Abstract
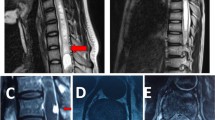
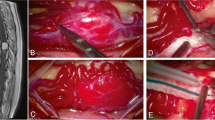
Hemangioblastomas are highly vascularised tumors of the central nervous system and account for 1.5–2.5% of all spinal cord tumors. Because of the rarity of these tumors, surgical experience is often limited and, therefore, treatment and indications for timing of surgery are discussed controversial. The authors reviewed their data of 23 consecutive patients with respect to timing of surgery, microsurgical technique, and follow-up. Clinical records of 23 consecutive patients with intramedullary hemangioblastomas who underwent first surgery in our department between 1990 and 2005 were reviewed. In three cases the tumors were localised at the craniocervical junction; four patients had a single tumor in the cervical spine, six patients multiple tumors in the cervical and thoracic spine, eight patients in the thoracic spine only, one patient in the conus region, and one patient had multiple tumors located in the thoracic and lumbar spine. In eight patients, a von-Hippel-Lindau disease (VHL) was associated. The neurological follow-up was evaluated according to the classification of McCormick. Operation was recommended to every symptomatic patient as early as possible. In asymptomatic patients with a sporadic tumor surgery was discussed for diagnostic purposes at any time. In VHL patients, surgery was recommended if tumor growth was observed on MRI in the next practicable time. All tumors were diagnosed by magnetic resonance imaging and in all cases but one a DSA was performed. All patients were treated microsurgically through a posterior approach. The tumors in the spinal cord were removed microsurgically through a partial hemilaminectomy (n = 1), a hemilaminectomy (n = 15), or laminectomy (n = 4) and at the craniocervical junction (n = 3) through a suboccipital craniotomy. During follow-up after 6 months, 18 patients remained neurologically stable (17 in McCormick grade I and 1 in McCormick grade II) and 5 patients recovered to a better status (3 from grade III to II, 2 from grade II to I). There was one complication with a CSF fistula and one recurrence/incomplete removal. Following the above-mentioned principles of microsurgical removal of intramedullary hemangioblastomas, operation is possible with a low procedure-related morbidity and can be recommended especially in VHL patients with progressive symptoms or tumor growth during follow-up. Patients without VHL most frequently require hemangioblastoma resection for diagnostic purposes and/or because symptoms prompted an imaging work-up that lead to the discovery of the tumor.



Similar content being viewed by others
References
Chu BC, Terae S, Hida K, Furukawa M, Abe S, Miyasaka K (2001) MR findings in spinal hemangioblastoma: correlation with symptoms and with angiographic and surgical findings. AJNR Am J Neuroradiol 22:206–217
Isu T, Abe H, Iwasaki Y, Akino M, Koyanagi I, Hida K, Miyasaka K, Saito H (1991) Diagnosis and surgical treatment of spinal hemangioblastoma. No Shinkei Geka 19:149–155
Malis LI (2002) Atraumatic bloodless removal of intramedullary hemangioblastomas of the spinal cord. J Neurosurg 97:1–6
McCormick PC, Torres R, Post KD, Stein BM (1990) Intramedullary ependymoma of the spinal cord. J Neurosurg 72:523–532
Neumann HP, Eggert HR, Weigel K, Friedburg H, Wiestler OD, Schollmeyer P (1989) Hemangioblastomas of the central nervous system. A 10-year study with special reference to von Hippel-Lindau syndrome. J Neurosurg 70:24–30
Rengachary SS, Blount JP (1996) Hemangioblastomas. In: Wilkins RH, Rengachary SS (eds) Neurosurgery. McGraw-Hill, New York, pp 1205–1219
Samii M, Klekamp J (1994) Surgical results of 100 intramedullary tumors in relation to accompanying syringomyelia. Neurosurgery 35:865–873, discussion 873
Seifert V, Trost HA, Stolke D (1990) Microsurgery of spinal angioblastoma. Neurochirurgia (Stuttg) 33:100–105
Trost HA, Seifert V, Stolke D (1993) Advances in diagnosis and treatment of spinal hemangioblastomas. Neurosurg Rev 16:205–209
Van Velthoven V, Reinacher PC, Klisch J, Neumann HP, Glasker S (2003) Treatment of intramedullary hemangioblastomas, with special attention to von Hippel-Lindau disease. Neurosurgery 53:1306–1313, discussion 1313–1304
Wu TC, Guo WY, Lirng JF, Wong TT, Chang FC, Luo CB, Teng MM, Chang CY (2005) Spinal cord hemangioblastoma with extensive syringomyelia. J Chin Med Assoc 68:40–44
Yasargil MG, Antic J, Laciga R, de Preux J, Fideler RW, Boone SC (1976) The microsurgical removal of intramedullary spinal hemangioblastomas. Report of twelve cases and a review of the literature. Surg Neurol 3:141–148
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boström, A., Hans, FJ., Reinacher, P.C. et al. Intramedullary hemangioblastomas: timing of surgery, microsurgical technique and follow-up in 23 patients. Eur Spine J 17, 882–886 (2008). https://doi.org/10.1007/s00586-008-0658-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-008-0658-1