Abstract
Background
Limited information is available on the incidence of postoperative pancreatic fistula (POPF) after D2 gastrectomy with the strict use of the International Study Group of Pancreatic Fistula (ISGPF) criteria, particularly so in Western patients.
Methods
All patients who underwent gastrectomy for adenocarcinoma at the Karolinska University Hospital Huddinge from 2006 until June 2012 were identified via hospital records and reviewed for type of surgical procedure, postoperative morbidity, incidence, and risk factors for POPF.
Results
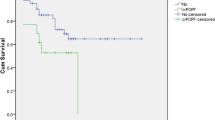
Ninety-two of 107 cases had a D2 gastrectomy eligible for evaluation of POPF, of which 83 (90 %) also underwent bursectomy. Seven patients fulfilled the criteria for POPF grade A (7.6 %), 5 met the criteria for POPF grade B (5.4 %), and 6 the criteria for POPF grade C (6.5 %). The incidence of POPF grade B or C was 4.9 % among the 82 patients for whom no pancreatic resection was performed and 70 % among 10 cases with concomitant pancreatic resection. The latter (OR 156.2, 95 % CI 8.00–3046.93) and age (OR 1.2, 95 % CI 1.02–1.35) were found to be the only risk factors for POPF after gastrectomy upon a multivariate analysis.
Conclusions
In this series of Western patients, POPF grade B or C according to the ISGPF criteria was uncommon after D2 gastrectomy without pancreatic resection. Bursectomy was not a risk factor for POPF.
Similar content being viewed by others
Introduction
The importance of D2 lymphadenectomy for the long-term survival after surgery for gastric cancer is no longer questioned. The pivotal role of en bloc resection of the first and second tier nodes has been extensively studied in Japan, and two randomized trials also showed that D2 gastrectomy can be performed with comparable mortality to D1 gastrectomy when modern principles are followed in high-volume centers [1, 2]. However, two major European randomized trials comparing D1 and D2 dissection found a substantial increase in postoperative morbidity and mortality after D2, which counterbalanced the oncological benefit of D2 at the 5-year follow-up [3–6]. The high incidence of postoperative complications and mortality in the British MRC trial was mainly the result of the frequent pancreatic tail resections in the D2 group, which was expected based on previous observations [7]. After the introduction of pancreas-preserving gastrectomy [8], this morbidity was alleged to be controlled, and pancreatic resection were restricted to cases with direct overgrowth of the tumor into the gland. Postoperative pancreatic fistula (POPF) may, however, also occur as a consequence of inadvertent damage to the pancreas during lymphadenectomy, or during bursectomy, as an integrated procedure-related risk. In this context it has to be realized that a generally accepted and validated definition of pancreatic damage and fistula formation was not applied in the European randomized D1 versus D2 trials. In the past the definition of POPF after gastric cancer surgery has varied also in the Japanese literature. In 2005 the International Study Group of Pancreatic Fistula (ISGPF) divided POPF into three degrees of severity. This definition has gained general acceptance in the literature covering pancreatic surgery [9] and the latest Japanese publications that report on POPF after gastrectomy have accordingly used the ISGPF definition [10–12]. To our knowledge, there is no corresponding information from the Western hemisphere, when this standardized classification has been used to describe the outcome of D2 gastrectomy, with particular emphasis on the impact of bursectomy.
Patients and methods
Inclusion of patients
All patients who underwent resection for gastric adenocarcinoma at the Karolinska University Hospital (Huddinge site) from 2006 to June 2012 were identified via the computerized patient record systems at the Karolinska University Hospital (Orbit and Take Care) using the ICD codes JDDxx, JDCxx for gastric surgery. Baseline patient data regarding age, gender, body mass index (BMI), preoperative workup, TNM stage, American Society of Anesthesiologists (ASA) scores and the plan and outcome for oncological and surgical treatment were reviewed and analyzed. This study was approved by the local ethics committee.
Intraoperative data and definition of lymph node dissection
Operative and patient records were assessed with regard to patient characteristics and demographics (Table 1), operative and perioperative data (Table 2), and pathological data (Table 3). All patients were operated through a laparotomy. D1 dissection in total gastrectomy was here defined as resection of lymph node stations 1–7 and for distal gastrectomy including lymph node stations 1, 3, 4d, 5, 6 and 7. D2 dissection was defined as D1 + at least lymph node stations 8, 9, 11p, and 12a. In 7 cases presenting with a T1 gastric cancer, a pylorus- and vagus-preserving gastrectomy was performed together with a modified D2 dissection at lymph node station 5. D0 was defined as anything less than D1. After total gastrectomy, the patients were reconstructed with a 60- to 70-cm-long retrocolic Roux-en-Y jejunal loop. A majority (22 patients, 79 %) of the distal gastrectomies had a Roux-en-Y reconstruction, and the remaining cases had a Billroth II type omega loop with entero–entero anastomosis. The seven patents with pylorus-preserving gastrectomy were reconstructed with a gastro-gastrostomy. During bursectomy the entire posterior leaf of the peritoneum covering the lesser sac over the transverse mesocolon and the pancreas was excised en bloc. In a majority of the D2 cases (65 patients, 71 %), an abdominal drain was inserted to drain the lesser sac. Otherwise, the specified complications were diagnosed on clinical grounds, by the use of computed tomography (CT) scanning, and through ultrasound-guided percutaneous puncture with additional drain insertion.
Postoperative complications and pancreatic fistula formation
Patients were categorized into those having none or grade A, B, or C fistulas, based on the ISGPF definition [9]. The presence of a biochemical leakage, classified as grade A, was defined as a pancreatic amylase output higher than three times the upper serum level on or after the third postoperative day or later, from a drain placed during surgery. A clinically significant grade B pancreatic fistula was present if any therapeutic intervention was required to normalize a fluid collection or abscess adjacent to the pancreas combined with a pancreatic amylase output higher than three times the upper serum level in drainage fluid. In case of the occurrence of severe clinical repercussions, this was graded as a grade C fistula. Postoperative complications are presented in Table 4 and severity according to modified Clavien–Dindo scoring system in Table 5 [13].
Statistics
Data are presented as median (interquartile range). Fisher’s exact test and Mann–Whitney U test were used for categorical and continuous variables respectively. Risk factors were tested in univariate analysis, and the risk factors with a p value <0.1 were tested in a multivariate model with logistic regression analysis. Stata software was used for the calculations.
Results
Intraoperative data
During the 6.5-year inclusion period, 107 resections for gastric adenocarcinoma were completed. D0 dissection was performed in 5 patients (4.7 %) and D1 in 9 patients (8.4 %). The remaining 93 patients (87 %) underwent D2 dissection. One patient underwent a concomitant total pancreatectomy and was excluded from the analysis because of inability to develop POPF, resulting in 92 patients eligible for assessment of POPF after D2 gastrectomy. Eighty-three cases also had a bursectomy (90 %). The median number of lymph nodes examined for D2 patients in the pathology report was 21. In 4 patients it was not stated how many lymph nodes were retrieved, and for some patients the pathology report stated the number of lymph nodes examined but not the number of nodes present in the specimen. The clinical and demographic characteristics of the patients are presented in Table 1. In total, 21 patients underwent splenectomy, of which 6 also had a concomitant pancreatic resection. Ten patients had suspicion of tumor extension into the pancreas or proximal duodenum and underwent a simultaneous pancreatic resection. Four patients underwent a Whipple procedure, 4 underwent distal pancreatic resection with splenectomy, and 2 patients a local excision of lymph node conglomerates extending into the pancreas. Four of the 10 cases with pancreatic resection were classified as R0 resections according to the pathology report, 4 as R1 and 2 as R2. Of the latter, both were treated as emergencies because of bleeding. The details of the type and number of combined resections are presented in Table 2.
Postoperative pancreatic fistula
Seventy-four patients with D2 gastrectomies completed were classified as having no pancreatic fistula (80 %). This group included patients with intraabdominal abscesses needing insertion of percutaneous drains, for which the analysis of drainage fluid showed no signs of increased levels of pancreatic amylase, as well as 1 patient who had an abscess without any connection to the pancreas, for whom analysis of pancreatic amylase in drainage fluid was unavailable. Moreover, among 65 patients with intraabdominal drains inserted prophylactically allowing for continuous measurement of pancreatic amylase in the drainage fluid, 7 presented with levels three times higher than the plasma counterpart on the third day or later. None of these patients required any additional intervention and were accordingly classified as having POPF grade A (7.6 % of all 92 cases). Two patients had signs of peri-pancreatic fluid collections, and 3 patients had persistent elevated levels of pancreatic amylase in drains placed during surgery, which required specifically directed interventions, thus fulfilling the criteria for POPF grade B (5.4 %). Six patients presented with a more complex postoperative course together with elevated pancreatic amylase outputs from the drains, mandating more aggressive therapies, and were thus classified as POPF grade C (6.5 %).
Other surgical complications
Infectious complications from the abdominal cavity as well as from the lungs dominated the morbidity profile (Table 4). Seven patients had anastomotic leakage (7.6 %), 3 from the esophagojejunal anastomosis (5.3 % of the total gastrectomy cases) and 4 from the gastro–entero or entero–entero anastomoses (4.3 %). Four patients suffered from leakage from the closed duodenal bulb (4.3 %). The overall reoperation rate including endoscopic procedures in general anesthesia was 19.6 % (18 patients). The indications for these procedures were bleeding (8), anastomotic or duodenal bulb leakage (7), small bowel obstruction (2), and splenic infarction (1). The postoperative complication panorama according to the Clavien–Dindo grading is presented in Table 5, showing that 36 patients (39 %) were classified as grade 3 or worse. Among the patients with anastomotic or duodenal bulb leakage, 5 patients had elevated levels of pancreatic amylase in drainage fluid with a concomitant increase of bilirubin. Two of these patients had normal values of pancreatic amylase in the drainage on the third and fourth postoperative day before diagnosis of the leakage.
In total, 22 patients had an intraabdominal abscess. Ten of these could be attributed to POPF grade B or C and 6 to anastomotic or duodenal bulb leakages. Of the remaining 6 patients, 1 for whom measurements of pancreatic amylase in drainage fluid were available was classified as having POPF grade A. Four patients had normal pancreatic amylase values between the second and sixth postoperative day, before the diagnosis of the abscess, and 1 patient had an abscess located in conjunction to the Douglas pouch. These 5 patients were classified as having no POPF.
Risk factors for postoperative pancreatic fistula (POPF)
Univariate analysis identified pancreatic resection and splenectomy as risk factors for the development of POPF grade B/C (Table 6). Seven of the 11 patients who developed POPF grade B/C underwent pancreatic resection. Two patients who had a splenectomy without pancreatic resection also developed POPF grade B/C, and 1 patient for whom no additional organ resection was performed had undergone reoperation because of bleeding before the development of POPF grade B. In the multivariate analysis, incorporating the three factors with a p value <0.1 according to the univariate analysis (age, splenectomy, and pancreatic resection), pancreatic resection and age emerged as significant risk factors (Table 7).
Discussion
Our consecutive experience from 92 D2 gastrectomies demonstrates that POPF is a rare complication, but in 11 patients (12 %) POPF grade B or C developed. Previous data on the incidence of POPF after gastrectomy with D2 lymphadenectomy vary from a few percent up to nearly 50 %, and most of these reports originate from the Far East [14–19]. This substantial variation may be explained by case mix, but more importantly because of different definitions of POPF. In a review from 1991 to 2000, 26 different definitions of what constitutes a POPF could be identified [20]. The ISGPF definition of POPF was presented and shortly thereafter modified in 2005 and divided, based on clinical severity, this complication into three grades [9]. The true risk of POPF after gastrectomy must therefore be reevaluated according to the updated ISGPF definition of POPF. In 65 patients (71 %) we inserted a prophylactic drain and measured pancreatic amylase in the drainage fluid to carefully ascertain how often a grade A POPF develops after D2 gastrectomy incorporating bursectomy in most cases. From a strict methodological perspective the estimation of the true figures on the incidence of POPF grade A mandates prophylactic placements of drains in all patients; otherwise, infallibly an underestimation of the incidence will follow. However, neither after gastrectomy nor after pancreatic resection has evidence been presented to justify the routine use of such drains [21, 22].
As shown in several other studies, we found that the dominating risk factor for POPF grade B and C was concomitant pancreatic resection, but determined no impact of BMI or splenectomy as in previous studies [10, 11]. There was a minor effect of patient age on the risk of POPF. In this context it has to be recalled that all our patients who submitted to pancreatic resection had a soft texture of the pancreatic gland with a thin main duct diameter and large volume of the remaining gland [23, 24]. All these factors are known to contribute to the risk of leakage from the pancreatic remnant. Accordingly, during recent years we have carefully taken into account these factors, particularly in the choice of operative strategy when resection of the pancreas is mandated. The ISGPF definition has also been applied in a few recent studies on gastrectomy, all from Japan, with reported figures ranging from a 4.3 % incidence of grade B/C fistulas after laparoscopic distal gastrectomy in patients with early gastric cancer [10] to a 22 % incidence after total gastrectomy with D2 dissection without pancreatic resection [11]. Given the similarities in lymph node dissection between these studies, it is possible that other factors such as tumor size or the extent of gastric resection may be determinant factors for the development of POPF, rather than the extent of lymph node dissection. There are no data in the literature supporting the hypothesis that dissection close to the pancreas, which is necessary during D2 lymphadenectomy, increases the incidence of POPF [1, 25]. Our data show that provided that the pancreatic gland remains intact, D2 gastrectomy can be performed with a low incidence of POPF and mortality also in Western patients. In fact, of our 11 cases with POPF grade B/C, 7 had undergone a pancreatic resection, 2 had a splenectomy, and 1 patient with POPF grade B had an acute reoperation because of postoperative bleeding. It should, however, be mentioned that the incidence of POPF grade B or C may have been slightly underestimated in the cases with anastomotic dehiscence. In three cases with anastomotic or duodenal bulb leakages, we lacked documentation of pancreatic amylase in the drainage fluid before the diagnosis. At that time we observed a concomitant increase of bilirubin in the drainage fluid, which precluded any straightforward determination of a simultaneous POPF.
Bursectomy is another surgical factor that has the potential to expose the pancreas to a risk of damage and thereby induce POPF. This procedure includes dissection adjacent to the anterior aspect of the pancreas to separate the posterior peritoneal sheet covering the lesser sac. We observed a low frequency of POPF in patients submitted to bursectomy but without pancreatic resection, suggesting that also this part of the D2 dissection can be done safely in Western patients. A recent Japanese randomized trial comparing gastrectomy with or without bursectomy found no increased incidence of POPF (again not using the ISGPF criteria) in the bursectomy group [26]. One would expect that total gastrectomy, which may include splenectomy in contrast to distal gastrectomy, should have been associated with an increased risk of POPF grade B or C in the univariate analysis, in accordance with previous studies [27]. We believe that the reason why no such relationship was found herein was that the pancreatic resections were relatively evenly distributed between total and distal gastrecomies (six and four, respectively).
The clinical significance of grade A fistulas remains unsolved, even in the literature covering pancreatic surgery. Recent data may, however, suggest it to be an early marker for subsequent more clinically important complications [28]. Obviously more controlled observations are needed to clarify the predictive role of assessing early postoperative drain amylase output. The majority of our cases followed a benign postoperative course. However, 36 patients (39 %) had postoperative complications classified as Clavien–Dindo grade 3 or worse; this may partially be explained by the large number of multiorgan resections. In this group, 18 patients (50 %) had additional organ resection other than gastrectomy, and 6 of those 18 had at least two additional organs resected. The anastomotic leak rate from the esophagojejunostomy needs to be less than 5 %. There are some reasons behind our figures converging toward that level. One is the comparatively high rate of multivisceral resections and another may be a high median BMI (25.2); this has been defined as a risk factor for anastomotic leakage in gastric surgery [29, 30]. Based on current clinical evidence it is difficult to define a causal relationship between POPF and anastomotic complications when the procedures do not involve the pancreatic gland per se.
In conclusion, D2 gastrectomy without any resection of the pancreatic gland has a low incidence of POPF grade B or C. D2 lymphadenectomy and bursectomy per se expose the pancreas to a minimal and an acceptable risk of damage. Pancreatic resection in association with gastrectomy adds a substantial risk of clinically significant POPF and morbidity, and should if possible be avoided.
References
Degiuli M, Sasako M, Ponti A. Morbidity and mortality in the Italian Gastric Cancer Study Group randomized clinical trial of D1 versus D2 resection for gastric cancer. Br J Surg. 2010;97:643–9.
Wu CW, Hsiung CA, Lo SS, Hsieh MC, Chen JH, Li AF, et al. Nodal dissection for patients with gastric cancer: a randomised controlled trial. Lancet Oncol. 2006;7:309–15.
Cuschieri A, Fayers P, Fielding J, Craven J, Bancewicz J, Joypaul V, et al. Postoperative morbidity and mortality after D1 and D2 resections for gastric cancer: preliminary results of the MRC randomised controlled surgical trial. The Surgical Cooperative Group. Lancet. 1996;347:995–9.
Bonenkamp JJ, Songun I, Hermans J, Sasako M, Welvaart K, Plukker JT, et al. Randomised comparison of morbidity after D1 and D2 dissection for gastric cancer in 996 Dutch patients. Lancet. 1995;345:745–8.
Bonenkamp JJ, Hermans J, Sasako M, van de Velde CJ, Welvaart K, Songun I, et al. Extended lymph-node dissection for gastric cancer. N Engl J Med. 1999;340:908–14.
Cuschieri A, Weeden S, Fielding J, Bancewicz J, Craven J, Joypaul V, et al. Patient survival after D1 and D2 resections for gastric cancer: long-term results of the MRC randomized surgical trial. Surgical Co-operative Group. Br J Cancer. 1999;79:1522–30.
Lundell L, Grip I, Olbe L. Pancreatic resection additional to gastrectomy for gastric cancer. Effect on postoperative morbidity. Acta Chir Scand. 1986;152:145–9.
Maruyama K, Sasako M, Kinoshita T, Sano T, Katai H, Okajima K. Pancreas-preserving total gastrectomy for proximal gastric cancer. World J Surg. 1995;19:532–6.
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery (St. Louis). 2005;138:8–13.
Jiang X, Hiki N, Nunobe S, Kumagai K, Nohara K, Sano T, et al. Postoperative pancreatic fistula and the risk factors of laparoscopy-assisted distal gastrectomy for early gastric cancer. Ann Surg Oncol. 2012;19:115–21.
Miki Y, Tokunaga M, Bando E, Tanizawa Y, Kawamura T, Terashima M. Evaluation of postoperative pancreatic fistula after total gastrectomy with D2 lymphadenectomy by ISGPF classification. J Gastrointest Surg. 2011;15:1969–76.
Obama K, Okabe H, Hosogi H, Tanaka E, Itami A, Sakai Y. Feasibility of laparoscopic gastrectomy with radical lymph node dissection for gastric cancer: from a viewpoint of pancreas-related complications. Surgery (St. Louis). 2011;149:15–21.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Chikara K, Hiroshi S, Masato N, Hirotoshi A, Goro M, Hidetaka O. Indications for pancreaticosplenectomy in advanced gastric cancer. Hepatogastroenterology. 2001;48:908–12.
Ichikawa D, Kurioka H, Yamaguchi T, Koike H, Okamoto K, Otsuji E, et al. Postoperative complications following gastrectomy for gastric cancer during the last decade. Hepatogastroenterology. 2004;51:613–7.
Kunisaki C, Shimada H, Ono H, Otsuka Y, Matsuda G, Nomura M, et al. Predictive factors for pancreatic fistula after pancreaticosplenectomy for advanced gastric cancer in the upper third of the stomach. J Gastrointest Surg. 2006;10:132–7.
Sano T, Sasako M, Katai H, Maruyama K. Amylase concentration of drainage fluid after total gastrectomy. Br J Surg. 1997;84:1310–2.
Sano T, Sasako M, Yamamoto S, Nashimoto A, Kurita A, Hiratsuka M, et al. Gastric cancer surgery: morbidity and mortality results from a prospective randomized controlled trial comparing D2 and extended para-aortic lymphadenectomy. Japan Clinical Oncology Group study 9501. J Clin Oncol. 2004;22:2767–73.
Sasako M, Katai H, Sano T, Maruyama K. Management of complications after gastrectomy with extended lymphadenectomy. Surg Oncol. 2000;9:31–4.
Bassi C, Butturini G, Molinari E, Mascetta G, Salvia R, Falconi M, et al. Pancreatic fistula rate after pancreatic resection. The importance of definitions. Dig Surg. 2004;21:54–9.
Conlon KC, Labow D, Leung D, Smith A, Jarnagin W, Coit DG, et al. Prospective randomized clinical trial of the value of intraperitoneal drainage after pancreatic resection. Ann Surg. 2001;234:487–93 (discussion 493–494).
Liu HP, Zhang YC, Zhang YL, Yin LN, Wang J. Drain versus no-drain after gastrectomy for patients with advanced gastric cancer: systematic review and meta-analysis. Dig Surg. 2011;28:178–89.
Frozanpor F, Albiin N, Linder S, Segersvard R, Lundell L, Arnelo U. Impact of pancreatic gland volume on fistula formation after pancreatic tail resection. JOP. 2010;11:439–43.
Ansorge C, Strommer L, Andren-Sandberg A, Lundell L, Herrington MK, Segersvard R. Structured intraoperative assessment of pancreatic gland characteristics in predicting complications after pancreaticoduodenectomy. Br J Surg. 2012;99:1076–82.
Wu CW, Hsiung CA, Lo SS, Hsieh MC, Shia LT, Whang-Peng J. Randomized clinical trial of morbidity after D1 and D3 surgery for gastric cancer. Br J Surg. 2004;91:283–7.
Imamura H, Kurokawa Y, Kawada J, Tsujinaka T, Takiguchi S, Fujiwara Y, et al. Influence of bursectomy on operative morbidity and mortality after radical gastrectomy for gastric cancer: results of a randomized controlled trial. World J Surg. 2011;35:625–30.
Otsuji E, Yamaguchi T, Sawai K, Okamoto K, Takahashi T. Total gastrectomy with simultaneous pancreaticosplenectomy or splenectomy in patients with advanced gastric carcinoma. Br J Cancer. 1999;79:1789–93.
Sutcliffe RP, Battula N, Haque A, Ali A, Srinivasan P, Atkinson SW, et al. Utility of drain fluid amylase measurement on the first postoperative day after pancreaticoduodenectomy. World J Surg. 2012;36:879–83.
Bickenbach KA, Denton B, Gonen M, Brennan MF, Coit DG, Strong VE. Impact of obesity on perioperative complications and long-term survival of patients with gastric cancer. Ann Surg Oncol. 2013;20:780–7.
Ojima T, Iwahashi M, Nakamori M, Nakamura M, Naka T, Ishida K, et al. Influence of overweight on patients with gastric cancer after undergoing curative gastrectomy: an analysis of 689 consecutive cases managed by a single center. Arch Surg. 2009;144:351–8 (discussion 358).
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kung, CH., Lindblad, M., Nilsson, M. et al. Postoperative pancreatic fistula formation according to ISGPF criteria after D2 gastrectomy in Western patients. Gastric Cancer 17, 571–577 (2014). https://doi.org/10.1007/s10120-013-0307-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-013-0307-1