %, vertebrobasilar and posterior cerebral artery (VB-PCA) region 25 %, and anterior cerebral artery (ACA) including the anterior communicating artery 5 %. The cavernous ICA segment (n = 21, 16 %) and the MCA bifurcation (n = 25, 19 %) were the most frequent specific locations. Half (n = 11) of all fusiform aneurysms were found in the VB-PCA region. As many as 41 % of the giant MCA aneurysms were ruptured. Major anatomic variations were found in three (2 %) and multiple giant aneurysms in three (2 %) patients. Wall calcification was noted in 24 % and intraluminal thrombosis in 33 % of ruptured giant aneurysms (n = 42).
Conclusions
The majority of giant aneurysms are located in the ICA and MCA regions, while the ACA region is an exceptional site. The MCA region is the most common site for ruptured giant aneurysms. Associated anatomic variations and the multiplicity of giant aneurysms are a rare finding.





Similar content being viewed by others
Abbreviations
- A2–A5 :
-
A2–A5 segments of anterior cerebral artery
- ACA :
-
anterior cerebral artery
- Acom :
-
anterior communicating artery
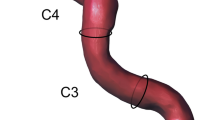
- C1 :
-
cervical segment of the internal carotid artery
- C4 :
-
cavernous segment of the internal carotid artery
- C6 :
-
ophthalmic segment of the internal carotid artery
- C7 :
-
communicating segment of the internal carotid artery
- CT :
-
computer tomography
- CT angiography :
-
computed tomography angiography
- DSA :
-
digital subtraction angiography
- HUCH :
-
Helsinki University Central Hospital
- ICA :
-
internal carotid artery
- M1 :
-
M1 segment of middle cerebral artery
- MCA :
-
middle cerebral artery
- MR angiography :
-
magnetic resonance angiography
- MRI :
-
magnetic resonance imaging
- PACS :
-
Picture Archiving and Communicating System
- PCA :
-
posterior cerebral artery
- Pcom :
-
posterior communicating artery
- SAH :
-
subarachnoid hemorrhage
- VB :
-
vertebrobasilar
- VB-PCA :
-
vertebrobasilar and posterior cerebral artery region
References
Cantore G, Santoro A, Guidetti G, Delfinis CP, Colonnese C, Passacantilli E (2008) Surgical treatment of giant intracranial aneurysms: current viewpoint. Neurosurgery 63(4 Suppl 2):279–289
Choi IS, David C (2003) Giant intracranial aneurysms: development, clinical presentation and treatment. Eur J Radiol 46(3):178–194
Darsaut TE, Darsaut NM, Chang SD et al (2011) Predictors of clinical and angiographic outcome after surgical or endovascular therapy of very large and giant intracranial aneurysms. Neurosurgery 68(4):903–915
dos Santos ML, Spotti AR, dos Santos RM, Borges MA, Ferrari AF, Colli BO, Tognola WA (2013) Giant intracranial aneurysms: morphology and clinical presentation. Neurosurg Rev 36(1):117–122
Drake CG, Peerless SJ (1997) Giant fusiform intracranial aneurysms: review of 120 patients treated surgically from 1965 to 1992. J Neurosurg 87(2):141–162
Drake CG, Peerless SJ, Hernesniemi JA (1996) Giant basilar trunk aneurysms: 59 patients. In: Drake CG, Peerless SJ, Hernesniemi JA (eds) Surgery of vertebrobasilar aneurysms: London, Ontario experience on 1767 patients. Springer, Vienna, pp 143–166
Hahn CD, Nicolle DA, Lownie SP, Drake CG (2000) Giant cavernous carotid aneurysms: clinical presentation in fifty-seven cases. J Neuroophthalmol 20(4):253–258
Hanel RA, Spetzler RF (2008) Surgical treatment of complex intracranial aneurysms. Neurosurgery 62(6 Suppl 3):1289–1297
Huttunen T, Von und zu Fraunberg M, Frösen J, Lehecka M, Tromp G, Helin K, Koivisto T, Rinne J, Ronkainen A, Hernesniemi J, Jääskeläinen JE (2010) Saccular intracranial aneurysm disease: distribution of site, size, and age suggests different etiologies for aneurysm formation and rupture in 316 familial and 1454 sporadic eastern Finnish patients. Neurosurgery 66(4):631–638
Linskey ME, Sekhar LN, Hirsch W Jr, Yonas H, Horton JA (1990) Aneurysms of the intracavernous carotid artery: clinical presentation, radiographic features, and pathogenesis. Neurosurgery 26(1):71–79
Locksley HB (1966) Natural history of subarachnoid hemorrhage, intracranial aneurysms and arteriovenous malformations. Based on 6368 cases in the cooperative study. J Neurosurg 25(2):219–239
Lozier AP, Kim GH, Sciacca RR, Connolly ES Jr, Solomon RA (2004) Microsurgical treatment of basilar apex aneurysms: perioperative and long-term clinical outcome. Neurosurgery 54(2):286–296
Lubicz B, Leclerc X, Gauvrit JY, Lejeune JP, Pruvo JP (2004) Giant vertebrobasilar aneurysms: endovascular treatment and long-term follow-up. Neurosurgery 55(2):316–23
Sughrue ME, Saloner D, Rayz VL, Lawton MT (2011) Giant intracranial aneurysms: evolution of management in a contemporary surgical series. Neurosurgery 69(6):1261–70
Tamaki N, Kim S, Ehara K, Asada M, Fujita K, Taomoto K, Matsumoto S (1991) Giant carotid-ophthalmic artery aneurysms: direct clipping utilizing the “trapping-evacuation” technique. J Neurosurg 74(4):567–572
The International Study of Unruptured Intracranial Aneurysms Investigators (1998) Unruptured intracranial aneurysms—risk of rupture and risks of surgical intervention. International Study of Unruptured Intracranial Aneurysms Investigators. N Engl J Med 339(24):1725–1733
Japan Investigators UCAS, Morita A, Kirino T, Hashi K, Aoki N, Fukuhara S, Hashimoto N, Nakayama T, Sakai M, Teramoto A, Tominari S, Yoshimoto T (2012) The natural course of unruptured cerebral aneurysms in a Japanese cohort. N Engl J Med 366(26):2474–2482
Wiebers DO, Whisnant JP, Huston J 3rd, Meissner I, Brown RD Jr, Piepgras DG, Forbes GS, Thielen K, Nichols D, O’Fallon WM, Peacock J, Jaeger L, Kassell NF, Kongable-Beckman GL, Torner JC, International Study of Unruptured Intracranial Aneurysms Investigators (2003) Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 362(9378):103–110
Conflicts of interest
None.
Financial disclosure
The authors of this study have no relevant financial or nonfinancial relationships to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nurminen, V., Lehecka, M., Chakrabarty, A. et al. Anatomy and morphology of giant aneurysms—angiographic study of 125 consecutive cases. Acta Neurochir 156, 1–10 (2014). https://doi.org/10.1007/s00701-013-1933-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-013-1933-4