Abstract
Brainstem hemangioblastomas are benign, highly vascular tumors located in the mesencephalon, pons, and medulla oblongata. Although surgical resection is currently considered the main therapeutic option for symptomatic lesions, evidence supporting the application of microsurgery has not been systematically assessed. This meta-analysis aims to evaluate the safety and efficacy of surgical treatment for brainstem hemangioblastomas. A comprehensive search of the PubMed, Embase, and Web of Science databases was performed to identify all English language publications reporting the outcomes of surgical treatment for brainstem hemangioblastomas. Studies from January 1990 to July 2019 with ≥ 10 cases were included. We analyzed the surgical outcomes, including gross total resection, mortality, neurological morbidity, and functional outcome according to the McCormick Scale or Karnofsky Performance Scale. Thirteen studies with 473 cases were included. The pooled proportion of gross total resection was 98% (95% confidence interval (CI), 94–100%). Overall mortality and neurological morbidity were 4 (95% CI, 2–6%) and 13% (95% CI, 7–20%), respectively. Favorable functional outcomes at the last follow-up were achieved in 85% (95% CI, 78–92%) of all patients. Improved or stable functional outcomes at long-term follow-up were achieved in 94% (95% CI, 89–97%) of patients. This meta-analysis revealed that surgical treatment for brainstem hemangioblastomas is technically feasible and effective with lasting patient benefits and cure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hemangioblastomas are relatively rare and histologically benign neoplasms, which may occur either sporadically or in association with von Hippel-Lindau disease (VHL) [16]; they usually grow slowly and account for 1.5–3.7% of intracranial tumors [3, 18, 23, 33] and 3–4% of spinal tumors [3, 18]. Hemangioblastomas of the central nervous system (CNS) are most commonly located in the cerebellum, followed by the spinal cord and brainstem [32].
To date, therapeutic options include radiosurgery and microsurgical resection of the tumor. Radiosurgery may cause severe radiation-induced adverse effects and is only appropriate for inoperable, residual, or recurrent hemangioblastomas [29]. Thus, microsurgical resection of tumors is considered the optimal option for patients with symptomatic or progressive CNS hemangioblastoma [7, 9, 24].
Brainstem hemangioblastomas are defined as tumors originating from the mesencephalon, pons, and medulla oblongata; they account for 5–15% of all intracranial hemangioblastomas [6, 12]. The complex anatomical structures and pivotal neural structures of the brainstem create a higher risk for morbidity and mortality. Consequently, surgical treatment for brainstem hemangioblastoma poses a significant challenge for neurosurgeons. To date, there have been many studies on the surgical outcomes of microsurgical resection of brainstem hemangioblastomas [4, 10, 13, 15, 17, 22, 33,34,35,36,37,38, 40]. We conducted a meta-analysis of surgical outcomes from the published literature to evaluate the safety and efficacy of surgical treatment for brainstem hemangioblastoma in this study.
Materials and methods
We conducted a meta-analysis following the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [20].
Study selection
We performed a comprehensive literature review using appropriate medical subject heading (MeSH) terms and the corresponding random words, including“brainstem”, “pons”, “mesencephalon”, “medulla oblongata”, “hemangioblastoma”, “von Hippel-Lindau disease”, “surgery”, “microsurgery”, “neurosurgery”, and “craniotomy”, in both “AND” and “OR” combinations to search the PubMed, Embase, and Web of Science databases. The search strategy can be found in Online Resource 1.
Inclusion and exclusion criteria
Studies were included if they (1) were published from January 1990 to July 2019; (2) reported extent of tumor resection; (3) reported postoperative mortality; and (3) reported the preoperative and postoperative functional status. Exclusion criteria were as follows: non-English studies, case reports, review articles, conference abstracts, technical notes, operative video, articles that reported less than 10 cases, and studies lacking critical data.
Data extraction
Extracted data included the first author’s name, publication year, country, patient demographics, tumor locations, and the total numbers of cases. We studied the surgical outcomes, including extent of tumor resection, postoperative mortality, and preoperative and postoperative functional status in the hospital and at long-term follow-up. Assessment of functional status was based on the McCormick Scale [19] or Karnofsky Performance Scale (KPS) [26]. Neurological morbidity was defined as the proportion of patients experiencing deterioration of short-term functional status, which was usually assessed immediately after surgery or at discharge.
Quality assessment
The quality of all the included studies was graded using the methodological index for non-randomized studies (MINORS) [28]. The assessment of study quality was based on the checklist of 8 items for noncomparative studies, and the evaluation was scored 0 (not reported), 1 (reported but inadequate), or 2 (reported and adequate) for each item. Two authors (Yin and Li) graded the studies independently. Disagreement was solved by discussion.
Statistical analysis
The meta-analyses were performed in the statistical software R version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria) [1] using the meta-packages [2]. The Freeman-Tukey double arcsine method was used for the transformation of surgical outcomes of each study prior to calculating the pooled results [8]. We used random-effects model in all the analyses. Between-study heterogeneity was assessed with Cochran’s Q test [5]. A P value for the test of heterogeneity < 0.10 was considered evidence of heterogeneity [27]. The I2 statistic, which describes the percentage of variance due to heterogeneity, was also considered. Heterogeneity across all the studies was classified into low, moderate, and high with I2 values of 25, 50, and 75%, respectively [11]. Egger’s linear regression test was applied to assess potential publication bias. A P value < 0.05 for the Egger’s test was considered statistically significant [30].
Results
The search initially yielded 694 studies. A total of 473 studies were included after the removal of duplicates. On initial abstract and title review, we removed 144 case reports, 50 letters or article comments, 42 conference articles, 39 articles reporting non-relevant research topics, 14 articles about operative videos, 12 technical notes, and 109 studies reporting hemangioblastomas in other locations. After carefully screening the remaining studies, we excluded 23 studies without sufficient data, 9 non-English studies, 6 studies with fewer than 10 cases, 5 conference articles, and 3 studies reporting non-relevant research topics. Four of the 17 remaining studies fulfilling inclusion criteria were removed for failing to provide extractable data. Thus, a total of 13 identified studies were included in this meta-analysis (Fig. 1) [4, 10, 13, 15, 17, 22, 33,34,35,36,37,38, 40]. Details of the included studies are shown in Table 1.
Baseline characteristics
All 13 studies were retrospective and observational. A total of 473 patients with brainstem hemangioblastomas were presented, of whom 221 were females (46.7%) and 252 were males (53.3%). The mean age of the included patients at surgery was 34.0 years (range 6–71 years). Forty-one percent of the hemangioblastomas were associated with cyst formation. The size of the tumors or cysts was reported in 7 studies [4, 10, 13, 15, 17, 36, 37], and the mean diameter was 21.3 mm (range 2–56 mm). In total, 39.6% of the tumors were related to VHL disease [10, 13, 15, 17, 22, 33,34,35, 37, 40]. The most common region involved was the medulla oblongata (55.0%). According to the relationship between the tumor and surrounding parenchyma, 15.1% of brainstem hemangioblastomas were entirely intrabrainstem or intramedullary [4, 10, 13, 15, 17, 34]. Details of the study characteristics are shown in Table 2.
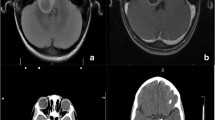
Extent of tumor resection
All 13 included articles provided complete information on tumor resection that could be extracted and analyzed [4, 10, 13, 15, 17, 22, 33,34,35,36,37,38, 40]. The extent of tumor resection was confirmed by postoperative computed tomography (CT) or magnetic resonance imaging (MRI). Gross total resection was achieved in 98% (95% CI, 94–100%; I2 = 71%) of the cases. The heterogeneity between the groups was significant (I2 = 71%, P < 0.01) (Fig. 2 and Table 2).
Postoperative mortality and morbidity
Surgical mortality was reported in all the included articles [4, 10, 13, 15, 17, 22, 33,34,35,36,37,38, 40]. The results showed that the pooled proportion of surgical mortality was 4% (95% CI, 2–6%; I2 = 0%). Heterogeneity testing revealed no evidence of heterogeneity between all the groups (I2 = 0%, P = 0.47) (Fig. 2 and Table 2).
Data on neurological morbidity were analyzed in 8 of 13 studies [4, 10, 13, 15, 17, 22, 35, 37]. The cumulative proportion of morbidity was 13% (95% CI, 7–20%; I2 = 57%). There was evident heterogeneity between the groups (I2 = 57%, P = 0.02) (Fig. 2 and Table 2).
Functional outcomes at long-term follow-up
Functional outcomes at long-term follow-up were reported in 8 studies [4, 10, 13, 15, 22, 34, 38, 40]. A favorable functional status was determined if the patient was self-independent with grade I/II on the McCormick Scale or KPS ≥ 80. The pooled results showed that a favorable functional outcome was achieved in 85% (95% CI, 78–92%; I2 = 50%) of all patients at long-term follow-up. The heterogeneity between the groups was relatively moderate (I2 = 50%; P = 0.05) (Fig. 2 and Table 2).
We also compared postoperative functional status at the last follow-up compared with the preoperative functional condition. Data were obtained from 10 studies [4, 10, 13, 15, 17, 22, 34, 35, 37, 38]. The pooled analysis showed that improved or stable functional outcomes at the last follow-up compared with the preoperative function condition were achieved in 94% of patients (95% CI, 89–97%; I2 = 51%). Heterogeneity was obvious with I2 = 51% and P = 0.03 for heterogeneity (Fig. 2 and Table 2).
Quality assessment
All the included studies were self-controlled trials, which can reflect the outcomes of surgical treatment credibly and the impact on the patients accurately. In the assessment of quality, the mean value of the MINORS score was 13.5 (median, 14; range, 11–15). According to the MINORS score, the quality level of the included studies was overall acceptable, even though none of the studies received a full score on all the items. No study was excluded because of low quality. The MINORS scores are given in Online Resource 2.
Heterogeneity and sensitivity analysis
Statistical heterogeneity across all the included studies was generally acceptable for most outcomes. Significant heterogeneity with I2 > 50% was observed in the meta-analysis of total tumor resection (I2 = 71%), surgical morbidity (I2 = 56%), and functional improvement at long-term follow-up (I2 = 51%) (Table 2). Specifically, the heterogeneity for total tumor resection was high with I2 = 71% if Joseph’s study was included. The sensitivity analysis showed that the heterogeneity for the total resection outcome was reduced to I2 = 0% after omitting Joseph’s study. Therefore, Joseph’s study may be a cause of significant heterogeneity in the analysis of total tumor resection, and the result should be interpreted with caution. Sensitivity tests were also utilized to inspect the possible causes of between-study heterogeneity for surgical morbidity and long-term neurological function improvement. No factors were recognized as being responsible for the heterogeneity.
Publication bias
Egger’s test was used to identify possible publication bias. The P value > 0.5 for each meta-analysis revealed no evidence of significant publication bias (Table 2).
Discussion
The incidence of brainstem hemangioblastoma is 2–20% of all intracranial hemangioblastomas, and the most common location is the medulla oblongata. Hemangioblastomas of the brainstem usually occur as solid tumors [39]. Brainstem hemangioblastomas are benign lesions located in complicated anatomical structures, which may cause severe neurological deficits and even death. To date, surgical resection has often been the first option for brain hemangioblastomas that appear to be symptomatic or radiologically progressive. In the past, surgical resection of brainstem hemangioblastomas resulted in poor outcomes due to the complex structure of the brainstems and the rich blood supply of hemangioblastomas. Consequently, a number of patients were referred for radiosurgery. With the advent of microscopy and advances in microsurgical techniques, however, total tumor resection and mortality have become acceptable. Many studies have reported outcomes with respect to the safety and efficacy of brainstem hemangioblastoma surgery. By analyzing all brainstem hemangioblastoma cases from 13 studies, our meta-analysis provided data on the outcomes of surgical treatment and information for neurosurgeons to treat brainstem hemangioblastomas. This study revealed that surgical resection of brainstem hemangioblastomas was reliable, with favorable functional outcomes in 94% of patients. It was technically feasible to remove brainstem hemangioblastomas surgically according to the high rate of total tumor resection (99%) and acceptable rates of postoperative mortality (4%) and neurological morbidity (15%).
As hemangioblastomas are benign and highly vascularized neoplasms with possibilities of recurrence, the primary goal of surgery is radical resection of tumors without significant damage to the surrounding parenchyma. The mortality and complication rates increase markedly with secondary operation on the residual tumors [10, 17]. Neurosurgeons, therefore, always endeavor to remove the tumors completely to avoid tumor recurrence and reoperations, which contributes to the high rate of total resection. To accomplish total resection, it is recommended that surgical management adheres to the principle of arteriovenous malformation surgery, which includes identification and division of the feeding arteries, followed by dissection of the lesion with the preservation of the main draining veins and the occlusion of the main draining veins at the last moment [13, 15, 17, 37, 38, 40]. It is important to perform en bloc resection of both solid and cystic lesions, as piecemeal resection may lead to unmanageable intraoperative bleeding. Fully exposing the operative field is critical for intraoperatively locating the lesions and successfully completing the operation. For the dorsal lesions, the suboccipital approach was usually chosen for the craniotomy. The far-lateral approach was performed for lesions located in the ventral part of the brainstem. In particular, C1 and C2 laminectomy were used to enlarge the caudal exposure for lower brainstem lesions if necessary. The pooled proportion calculated in this meta-analysis revealed that total gross resection was achieved in 99% of all cases, indicating that total resection is technically practicable and feasible.
The pooled mortality of all cases was 4%. The result was relatively low but not highly favorable. Although the optimal timing for surgery is debatable, the consensus on the operative intervention among most neurosurgeons is based on the progression of neurologic symptoms or evidence of tumor growth [10, 17, 22, 35, 38]. Therefore, patients treated by surgery were more likely to have giant tumors or unfavorable preoperative functional status that was associated with the high rate of complications and mortality. Furthermore, solid hemangioblastomas usually occur in the brainstem, which raises the risk of parenchyma injuries and consequently increases the mortality [40].
However, compared with the high mortality in the pre-microsurgical era, the mortality in our meta-analysis has significantly improved [4, 38, 40]. Microsurgery at present is generally a safe option for patients with brainstem hemangioblastoma. The improvement of surgical mortality may be attributed to the advent of microscopes as well as advances in surgical techniques, including intraoperative neurophysiological monitoring, preoperative angiography, and embolization [4, 15, 17, 38, 40]. Preoperative angiography contributed to a better understanding of the vascular arrangement and design of the surgical strategy. The role of preoperative embolization and the necessity of intraoperative neurophysiological monitoring, however, remain controversial. Specifically, Wu et al. reported favorable outcomes of 11 patients undergoing preoperative embolization and concluded that preoperative embolization was a safe and effective adjunct treatment [36]. Contrary to his study, many authors insisted that preoperative embolization was likely to cause complications linked to the procedures, such as bleeding, tumor swelling, and vessel occlusion with consecutive infarction.
Seven articles reported the causes of death, among which postoperative pneumonia was a major cause of mortality, followed by intracranial hematoma, brainstem injury, and cardiac infarction or heart failure. Although advances in surgical techniques and instruments have improved surgical outcomes, it remains important to call attention to postoperative complications. The occurrence of postoperative complications varied widely across all the studies. The most common complications included gastrointestinal ulceration or bleeding, pneumonia, lower cranial nerve deficits, hydrocephalus, and CSF leakage. Injury of the dorsal motor nucleus of the vagus nerve may account for the gastrointestinal ulceration or bleeding and respiratory center dysfunction may account for the observed pneumonia. Deficits of the lower cranial nerve usually occurred due to damage to the medulla and manifested as dysphagia and hoarseness. Hydrocephalus and CSF leakage were common complications in the posterior fossa, as reported in the literature [25]. Most of the complications were cured with active and positive treatment. Meticulous microsurgical techniques with adequate postoperative management and care may reduce the incidence of postoperative complications.
Both brainstem lesions and surgical treatment may result in neurological deficits; thus, it is of great significance to assess the functional outcomes of patients with brainstem hemangioblastomas. Comparing preoperative and postoperative scores of McCormick scale or KPS, which has been used in many studies, is considered a practical method to demonstrate the functional outcome of brainstem hemangioblastoma surgery. By analyzing the data on the functional conditions, this meta-analysis revealed that 11% of patients experienced a worse neurological condition immediately after surgery or at discharge, however, most of which were notably transient and usually improved at long-term follow-up. Based on the low morbidity rate and reversible function after surgery, therefore, it seemed a reasonable hypothesis that surgical resection of hemangioblastomas prevents the decline of neurological function. We also considered long-term functional outcomes. The pooled rate of improved functional status at the last follow-up was 85% in our meta-analysis, supporting the evidence that most patients can live and work independently and normally after surgery. It was also observed that favorable outcomes of long-term functional status were generally achieved in a majority of the patients at the last follow-up.
Several factors may have influenced the postoperative outcomes. It is generally agreed that the preoperative functional condition is a good predictor of postoperative neurological function status. Patients with good preoperative function are apt to improve neurologically or remain stable. Furthermore, it was also observed that the patients who had undergone neurosurgical procedures or radiosurgeries were more likely to suffer from the deterioration of neurological function. Some studies suggested that larger tumor or cyst size increased surgical morbidity and mortality, while other studies came to the conclusion that the tumor or cyst size did not affect the results. Despite the controversy regarding the role of tumor size, it is advisable to carefully evaluate the risk of intraoperative bleeding and postoperative complications when treating larger lesions. In particular, Wind et al. considered the presence of syringobulbia as a positive factor for immediate neurological improvement, while Giammattei et al. found brainstem edema a negative prognostic factor. Further investigations are required to confirm the association between these factors and surgical outcome.
Although surgical treatment is a therapeutic approach to cure CNS hemangioblastomas, radiosurgery has a role in the management of hemangioblastomas, especially for patients with nonresectable, residual, and recurrent tumors [14, 31]. Pan et al. analyzed 26 studies on stereotactic radiosurgery for the treatment of difficult-to-resect hemangioblastomas and proposed that stereotactic radiosurgery can serve as a reliable treatment alternative with relatively long-term efficacy in radiographic and symptomatic control. In Pan’s study, the pooled 5-year progression-free survival was 88.43%. The pooled 5-year PFS for patients with intracranial lesions is 88.44%, and with spinal lesions is 90.42%. Factors including solid tumors, smaller tumors, VHL-related lesions, and a greater marginal dose were found to be associated with better tumor control. Adverse events were related to increasing marginal dose, independent of tumor volume [21]. Despite this favorable conclusion, the utility of stereotactic radiosurgery on brainstem hemangioblastomas is limited and requires more study.
Limitations
Several limitations should be considered in the present meta-analysis, so the interpretation of the results needs to be cautious. Firstly, all the included articles were retrospective and observational studies with inherent limitations, and no randomized clinical studies were included. Furthermore, many of the studies had limited sample sizes, which may have affected the results. Omitting a study when calculating the pooled mortality may have led to an underestimation of the results. Data on functional condition were available for few studies, which limited a definitive conclusion. In addition, only English language studies were included, which may have led to a lack of information from studies published in different languages. Since our study is exploratory, clinicians should use these data for decision-making cautiously.
Conclusions
In conclusion, while hemangioblastomas are challenging lesions to remove, most brainstem hemangioblastomas can be successfully resected with generally favorable mortality, morbidity, and neurological function. Surgical treatment is a therapeutic management to cure brainstem hemangioblastoma and can create patient lasting benefit and cure. Due to the limited scale of some studies and a lack of randomized trials, however, further investigations are needed to confirm these findings.
References
(2017) R: A Language and Environment for Statistical Computing [computer program]
Balduzzi S, Rucker G, Schwarzer G (2019) How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health 22:153–160. https://doi.org/10.1136/ebmental-2019-300117
Bostrom A, Hans FJ, Reinacher PC, Krings T, Burgel U, Gilsbach JM, Reinges MH (2008) Intramedullary hemangioblastomas: timing of surgery, microsurgical technique and follow-up in 23 patients. Eur Spine J 17:882–886. https://doi.org/10.1007/s00586-008-0658-1
Chen LF, Yang Y, Yu XG, Bu B, Xu BN, Zhou DB (2013) Operative management of brainstem hemangioblastomas. J Clin Neurosci 20:1727–1733. https://doi.org/10.1016/j.jocn.2013.01.027
Cochran WG (1954) The combination of estimates from different experiments. Biometrics 10:101–129. https://doi.org/10.2307/3001666
Conway JE, Chou D, Clatterbuck RE, Brem H, Long DM, Rigamonti D (2001) Hemangioblastomas of the central nervous system in von Hippel-Lindau syndrome and sporadic disease. Neurosurgery 48:55–62; discussion 62-53. https://doi.org/10.1097/00006123-200101000-00009
Cui H, Zou J, Bao YH, Wang MS, Wang Y (2017) Surgical treatment of solid hemangioblastomas of the posterior fossa: a report of 28 cases. Oncol Lett 13:1125–1130. https://doi.org/10.3892/ol.2016.5531
Freeman MF, Tukey JW (1950) Transformations related to the angular and the square root. Ann Math Stat 21:607–611. https://doi.org/10.1214/aoms/1177729756
Fukuda M, Takao T, Hiraishi T, Yoshimura J, Yajima N, Saito A, Fujii Y (2014) Clinical factors predicting outcomes after surgical resection for sporadic cerebellar hemangioblastomas. World Neurosurg 82:815–821. https://doi.org/10.1016/j.wneu.2014.06.018
Giammattei L, Messerer M, Aghakhani N, David P, Herbrecht A, Richard S, Parker F (2016) Surgical resection of medulla oblongata hemangioblastomas: outcome and complications. Acta Neurochir 158:1333–1341. https://doi.org/10.1007/s00701-016-2834-0
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. Bmj 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Hussein MR (2007) Central nervous system capillary haemangioblastoma: the pathologist's viewpoint. Int J Exp Pathol 88:311–324. https://doi.org/10.1111/j.1365-2613.2007.00535.x
Joseph J, Behari S, Gupta S, Bhaisora KS, Gandhi A, Srivastava A, Jaiswal AK (2018) Brain-stem hemangioblastomas: the seemingly innocuous lesion in a perilous location. Neurol India 66:779–796. https://doi.org/10.4103/0028-3886.232294
Kano H, Niranjan A, Mongia S, Kondziolka D, Flickinger JC, Lunsford LD (2008) The role of stereotactic radiosurgery for intracranial hemangioblastomas. Neurosurgery 63:443–450; discussion 450-441. https://doi.org/10.1227/01.Neu.0000313120.81565.D7
Liu X, Zhang Y, Hui X, You C, Yuan F, Chen W, Zhang S (2015) Surgical management of medulla oblongata hemangioblastomas in one institution: an analysis of 62 cases. Int J Clin Exp Med 8:5576–5590
Lonser RR, Glenn GM, Walther M, Chew EY, Libutti SK, Linehan WM, Oldfield EH (2003) von Hippel-Lindau disease. Lancet 361:2059–2067. https://doi.org/10.1016/s0140-6736(03)13643-4
Ma D, Wang Y, Du G, Zhou L (2015) Neurosurgical management of brainstem hemangioblastomas: a single-institution experience with 116 patients. World Neurosurg 84:1030–1038. https://doi.org/10.1016/j.wneu.2015.05.030
Mandigo CE, Ogden AT, Angevine PD, McCormick PC (2009) Operative management of spinal hemangioblastoma. Neurosurgery 65:1166–1177. https://doi.org/10.1227/01.Neu.0000359306.74674.C4
McCormick PC, Torres R, Post KD, Stein BM (1990) Intramedullary ependymoma of the spinal cord. J Neurosurg 72:523–532. https://doi.org/10.3171/jns.1990.72.4.0523
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Pan J, Jabarkheel R, Huang Y, Ho A, Chang SD (2018) Stereotactic radiosurgery for central nervous system hemangioblastoma: systematic review and meta-analysis. J Neuro-Oncol 137:11–22. https://doi.org/10.1007/s11060-017-2697-0
Pavesi G, Berlucchi S, Munari M, Manara R, Scienza R, Opocher G (2010) Clinical and surgical features of lower brain stem hemangioblastomas in von Hippel-Lindau disease. Acta Neurochir 152:287–292. https://doi.org/10.1007/s00701-009-0512-1
Resche F, Moisan JP, Mantoura J, de Kersaint-Gilly A, Andre MJ, Perrin-Resche I, Menegalli-Boggelli D, Lajat Y, Richard S (1993) Haemangioblastoma, haemangioblastomatosis, and von Hippel-Lindau disease. Adv Tech Stand Neurosurg 20:197–304
Roberti F, Jones RV, Wright DC (2007) Cranial nerve hemangioblastomas. Report of a rare case and review of literature. Surg Neurol 67:640–646; discussion 646. https://doi.org/10.1016/j.surneu.2006.08.085
Santamarta D, Blazquez JA, Maillo A, Munoz A, Caballero M, Morales F (2003) Analysis of cerebrospinal fluid related complications (hydrocephalus, fistula, pseudomeningocele and infection) following surgery for posterior fossa tumors. Neurocirugia (Astur) 14:117–126
Schag CC, Heinrich RL, Ganz PA (1984) Karnofsky performance status revisited: reliability, validity, and guidelines. J Clin Oncol 2:187–193. https://doi.org/10.1200/jco.1984.2.3.187
Sedgwick P (2015) Meta-analyses: what is heterogeneity? Bmj 350:h1435. https://doi.org/10.1136/bmj.h1435
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
Smalley SR, Schomberg PJ, Earle JD, Laws ER Jr, Scheithauer BW, O'Fallon JR (1990) Radiotherapeutic considerations in the treatment of hemangioblastomas of the central nervous system. Int J Radiat Oncol Biol Phys 18:1165–1171. https://doi.org/10.1016/0360-3016(90)90454-r
Sterne JA, Egger M (2001) Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol 54:1046–1055. https://doi.org/10.1016/s0895-4356(01)00377-8
Tago M, Terahara A, Shin M, Maruyama K, Kurita H, Nakagawa K, Ohtomo K (2005) Gamma knife surgery for hemangioblastomas. J Neurosurg 102(Suppl):171–174. https://doi.org/10.3171/jns.2005.102.s_supplement.0171
Wanebo JE, Lonser RR, Glenn GM, Oldfield EH (2003) The natural history of hemangioblastomas of the central nervous system in patients with von Hippel-Lindau disease. J Neurosurg 98:82–94. https://doi.org/10.3171/jns.2003.98.1.0082
Wang C, Zhang J, Liu A, Sun B (2001) Surgical management of medullary hemangioblastoma. Report of 47 cases. Surg Neurol 56:218–226; discussion 226-217. https://doi.org/10.1016/s0090-3019(01)00590-0
Weil RJ, Lonser RR, DeVroom HL, Wanebo JE, Oldfield EH (2003) Surgical management of brainstem hemangioblastomas in patients with von Hippel-Lindau disease. J Neurosurg 98:95–105. https://doi.org/10.3171/jns.2003.98.1.0095
Wind JJ, Bakhtian KD, Sweet JA, Mehta GU, Thawani JP, Asthagiri AR, Oldfield EH, Lonser RR (2011) Long-term outcome after resection of brainstem hemangioblastomas in von Hippel-Lindau disease. J Neurosurg 114:1312–1318. https://doi.org/10.3171/2010.9.Jns10839
Wu P, Liang C, Wang Y, Guo Z, Li B, Qiu B, Li X, Wen Z, Pan Q (2013) Microneurosurgery in combination with endovascular embolisation in the treatment of solid haemangioblastoma in the dorsal medulla oblongata. Clin Neurol Neurosurg 115:651–657. https://doi.org/10.1016/j.clineuro.2012.07.026
Xu QW, Xu R, Du ZY, Gao X (2010) Surgical treatment for hemangioblastomas in the medulla oblongata. Acta Neurochir 152:1331–1335. https://doi.org/10.1007/s00701-010-0668-8
Yin L, Zhang L, Hao S, Zhang J, Wu Z (2014) Medullary hemangioblastoma: 34 patients at a single institution. J Clin Neurosci 21:250–255. https://doi.org/10.1016/j.jocn.2013.03.037
Young S, Richardson AE (1987) Solid haemangioblastomas of the posterior fossa: radiological features and results of surgery. J Neurol Neurosurg Psychiatry 50:155–158. https://doi.org/10.1136/jnnp.50.2.155
Zhou LF, Du GH, Mao Y, Zhang R (2005) Diagnosis and surgical treatment of brainstem hemangioblastomas. Surg Neurol 63:307–315. https://doi.org/10.1016/j.surneu.2004.07.038
Funding
This work was supported by the Chinese National Nature Science Foundation (Grant No. 81541119) and Peking University First Hospital Cross Clinical Study Foundation.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors, and written informed consent was not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yin, X., Li, C., Li, L. et al. Safety and efficacy of surgical treatment for brainstem hemangioblastoma: a meta-analysis. Neurosurg Rev 44, 799–806 (2021). https://doi.org/10.1007/s10143-020-01305-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-020-01305-3