Abstract
Sixty-five patients with main diagnosis of sepsis, who were directly admitted to the emergency department (ED) and had fatal outcomes after transfer to the medical intensive care units (MICU), were included. Patients who died within 48 hours of MICU transfer were defined as having rapidly fatal outcomes (RFO). The following clinical variables, including diagnosis of infection source; results of blood, sputum, and urine cultures; management for sepsis in the ED and MICU and survival time, were analyzed. There were 30 (46%) patients with RFO. The median survival time in the RFO group was 22.6 hours in MICU. Klebsiella pneumoniae was the most common pathogen isolated from blood (7/65, 10.7%) and relevant sputum samples (7/45, 15.5% ). Multivariate analysis revealed that age, gender and positive sputum culture for K. pneumoniae (hazard ratio, 11.898, p < 0.001) were independently associated with RFO in septic patients. The median survival times for patients with positive and negative K. pneumoniae sputum culture were 17 hours and 66.8 hours (p < 0.001, by the log rank test), respectively. This study found that positive sputum culture of K. pneumoniae was an important independent predictive factor of RFO in septic patients admitted to the MICU.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis is one of the main causes of death among hospitalized patients and has high mortality rates ranging from 20 to 40% in the United States [1]. Although current evidence suggests hospital mortality of sepsis can be reduced by the use of sepsis care bundles [2], few studies have investigated the risk factors for rapidly fatal outcome in septic patients. Alcoholic patients with bacteremic pneumonia due to Klebsiella pneumoniae were found to have high mortality, short onset of illness, and short survival before and after hospital admission [3]. Although increasing studies have shown the potential of biomarkers such as protein C and macrophage migration inhibitory factor (MIF) to predict early death in severe sepsis [4–6], a better understanding of the predicting host factors, pathogens and management in septic patients is crucial to prevent their rapidly fatal outcomes.
This study investigated the potential risk factors for rapidly fatal outcomes in septic patients including underlying conditions, pathogens, and management in the emergency department (ED) and medical intensive care unit (MICU).
Materials and methods
Setting and patients
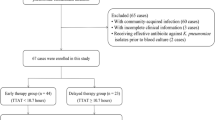
The medical records of all patients with sepsis (including severe sepsis and septic shock) who were transferred to the MICU (23 beds in a 600-bed regional teaching hospital) after ED admission between July 2005 and June 2006 were reviewed. Only patients with a main diagnosis of sepsis, direct transfer from the ED and fatal outcomes in the MICU were included in this study. Patients who were transferred from other intensive care units or from a general ward were excluded. At least two sets of blood culture were obtained from all patients either in the ED or MICU. The gender, age, drinking habits, and underlying diseases of the patients were recorded. The following clinical variables during the patient’s stay in the ED and MICU were also recorded: clinical diagnosis (including systemic inflammatory response syndrome (SIRS), sepsis, pneumonia, urinary tract infection (UTI), intra-abdominal infection (IAI), organ dysfunction, etc.); management (including obtaining cultures, antibiotic regimen, insertion of central venous catheter, amount of fluid resuscitation, mechanical ventilator requirement, PaO2/FiO2 ratio, vasopressor use, steroid use, and component therapy), hemogram, blood gas, blood chemistry, coagulation profile, results of blood, sputum, urine and other cultures; chest radiographic features and survival time. All chest radiographs were read and consensus on findings was reached by two of the authors.
Definitions
Rapidly fatal outcome (RFO) was defined as a septic patient who died within 48 hours after MICU admission. The late fatal outcome (LFO) group was defined as a septic patient who died more than 48 hours after MICU admission. A clinical diagnosis of pneumonia, UTI and IAI was made at the time of ED admission if the patients presented with associated symptoms, laboratory data or radiographic evidence [7]. Cultures of sputum, urine and other specimens were obtained according to the judgment of clinicians at the ED or MICU. All patients had at least two sets of blood cultures; sputum cultures were obtained in 45 patients and urine cultures were collected in 44 patients. The results of sputum culture were considered of clinical significance if they had good quality Gram stain showing numerous polymorphonuclear cells (>25 in a × 100 microscopic field) and few squamous cells (<10 in a × 100 microscopic field) [8]. Blood culture specimens were inoculated into BACTEC culture bottles using the BACTEC 9240 system (Becton Dickinson, Cockeysville, MD, USA). Sputum culture specimens were processed on blood agar, chocolate agar, and eosin methylene blue agar media. Antimicrobial susceptibility was determined by the disk diffusion method, as described by the Clinical and Laboratory Standards Institute (CLSI) [9]. Extended-spectrum β-lactamase (ESBL) production of Escherichia coli and K. pneumoniae was determined by the disk diffusion method using both cefotaxime and ceftazidime alone and in combination with clavulanic acid as recommended by the CLSI [9].
The diagnosis of SIRS, sepsis and organ dysfunction was made according to 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference and Surviving Sepsis Campaign 2008 criteria [10, 11]. Empiric antibiotic treatment was considered appropriate if it included intravenous antimicrobials to which the specific isolate (or isolates, if polymicrobial) showed in vitro susceptibility [12].
Statistical analysis
The data were complied and analyzed with the statistical package SPSS 13.0 (SPSS Inc., Chicago, IL). All continuous data were expressed as mean ± standard deviation (SD) and compared using a two-tailed Student’s t-test. Categorical variables were reported as a percentage and compared using chi-square or Fisher’s exact test when appropriate. Multivariate Cox regression analysis after adjustment for age and gender was used to identify independently significant factors in predicting rapidly fatal outcome. Survival curves were plotted using the Kaplan-Meier method and examined by log-rank test. A value of p < 0.05 was considered statistically significant.
Results
A total of 849 patients were admitted to the MICU during the study period. Among these patients, 168 were directly admitted to the ED and were transferred to the MICU for further management under the main diagnosis of sepsis and 65 of them died in the MICU during the study period. The overall mortality in the MICU was 21.9% and the in-ICU mortality was 38.6% in the study group. Forty seven of these patients were male and the mean age of all patients was 71 years, with a range of 28–95 years. Thirty patients (46%) had RFO. There was no significant difference between the RFO and LFO groups in age, gender, drinking habit, underlying diseases, diagnosis, organ dysfunction (not shown), laboratory data (not shown), treatment and the time spent in the ED (Table 1). However, the RFO group had a significantly lower incidence of IAI (3.33% vs. 25.7%, p = 0.013) and a significantly higher incidence of renal dysfunction (75.0% vs. 44.1%, p = 0.041) diagnosed in the MICU (Table 2). Only half of these patients received empirical antimicrobial therapy in the ED (Table 1). After admission to the MICU, all of them received empirical antibiotic treatment. The most commonly used antibiotics in the ED and the MICU were cefuroxime and ceftriaxone. There was no significant difference in the use of empirical antibiotics and appropriate antibiotic therapy in the ED and MICU between patients with RFO and LFO (data not shown). Other diagnoses, laboratory data (not shown), and management in the MICU were not significantly different between the two groups.
The positive rates of blood, sputum, and urine cultures were 53.8% (35/65), 40.0% (18/45), and 50.0% (22/44), respectively. Other positive culture results included wound (7/8) and body fluid (2/12). K. pneumoniae was the most common pathogen isolated from blood (10.7%, 7/65) and sputum (15.5%, 7/45) cultures. The RFO group had a significantly higher incidence of positive K. pneumoniae culture from both blood (23.3% vs. 0.00%, p = 0.002) and sputum (27.3% vs. 4.34%, p = 0.034) (Table 3). Four patients had multiple pathogens in blood cultures including K. pneumoniae and group D Streptococcus, methicillin-resistant Staphylococcus aureus (MRSA) and Streptococcus agalactiae, methicillin resistant S. epididermis (MRSE) and Micrococcus spp., and coagulase-negative staphylococci (CoNS) and Bacteroides thetaiotaomicron, respectively. All K. pneumoniae isolates recovered from sputum specimens were pure cultures but one patient had multiple isolates from sputum culture including MSSA, S. pyogenes, and Mycobacterium tuberculosis. Two patients had multiple isolates from urine culture including K. oxytoca and ESBL-producing E. coli, and K. pneumoniae and E. coli, respectively.
The results of Cox regression analyses of factors associated with rapidly fatal outcome are summarized in Table 4. The univariate analysis identified four variables associated with rapidly fatal outcome in septic patients: intraabdominal infection (IAI) diagnosed in the MICU; positive blood culture for K. pneumoniae; renal dysfunction diagnosed in the MICU; and positive sputum culture for K. pneumoniae. In the multivariate analysis after adjustment for age and gender, three factors including age, gender and positive sputum culture for K. pneumoniae were independently associated with rapidly fatal outcome in septic patients. The hazard ratio estimate for patients with positive sputum culture for K. pneumoniae was 11.898 (95% confidence interval, 3.115–45.444; p < 0.001).
All patients died during their stay in the MICU. The overall median survival time in MICU was 57 hours. Survival curves for all patients based on positive sputum culture of K. pneumoniae are presented in Fig. 1. The median survival time of patients with positive sputum culture for K. pneumoniae and the remaining patients were 17 hours and 66.8 hours, respectively (p < 0.001, by the log-rank test).
A total of 11 patients had positive sputum and/or blood cultures for K. pneumoniae. Ten of them died within 48 hours after admission to the MICU. Three of them had K. pneumoniae isolates from both sputum and blood. The mean age of the 11 patients was 61 years and ranged from 32 to 95 years. Their underlying conditions included alcohol intake (6/11), diabetes mellitus (3/11), liver cirrhosis (1/11), and malignancy (1/11). The initial radiographic finding of these 11 patients revealed no active lung lesion in two patients with K. pneumoniae isolated from blood culture. The initial radiographic findings of the remaining nine patients included unilateral lobar consolidation in six patients, bilateral lobar consolidation in two patients, and unilateral pleural effusion in three patients.
All isolates of K. pneumoniae from sputum and/or blood were susceptible to cefazolin, cefuroxime, ampicillin/sulbactam, ceftriaxone, and levofloxacin but resistant to ampicillin by the routine disk diffusion method. Five of the 11 patients received appropriate empirical antibiotics in the ED (two with piperacillin-tazobactam, one with ampicillin/sulbactam, one with levofloxacin and one with cefazolin), and all 11 patients received appropriate antibiotics in the MICU (two with cefuroxime, four with ceftriaxone, one with cefazolin, one with imipenem, two with levofloxacin and one with combination therapy of ceftriaxone and levofloxacin).
Discussion
Analysis of the clinical data of 65 patients with a main diagnosis of sepsis who were transferred from the ED to the MICU revealed that positive culture of K. pneumoniae in relevant sputum samples was an independent predictor of rapidly fatal outcome. K. pneumoniae was the most common cause of severe pneumonia in patients without response to initial empiric antibiotics who required mechanical ventilation [13]. Significantly elevated interleukin 10 (IL-10) level in the bronchoalveolar lavage (BAL) fluids and serum of patients with positive BAL culture for K. pneumoniae was found compared to other pathogens [13]. A previous study also showed that bacteremic K. pneumoniae pneumonia (BKPP) caused RFO in alcoholics despite management with adequate antibiotics and intensive care [3].
In Taiwan, community-acquired BKPP was due to mucoid phenotype (100%), aerobactin production (83%), and capsular K1 or K2 serotype (75%) in younger patients without serious underlying diseases [14]. All of these findings indicate the high virulence of K. pneumoniae, which induced a marked immune response compared to other pathogens and could lead to rapidly fatal outcome even in younger and previously healthy people.
Recent studies suggested that high serum MIF levels and inappropriate adrenal response were associated with early death in patients with severe sepsis [5, 6]. Intra-peritoneal injection of recombinant MIF in a rat model of sepsis induced disseminated intravascular coagulation (DIC) in plasma [15]. Continuously high levels of soluble fibrin and low protein C levels were also found in septic patients with DIC [16]. In a mouse model of systemic K. pneumonia infection the elevation of plasma IL-10 was observed within 24 hours and peaked within 12 hours after infection. Rukavina et al. speculated that the dynamic of greater IL-10 production in infected animals during the early phase was responsible for inadequate inflammatory reaction and control of the infection [17]. All of these findings suggest a combination of high serum IL-10 and high MIF level could lead to RFO in septic patients with suppression of inflammatory response and development of DIC.
Surprisingly, there was no significant difference in the diagnosis and management at the ED between the RFO and LFO groups. There are two possible reasons which may explain this finding. First, the treatment for sepsis was not adequate to overcome rapidly fatal outcome and more effective therapy such as activated protein C and optimization of glycemic control was not available to these patients. Second, these similar results might indicate poor compliance with initial resuscitation and infection control measures in both ED groups of patients including low rates of obtaining blood cultures, prescribing empirical antibiotics, insertion of central venous catheter, and conservative fluid resuscitation [11]. Inadequate use of these measures seems to be a global issue in implementation of surviving sepsis campaign guidelines. De Miguel-Yanes et al. reported 15% of septic patients had no blood cultures drawn, and only two thirds of septic patients had received their first dose of antibiotics within 6 hours after admission [16]. In addition, 46.6% of their cases of severe sepsis or shock received aggressive fluid therapy and no patient had central venous pressure monitoring at the ED [16]. Ferrer et al. reported that the compliance with performing blood cultures and early administration of broad-spectrum antibiotics was only 54.4% and 66.5%, respectively, before an educational program to improve the process of care for severe sepsis [2]. Although earlier implementation of sepsis care bundles could reduce mortality and MICU stay, no study has demonstrated such management could prevent rapidly fatal outcome [17, 18]. Further study is needed to determine whether implementation of the current 6-hour and 24-hour sepsis care bundles is reasonable to prevent rapidly fatal outcomes on the basis of cytokine intervention and administration of APC.
The empirical antibiotic treatments given in the ED and MICU seemed to be ineffective in our patients with positive sputum and blood culture of K. pneumoniae even though sensitivity testing showed the isolates were all sensitive to these empirical antibiotics. There are several possible causes which may explain this finding. First, only five patients (45.5%) received effective empirical antibiotics in the ED and there was a delay in receiving empirical antibiotics in the ED in another 6 patients (54.5%). Second, a retrospective study by Thom et al. found that appropriate empiric antimicrobial therapy for K. pneumoniae bacteremia was not associated with lower in-hospital mortality [12]. This suggests that the choice of empiric antimicrobial agents might not improve outcomes and that baseline severity of illness was a potential confounding factor of the association between mortality and antimicrobial therapy [12]. Third, Fang et al. reported that first line empirical antibiotics had at least 98% disk susceptibility in a retrospective cohort study involving 177 cases of K. pneumoniae pyogenic liver abscess [19]. The mortality rate (2.8%) in their study was low because most patients (94%) received a third-generation cephalosporin. Septic ocular or central nervous system complications developed in 23 of their patients (13.0%) and K. pneumoniae genotype K1 was the only significant risk factor for this type of septic complication, even with appropriate antimicrobial therapy. This finding suggests K. pneumoniae genotype K1 could be susceptible to empirical antibiotics but still have high virulence and result in serious complications or even mortality in patients with conditions other than pyogenic liver abscess. Further studies are needed to delineate the serial change of virulence of K. pneumoniae genotype K1 before and after the prescription of empirical antibiotics.
Several limitations of this study should be mentioned. First, the results should not be applied to regions other than Southeast Asia and South Africa because of geographic differences in the spectrum of disease caused by K. pneumoniae [14]. Second, the role of the most recent biomarkers which have been found to predict early mortality from sepsis, such as MIF and protein C, could not be determined in this analysis because of the retrospective study design. Third, the serotype and genotype of K. pneumoniae isolates from our patients could not be further evaluated because they were no longer available at the time of the study. Further prospective study is needed to explore the relationships among virulence of K. pneumoniae, cytokine intervention, current sepsis care bundles and the early diagnosis and treatment of septic patients with rapidly fatal outcome.
In conclusion, this retrospective study identified positive sputum culture of K. pneumoniae as the most powerful predictor of rapidly fatal outcome in septic patients. Whether activated protein C is the medication of choice to avoid rapidly fatal outcome in sepsis care bundles will require further investigation.
References
Martin GS, Mannino DM, Eaton S, Moss M (2003) The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 348:1546–1554
Ferrer R, Artigas A, Levy MM, Blanco J, González-Díaz G, Garnacho-Montero J et al (2008) Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain. JAMA 299:2294–2303
Jong GM, Hsiue TR, Chen CR, Chang HY, Chen CW (1995) Rapidly fatal outcome of bacteremic Klebsiella pneumoniae pneumonia in alcoholics. Chest 107:214–217
Macias WL, Nelson DR (2004) Severe protein C deficiency predicts early death in severe sepsis. Crit Care Med 32(5 Suppl):S223–S228
Chuang CC, Wang ST, Chen WC, Chen CC, Hor LI, Chuang YC (2007) Increases in serum macrophage migration inhibitory factor in patients with severe sepsis predict early mortality. Shock 27:503–506
Emonts M, Sweep FC, Grebenchtchikov N, Geurts-Moespot A, Knaup M, Chanson AL et al (2007) Association between high levels of blood macrophage migration inhibitory factor, inappropriate adrenal response, and early death in patients with severe sepsis. Clin Infect Dis 44:1321–1328
Sun HY, Chen SY, Chang SC, Pan SC, Su CP, Chen YC (2006) Community-onset Escherichia coli and Klebsiella pneumoniae bacteremia: influence of health care exposure on antimicrobial susceptibility. Diagn Microbiol Infect Dis 55:135–141
Miyashita N, Shimizu H, Ouchi K, Kawasaki K, Kawai Y, Obase Y et al (2008) Assessment of the usefulness of sputum Gram stain and culture for diagnosis of community-acquired pneumonia requiring hospitalization. Med Sci Monit 14: CR171–CR176
Clinical and Laboratory Standards Institute (CLSI) (2006) Performance standards for antimicrobial disk susceptibility tests: 9th ed. Approved standard M2-A9. CLSI, Wayne, PA
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D et al (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med 31:1250–1256
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R et al (2008) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 36:296–327
Thom KA, Schweizer ML, Osih RB, McGregor JC, Furuno JP, Perencevich EN et al (2008) Impact of empiric antimicrobial therapy on outcomes in patients with Escherichia coli and Klebsiella pneumoniae bacteremia: a cohort study. BMC Infect Dis 8:116
Wu CL, Chan MC, Chang GC, Lee YL, Chin CS, Chang KM et al (2006) Etiology and cytokine expression in patients requiring mechanical ventilation due to severe community-acquired pneumonia. J Formos Med Assoc 105:49–55
Yu VL, Hansen DS, Ko WC, Sagnimeni A, Klugman KP, von Gottberg A et al (2007) Virulence characteristics of Klebsiella and clinical manifestations of K. pneumoniae bloodstream infections. Emerg Infect Dis 13:986–993
Nishihira J, Mizue Y, Sakamoto W (1999) Induction of T-kininogen and tumor necrosis factor-alpha by macrophage migration inhibitory factor in vivo. Semin Thromb Hemost 25:557–562
De Miguel-Yanes JM, Andueza-Lillo JA, González-Ramallo VJ, Pastor L, Muñoz J (2006) Failure to implement evidence-based clinical guidelines for sepsis at the ED. Am J Emerg Med 24:553–559
Zambon M, Ceola M, Almeida-de-Castro R, Gullo A, Vincent JL (2008) Implementation of the Surviving Sepsis Campaign guidelines for severe sepsis and septic shock: we could go faster. J Crit Care 23:455–460
Gao F, Melody T, Daniels DF, Giles S, Fox S (2005) The impact of compliance with 6-hour and 24-hour sepsis bundles on hospital mortality in patients with severe sepsis: a prospective observational study. Crit Care 9:R764–R770
Fang CT, Lai SY, Yi WC, Hsueh PR, Liu KL, Chang SC (2007) Klebsiella pneumoniae genotype K1: an emerging pathogen that causes septic ocular or central nervous system complications from pyogenic liver abscess. Clin Infect Dis 45:284–293
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chuang, TY., Lin, CJ., Chou, TC. et al. Positive culture for Klebsiella pneumoniae in relevant sputum samples as a predictor of rapidly fatal outcome in septic patients at medical intensive care units. Eur J Clin Microbiol Infect Dis 29, 969–975 (2010). https://doi.org/10.1007/s10096-010-0953-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-010-0953-8