Abstract.
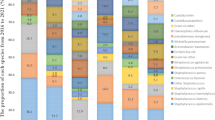
The epidemiology of bacterial pathogens causing bloodstream infection was studied in 16 hospitals in Lombardy (northern Italy) over a 2-year period (1999 and 2000). Overall, 2,924 microorganisms causing significant bacteremia were collected. The most frequent isolates were Escherichia coli (n=663; 22.7%), Staphylococcus aureus (n=534; 18.3%), Staphylococcus epidermidis (n=242; 8.2%), and Pseudomonas aeruginosa (n=176; 6.0%). Unlike Escherichia coli, which was usually acquired from the community, Staphylococcus aureus, Staphylococcus epidermidis, and Pseudomonas aeruginosa were usually acquired in hospitals. Rates of resistance to oxacillin and its associated traits were significantly higher among hospital-acquired staphylococci as compared to those of isolates from the community. Escherichia coli was highly susceptible to extended-spectrum cephalosporins, with a very low percentage of strains producing extended-spectrum ß-lactamases (ESBLs). On the contrary, production of ESBL appeared to be an important mechanism of resistance among nosocomial isolates of Klebsiella pneumoniae. Resistance to ciprofloxacin was widespread in several members of the family Enterobacteriaceae, with rates often exceeding 10%. Moreover, with regard to ciprofloxacin, there were no significant differences between rates of resistance among Enterobacteriaceae causing hospital-acquired infections versus those causing community-acquired infections. Multidrug resistance was commonly observed in Pseudomonas aeruginosa, indicating the need for new antimicrobial agents that are more active against nonfermentative gram-negative bacteria. In conclusion, epidemiological studies of the prevalence and antimicrobial susceptibility patterns of blood isolates in northern Italy appear to provide useful information for both empirical treatment of suspected infections and better management of patients.
Similar content being viewed by others
References
Mylotte JM, Tayara A (2000) Blood cultures: clinical aspects and controversies. Eur J Clin Microbiol Infect Dis 19:157–163
Reimer LG, Wilson ML, Weinstein MP (1997) Update on detection of bacteremia and fungemia. Clin Microbiol Rev 10:444–465
DiGiovine B, Chenoweth C, Watts C, Higgins M (1999) The attributable mortality and costs of primary nosocomial bloodstream infections in the intensive care unit. Am J Respir Crit Care Med 160:976–981
Karchmer AW (2000) Nosocomial bloodstream infections: organisms, risk factors, and implications. Clin Infect Dis 31 [Suppl 4]:139–143
Gikas A, Samonis G, Christidou A, Papadakis J, Kofteridis D, Tselentis Y, Tsaparas N (1998) Gram-negative bacteremia in non-neutropenic patients: a 3-year review. Infection 26:155–159
Leibovici L, Shraga I, Drucker M, Konigsberger H, Samra Z, Pitlik SD (1998) The benefit of appropriate empirical antibiotic treatment in patients with bloodstream infection. J Intern Med 244:379–386
Pfaller MA, Jones RN, Doern GV, Kugler K, the SENTRY Participants Group (1998) Bacterial pathogens isolated from patients with bloodstream infection: frequencies of occurrence and antimicrobial susceptibility patterns from the SENTRY antimicrobial surveillance program (United States and Canada, 1997). Antimicrob Agents Chemother 42:1762–1770
Bouza E, Pérez-Molina J, Muñoz P on behalf of the Cooperative Group of the European Study Group on Nosocomial Infections (ESGNI) (1999) Report of ESGNI-001 and ESGNI-002 studies. Bloodstream infections in Europe. Clin Microbiol Infect 5 [Suppl 2]:1–12
Fluit AC, Jones ME, Schmitz F-J, Acar J, Gupta R, Verhoef J, the SENTRY Participants Group (2000) Antimicrobial susceptibility and frequency of occurrence of clinical blood isolates in Europe from the SENTRY antimicrobial surveillance program, 1997 and 1998. Clin Infect Dis 30:454–460
Bax R, Bywater R, Cornaglia G, Goossens H, Hunter P, Isham V, Jarlier V, Jones R, Phillips I, Sahm D, Senn S, Struelens M, Taylor D, White A (2001) Surveillance of antimicrobial resistance – what, how and whither? Clin Microbiol Infect 7:316–325
Brun-Buisson C, Doyon F, Carlet J, the French Bacteremia-Sepsis Study Group (1996) Bacteremia and severe sepsis in adults: a multicenter prospective survey in ICUs and wards of 24 hospitals. Am J Respir Crit Care Med 154:617–624
Edgeworth JD, Treacher DF, Eykyn SJ (1999) A 25-year study of nosocomial bacteremia in an adult intensive care unit. Crit Care Med 27:1421–1428
Garrouste-Orgeas M, Chevret S, Mainardi JL, Timsit JF, Misset B, Carlet J (2000) A one-year prospective study of nosocomial bactaeremia in ICU and non-ICU patients and its impact on patient outcome. J Hosp Infect 44:206–213
National Committee for Clinical Laboratory Standards (1997) Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard M7-A4. NCCLS, Wayne, PA
Jarlier V, Nicolas M-H, Fournier G, Philippon A (1998) Extended broad-spectrum ß-lactamases conferring transferable resistance to newer ß-lactam agents in Enterobacteriaceae: hospital prevalence and susceptibility patterns. Rev Infect Dis 10:867–878
Dornbusch K, King A, Legakis N, the European Study Group on Antibiotic Resistance (ESGAR) (1998) Incidence of antibiotic resistance in blood and urine isolates from hospitalized patients. Report from a European collaborative study. Scand J Infect Dis 30:281–288
Weinstein MP, Towns ML, Quartey SM, Mirrett S, Reimer LG, Parmigiani G, Reller LB (1997) The clinical significance of positive blood cultures in the 1990s: a prospective comprehensive evaluation of the microbiology, epidemiology, and outcome of bacteremia and fungemia in adults. Clin Infect Dis 24:584–602
Salomão R, Rigato O, Pignatari AC, Freudenberg MA, Galanos C (1999) Bloodstream infections: epidemiology, pathophysiology and therapeutic perspectives. Infection 27:1–11
Rahal JJ (2000) Extended-spectrum ß-lactamases: how big is the problem? Clin Microbiol Infect 6 [Suppl 2]:2–6
Kaye KS, Fraimow HS, Abrutyn E (2000) Pathogens resistant to antimicrobial agents. Infect Dis Clin North Am 14:293–319
Spanu T, Luzzaro F, Perilli M, Amicosante G, Toniolo A, Fadda G (2002) Occurrence of extended-spectrum ß-lactamases in members of the family Enterobacteriaceae in Italy: implications for resistance to ß-lactams and other antimicrobial drugs. Antimicrob Agents Chemother 46:196–202
Vahaboglu H, Öztürk R, Aygün G, Coskunkan F, Yaman A, Kaygusuz A, Leblebicioglu H, Balik I, Aydin K, Otkun M (1997) Widespread detection of PER-1-type extended-spectrum ß-lactamases among nosocomial Acinetobacter and Pseudomonas aeruginosa isolates in Turkey: a nationwide multicenter study. Antimicrob Agents Chemother 41:2265–2269
Rossolini GM, Riccio ML, Cornaglia G, Pagani L, Lagatolla C, Selan L, Fontana R (2000) Carbapenem-resistant Pseudomonas aeruginosa with acquired bla VIM metallo-ß-lactamase determinants, Italy. Emerg Infect Dis 6:312–313
Tsakris A, Pournaras S, Woodford N, Palepou M-F, Babini GS, Douboyas J, Livermore DM (2000) Outbreak of infections caused by Pseudomonas aeruginosa producing VIM-1 carbapenemase in Greece. J Clin Microbiol 38:1290–1292
Luzzaro F, Mantengoli E, Perilli M, Lombardi G, Orlandi V, Orsatti A, Amicosante G, Rossolini GM, Toniolo A (2001) Dynamics of a nosocomial outbreak of multidrug-resistant Pseudomonas aeruginosa producing the PER-1 extended-spectrum ß-lactamase. J Clin Microbiol 39:1865–1870
Docquier J-D, Luzzaro F, Amicosante G, Toniolo A, Rossolini GM (2001) Multidrug-resistant Pseudomonas aeruginosa producing PER-1 extended-spectrum serine-ß-lactamase and VIM-2 metallo-ß-lactamase. Emerg Infect Dis 7:910–911
Acknowledgements
This work was partially supported by a grant from the Italian Ministry for Education (COFIN) and a contribution from Wyeth-Lederle Laboratories (Rome, Italy).
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Members of the AMCLI Lombardia Hospital Infections Study Group (Coordinator: E.F. Viganò), along with participating hospitals, are as follows: M. Arghittu, Ospedale Vizzolo-Predabissi, Melegnano; L. Bertinotti and E.F. Viganò, Ospedale Civile, Legnano; M. Cainarca and E. Guagnellini, Ospedale San Paolo, Polo Universitario, Milan; M. Facchini, Ospedale V. Buzzi, Milan; A. Grossi and C. Ramella, Ospedali Riuniti, Treviglio; F. Luzzaro and A. Toniolo, Ospedale di Circolo, Varese; D. Naldani, Casa di Cura Beato Matteo, Vigevano; G. Nesci, Ospedale Caduti Bollatesi, Bollate; A. Sala and R. Vaiani, Ospedale A. Manzoni, Lecco; R. Sala, Ospedale S. Leopoldo Mandic, Merate; C. Sturla and M. Montuori, Ospedale S. Antonio Abate, Gallarate; R. Terramocci, Ospedale Valduce, Como; P. Troupioti, Ospedale E. Morelli, Sondalo; M. Saudelli, Ospedale Fatebenefratelli, Milan; G. Viola, Istituto Nazionale Tumori, Milan; and A. Vitali, Ospedale S.S. Trinità, Romano di Lombardia.
Rights and permissions
About this article
Cite this article
Luzzaro, F., Viganò, E.F., Fossati, D. et al. Prevalence and Drug Susceptibility of Pathogens Causing Bloodstream Infections in Northern Italy: A Two-Year Study in 16 Hospitals. Eur J Clin Microbiol Infect Dis 21, 849–855 (2002). https://doi.org/10.1007/s10096-002-0837-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-002-0837-7