Abstract
Background
Alongside the recent worldwide expansion of hypervirulent Klebsiella pneumoniae (KP) infections, the available literature regarding cases of community acquired pneumonias (KP-CAP) remains scarce but reports a strikingly high and early mortality. We performed a retrospective multicenter study (7 ICU in France) between 2015 and 2019, comparing prognosis and severity of KP-CAP versus Streptococcus pneumoniae - CAP (SP-CAP).
Methods
For each KP-CAP, three SP-CAP admitted in ICUs within the same center and within the same 6-month window were selected. When available, KP strains were studied, and bacterial virulence was genetically assessed for virulence factors. The primary outcome was in-hospital mortality. Associations between clinical outcomes and type of infection were tested using univariate and multivariate logistic regressions, adjusted for pairing variables.
Results
Twenty-seven KP-CAP and 81 SP-CAP were included. Respective in-hospital mortality rates were 59% (n = 16) and 17% (n = 14, p < 0.001), despite adequate antibiotic therapy. KP-CAP median time from admission to death was 26.9 h [IQR 5.75–44 h] and were significantly associated with higher rates of multiple organ failures (93% vs. 42%, p < 0.001), disseminated intravascular coagulation (12% vs. 1.3%, p = 0.046), septic shock (median lactate on ICU admission 4.60 vs. 2.90 mmol/L, p = 0.030) and kidney failure (KDIGO-3: 87% vs. 44%, p < 0.001). Interestingly, alcoholism was the only identified predisposing factor of KP-CAP. Severity on ICU admission (2-fold higher for KP-CAP) was the only factor associated with mortality in a multivariate analysis.
Conclusion
We described a strong association between KP-CAP infection and higher and earlier mortality when compared to SP-CAP. Moreover, alcoholism was the sole predisposing factor associated with KP-CAP infection. These findings should raise awareness of clinicians involved in the management of severe CAP about this microbiological etiology. Future prospective studies are needed to confirm these results and to design strategies to improve the prognosis of such infections.
Similar content being viewed by others
Background
Community acquired pneumonia (CAP) is a leading cause of death worldwide [1, 2]. CAP mortality rate is particularly high in the intensive care setting (ICU) where it approaches 20%, all microbial causes combined [3, 4]. Klebsiella pneumoniae (KP) was first described in the lungs of alcoholic patients dying from severe CAP, known as Friedlander pneumonia [5]. However, KP remains most known in western countries for its classical pathotype responsible for hospital-acquired infections in fragile subjects and concerns due to the acquisition of antibiotic resistance, notably carbapenemases [6]. Another and highly threatening KP pathotype is hypervirulent-KP (HvKP). HvKP has rapidly spread worldwide since its first description in 1986 in Taiwan, with a clinical signature of multiple secondary infectious foci, community-acquired liver abscesses among young, or diabetic, or otherwise healthy patients [7]. This clinical phenotype is associated with hypermucoviscosity on agar plate culture (identified by string test), reflecting overproduction of its external capsule [8]. Mortality from those HvKP infections is usually low and concern arise from their functional outcome due to possible eye and brain infections [9].
During HvKP expansion, cases of CAP due to KP (KP-CAP) were reported, with a strikingly high and early mortality, ranging from 55 to 100%, first in Taiwan and later in France [10,11,12,13,14,15]. In comparison, a recent 1-year survey of all French ICUs found that the 30-day mortality of Streptococcus pneumoniae (SP) CAP (which is the most frequent cause CAP in the ICU setting), was about 23% [16].
Hence, KP-CAP requiring ICU admission could be an emerging, deadly infection with a possible involvement of HvKP strains and would likely be associated with a higher mortality than of SP-CAP. Former studies on KP-CAP reported high mortality over small data samples and are difficult to compare due to heterogenous setting, patient selection, various epidemiological settings and sometimes lack of control group.
To address these questions, we designed a retrospective multicenter study including ICU patients to evaluate the prognosis of KP infections presenting as CAP, compared to CAP caused by SP (SP-CAP).
Methods
Study design and setting
We conducted a retrospective multicenter case-cohort study among 7 ICUs in the Ile-de-France region of France (Paris and suburb hospitals), between January 1st 2015 and, December 31st 2019.
Participating centers were Louis Mourier hospital (Colombes), EOLE ICU (Pitié-Salpêtrière hospital, Paris), Henri Mondor hospital (Creteil), Kremlin Bicêtre hospital (Kremlin-Bicêtre), Avicenne hospital (Bobigny), Saint Antoine hospital (Paris) and Georges Pompidou European Hospital (Paris).
Cases of KP-CAP were paired with controls, SP-CAP, according to center and year of admission (see statistical analysis below). S. pneumoniae was chosen as a control micro-organism due to its well described mortality rates [16, 17], as well as its widespread distribution across centers, to limit the risk of center-specific recruitment of other GNR-associated pneumonias.
Data origin and data collection
Patients were selected by screening the Programme de Medicalisation des Systèmes d’information (PMSI) database of each center, centralizing encoded diagnosis based on the International Classification of Diseases, 10th Revision (ICD-10).
Diagnosis were reviewed by the investigators based on electronic medical records by a team of trained clinicians (VG, SBG and DR). Data was anonymized and collected on a Redcap database hosted on the Assistance Publique – Hôpitaux de Paris (APHP) servers.
Study population
All patients with an age over 18 admitted to ICUs with a final diagnosis of KP-CAP or SP-CAP were screened. We included all patients with monobacterial KP-CAP or SP-CAP. Experts confirmed CAP diagnosis by reviewing clinical, biological, microbiological and radiologic data allowing for differential diagnosis exclusion (i.e. cardiogenic pulmonary edema, exacerbation of chronic obstructive pulmonary disease with no evidence of CAP, etc.). We excluded nosocomial pneumonias (defined as pneumonia developed 48 h after hospital admission), health care associated pneumonias (defined as patients hospitalized within 3 months before admission including recurrent stays for specific treatment administration, or patients living in an institution) as well as aspiration pneumonias (defined as pneumonias occurring after an evocative event in the medical story). The initial antibiotic regimen (initiated within the first six hours of ICU admission) was deemed adequate if it aligned with the results of antibiotic susceptibility testing (bacterial isolate susceptible to one or more antibiotic).
Study objectives and study criteria
Study objectives were first, to assess the prognosis of KP-CAP infection for patients admitted in an intensive care unit and secondly to assess the severity, predisposing factors, and virulence of KP-CAP infection as compared to those of SP-CAP.
Primary outcome was hospital mortality. Secondary outcomes included (1) evaluation of severity (reflected by the following criteria: Simplified acute physiology score II (SAPS II) on ICU admission, highest Sepsis related organ failure assessment (SOFA) score, within 72 h of ICU stay, multiple organ failure occurrence, septic shock rates [18], acute respiratory distress syndrome (ARDS) [19] rates and mechanical ventilation duration, acute kidney injury rates and severity [20]), (2) predisposing factors (alcoholism, diabetes, immunosuppression and other comorbidities) and (3) bacterial virulence (positivity of blood cultures, search for secondary localization with lumbar puncture or imaging).
Microbiology
When available, KP strains were studied, and bacterial virulence genes were genetically assessed with multiplex PCR testing as described by Compain et al. for the detection of seven virulence factors and K1/K2 capsular serotypes. [21] Standard bacteriological procedures are described in Appendix material 1.
Statistical analysis
Categorical variables were expressed as percentages, quantitative variables as median [interquartile range, IQR]. Normal distribution of variables was tested by Shapiro-Wilk test, and comparisons of independent quantitative and qualitative variables between groups were performed using the Wilcoxon test and the Kruskal-Wallis non-parametric tests as appropriate.
Associations between the bacterial species responsible for the infection and clinical outcomes were tested using univariate and multivariate logistic regressions, and expressed as odds ratios (OR) and their 95% confidence intervals (CI 95%). Multivariate models were adjusted for pairing variables.
A p value < 0.05 was considered significant. Data were analyzed using R 4.1.2 version (http://www.rproject.org).
Pairing
Pairing was achieved by randomly selecting 3 SP-CAP for 1 KP-CAP, admitted in ICUs within the same center and within the same 6-month window (a one-year window was used if not available), to account for caring practices bias.
Results
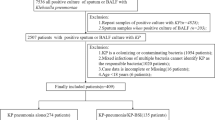
We included a total of 108 patients in the final analysis: 27 KP-CAP and 81 SP-CAP. Appendix Fig. 1 describes the flowchart. Their baseline characteristics are displayed in Table 1 and in Appendix Table 1. Briefly, there was no statistical difference between the two groups except alcohol use disorder which was significantly associated with KP-CAP patients (58% vs. 22%, p = 0.002). Interestingly, we did not observe significant difference for immunosuppression, cancer, cirrhosis, chronic kidney disease (Table 1), neither for Charlson comorbidity index (median 4 [2, 4] vs. 4 [2, 5]). There was no statistical difference in recruitment between centers.
Evolution of SOFA scores from admission to day 3. SOFA scores from admission to day 3 for SP-CAP (left panel) and KP-CAP (right panel) showing boxplots for SOFA at admission (day 0, purple), maximum SOFA from admission to day 3 (blue) and at day 3 (yellow) - SOFA Day 0: KP = 12 (8, 14) vs. SP = 5 (2, 8), p < 0.001 - Max SOFA (Day 0-Day 3): KP = 15 (12, 16) vs. SP = 5 (2, 11), p < 0.001 - SOFA Day 3: KP = 2 (1, 5) vs. 3 (1, 7), NS
In-hospital mortality was higher in the KP-CAP group as compared to the SP-CAP group (59% vs. 17% respectively, p < 0.001). The peak of mortality occurred during the first days following admission, as suggested by a median delay from admission to death among KP-CAP patients of 26.9 h [5.75–44 h].
In an univariate logistic regression, KP-CAP was associated with in-hospital mortality (OR: 6.86, 95% CI: 2.67–18.5, p < 0,001), which was confirmed in a multivariate analysis taking into account the center of recruitment and the year of admission (OR 7.85, 95% CI: 2.92–22.7, p < 0.001). When adjusting on SAPSII score on admission, the association between KP-CAP and hospital mortality was no longer significant (OR 1.84, 95% CI: 0.43–7.61, p = 0.4) (Appendix Table 2). Of note, median SAPSII score on admission was higher among KP-CAP versus SP-CAP patients (82 [56, 92] vs. 40 [28, 62] respectively, p < 0.001) (Table 1). SOFA score on admission was also significantly higher among KP-CAP patients (12 [8, 14]) than that of SP-CAP (5 [2, 8], p < 0.001), as was the maximum SOFA score between ICU admission and day 3 (15 [12, 16] vs. 5 [2, 11] respectively, p < 0.001) (Table 1; Fig. 1). To be noted, time from first symptoms to ICU admission were available for 17/27 KP-CAP patients (median of 48 h, IQR [24–96]) and for 65/81 SP-CAP cases (median 72 h, IQR [48–120]), which was not significantly different (p = 0.9).
During ICU stay, KP-CAP patients presented significantly more severe phenotypes with higher rates of multiple organ failures (93% vs. 42%, p < 0.001), disseminated intravascular coagulation (12% vs. 1.3%, p = 0.046), septic shock (median lactate on ICU admission 4.60 vs. 2.90 mmol/L, p = 0.030) and kidney failure (KDIGO-3: 87% vs. 44%, p < 0.001). There was no difference in ARDS (78% vs. 79%, p > 0.9) even though KP-CAP were more susceptible to receive endotracheal intubation for mechanical ventilation (85% vs. 42%, p < 0.001). (Table 2).
Underlying comorbidities were not solely driving severity: correlation analysis through linear regression showed significantly higher SAPS on admission among KP-CAP patients when adjusted for Charlson Comorbidity Index (mean difference 27 points (95%CI 17–38, p < 0.001) (Appendix Fig. 2).
Moreover, antibiotic susceptibility testing showed that the vast majority of initial empiric antibiotic therapy was adequate as only one was inadequate (a 75-year-old woman diagnosed with KP-CAP and influenza virus co-infection, with KP expressing extended spectrum beta-lactamase, revealing an agammaglobulinemia, who eventually survived). KP-CAP patients presented more positive blood cultures as compared to SP-CAP patients, although this was not significant (52% vs. 23%, p = 0.14) (Table 3). Initial antibiotic regimens are available in Appendix Table 3. No early change of antibiotics (within 24 h of the first line) was noted in the cohort. Prevalence of co-infection with respiratory viruses were not statistically different in KP-CAP (2/27, both influenza virus) and SP-CAP (17/81, details in Appendix Table 4, p = 0.14).
It is noteworthy that, when performed within the first 48 h (11/27), CT scans only showed signs of classical CAP (lobar consolidation = 9, interstitial infiltrate = 2, pleurisis = 1) without specific pattern associated with KP-CAP. In addition, when performed in KP-CAP patients, cerebrospinal fluid analysis (N = 4) was normal and abdominal CT scan did not show hepatic abscess (N = 9).
Finally, available KP strains (n = 4) were screened retrospectively for hypervirulent genotype by multiplex PCR as an exploratory analysis (Appendix Table 5). All tested isolates were compatible with hypervirulent strains as they expressed either a K2 or a K1 serotype (2 each) and were positive for classical Hv-KP virulence factors i.e., hypermucoviscosity (regulator of mucoid phenotype A (rmpA), all positives), and siderophores (iutA, entB, ybts, all positives).
Discussion
Our study showed that infection with monobacterial KP-CAP was associated with a high in-hospital mortality, strikingly superior to that of SP-CAP (58% vs. 17%, p < 0.001) in an ICU setting.
These mortality rates are in accordance with previous studies focusing on KP-CAP. Rafat et al. and Moutel et al. reported mortality rates of 50% and 56%, respectively, whereas others reported even higher rates (75% in Paganin et al. or 100% in Jong et al.) [10, 11, 14, 15]. SP-CAP mortality observed in the present study is close to the 30-day mortality of 23% observed in a recent ICU study in France [16]. To our knowledge, this is the first retrospective cohort describing with detailed clinical and microbiological data, the prognosis and severity of KP-CAP infection in an ICU setting with a robust comparator, SP-CAP, the first and most well-described cause of CAP.
Interestingly, SAPS-II and SOFA scores on ICU admission captured the earlier severity of KP-CAP presentation compared to SP-CAP. These scores captured both the clinical severity and the medical history burden of the patients. [22, 23] This initial dramatic presentation might have been the principal driving factor of the observed mortality, as association between mortality and bacterial cause of the CAP was no longer significant when adjusted of SAPS-II score on admission. This clinical severity continued to worsen rapidly during the first 72 h after admission among KP-CAP patients despite adequate antibiotic therapy. Notably, one patient received a combination of beta-lactam/beta-lactam inhibitor as a first line regimen. This patient died within the first 24 h after ICU admission, and it cannot be excluded that this antibiotic regimen was suboptimal due to PK/PD issues and a potential marked inoculum effect even though the bacterial isolate was deemed susceptible. Even though respiratory distress severity was similar to that of SP-CAP as previously reported, KP-CAP patients displayed a more systemic disease with significantly more multiple organ failure, septic shock, kidney failure, and disseminated intravascular coagulation. Such clinical course resulted in premature death as the median time from admission to death was 27 h [IQR 5.75–44 h], a quite unusual figure in ICU patients hospitalized for lung infections.
Age and comorbidities were equally distributed between KP and SP-CAP groups, including classically described factors associated with CAP mortality. [24,25,26,27] Alcohol misusage was the only risk factor significantly more prevalent among KP-CAP patients, confirming previous data [10,11,12,13,14]. Indeed, correlation analysis between Charlson Comorbidity Index (CCI) and SAPS II on ICU admission revealed a significantly superior severity score in KP compared to SP-CAP patients (average + 27 SAPS II points for every CCI point-increment, Appendix Fig. 2). Therefore, considering roughly similar baseline characteristics between SP and KP-CAP patients, one could hypothesize that the observed increased mortality among KP-CAP was mainly driven by sepsis severity and K. pneumoniae pathogenesis itself. Moreover, when available, pulmonary and abdominal CT scan analysis failed to reveal a specific pattern for KP-CAP. Because of the retrospective nature of the study, biological markers were not collected as there were considerable differences in practices across the different centers, preventing efficient comparisons. However, this analysis is hampered by the lack of systematic assessment of biomarkers and radiological evaluation in all participating centers.
Exploratory analysis revealed that genomes of all available KP strains (n = 4) carried hypervirulence genes typically associated with Hv-KP, both during CAP and liver abscesses. [9, 13, 14, 21] Of those four cases, two died rapidly after admission (75 year-old woman: 31 h, 67 year-old man: 23 h), one died 4 months after the recorded episode (75-year-old man) and one survived (64 year-old man presenting with subacute excavated pneumonia and pleurisies).
Our study has limitations. First, as the identification of patients through French ICD-PMSI database might have induced bias in patient recruitment, [28] we chose strict inclusion criteria to maximize uniformity and comparability in our population, limiting our sample size. Second, delay from hospital admission to antibiotic therapy, a known risk factor for poor prognosis, was not timed precisely in the charts even though the timeframe of initial antibiotic introduction could be restricted to the first six hours based on the electronic records available. However, considering the initial presentation of KP-CAP and frequency of septic shock, it would seem unlikely that antibiotic therapy would have been delayed as compared to SP-CAP patients. Third, the majority of KP strains in our study was not available for genomic analysis. This drawback could reflect the relative unfamiliarity with this potential HvKP presentation or a selection bias in strains storage, particular strains (for example with a hypermucoviscous phenotype) being more likely stored. Our study hints for a broader education of clinicians and microbiologists involved in the care of these patients as similar presentations (i.e., severe septic shock with multiple organ failure and early mortality) could reveal a higher prevalence of hypervirulent strains in respiratory presentations than previously evaluated.
In conclusion, we showed that in comparison to SP-CAP, monobacterial infection with non-health care related KP-CAP was associated with significantly more severe presentation on ICU admission and worse prognosis, including rapidly occurring death.
Our study prompts for future broader prospective studies and registries aiming to decipher the epidemiology and virulence mechanisms underlying such severe conditions. Previous rapid dissemination of HvKP strains (i.e. in Taïwan [7, 8, 29]) as well as recent outbreaks of carbapenem resistant HvKP strains highlight the urgent need of close surveillance of these lethal infections. [30,31,32].
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396:1204–22.
GBD 2016 Lower Respiratory Infections Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990–2016: a systematic analysis for the global burden of Disease Study 2016. Lancet Infect Dis. 2018;18:1191–210.
Arnold FW, Wiemken TL, Peyrani P, Ramirez JA, Brock GN, CAPO authors. Mortality differences among hospitalized patients with community-acquired pneumonia in three world regions: results from the community-acquired Pneumonia Organization (CAPO) International Cohort Study. Respir Med. 2013;107:1101–11.
Walden AP, Clarke GM, McKechnie S, Hutton P, Gordon AC, Rello J, et al. Patients with community acquired pneumonia admitted to European intensive care units: an epidemiological survey of the GenOSept cohort. Crit Care. 2014;18:R58.
Köhler W, Mochmann H. [Carl Friedländer (1847–1887) and the discovery of the pneumococcus–in memory of the centenary of his death]. Z Arztl Fortbild (Jena). 1987;81:615–8.
Munoz-Price LS, Poirel L, Bonomo RA, Schwaber MJ, Daikos GL, Cormican M, et al. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect Dis. 2013;13:785–96.
Russo TA, Marr CM. Hypervirulent Klebsiella pneumoniae. Clin Microbiol Rev. 2019;32:e00001–19.
Paczosa MK, Mecsas J. Klebsiella pneumoniae: going on the offense with a strong defense. Microbiol Mol Biol Rev. 2016;80:629–61.
Rossi B, Gasperini ML, Leflon-Guibout V, Gioanni A, de Lastours V, Rossi G, et al. Hypervirulent Klebsiella pneumoniae in Cryptogenic Liver Abscesses, Paris, France. Emerg Infect Dis. 2018;24:221–9.
Jong GM, Hsiue TR, Chen CR, Chang HY, Chen CW. Rapidly fatal outcome of bacteremic Klebsiella pneumoniae pneumonia in alcoholics. Chest. 1995;107:214–7.
Paganin F, Lilienthal F, Bourdin A, Lugagne N, Tixier F, Génin R, et al. Severe community-acquired pneumonia: assessment of microbial aetiology as mortality factor. Eur Respir J. 2004;24:779–85.
Lin Y-T, Jeng Y-Y, Chen T-L, Fung C-P. Bacteremic community-acquired pneumonia due to Klebsiella pneumoniae: clinical and microbiological characteristics in Taiwan, 2001–2008. BMC Infect Dis. 2010;10:307.
Decré D, Verdet C, Emirian A, Le Gourrierec T, Petit J-C, Offenstadt G, et al. Emerging severe and fatal infections due to Klebsiella pneumoniae in two university hospitals in France. J Clin Microbiol. 2011;49:3012–4.
Rafat C, Messika J, Barnaud G, Dufour N, Magdoud F, Billard-Pomarès T, et al. Hypervirulent Klebsiella pneumoniae, a 5-year study in a French ICU. J Med Microbiol. 2018;67:1083–9.
Moutel M, Peju E, Gastli N, Gavaud A, Mira JP, Charlier C, et al. Bactériémie à Klebsiella pneumoniae hypervirulente en unité de soins intensifs: étude descriptive rétrospective. Médecine et Maladies Infectieuses Formation. 2022;1:8.
Dupuis C, Sabra A, Patrier J, Chaize G, Saighi A, Féger C, et al. Burden of pneumococcal pneumonia requiring ICU admission in France: 1-year prognosis, resources use, and costs. Crit Care. 2021;25:24.
Cillóniz C, Liapikou A, Martin-Loeches I, García-Vidal C, Gabarrús A, Ceccato A, et al. Twenty-year trend in mortality among hospitalized patients with pneumococcal community-acquired pneumonia. PLoS ONE. 2018;13:e0200504.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus definitions for Sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801–10.
ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307:2526–33.
Summary of Recommendation Statements. Kidney International Supplements. 2012;2:8–12.
Compain F, Babosan A, Brisse S, Genel N, Audo J, Ailloud F, et al. Multiplex PCR for detection of seven virulence factors and K1/K2 capsular serotypes of Klebsiella pneumoniae. J Clin Microbiol. 2014;52:4377–80.
Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–63.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European society of intensive care medicine. Intensive Care Med. 1996;22:707–10.
Luna CM, Palma I, Niederman MS, Membriani E, Giovini V, Wiemken TL, et al. The impact of age and comorbidities on the mortality of patients of different age groups admitted with community-acquired pneumonia. Ann Am Thorac Soc. 2016;13:1519–26.
Seymour CW, Gesten F, Prescott HC, Friedrich ME, Iwashyna TJ, Phillips GS, et al. Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med. 2017;376:2235–44.
Rüddel H, Thomas-Rüddel DO, Reinhart K, Bach F, Gerlach H, Lindner M, et al. Adverse effects of delayed antimicrobial treatment and surgical source control in adults with sepsis: results of a planned secondary analysis of a cluster-randomized controlled trial. Crit Care. 2022;26:51.
Garcia-Vidal C, Fernández-Sabé N, Carratalà J, Díaz V, Verdaguer R, Dorca J, et al. Early mortality in patients with community-acquired pneumonia: causes and risk factors. Eur Respir J. 2008;32:733–9.
O’Malley KJ, Cook KF, Price MD, Wildes KR, Hurdle JF, Ashton CM. Measuring diagnoses: ICD code accuracy. Health Serv Res. 2005;40:1620–39.
Chang D, Sharma L, Dela Cruz CS, Zhang D. Clinical epidemiology, risk factors, and control strategies of Klebsiella pneumoniae infection. Front Microbiol. 2021;12:750662.
Zhao Y, Zhang X, Torres VVL, Liu H, Rocker A, Zhang Y, et al. An outbreak of carbapenem-resistant and hypervirulent Klebsiella pneumoniae in an intensive care unit of a major teaching hospital in Wenzhou, China. Front Public Health. 2019;7:229.
Su S, Zhang J, Zhao Y, Yu L, Wang Y, Wang Y, et al. Outbreak of KPC-2 Carbapenem-resistant Klebsiella pneumoniae ST76 and Carbapenem-resistant K2 Hypervirulent Klebsiella pneumoniae ST375 strains in Northeast China: molecular and virulent characteristics. BMC Infect Dis. 2020;20:472.
Huang Y-H, Chou S-H, Liang S-W, Ni C-E, Lin Y-T, Huang Y-W, et al. Emergence of an XDR and carbapenemase-producing hypervirulent Klebsiella pneumoniae strain in Taiwan. J Antimicrob Chemother. 2018;73:2039–46.
Acknowledgements
Not applicable.
Funding
No funding was involved in this study.
Author information
Authors and Affiliations
Contributions
VG contributed to the conception, the acquisition and interpretation of data, drafted the manuscript. SG was a major contributor to the design, acquisition and interpretation of data and was a major contributor in writing the manuscript. TP, SG, HAO, NDP, JM and EG made substantial contributions to the acquisition of data. VLG, NM, and FB performed and analyzed multiplex PCR for KP virulence factors and capsular serotypes. NG made substantial contributions to the design of the study. CM performed the statistical analysis, was a major contributor to the interpretation of the results and contributed to writing the manuscript. DR was a major contributor to the design, acquisition and interpretation of data and was a major contributor in writing the manuscript.
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Every retrospectively collected data in each center was standard of care at the time. All procedures performed involving human participants were in accordance with the ethical standards of the national research committee and with the 1964 Helsinki declaration and its later amendments. This study was approved by local ethic committee (Comité d’Evaluation de l’Ethique des Projets de Recherche Biomédicale (CEERB) Paris Nord N°CER-2021-93). In accordance with French bioethics bylaws, we included all patients except when authorization to use clinical data was not allowed by the patient. All patients were informed of the present study by mail. No patient in our cohort waved their consent, and all successive patients who met inclusion criteria were included.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Grosjean, V., Gressens, S.B., Pham, T. et al. Community-acquired Klebsiella pneumoniae pneumonia in ICU: a multicenter retrospective study. Ann. Intensive Care 14, 69 (2024). https://doi.org/10.1186/s13613-024-01269-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-024-01269-3