Abstract
Background
KIT is frequently mutated in gastrointestinal stromal tumors (GISTs), and the treatment of GISTs largely relies on targeting KIT currently. In this study, we aimed to investigate the role of sprouty RTK signaling antagonist 4 (SPRY4) in GISTs and related mechanisms.
Methods
Ba/F3 cells and GIST-T1 cell were used as cell models, and mice carrying germline KIT/V558A mutation were used as animal model. Gene expression was examined by qRT-PCR and western blot. Protein association was examined by immunoprecipitation.
Results
Our study revealed that KIT increased the expression of SPRY4 in GISTs. SPRY4 was found to bind to both wild-type KIT and primary KIT mutants in GISTs, and inhibited KIT expression and activation, leading to decreased cell survival and proliferation mediated by KIT. We also observed that inhibition of SPRY4 expression in KITV558A/WT mice led to increased tumorigenesis of GISTs in vivo. Moreover, our results demonstrated that SPRY4 enhanced the inhibitory effect of imatinib on the activation of primary KIT mutants, as well as on cell proliferation and survival mediated by the primary KIT mutants. However, in contrast to this, SPRY4 did not affect the expression and activation of drug-resistant secondary KIT mutants, nor did it affect the sensitivity of secondary KIT mutants to imatinib. These findings suggested that secondary KIT mutants regulate a different downstream signaling cascade than primary KIT mutants.
Conclusions
Our results suggested that SPRY4 acts as negative feedback of primary KIT mutants in GISTs by inhibiting KIT expression and activation. It can increase the sensitivity of primary KIT mutants to imatinib. In contrast, secondary KIT mutants are resistant to the inhibition of SPRY4.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The type III receptor tyrosine kinase KIT is the receptor for stem cell factor (SCF). It belongs to the same receptor family together with FLT3, PDGFR, and CSF-1 receptor [1, 2]. Wild-type KIT is expressed as a monomer on the cell surface. Upon binding to SCF, KIT dimerizes, and its tyrosine kinase activity is activated, leading to the tyrosine phosphorylation of KIT which can further recruit and activate downstream signaling pathways, such as RAS/RAF/MEK/ERK and PI3 kinase/AKT, to mediate cell survival, proliferation, and differentiation. Gain-of-function mutations of KIT are a group of substitution mutations, deletion mutations, or duplication mutations of KIT that occur in malignancies, such as gastrointestinal stromal tumors (GISTs), mastocytosis, and acute myeloid leukemia. These mutations induce ligand-independent activation of KIT, leading to cell transformation [2, 3].
GISTs are mesenchymal tumors that usually arise in the stomach or small intestine. They can also be found in the other parts of the digestive tract but with less frequency [4]. Surgical removal is efficient in the treatment of primary, non-metastatic GISTs, while high-risk GISTs and those with metastasis need targeted therapy against KIT [5, 6]. Currently, several KIT inhibitors including imatinib, sunitinib, regorafinib, and ripretinib have been approved as first-, second-, third-, and fourth-line targeted therapy of GISTs respectively, and have dramatically improved treatment outcomes [7,8,9,10]. Of those, imatinib has been shown to improve patient survival for years, while sunitinib, regorafinib, and ripretinib can only improve patient survival for few months. The relapse often occurs due to gaining drug-resistant secondary mutation of KIT [11,12,13,14] or activation of alternative signaling pathways by GISTs [15, 16].
Sprouty RTK signaling antagonist 4 (SPRY4) is highly expressed in GISTs, as reported previously [17], but its exact role and the underlying mechanism remain elusive. In this study, we found that SPRY4 associated with KIT, and inhibited the expression and activation of both wild-type KIT and primary KIT mutants, but not secondary KIT mutants. Furthermore, we found that the presence of SPRY4 increased the sensitivity of primary KIT mutants but not secondary KIT mutants to imatinib, suggesting that SPRY4 plays a key role in the oncogenesis of GISTs mediated by KIT mutants, and in the response of GISTs to imatinib treatment.
Materials and methods
Cytokine, antibodies, and inhibitor
SPRY4 antibody, AKT antibody, phosphor-ERK (T202/Y204) antibody, ERK antibody, HRP-conjugated goat anti-rabbit IgG antibody, HRP-conjugated donkey anti-goat IgG antibody, HRP-conjugated goat anti-mouse IgG antibody, and HRP-conjugated β-actin antibody were purchased from Santa Cruz Biotechnology (Dallas, TX). Anti-KIT antibody was purified as previously described [18] by Gene-van Biology (Beijing, China). PE-conjugated anti-KIT antibody was purchased from Biolegend (San Diego, CA). Anti-pY antibody 4G10 and chemiluminescent HRP substrate were purchased from Millipore (Billerica, MA). Phosphor-AKT (S473) antibody was purchased from Cell Signaling Technology (Danvers, MA). Recombinant human stem cell factor (SCF) was purchased from ORF Genetics (Kópavogur, Iceland). KIT inhibitor imatinib was purchased from MedChemExpress (Monmouth Junction, NJ).
Cell culture
Ba/F3 cells (DSMZ) were grown in RPMI 1640 medium supplemented with 100 units/ml penicillin, 100 μg/ml streptomycin, 10 ng/ml recombinant murine IL-3, and 10% heat-inactivated fetal bovine serum. EcoPack cells (Clontech) and GIST-T1 cells (Cosmo) were grown in DMEM medium supplemented with 10% fetal bovine serum, 100 units/ml penicillin, and 100 μg/ml streptomycin.
Construction of SPRY4 expressing plasmid and cell lines
Human SPRY4 cDNA with FLAG tag at 3’ end was synthesized and inserted into the retroviral vector pMSCVneo. In order to establish Ba/F3 cells stably expressing KIT and SPRY4, EcoPack cells were transfected with pMSCVneo/SPRY4 using lipofactamine 2000 (Thermo Fisher Scientific) according to the manufacturer’s instruction, supernatants were used to infect Ba/F3 cells expressing wild-type KIT and KIT mutants that were established before [19], followed by selection with 1 mg/ml neomycin for two weeks. The expression of SPRY4 was examined by western blot.
Cell stimulation, immunoprecipitation, and western blot
Ba/F3 cells were washed with PBS and starved in RPMI 1640 medium without serum and IL-3 in the cell incubator for 4 h, followed by SCF stimulation (100 ng/ml) at 37 ℃ for 2 min. After washing with ice-cold PBS, cells were lysed in a lysis buffer containing 1% Triton X-100, 25 mM Tris, pH 7.5, 150 mM NaCl, 5 mM EDTA, 10% glycerol, 2 mg/ml aprotinin, 1 mM Na3VO4, and 1 mM phenylmethylsulfonyl fluoride on ice for 15 min. Cell lysates were centrifuged at 12,000 rpm for 15 min at 4 ℃ and the supernatants were proceeded for immunoprecipitation or mixed with SDS-PAGE loading buffer and proceeded for western blot analysis. For immunoprecipitation, cell lysates were incubated end-over-end with indicated antibody for 1 h at 4 ℃ followed by incubation with Dynabeads™ protein G (Thermo Fisher Scientific) for 30 min at 4 ℃. The immunoprecipitates were washed with lysis buffer, mixed with SDS-PAGE loading buffer, and boiled for 5 min, followed by separation by SDS-PAGE and electro-transfer to PVDF membranes (Millipore). The membranes were blocked in PBS with 0.2% tween-20 (PBST) for 1 h at room temperature and then incubated with indicated primary antibody at 4 ℃ overnight. After washing with PBST, the membranes were incubated with HRP-conjugated secondary antibody at room temperature for 2 h. The membranes were washed with PBST and developed with chemiluminescent HRP substrate (Millipore).
GIST-T1 cells were washed with PBS and starved in DMEM medium without serum for 4 h in the cell incubator, followed by cell lysis and further proceeding as aforementioned.
Cell survival, proliferation, and cell cycle assay
Ba/F3 cells were washed with PBS, and grown in Ba/F3 growth medium without IL-3 but with 100 ng/ml SCF or no cytokine as control, or other treatment as indicated. After incubation for 72 h, cells were stained with PE annexin V apoptosis detection kit (BD Biosciences), and cell apoptosis was analyzed by flow cytometry. Cell proliferation in 96-well plates was examined by CCK8 kit (AbMole) according to the manufacturer’s instruction. For cell cycle assay, cells were stained with PI reagent (Keygen Biotech) and examined by flow cytometry.
GIST-T1 cells were treated as indicated and incubated in the cell incubator for 72 h. Cells were trypsinized and stained with PE annexin V apoptosis detection kit to detect apoptotic cells by flow cytometry. For cell cycle assay, cells were trypsinized, stained with PI reagent, and examined by flow cytometry. Cell proliferation in 96-well plates was examined by CCK8 kit (AbMole).
siRNAs and transfection
KIT siRNA (GGAUGGCACCUGAAAGCAUTT) and SPRY4 siRNA (GAGGCCTGTGGAAAGTGTAAGTGCA) were synthesized by Genepharma (Shanghai, China). GIST-T1 cells were transfected with indicated siRNA (50 nM) using Lipofectamine 2000 (Thermo Fisher Scientific) according to the manufacturer’s instructions. After incubation for 48 h, the expression of target genes or signal transduction was examined. Lentivirus expressing SPRY4 siRNA was constructed by Sheweisi (Tianjin, China).
RNA extraction and qRT-PCR
Total RNA was extracted from cells or tissues using RNAsimple Total RNA kit (Tiangen, China) followed by reverse transcription into cDNA using Reverse Transcription Kit (Takara, China). The relative expression of target genes was examined by real-time PCR using a two-step real-time RT-PCR kit (Takaka, Japan) with the program: 95 °C for 30 s followed by 40 cycles of 95 °C for 5 s, 60 °C for 34 s. RPL19 was used as the control. Primers are listed in Table 1.
Examination of KIT expression by flow cytometry
Ba/F3 cells were washed with PBS and incubated with PE-conjugated anti-KIT antibody in the dark at room temperature for 30 min, after washing with PBS, the cells were re-suspended in PBS, and KIT expression was analyzed by flow cytometry.
Animal experiments
Animal experiments were approved by the Ethics Committee of Ningxia Medical University. All mice were housed in a temperature-controlled room on a normal 12-h light–dark cycle with ad libitum access to food and water. C57BL/6N mice carrying germline KIT/V558A mutation were established by Cyagen Biosciences using CRISPR/Cas9-mediated genome engineering. Cas9 mRNA, gRNAs (AGTACAATGGAAGGTTGTCGAGG, CTTCCATTGTACTTCATACATGG, AGTACAATGGAAGGTTGTCGAGG), and donor oligo with V558A (GTT to GCC) mutation were generated by in vitro transcription and co-injected into fertilized eggs. After birth, the genotypes of the mice were examined, and KITV558A/WT mice were crossed with wild-type C57BL/6N mice to establish stable KITV558A/WT mice. KIT V558A/WT mice of 8-week-old were intraperitoneally injected with lentivirus expressing SPRY siRNA (3 days before imatinib treatment, twice a week, 3 days apart, each time 5 nmol), and/or treated with Imatinib at a dose of 50 mg/kg by intra-gastric administration daily. After treatment for 8 days, tumor sizes and volumes were measured, and tumor tissues were further analyzed by western blot or qRT-PCR.
Statistical analysis
Results were expressed as mean ± standard deviation of three independent experiments. Graphpad was used for statistical analysis. Multiple comparisons were analyzed by one-way ANOVA, and comparisons between two groups were analyzed by the t test, p < 0.05 is considered as significant.
Results
SPRY4 inhibits the expression of both wild-type KIT and primary KIT mutants in GISTs
SPRY4 is known to be highly expressed in GISTs [17]. In this study, we treated GISTs cell GIST-T1, which carries endogenous primary KIT mutant, with KIT inhibitor imatinib, which is used as the first-line targeted therapy of GISTs, or knocked-down KIT expression by siRNA transfection. We observed that both imatinib treatment and KIT siRNA transfection inhibited both mRNA and protein expression of SPRY4 (Fig. 1A, B), indicating that KIT increased the expression of SPRY4, which is in agreement with previous report [20]. We further investigated the possible regulation of SPRY4 on KIT and its downstream signaling by establishing Ba/F3 cells stably expressing frequently occurred primary KIT mutants W557K558del or V560D in GISTs with or without SPRY4. Flow cytometry examination showed that the expression of KIT mutants in Ba/F3 cells was decreased in the presence of SPRY4, suggesting that SPRY4 can inhibit the expression of primary KIT mutants. Similarly, the expression of wild-type KIT was also inhibited by SPRY4 (Fig. 1C). To confirm this observation, we knocked down SPRY4 expression in GIST-T1 cells, and observed that KIT protein expression was increased, while KIT mRNA levels were unchanged (Fig. 1D), suggesting that SPRY4 can inhibit KIT expression at the protein level but not the mRNA level. Since KIT can increase SPRY4 expression, SPRY4 may serve as a negative feedback regulator of KIT in GISTs.
SPRY4 inhibits the expression of both wild-type KIT and primary KIT mutants in GISTs. A GIST-T1 cells were washed with PBS three times and incubated in DMEM with or without imatinib (1 μM) for 4 h in the cell incubator, or the cells were transfected with KIT siRNA using lipofectamine 2000. After 48 h, cells were starved in DMEM for 4 h. Total cell lysates (TCL) were probed with 4G10, KIT, SPRY4, pAKT, AKT, pERK, ERK, and β-actin antibodies, respectively; B GIST-T1 cells were treated with imatinib (1 μM) for 8 h, expression of KIT and SPRY4 was analyzed by qRT-PCR. C Ba/F3 cells expressing wild-type KIT, KIT/W557K558del, or KIT/V560D with or without SPRY4 were stained with PE-anti-KIT antibody, and KIT expression was analyzed by flow cytometry. Solid line: cells without SPRY4 expression, dotted line: cells with SPRY4 expression, empty area: isotype control, gray area: PE-anti-KIT antibody. D GIST-T1 cells were transfected with SPRY4 siRNA, and total cell lysates were analyzed by western blot using 4G10, KIT, pAKT, AKT, pERK, ERK, and β-actin antibodies, respectively. Total RNA was extracted from the cells, and mRNA expression of KIT and SPRY4 was quantified by qRT-PCR. E Ba/F3 cells expressing wild-type KIT, KIT/W557K558del, or KIT/V560D with or without SPRY4 were incubated in RPMI 1640 medium plus 2% serum and 100 ng/ml SCF for 12 h, followed by cell lysis and western blot analysis of the expression of KIT, SPRY4, and β-actin. KIT expression was quantified, and the decrease of KIT expression after SCF stimulation in each cell was calculated
In addition to the ligand-independent activation of KIT mutants, GISTs express SCF which can increase KIT activation by autocrine or paracrine loop [21, 22]. To investigate the role of SPRY4 in regulating KIT expression when KIT is constitutively activated by ligand stimulation, we treated Ba/F3 cells with SCF for 12 h. Our results showed that the expression of both wild-type KIT and primary KIT mutants decreased after stimulation with SCF for 12 h, while the presence of SPRY4 further decreased the expression of KIT (Fig. 1E). These findings indicated that SPRY4 inhibits KIT expression when they are constitutively activated.
SPRY4 associates with KIT and inhibits the activation of both wild-type KIT and primary KIT mutants and their downstream signaling molecules
Since SPRY4 inhibits KIT expression and has been reported to inhibit RAS/RAF/MEK/ERK signaling [23, 24], we investigated the regulation of SPRY4 on the activation of KIT and its downstream signaling. By immunoprecipitation, we found that SPRY4 associated with both wild-type KIT and primary KIT mutants in Ba/F3 cells. In addition, examination of KIT activation showed that the presence of SPRY4 inhibited the activation of both wild-type KIT and primary KIT mutants (Fig. 2A). In agreement with that in Ba/F3 cells, the association between SPRY4 and KIT was demonstrated in GIST-T1 cells as well by immunoprecipitation (Fig. 2B), and knockdown of SPRY4 expression in GIST-T1 cells increased KIT activation (Fig. 1D), further supporting the notion that SPRY4 associated with KIT and inhibited KIT activation. The activation of RAS/RAF/MEK/ERK and PI3 kinase/AKT signaling pathways plays important roles in KIT-mediated cell survival and proliferation [1,2,3], our results showed that the presence of SPRY4 inhibited activation of both ERK and AKT mediated by both wild-type KIT and primary KIT mutants in Ba/F3 cells (Fig. 2A). Similarly, knockdown of SPRY4 expression in GIST-T1 cells increased activation of both ERK and AKT (Fig. 1D), suggesting that SPRY4 plays a critical role in the activation of downstream signaling of KIT.
SPRY4 associates with KIT and inhibits the activation of both wild-type KIT and primary KIT mutants and downstream signaling. A Ba/F3 cells expressing wild-type KIT, KIT/W557K558del, or KIT/V560D with or without SPRY4 were starved, followed by stimulation with SCF, total cell lysates were probed with SPRY4, pAKT, AKT, pERK, ERK, and β-actin antibodies respectively. KIT was immunoprecipitated using KIT antibody from the cell lysates and probed with 4G10, KIT, and SPRY4 antibodies, respectively. The signal intensity of 4G10 was quantified and normalized by KIT, and the signal intensity of pAKT and pERK was quantified and normalized by β-actin. B GIST-T1 cells were transfected with SPRY4 siRNA, and KIT was immunoprecipitated using KIT antibody from the cell lysates and probed with KIT and SPRY4 antibodies, respectively
SPRY4 inhibits the tumorigenesis of GISTs mediated by KIT mutant
As SPRY4 inhibits KIT signaling, we further investigated the role of SPRY4 in KIT-mediated cell survival and proliferation in vitro. The results showed that the presence of SPRY4 inhibited the survival of Ba/F3 cells expressing either wild-type KIT or KIT mutants (Fig. 3A). Additionally, the presence of SPRY4 inhibited the cell cycle progression and proliferation of Ba/F3 cells expressing either wild-type KIT or primary KIT mutants (Fig. 3B, C). To validate these findings, the expression of SPRY4 was knocked down in GIST-T1 cells. Consistent with the results in Ba/F3 cells, inhibition of SPRY4 expression increased cell cycle progression, proliferation, and survival of GIST-T1 cells (Fig. 3D).
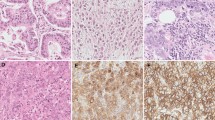
SPRY4 inhibits KIT mutant-mediated cell proliferation and survival of GISTs cells in vitro, and tumorigenesis of GISTs in vivo. A Ba/F3 cells expressing wild-type KIT, KIT/W557K558del, or KIT/V560D with or without SPRY4 were washed with PBS and re-suspended in Ba/F3 growth medium without IL-3 but with SCF or no cytokine as control. After 48 h, apoptotic cells were counted by flow cytometry after staining with PE annexin V apoptosis detection kit; B Cell growth was analyzed by CCK8 kit; C Cell cycle was analyzed by flow cytometry after staining with PI reagent. D GIST-T1 cells were transfected with SPRY4 siRNA, cell apoptosis, cell proliferation, and cell cycle were analyzed. E KITV558A/WT mice of 8 weeks old were intraperitoneally injected with lentivirus expressing SPRY4 siRNA, and/or treated with imatinib. After treatment, tumor size and weight were measured. F Tumors from mice were lysed, and the lysates were probed with KIT, SPRY4, and β-actin antibodies, respectively
To further investigate the role of SPRY4 in the tumorigenesis of GISTs in vivo, we injected lentivirus expressing SPRY4 siRNA into mice carrying germline KIT/V558A mutation, which is identical as human KIT/V559A mutation in familial GISTs [25], in order to knock down the expression of SPRY4. The results showed that injection of lentivirus expressing SPRY4 siRNA increased the tumor growth (Fig. 3E), suggesting that SPRY4 can inhibit the tumorigenesis of GISTs in vivo. In addition, imatinib treatment dramatically inhibited the tumor growth regardless of SPRY4 expression (Fig. 3E). Western blot analysis of tumor samples showed that knockdown of SPRY4 expression increased KIT expression, while inhibition of KIT activation by imatinib inhibited SPRY4 expression (Fig. 3F). These findings are consistent with the results in vitro, further suggesting that SPRY4 may serve as a negative feedback regulator of KIT in GISTs.
SPRY4 increases the sensitivity of primary KIT mutants to imatinib
Imatinib is the first-line targeted therapy for GISTs and has dramatically improved treatment outcomes [5, 7]. In this study, we investigated whether SPRY4 can regulate the response of GISTs to imatinib due to its important role in the regulation of the activation of KIT and downstream signaling. We treated Ba/F3 cells expressing KIT with various concentrations of imatinib and found that the presence of SPRY4 increased the inhibition of imatinib on the activation of both wild-type KIT and primary KIT mutants. Examination of the activation of downstream molecules ERK and AKT showed similar results (Fig. 4A). In the cell survival assay, the presence of SPRY4 further inhibited the survival of Ba/F3 cells expressing primary KIT mutants, but not wild-type KIT in addition to the inhibition by imatinib (Fig. 4B). Similarly, the inhibition of cell cycle progression and proliferation of Ba/F3 cells expressing both wild-type KIT and KIT mutants by imatinib was even stronger in the presence of SPRY4 (Fig. 4C, D). These results suggest that SPRY4 can increase the sensitivity of primary KIT mutants to imatinib.
SPRY4 increases the sensitivity of primary KIT mutants to imatinib. A Ba/F3 cells expressing wild-type KIT, KIT/W557K558del, or KIT/V560D with or without SPRY4 were washed and incubated with imatinib in RPMI 1640 medium for 4 h after stimulation with SCF, total cell lysates were probed with pAKT, AKT, pERK, ERK, and β-actin antibodies respectively. KIT was pulled down using KIT antibody from the cell lysates and probed with 4G10, KIT, and SPRY4 antibodies, respectively. The signal intensity of 4G10 was quantified and normalized by KIT. B Ba/F3 cells expressing wild-type KIT, KIT/W557K558del, or KIT/V560D with or without SPRY4 were washed with PBS and grown in Ba/F3 growth medium without IL-3 but with SCF, or with imatinib. After 48 h, apoptotic cells were counted by flow cytometry after staining with PE annexin V apoptosis detection kit; C Cell proliferation was analyzed by CCK8 kit; D Cell cycle was analyzed by flow cytometry after staining with PI reagent
The expression and activation of secondary KIT mutants are not altered by SPRY4
The application of targeted therapy against KIT in the clinic has dramatically improved the survival of GIST patients. However, gaining drug-resistant secondary mutation of KIT or activation of alternative signaling pathways can lead to treatment failure [11,12,13,14,15,16]. To investigate whether SPRY4 can inhibit secondary mutations of KIT, Ba/F3 cells expressing the commonly occurred secondary mutations of KIT with or without SPRY4 were established. Since the secondary mutations of KIT occur in the same chromosome as the primary KIT mutation [11, 12, 26], therefore KIT carries both primary mutation and secondary mutation of KIT when the latter mutation occurs. Examination of KIT expression showed that the expression of the often-occurred secondary KIT mutants W557K558del/V654A and W557K558del/N822K was not affected by SPRY4 (Fig. 5A), in contrast to the inhibited expression of wild-type KIT and primary KIT mutants by SPRY4 (Fig. 1C). When stimulated by SCF for an extended period to mimic the in vivo situation where GISTs express SCF which can activate KIT constitutively by autocrine or paracrine loop, the reduction of the expression of secondary KIT mutants showed no difference in the presence or absence of SPRY4 (Fig. 5B). Similar to the regulation of KIT expression by SPRY4, the activation of secondary KIT mutants and downstream signaling molecules ERK and AKT was not changed by SPRY4 although SPRY4 associates with secondary mutations of KIT (Fig. 5C). These findings suggest that the secondary KIT mutants were resistant to the inhibition of SPRY4, in contrast to the inhibition of the activation of wild-type KIT and primary KIT mutants by SPRY4.
SPRY4 associates with secondary KIT mutants but doesn’t change their expression and activation. A Ba/F3 cells expressing KIT/W557K558del/V654A or KIT/W557K558del/N822K with or without SPRY4 were stained with PE-anti-KIT antibody, and KIT expression was analyzed by flow cytometry. Solid line: cells without SPRY4 expression, dotted line: cells with SPRY4 expression, empty area: isotype control, gray area: PE-anti-KIT antibody. B Ba/F3 cells expressing KIT/W557K558del/V654A or KIT/W557K558del/N822K with or without SPRY4 were incubated in RPMI 1640 medium plus 2% serum and 100 ng/ml SCF for 12 h, followed by cell lysis and western blot analysis of the expression of KIT, SPRY4, and β-actin. KIT expression was quantified, and the decrease of KIT expression after SCF stimulation in each cell was calculated. C Ba/F3 cells expressing KIT/W557K558del/V654A or KIT/W557K558del/N822K with or without SPRY4 were washed and starved in RPMI 1640 medium for 4 h, followed by stimulation with 100 ng/ml SCF for 2 min, cells were lysed. Total cell lysates were analyzed by western blot using pAKT, AKT, pERK, ERK, and β-actin antibodies, respectively. KIT was pulled down using KIT antibody from the cell lysates and probed with 4G10, KIT, and SPRY4 antibodies, respectively. The signal intensity of 4G10 was quantified and normalized by KIT, and the signal intensity of pAKT and pERK was quantified and normalized by β-actin
Secondary KIT mutants-mediated cell survival, proliferation, and their sensitivity to imatinib are not altered by SPRY4
Given that the expression and the activation of secondary mutation of KIT are resistant to the inhibition of SPRY4, we investigated whether the cell survival and proliferation mediated by secondary mutations of KIT are also resistant to the inhibition of SPRY4. As expected, the secondary mutations of KIT-mediated cell survival were not affected by the expression of SPRY4 (Fig. 6A). Similarly, the proliferation and the cell cycle progression of cells expressing secondary KIT mutants were not inhibited by SPRY4 (Fig. 6B, C), further indicating that secondary KIT mutants are resistant to the inhibition of SPRY4. This resistance may play a role in the relapse of GISTs when secondary mutations of KIT are acquired by GISTs.
Secondary KIT mutant-mediated cell survival, proliferation, and their sensitivity to imatinib are not altered by SPRY4. A Ba/F3 cells expressing KIT/W557K558del/V654A or KIT/W557K558del/N822K with or without SPRY4 were washed and grown for 48 h in Ba/F3 growth medium without IL-3 but with SCF or no cytokine as control. Apoptotic cells were counted by flow cytometry after staining with PE annexin V apoptosis detection kit. B Cell growth was analyzed by CCK8 kit. C Cell cycle was analyzed by flow cytometry after staining with PI reagent. D Ba/F3 cells expressing KIT/W557K558del/V654A or KIT/W557K558del/N822K with or without SPRY4 were washed and starved in RPMI 1640 medium with imatinib for 4 h, followed by stimulation with 100 ng/ml SCF for 2 min, total cell lysates were probed with pAKT, AKT, pERK, ERK, and β-actin antibodies, respectively. KIT was pulled down using KIT antibody from the cell lysates and probed with 4G10, KIT, and SPRY4 antibodies, respectively. E Ba/F3 cells expressing KIT/W557K558del/V654A or KIT/W557K558del/N822K with or without SPRY4 were washed and grown for 48 h in Ba/F3 growth medium without IL-3 but with SCF and imatinib. Cell proliferation was analyzed by CCK8 kit
Secondary KIT mutants are resistant to the first-line targeted therapy drug imatinib in the treatment of GISTs. To test whether SPRY4 can change the response of secondary KIT mutants to imatinib, we treated cells expressing secondary KIT mutants with imatinib. We found no change in KIT activation in cells expressing secondary KIT mutants in response to imatinib when SPRY4 was expressed, in contrast to the inhibited activation of primary KIT mutants by SPRY4 in response to imatinib treatment. Examination of the activation of downstream signaling molecules ERK and AKT showed similar results (Fig. 6D). Similarly, examination of secondary KIT mutant-mediated cell proliferation showed that SPRY4 didn’t change the growth of cells expressing secondary KIT mutants in response to imatinib treatment (Fig. 6E), which may contribute to the resistance of secondary KIT mutants to imatinib.
Discussion
SPRY4 is highly expressed in GISTs [17], and loss of SPRY4 expression in mice can result in hyperplasia of interstitial cells of cajal (ICC) [27], the cell type from which GISTs are believed to originate [28,29,30]. In this study, we found that SPRY4 can associate with both wild-type KIT and frequently occurred primary KIT mutants in GISTs, and inhibit their expression and activation, which leads to reduced cell survival and proliferation in vitro, and decreased tumorigenesis of GISTs in vivo. Our findings shed light on how SPRY4 regulates KIT signaling in GISTs, extending our understanding of KIT-mediated tumorigenesis of GISTs and its regulation.
Sprouty was identified in Drosophila as an antagonist of FGF signaling [31], and it inhibits RAS signaling [32]. Four homologs SPRY1, SPRY2, SPRY3, and SPRY4 are expressed in mammals [31, 33,34,35], and like sprouty in Drosophila, they also regulate RAS/RAF/MEK/ERK signaling pathway [23, 24]. In addition to its role in normal situation, SPRY4 was identified as a tumor suppressor in lung cancer [36], breast cancer [37, 38], prostate cancer [39], colon cancer [40], ovarian cancer [41], and melanoma [42]. In this study, unlike the direct inhibition of RAS/RAF/MEK/ERK signaling pathway by SPRY4, we found that SPRY4 can physically associate with KIT and inhibit KIT expression and activation in GISTs, leading to reduced activation of downstream signaling pathways including RAS/RAF/EMK/ERK signaling pathway.
70–80% of GISTs carry gain-of-function mutations of KIT that confer the receptor ligand-independent constitutive activation of the receptor and their downstream signaling pathways, such as RAS/RAF/MEK/ERK and PI3 kinases/AKT, leading to the tumorigenesis of GISTs [43,44,45,46]. In addition to the ligand-independent activation, KIT mutants have different signaling properties. For example, SRC family kinases are necessary for the full activation of wild-type KIT, while the activation of D816V mutation of KIT, which is the dominant mutation in mastocytosis, is independent of SRC family kinases [47]. In this study, our results showed that SPRY4 can inhibit both wild-type KIT and primary KIT mutants in GISTs.
Acquisition of the secondary mutations of KIT is one of the main causes of drug resistance and relapse of GISTs treated by imatinib [11,12,13]. Although the second-, third-, and fourth-line targeted therapy drugs (regorafinib, sunitinib, and ripretinib) are available for treating relapsed tumors, they can only increase patient survival for a few months and are far from satisfactory. Overcoming drug resistance mediated by secondary mutations of KIT remains challenging. A better understanding of the activation of secondary KIT mutants and their regulation is necessary to improve the treatment outcomes. Compared with primary KIT mutants, secondary KIT mutants have much stronger ligand-independent activation [19]. Our results showed that the secondary KIT mutants can escape the negative feedback of SPRY4, suggesting the different regulation of secondary KIT mutants, which may contribute to the drug resistance and relapse of GISTs. Further investigation is required to determine why secondary KIT mutants are resistant to the inhibition of SPRY4. In summary, our results show that SPRY4 can inhibit the expression and activation of primary KIT mutants (Fig. 7) but not secondary KIT mutants, and it can sensitize primary KIT mutants to imatinib in the treatment of GISTs.
Data availability
The data used to support the findings of this study are available from the corresponding author upon reasonable request.
References
Tsai M, Valent P, Galli SJ. KIT as a master regulator of the mast cell lineage. J Allergy Clin Immunol. 2022;149:1845–54.
Lennartsson J, Ronnstrand L. Stem cell factor receptor/c-Kit: from basic science to clinical implications. Physiol Rev. 2012;92:1619–49.
Foster BM, Zaidi D, Young TR, Mobley ME, Kerr BA. CD117/c-kit in cancer stem cell-mediated progression and therapeutic resistance. Biomedicines. 2018;35:512.
Soreide K, Sandvik OM, Soreide JA, Giljaca V, Jureckova A, Bulusu VR. Global epidemiology of gastrointestinal stromal tumours (GIST): a systematic review of population-based cohort studies. Cancer Epidemiol. 2016;40:39–46.
Nishida T, Yoshinaga S, Takahashi T, Naito Y. Recent progress and challenges in the diagnosis and treatment of gastrointestinal stromal tumors. Cancers. 2021;13:3158.
Patel SR, Reichardt P. An updated review of the treatment landscape for advanced gastrointestinal stromal tumors. Cancer. 2021;127:2187–95.
Joensuu H, Roberts PJ, Sarlomo-Rikala M, Andersson LC, Tervahartiala P, Tuveson D, et al. Effect of the tyrosine kinase inhibitor STI571 in a patient with a metastatic gastrointestinal stromal tumor. N Engl J Med. 2001;344:1052–6.
Demetri GD, van Oosterom AT, Garrett CR, Blackstein ME, Shah MH, Verweij J, et al. Efficacy and safety of sunitinib in patients with advanced gastrointestinal stromal tumour after failure of imatinib: a randomised controlled trial. Lancet. 2006;368:1329–38.
Demetri GD, Reichardt P, Kang YK, Blay JY, Rutkowski P, Gelderblom H, et al. Efficacy and safety of regorafenib for advanced gastrointestinal stromal tumours after failure of imatinib and sunitinib (GRID): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381:295–302.
Blay JY, Serrano C, Heinrich MC, Zalcberg J, Bauer S, Gelderblom H, et al. Ripretinib in patients with advanced gastrointestinal stromal tumours (INVICTUS): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2020;21:923–34.
Chen LL, Trent JC, Wu EF, Fuller GN, Ramdas L, Zhang W, et al. A missense mutation in KIT kinase domain 1 correlates with imatinib resistance in gastrointestinal stromal tumors. Can Res. 2004;64:5913–9.
Heinrich MC, Corless CL, Blanke CD, Demetri GD, Joensuu H, Roberts PJ, et al. Molecular correlates of imatinib resistance in gastrointestinal stromal tumors. J Clin Oncol. 2006;24:4764–74.
Tamborini E, Bonadiman L, Greco A, Albertini V, Negri T, Gronchi A, et al. A new mutation in the KIT ATP pocket causes acquired resistance to imatinib in a gastrointestinal stromal tumor patient. Gastroenterology. 2004;127:294–9.
Antonescu CR, Besmer P, Guo T, Arkun K, Hom G, Koryotowski B, et al. Acquired resistance to imatinib in gastrointestinal stromal tumor occurs through secondary gene mutation. Clin Cancer Res. 2005;11:4182–90.
Cao J, Wei J, Yang P, Zhang T, Chen Z, He F, et al. Genome-scale CRISPR-Cas9 knockout screening in gastrointestinal stromal tumor with Imatinib resistance. Mol Cancer. 2018;17:121.
Huang WK, Akcakaya P, Gangaev A, Lee L, Zeljic K, Hajeri P, et al. miR-125a-5p regulation increases phosphorylation of FAK that contributes to imatinib resistance in gastrointestinal stromal tumors. Exp Cell Res. 2018;371:287–96.
Nielsen TO, West RB, Linn SC, Alter O, Knowling MA, O’Connell JX, et al. Molecular characterisation of soft tissue tumours: a gene expression study. Lancet. 2002;359:1301–7.
Blume-Jensen P, Siegbahn A, Stabel S, Heldin CH, Ronnstrand L. Increased Kit/SCF receptor induced mitogenicity but abolished cell motility after inhibition of protein kinase C. EMBO J. 1993;12:4199–209.
Zhu G, Shi J, Zhang S, Guo Y, Huang L, Zhao H, et al. Loss of PI3 kinase association improves the sensitivity of secondary mutation of KIT to Imatinib. Cell Biosci. 2020;10:16.
Gromova P, Ralea S, Lefort A, Libert F, Rubin BP, Erneux C, et al. Kit K641E oncogene up-regulates Sprouty homolog 4 and trophoblast glycoprotein in interstitial cells of Cajal in a murine model of gastrointestinal stromal tumours. J Cell Mol Med. 2009;13:1536–48.
Theou-Anton N, Tabone S, Brouty-Boye D, Saffroy R, Ronnstrand L, Lemoine A, et al. Co expression of SCF and KIT in gastrointestinal stromal tumours (GISTs) suggests an autocrine/paracrine mechanism. Br J Cancer. 2006;94:1180–5.
Hirano K, Shishido-Hara Y, Kitazawa A, Kojima K, Sumiishi A, Umino M, et al. Expression of stem cell factor (SCF), a KIT ligand, in gastrointestinal stromal tumors (GISTs): a potential marker for tumor proliferation. Pathol Res Pract. 2008;204:799–807.
Hanafusa H, Torii S, Yasunaga T, Nishida E. Sprouty1 and Sprouty2 provide a control mechanism for the Ras/MAPK signalling pathway. Nat Cell Biol. 2002;4:850–8.
Sasaki A, Taketomi T, Kato R, Saeki K, Nonami A, Sasaki M, et al. Mammalian Sprouty4 suppresses Ras-independent ERK activation by binding to Raf1. Nat Cell Biol. 2003;5:427–32.
Ke H, Kazi JU, Zhao H, Sun J. Germline mutations of KIT in gastrointestinal stromal tumor (GIST) and mastocytosis. Cell Biosci. 2016;6:55.
Mahadevan D, Cooke L, Riley C, Swart R, Simons B, Della Croce K, et al. A novel tyrosine kinase switch is a mechanism of imatinib resistance in gastrointestinal stromal tumors. Oncogene. 2007;26:3909–19.
Thys A, Vandenberghe P, Hague P, Klein OD, Erneux C, Vanderwinden JM. Hyperplasia of interstitial cells of cajal in sprouty homolog 4 deficient mice. PLoS ONE. 2015;10: e0124861.
Kindblom LG, Remotti HE, Aldenborg F, Meis-Kindblom JM. Gastrointestinal pacemaker cell tumor (GIPACT): gastrointestinal stromal tumors show phenotypic characteristics of the interstitial cells of Cajal. Am J Pathol. 1998;152:1259–69.
Sircar K, Hewlett BR, Huizinga JD, Chorneyko K, Berezin I, Riddell RH. Interstitial cells of Cajal as precursors of gastrointestinal stromal tumors. Am J Surg Pathol. 1999;23:377–89.
Robinson TL, Sircar K, Hewlett BR, Chorneyko K, Riddell RH, Huizinga JD. Gastrointestinal stromal tumors may originate from a subset of CD34-positive interstitial cells of Cajal. Am J Pathol. 2000;156:1157–63.
Hacohen N, Kramer S, Sutherland D, Hiromi Y, Krasnow MA. sprouty encodes a novel antagonist of FGF signaling that patterns apical branching of the Drosophila airways. Cell. 1998;92:253–63.
Casci T, Vinos J, Freeman M. Sprouty, an intracellular inhibitor of Ras signaling. Cell. 1999;96:655–65.
Minowada G, Jarvis LA, Chi CL, Neubuser A, Sun X, Hacohen N, et al. Vertebrate Sprouty genes are induced by FGF signaling and can cause chondrodysplasia when overexpressed. Development. 1999;126:4465–75.
de Maximy AA, Nakatake Y, Moncada S, Itoh N, Thiery JP, Bellusci S. Cloning and expression pattern of a mouse homologue of drosophila sprouty in the mouse embryo. Mech Dev. 1999;81:213–6.
Leeksma OC, Van Achterberg TA, Tsumura Y, Toshima J, Eldering E, Kroes WG, et al. Human sprouty 4, a new ras antagonist on 5q31, interacts with the dual specificity kinase TESK1. Eur J Biochem. 2002;269:2546–56.
Tennis MA, Van Scoyk MM, Freeman SV, Vandervest KM, Nemenoff RA, Winn RA. Sprouty-4 inhibits transformed cell growth, migration and invasion, and epithelial-mesenchymal transition, and is regulated by Wnt7A through PPARgamma in non-small cell lung cancer. Mol Cancer Res. 2010;8:833–43.
Vanas V, Muhlbacher E, Kral R, Sutterluty-Fall H. Sprouty4 interferes with cell proliferation and migration of breast cancer-derived cell lines. Tumour Biol. 2014;35:4447–56.
Jing H, Liaw L, Friesel R, Vary C, Hua S, Yang X. Suppression of Spry4 enhances cancer stem cell properties of human MDA-MB-231 breast carcinoma cells. Cancer Cell Int. 2016;16:19.
Wang J, Thompson B, Ren C, Ittmann M, Kwabi-Addo B. Sprouty4, a suppressor of tumor cell motility, is down regulated by DNA methylation in human prostate cancer. Prostate. 2006;66:613–24.
Zhou X, Xie S, Yuan C, Jiang L, Huang X, Li L, et al. Lower expression of SPRY4 predicts a poor prognosis and regulates cell proliferation in colorectal cancer. Cell Physiol Biochem. 2016;40:1433–42.
So WK, Cheng JC, Liu Y, Xu C, Zhao J, Chang VT, et al. Sprouty4 mediates amphiregulin-induced down-regulation of E-cadherin and cell invasion in human ovarian cancer cells. Tumour Biol. 2016;37:9197–207.
Kumar R, Njauw CN, Reddy BY, Ji Z, Rajadurai A, Klebanov N, et al. Growth suppression by dual BRAF(V600E) and NRAS(Q61) oncogene expression is mediated by SPRY4 in melanoma. Oncogene. 2019;38:3504–20.
Hirota S, Isozaki K, Moriyama Y, Hashimoto K, Nishida T, Ishiguro S, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279:577–80.
Antonescu CR, Sommer G, Sarran L, Tschernyavsky SJ, Riedel E, Woodruff JM, et al. Association of KIT exon 9 mutations with nongastric primary site and aggressive behavior: KIT mutation analysis and clinical correlates of 120 gastrointestinal stromal tumors. Clin Cancer Res. 2003;9:3329–37.
Kang HJ, Nam SW, Kim H, Rhee H, Kim NG, Kim H, et al. Correlation of KIT and platelet-derived growth factor receptor alpha mutations with gene activation and expression profiles in gastrointestinal stromal tumors. Oncogene. 2005;24:1066–74.
Emile JF, Brahimi S, Coindre JM, Bringuier PP, Monges G, Samb P, et al. Frequencies of KIT and PDGFRA mutations in the MolecGIST prospective population-based study differ from those of advanced GISTs. Med Oncol. 2012;29:1765–72.
Sun J, Pedersen M, Ronnstrand L. The D816V mutation of c-Kit circumvents a requirement for Src family kinases in c-Kit signal transduction. J Biol Chem. 2009;284:11039–47.
Funding
This study was supported by National Natural Science Foundation of China (82160521), Natural Science Foundation of Ningxia province (2022AAC02025) to JS, Natural Science Foundation of Ningxia province (2022AAC03182) to RB, the Research Grants Council of Hong Kong (14112618 and 14119120) to HZ. Additional support was provided by the Hong Kong Branch of CAS Center for Excellence in Animal Evolution and Genetics to HZ (8601012).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Ethical approval
All animal experiments were approved by the Ethics Committee of Ningxia Medical University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, S., Zhao, S., Liang, N. et al. SPRY4 inhibits and sensitizes the primary KIT mutants in gastrointestinal stromal tumors (GISTs) to imatinib. Gastric Cancer 26, 677–690 (2023). https://doi.org/10.1007/s10120-023-01402-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-023-01402-4