Abstract
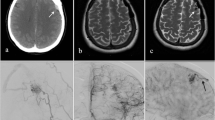
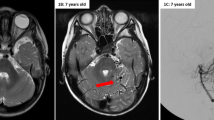
De novo intracerebral arteriovenous malformations (AVMs) are exceedingly rare with only seven reported cases in the literature. Although generally considered congenital by nature, the lesions do not manifest themselves clinically until the third or fourth decades of life. However, with the advent of improved imaging modalities and more frequent surveillance, an increasing number of de novo cases are being found challenging the concept AVMs develop in the perinatal/antenatal period. Alternatively, this phenomenon could represent a distinct entity in which lesion development occurs after birth. A PubMed search of “de novo cerebral arteriovenous malformation” was performed in which seven reported cases were found. The mean age at diagnosis was 14.7 years with a mean follow-up imaging study of 5.8 years. Lesion location was supratentorial in all previously described cases. This case involves an 18-year-old male with congenital hydrocephalus and seizures diagnosed at 7 months of age. The patient underwent a ventriculoperitoneal shunt and was followed frequently by a neurologist. The last diagnostic imaging was an unremarkable MRI of the brain at age 12. Seven years later, the patient presented with an intracerebral hemorrhage. A CT angiogram demonstrated a large brainstem AVM with an intraparenchymal hemorrhage and intraventricular extension. This case is unique in that it is the first infratentorial de novo AVM. The congenital nature of AVMs is challenged with the increasingly described series of patients with previously documented normal radiographic imaging. This suggests there may be a subset of patients genetically predisposed to postnatal development of AVMs.






Similar content being viewed by others
References
Abdalla SA, Letarte M (2006) Hereditary haemorrhagic telangiectasia: current views on genetics and mechanisms of disease. J Med Genet 43(2):97–110. doi:10.1136/jmg.2005.030833
Abdulrauf SI, Malik GM, Awad IA (1999) Spontaneous angiographic obliteration of cerebral arteriovenous malformations. Neurosurgery 44(2):280–287, discussion 287–288
Akimoto H, Komatsu K, Kubota Y (2003) Symptomatic de novo arteriovenous malformation appearing 17 years after the resection of two other arteriovenous malformations in childhood: case report. Neurosurgery 52(1):228–231, discussion 231–222
Alvarez H, Perry V, Solle M, Castillo M (2012) De novo cerebral arteriovenous malformation in a child with previous cavernous malformation and developmental venous anomaly. J Neurosurg Pediatr 9(3):327–330. doi:10.3171/2011.12.PEDS11312
Bulsara KR, Alexander MJ, Villavicencio AT, Graffagnino C (2002) De novo cerebral arteriovenous malformation: case report. Neurosurgery 50(5):1137–1140, discussion 1140–1131
Chen Y, Zhu W, Bollen AW, Lawton MT, Barbaro NM, Dowd CF, Hashimoto T, Yang GY, Young WL (2008) Evidence of inflammatory cell involvement in brain arteriovenous malformations. Neurosurgery 62(6):1340–1349. doi:10.1227/01.neu.0000333306.64683.b5, discussion 1349–1350
Garcin B, Houdart E, Porcher R, Manchon E, Saint-Maurice JP, Bresson D, Stapf C (2012) Epileptic seizures at initial presentation in patients with brain arteriovenous malformation. Neurology 78(9):626–631. doi:10.1212/WNL.0b013e3182494d40
Geibprasert S, Pereira V, Krings T, Jiarakongmun P, Lasjaunias P, Pongpech S (2009) Hydrocephalus in unruptured brain arteriovenous malformations: pathomechanical considerations, therapeutic implications, and clinical course. J Neurosurg 110(3):500–507. doi:10.3171/2008.7.JNS0815
Gonzalez LF, Bristol RE, Porter RW, Spetzler RF (2005) De novo presentation of an arteriovenous malformation. Case report and review of the literature. J Neurosurg 102(4):726–729. doi:10.3171/jns.2005.102.4.0726
Hashimoto N, Nozaki K (1999) Do cerebral arteriovenous malformations recur after angiographically confirmed total extirpation? Crit Rev Neurosurg: CR 9(3):141–146
Kader A, Goodrich JT, Sonstein WJ, Stein BM, Carmel PW, Michelsen WJ (1996) Recurrent cerebral arteriovenous malformations after negative postoperative angiograms. J Neurosurg 85(1):14–18. doi:10.3171/jns.1996.85.1.0014
Kilic T, Pamir MN, Kullu S, Eren F, Ozek MM, Black PM (2000) Expression of structural proteins and angiogenic factors in cerebrovascular anomalies. Neurosurgery 46(5):1179–1191, discussion 1191–1172
Kim H, Sidney S, McCulloch CE, Poon KY, Singh V, Johnston SC, Ko NU, Achrol AS, Lawton MT, Higashida RT, Young WL, Project UBS (2007) Racial/ethnic differences in longitudinal risk of intracranial hemorrhage in brain arteriovenous malformation patients. Stroke: J Cereb Circ 38(9):2430–2437. doi:10.1161/STROKEAHA.107.485573
Kim H, Su H, Weinsheimer S, Pawlikowska L, Young WL (2011) Brain arteriovenous malformation pathogenesis: a response-to-injury paradigm. Acta neurochir Suppl 111:83–92. doi:10.1007/978-3-7091-0693-8_14
Kondziolka D, Humphreys RP, Hoffman HJ, Hendrick EB, Drake JM (1992) Arteriovenous malformations of the brain in children: a forty year experience. Can J Neurol Sci 19(1):40–45
Leblanc GG, Golanov E, Awad IA, Young WL, Biology of Vascular Malformations of the Brain NWC (2009) Biology of vascular malformations of the brain. Stroke: J Cereb Circ 40(12):e694–e702. doi:10.1161/STROKEAHA.109.563692
Mahajan A, Manchandia TC, Gould G, Bulsara KR (2010) De novo arteriovenous malformations: case report and review of the literature. Neurosurg Rev 33(1):115–119. doi:10.1007/s10143-009-0227-z
Marchuk DA, Srinivasan S, Squire TL, Zawistowski JS (2003) Vascular morphogenesis: tales of two syndromes. Hum Mol Genet 12(1):R97–R112
Mullan S, Mojtahedi S, Johnson DL, Macdonald RL (1996) Embryological basis of some aspects of cerebral vascular fistulas and malformations. J Neurosurg 85(1):1–8. doi:10.3171/jns.1996.85.1.0001
O'Shaughnessy BA, DiPatri AJ Jr, Parkinson RJ, Batjer HH (2005) Development of a de novo cerebral arteriovenous malformation in a child with sickle cell disease and moyamoya arteriopathy. Case report. J Neurosurg 102(2 Suppl):238–243. doi:10.3171/jns.2005.102.2.0238
Schmit BP, Burrows PE, Kuban K, Goumnerova L, Scott RM (1996) Acquired cerebral arteriovenous malformation in a child with moyamoya disease. Case report. J Neurosurg 84(4):677–680. doi:10.3171/jns.1996.84.4.0677
Stevens J, Leach JL, Abruzzo T, Jones BV (2009) De novo cerebral arteriovenous malformation: case report and literature review. AJNR Am J Neuroradiol 30(1):111–112. doi:10.3174/ajnr.A1255
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke:J Cereb Circ 19(5):604–607
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Martin M. Mortazavi and Louis J. Kim, Seattle, USA
With an average annual risk of bleeding of 2–4 %, arteriovenous malformations (AVM) account for 3 % of hemorrhagic strokes and 9 % of subarachnoid hemorrhage [1]. They represent the most common cause of childhood hemorrhagic stroke [2]. Infratentorial AVMs are uncommon, comprise less than 15 % of all cerebral AVMs, and are associated with higher annual risk of hemorrhage, reaching up to 11 % [3, 4].
Up to our knowledge, eight cases of acquired AVM have been reported in the literature thus far [5–12]. More cases are expected due to the advancement of neuroimaging. In all of these cases, the malformation has developed in the supratentorial area. The interesting finding of infratentorial de novo AVM reported in the current article is therefore unique.
The etiology of AVM is still unknown. The early theory of a static congenital malformation of solely genetic origin has been questioned with the reported cases of de novo AVM and AVM recurrence after successful treatment. Therefore, later studies have suggested that acquired somatic conditions including trauma, inflammation, and radiation are potentially involved, and they may represent a second hit for de novo AVM development [2, 13]. This may also explain the occurrence of AVM in certain vascular territory and absence in another, in a genetically predisposed patient. However, this theory was only tested on mice, and no genetic studies were performed on patients with de novo AVM to date. Certain genes have been associated with AVM and well documented in this current manuscript. The incidence of a “second hit” is interesting as there is a potential parallel in hereditary hemorrhagic telangiectasia (HHT). Park et al. [13] reported de novo subdermal AVM formation following wounding of an activin receptor-like kinase-1 (ALK-1)-deficient mouse. ALK-1 is a transforming growth factor-β (TGF-β) receptor protein that inhibits the TGF-β-induced vascular endothelial growth factor (VEGF) expression in endothelial cells, and its deficiency is one of the main underlying causes of a “second hit,” in this case, the wound itself that could induce the release of multiple angiogenic factors, including VEGF, which potentially could lead to local AVM formation [13].
It must again be noted that none of reported cases of de novo AVM were for patients with HHT, and unique molecular mechanism is, therefore, sought after.
At our institution, the treatment approach to brainstem AVMs is dictated by the accessibility and size of the lesion. In general, Spetzler–Martin grade 3 lesions are suitable for resection. For grade 4 and 5 AVMs, treatment is conservative or radiosurgery. In our experience, the specific location within the brainstem and degree of surgical accessibility greatly influences the likelihood of surgical success without permanent neurological morbidity.
References
1. Mortazavi MM et al (2013) Long-term control of large pontine arteriovenous malformation using gamma knife therapy: a review with illustrative case. Brain Behav 3(4): 329–334
2. Achrol AS et al (2009) Pathogenesis and radiobiology of brain arteriovenous malformations: implications for risk stratification in natural history and posttreatment course. Neurosurg Focus 26(5): E9
3. Arnaout OM et al (2009) Posterior fossa arteriovenous malformations. Neurosurg Focus 26(5): E12
4. Stapf C et al (2006) Predictors of hemorrhage in patients with untreated brain arteriovenous malformation. Neurology. 66(9): 1350–5
5. Alvarez H et al (2012) De novo cerebral arteriovenous malformation in a child with previous cavernous malformation and developmental venous anomaly. J Neurosurg Pediatr 9(3): 327–30
6. Bulsara KR et al (2002) De novo cerebral arteriovenous malformation: case report. Neurosurgery 50(5): 1137–40; discussion 1140–1
7. Gonzalez LF et al (2005) De novo presentation of an arteriovenous malformation. Case report and review of the literature. J Neurosurg 102(4): 726–9
8. Mathon B et al (2013) De novo arteriovenous malformation after brain radiotherapy for medulloblastoma in a child. Neurology 81(4): 398–9
9. O’Shaughnessy BA et al (2005) Development of a de novo cerebral arteriovenous malformation in a child with sickle cell disease and moyamoya arteriopathy. Case report. J Neurosurg 102(2 Suppl): 238–43
10. Schmit BP et al (1996) Acquired cerebral arteriovenous malformation in a child with moyamoya disease. Case report. J Neurosurg 84(4): 677–80
11. Stevens J et al (2009) De novo cerebral arteriovenous malformation: case report and literature review. AJNR Am J Neuroradiol 30(1): 111–2
12. Mahajan A et al (2010) De novo arteriovenous malformations: case report and review of the literature. Neurosurg Rev 33(1): 115–9
13. Park SO et al (2009) Real-time imaging of de novo arteriovenous malformation in a mouse model of hereditary hemorrhagic telangiectasia. J Clin Invest 119(11): 3487–96
Oliver Müller and Ulrich Sure, Essen, Germany
Kilbourn et al. report on the first de novo AVM of the posterior fossa, so far. De novo AVMs are indeed exceptional occurrences with respect to this latest review. Scarce information is available on the incidence of brain AVMs. Large prospective studies estimated an incidence of brain AVMs of 1.3 per 100,000 person-years with a cumulative bleeding risk of 0.51 [1]. On the other hand, a large study on incidental MRI findings did not detect any brain AVMs among 2,000 scans [2]. With this in mind, the present report should inspire us to dig even deeper into the potential biology of brain AVMs.
Are AVMs hereditary, connatal, or acquired lesions? Several studies have uncovered proliferative and neoangiogenetic abilities within the AVM vasculature [3–6] that might even be induced by previous partial treatment. Are AVMs benign vascular tumors rather than true malformations?
ARUBA has told us that medical treatment is superior to medical treatment and intervention over a (too short for a benign tumor or malformation) 33-month period in unruptured AVMs [7]. However, this conclusion must be discussed highly controversially since 87 % of the malformations (assessed for eligibility) were excluded from statistical analysis in this prospective study. In the treatment arm group, the vast majority of patients was not treated surgically (more than 80 %), suggesting that these AVMs were only occluded partially with all potential risk of a remaining nidus. If future research reveals a more aggressive growth behavior as shown in de novo AVMs, this finding will furthermore downsize the significance of the results of the ARUBA study which was designed under the assumption that AVMs are rather stable non-neoplastic non-growing lesions.
Therefore, the present well-documented case is an important contribution to the literature.
References
1. Stapf C et al (2003) The New York Islands AVM Study: design, study progress, and initial results. Stroke 34(5): e29–33
2. Vernooij MW et al (2007) Incidental findings on brain MRI in the general population. N Engl J Med 357(18): 1821–8
3. Rothbart D et al (1996) Expression of angiogenic factors and structural proteins in central nervous system vascular malformations. Neurosurgery 38(5): 915–24; discussion 924–5
4. Kilic T et al (2000) Expression of structural proteins and angiogenic factors in cerebrovascular anomalies. Neurosurgery 46(5): 1179–91; discussion 1191–2
5. Sure U et al (2001) Treatment-induced neoangiogenesis in cerebral arteriovenous malformations. Clin Neurol Neurosurg 103(1): 29–32
6. Sandalcioglu IE et al (2010) Proliferation activity is significantly elevated in partially embolized cerebral arteriovenous malformations. Cerebrovasc Dis 30(4): 396–401
7. Mohr JP et al (2014) Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, non-blinded, randomised trial. Lancet 383(9917): 614–21
Rights and permissions
About this article
Cite this article
Kilbourn, K.J., Spiegel, G., Killory, B.D. et al. Case report of a de novo brainstem arteriovenous malformation in an 18-year-old male and review of the literature. Neurosurg Rev 37, 685–691 (2014). https://doi.org/10.1007/s10143-014-0557-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-014-0557-3