Abstract
Bloodstream infection coupled with drug resistance in bloodborne bacteria is a major health problem globally. The current study sought to identify the bacterial spectrum, extended-spectrum -lactamase production, and antimicrobial resistance pattern in patients with bloodstream infection. This prospective cross-sectional study was conducted at Arsho Advanced Medical Laboratory, Addis Ababa, Ethiopia from January 2019- until July 2020. Blood collected from patients was inoculated into blood culture bottles and incubated appropriately. Identification, antimicrobial susceptibility testing, and extended-spectrum β-lactamase-production were determined with the VITEK 2 compact system. Of the samples collected, 156 (18.5%) were culture-positive. Klebsiella pneumoniae and Staphylococcus epidermidis were the dominant isolates. In Gram-negative bacteria, the prevalence of drug resistance was the highest against ampicillin (80.8%) and the lowest against imipenem (5.2%). While in Gram-positive bacteria it was the highest against clindamycin and the lowest against vancomycin and daptomycin. The prevalence of multi-drug resistance and extended-spectrum β-lactamase production of Gram-negative bacteria were 41.6% and 34.2%, respectively. The prevalence of bloodstream infection was 18.5%. Serious life-threatening pathogens including S. aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, Escherichia coli, and Enterobacter spp was predominant. The prevalence of multi-drug resistance to both Gram-positive and Gram-negative bacteria and extended-spectrum β-lactamase-production were high but prevalence of carbapenem resistance was low. All these situations call for the establishment of strong infection control strategies, a drug regulatory system, and established antibiotic stewardship in healthcare settings.
Similar content being viewed by others
Introduction
Bloodstream infection is among the most common hospital and community-acquired infections, causing substantial death and morbidity globally1,2. The infection accounts for 10–20% of all hospital-acquired infections and ranks 8th in causing death3. About 48.9 million cases of bloodstream infection (BSI) and 11.0 million BSI-related deaths were reported in 20174. In sub-Saharan countries, BSI is mostly seen in children below 5 years of age, and the death rate of children in developing countries versus the developed ones is found to be in the range of 100–250 and 10–30 per 1000, respectively4.
The rapid increase and spread of antibiotic resistance at different levels in the community and device-associated healthcare infections have become one of the three most important problems facing human health5,6,7. The co-existence of a high burden of infectious diseases and the rapid increase and spread of antimicrobial resistance have made the problem more serious in developing countries8. Consequently, antimicrobial resistance is estimated to cause 700,000 deaths per year, a number projected to rise to 10 million deaths annually by 20509.
A wide range of Gram-negative and Gram-positive bacteria have been isolated in BSIs, among which Acinetobacter spp, P. aeruginosa, E. coli, and K. pneumoniae are the predominant Gram-negative bacteria, while coagulase-negative staphylococci (CoNS), S. aureus, enterococci, and alpha-hemolytic streptococci are the most common Gram-positive bacteria. However, the predominant bacterial species in BSI differ from setting to setting as the result of global differences in epidemiological and geographic features across regions10 These bacteria have also been recognized as the most serious multi-drug-resistant pathogens11. The situation is more serious in low-income countries, where drug abuse is a common problem12. Bacterial isolates that are non-susceptible to at least one drug in three or more drug categories are multi-drug resistance. Limiting uptake of a drug, modification of a drug target, inactivation of a drug, and active efflux of a drug are the main mechanisms of bacterial drug resistance.
Shortage of efficient diagnostic microbiology laboratories and difficulty in accessing effective antibiotic therapy for resistant pathogens have also remained major problems in low-income countries8,13,14. In low-income countries, identification and drug susceptibility testing of bacterial pathogens have been performed by a routine procedure involving a few biochemical tests and an agar diffusion assay against a few antibacterial agents, both of which are less accurate. Against this backdrop, the current study was designed to use the VITEK 2 compact system to determine the prevalence of BSI, the spectrum of bacterial bloodstream pathogens, the prevalence of extended-spectrum β-lactamase-producing Gram-negative bacteria, and their antimicrobial resistance profile.
Materials and methods
Study setting, design, and population
This prospective cross-sectional study was conducted at Arsho Advanced Medical Laboratory, Addis Ababa, Ethiopia, from January 2019 until July 2020. Patients suspected of having a bloodstream infection and those who fulfilled the standard operating procedure (SOP) of blood sample collection in the laboratory were included in the study.
Specimen collection and inoculation
Before blood collection, the skin of each study patient was disinfected with 70% alcohol and subsequently with povidone-iodine. About 10 or 5 ml of venous blood in duplicate sterile tubes were collected aseptically from adults and children, respectively, by qualified nurses. Blood samples were inoculated into duplicate blood culture bottles containing 50 mL (adults) and 25 mL (for children) of sterile brain–heart infusion broth (Oxoid, Basingstoke, Hampshire, UK) under a biosafety cabinet. Blood culture bottles that showed signs of bacterial growth were subjected to Gram staining followed by sub-culturing into a blood agar base (Oxoid, Basingstoke, Hampshire, UK) to which 10% sheep blood was added, Chocolate agar (Oxoid, Basingstoke, Hampshire, UK), and MacConkey agar (Oxoid, Basingstoke, Hampshire, UK) after overnight, 48, and 72 h of incubation at 37 °C. Blood agar and chocolate agar plates were incubated at 37 °C in a 5% CO2 incubator for 24–72 h, while MacConkey agar plates were kept at 37 °C aerobically for 24 h. A terminal subculturing was done on chocolate agar for bottles that did not show visible growth within 7 days before being reported as negative. Blood culture was considered positive if growth was detected in both duplicate blood culture bottles only.
Identification, antimicrobial susceptibility testing, and production of Extended Spectrum β- Lactamase
Identification, antimicrobial susceptibility testing, and production of Extended Spectrum β- Lactamase were determined with the automated VITEK 2 compact system (bioMérieux, France) as per the instruction of the manufacturer.
Test for carbapenemase production
Test for carbapenemase production of bacterial isolates which were resistant to imipenem (IPM 10 µg) and, meropenem (MEM 10 µg) and ertapenem (ERT 10 µg) were subjected for confirmation for carbapenemase production. Confirmation for carbapenemase production in Gram-negative bacteria was conducted by Modified Hodge Test (MHT) where Mueller–Hinton agar plate was inoculated with a 1:10 dilution of a 0.5 densitometer standardized suspension of over-night sub-cultured E. coli ATCC 25922 and streaked for confluent growth using a swab. A 10 µg ertapenem disk was placed in the center, and each test isolate was streaked from the disk to the edge of the plate. A positive Modified Hodge Test (MHT) was indicated by clover leaf-like indentation of the E. coli ATCC 25922 growing along the test organism growth streak within the disk diffusion zone.
Data quality assurance and quality control
Pre-analytical and analytical procedures were performed following the standard operational procedure (SOP) of Arsho Advanced Medical Laboratory. The extracted information (post-analytical activities) such as laboratory findings were checked for eligibility, completeness, and consistency and recorded before entry into a statistical tool.
Data analysis and interpretation
The data was collected, cleaned and analyzed using SPSS version 20. Frequency and percentages of MDR, carbapenemase and ESBL producing gram-negative bacteria were calculated. Tables were used for data presentation.
Ethics statement and patient consent
The present work was conducted in accordance with the Declaration of Helsinki. All ethical considerations and obligations were duly addressed, and the study was carried out after obtaining ethical clearance from the ethical committee of the institute of the Advanced Medical Laboratory, Addis Ababa, Ethiopia. Informed consent was obtained from all subjects and/or their legal guardian(s). Personal information of patients and guardians was treated confidentially. Briefly, the aim of the work and its benefits were clearly described by each adult patient and the guardian. Adult patients and their guardians were not obliged to be involved in the study if they did not agree to participate in it. Once they consented to participate in the study and became disinterested to continue, they were free to withdraw from the study at any time during the course of the study.
Results
Socio-demographic characteristics
The demographic characteristics of the study patients are shown in Table 1. A total of 844 patients were included in the current work. Among these, 485 (57.5%) were females, and 359 (42.5%) were males. The majority of the study patients were in the age group of 25–44, and the least were in the age group of < 1 year (40; 4.7%). Out of the 844 blood samples collected, 156 (18.5) were culture-positive. Regarding gender, of 485 female patients, 88 (10.4%) were culture-positive. Similarly, of 359 male patients, 68 (8.1%) were culture-positive. Females were more affected than males. Regarding age, patients in the age group of 25–44 (5.1%) were more affected, followed by the age group 45–64 (4.7%), and by the age group > 65 (2.8).
Distribution of bacterial pathogens
The spectrum of bloodborne bacteria in the present study is shown in Table 2. A total of 156 bacterial isolates were documented, of which 79 (50.6%) were Gram-negative and 77 (49.4%) were Gram-positive. K. pneumoniae was the dominant Gram-negative bacterium (14.1%), followed by E. coli (9.0%) and Acinetobacter lwoffii (5.8%). Enterobacter cloacae, P. aeruginosa, and Acinetobacter baumannii were recovered in the same proportion, i.e., 4.5%. Staphylococcus epidermidis, a coagulase-negative Staphylococcus species, was the dominant Gram-positive isolate (17; 10.9%) followed by S. aureus (15; 9.6%). Enterococcus faecalis was the only non-Staphylococcus Gram-positive bacterium isolated in our study.
Percentage antimicrobial resistance profile of Gram-negative bacteria
Table 3 shows the overall percentage antimicrobial resistance profile of Gram-negative bacteria as well as the drug resistance profile of each pathogen per drug category. The overall drug resistance profile was the highest against ampicillin (80.8%) and the lowest against imipenem (5.2%). The drug resistance profile of the most commonly isolated Gram-negative bacterial pathogen was as follows: Resistance to Carbapenem: K. pneumoniae with a resistance rate of 2.0% to meropenem versus 1.0% to imipenem; E. coli with a resistance rate of 1.0% to imipenem versus 7.1% to meropenem; A. baumannii with a resistance rate of 0% to both meropenem and imipenem; E. cloacae with a resistance rate of 0% to both meropenem and imipenem, and P. aeruginosa with a resistance rate of 14.3% to meropenem versus 1.0% to imipenem. Resistance to cephalosporins:—Gram-negative bacteria were tested against 9 cephalosporin drugs. Out of 22 isolates of K. pneumoniae tested ≥ 82% of the isolates were resistant to 8 cephalosporin drugs except for cefoxitin with a resistance rate of 9.1%. Of the 14 isolates of E. coli tested, ≤ 50% of the isolates were resistant to 7 drugs, but 71.4% to cephalothin and 57.1% to cefazolin. The resistance rate of A. baumannii to cephalosporin drugs extended from 71.4% to 100%, where the isolates were 100% resistant to six cephalosporin drugs. The resistance rate of P. aeruginosa was 100% to 7 cephalosporin drugs except for cefepime (28.6%) and ceftazidime (42.9%). Resistance rate to aminoglycosides: K. pneumoniae, 32% to tobramycin vs 72.7% to gentamycin; E. coli, 14.3% to tobramycin vs 28.6% to gentamycin; A. baumannii, 28.6% to both tobramycin and gentamycin; P. aeruginosa, 14.3% to both tobramycin and gentamycin. Resistance rate against fluoroquinolones:—K. pneumoniae, 13.6% to levofloxacin vs 40.9% to ciprofloxacin; E. coli 50% to both levofloxacin and ciprofloxacin; A. baumannii 26.6% to levofloxacin vs 71.4% to ciprofloxacin; P. aeruginosa, 26.6 to levofloxacin vs 30% to ciprofloxacin. Resistance to β -lactam/β-lactamase inhibitor combination drugs:—K. pneumoniae 50.0% to ampicillin/clavulanic acid vs 32% to piperacillin/ tazobactam), E. coli, 21.4% to ampicillin/ clavulanic acid vs 14.3% piperacillin/tazobactam; A. baumannii 100% to ampicillin/ clavulanic acid vs 71.4% to piperacillin/ tazobactam; P. aeruginosa,100% to ampicillin/clavulanic acid vs 42.9% to piperacillin/ tazobactam.
Percentage antimicrobial resistance profile of Gram-positive bacteria
The antimicrobial resistance profile of Gram-positive cocci is shown in Table 4. Gram-positive bacteria were more resistant to clindamycin (70.1%), erythromycin (63.6%) tetracycline (61.0%). The resistance rate of Gram-positive bacteria against linezolid (2.6%), nitrofurantoin (2.6%), moxifloxacin (6.5%), and gentamycin (9.1%) was very low. Vancomycin (glycopeptide) and daptomycin (a cyclic lipopeptide antibiotic) showed a 100% susceptibility to all Gram-positive bacteria. E. faecalis showed a high level of resistance toward erythromycin (83.3%), minocycline (83.3%), tetracycline (83.3%), and quinupristin/dalfopristin (100%) while the species was 100% susceptible to high-level antibiotics such as vancomycin, daptomycin, and linezolid, a synthetic drug of the class oxazolidinones.
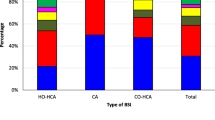
Multi-drug-resistant profile of Gram-negative bacteria
The MDR pattern of Gram-negative bacteria was determined by considering the following nine classes of antibiotics: Penicillin, cephalosporin; aminoglycosides; quinolones (fluoroquinolones); trimethoprim/sulfamethoxazole; tetracyclines; nitrofurantoin, combination drugs, and carbapenems. The overall prevalence of MDR Gram-negative bacteria was 41.6 (32/79) of which 77.3% (17/22) of K. pneumoniae, 85.8% (6/7) of A. baumannii, 28.6% (2/7) of P. aeruginosa, and 28.6% (4/14) of E. coli were MDR (Table 5).
Multidrug-resistant profile of Gram-positive bacteria
The MDR pattern of Gram-positive bacteria was determined by considering the following classes of antibiotics: aminoglycosides; quinolones (fluoroquinolones); trimethoprim/sulfamethoxazole; tetracyclines; nitrofurantoin, glycopeptide; a cyclic lipopeptide antibiotic; oxazolidinones; glycylcycline; streptomycin; lincomycin; macrolide; antimicrobials. The overall MDR prevalence rate of Gram-positive bacteria was 58.2 (46/77) of which 66.7% (10/15) of S. aureus, 66.7% (4/6) of E. faecalis, 66.7% (8/12) of S. warneri, and 52.9% (9/17) of S. epidermidis were MDR (Table 6).
Prevalence of extended-spectrum β- lactamase (ESBL) producing gram-negative bacteria
The overall prevalence of ESBL-producing Gram-negative was 26 (34.2%). There was intra-species variation in ESBLs production in which the highest percentage was recorded among K. pneumoniae, 55.5% (12/22) followed by E. coli, 50.0% (6/14), and the lowest production observed in K. oxytoca with 25% 1/4) (Table 7).
Discussion
In the present study, out of 844 blood samples processed for culture, 156 (18.5%) were culture-positive. Our finding was lower than BSI reported by earlier studies15,16,17,18 but higher than other studies19,20,21. The disparity in blood culture positivity rates in different studies could be attributed to differences in result interpretation, the volume of blood used (5 ml versus 10 ml), sample size, and the number of blood cultures to which the blood sample was inoculated (one versus two blood culture bottles).
In our study, 50.6% of BSIs were caused by Gram-negative while 49.4% were by Gram-positive bacteria. Gram-positive predominance BSIs (54% Gram-positive vs 45% Gram-negative) by Arega et al.16, (88.8% Gram-positive vs 11.2% Gram-negative) by Sharma et al.17, (52.7% Gram-positive vs 47.3% Gram-negative) by Arora et al.18, and (82.1% Gram-positive vs 17.9% Gram-negative bacteria) by Moyo et al.19 were documented. On the other hand, Gram-negative bacteria's predominance in causing BSIs was reported by many other researchers15,20. In the current work, coagulase-negative staphylococci Gram-positive bacteria, were the most common bacterial pathogen causing BSI. Our result was in concordance with various studies12,21. Although about > 85% of CoNS was noted as contaminants in the past22, studies have shown that CoNS are frequently associated with pediatric bloodstream infections and adults in settings where implanting of intravascular catheters and indwelling prosthetic devices are practiced23,24. The high prevalence of CoNS in the present study could partly be explained by the fact that about 19.0% of blood was collected from patients aged below 15 years and/or may be due to the use of an improved and highly sensitive automated machine for bacterial identification. However, as CoNS are also possible skin contaminants, their pathogenic status should be verified by other means before starting therapy. Staphylococcus aureus was the second most frequent cause of BSI followed by E. faecalis. S. aureus as the commonest Gram-positive bacterium causing BSIs has been demonstrated by other studies23,24.
Among the many Gram-negative bacteria reported in our study, those identified as serious life-threatening pathogens by WHO7 such as K. pneumoniae, A. baumannii, P. aeruginosa, and Enterobacter spp were the commonest isolates. Our result concurs with the report of Tsegaye et al.15 Khan et al.21, Kasanga et al.25 Ahmed et al.26.
Evaluation of the drug resistance pattern of Gram-negative bacterial pathogens to different drug categories demonstrated that they were highly resistant to most drug categories except carbapenems. Their percentage drug resistance rate extended from 5.2% for imipenem to 80.8% for ampicillin. Their overall drug resistance profile to the nine cephalosporin drugs tested, except for cefoxitin, ceftazidime, and cefepime was very high. Importantly, cephalosporins were less effective against the most common and important pathogens. Klebsiella pneumoniae with a resistance rate extending from 82.0% to 91.0% except for cefoxitin (9.1%); A. baumannii with a resistance rate extending from 71.4% to 100%; P. aeruginosa with a resistance rate of 100% except for ceftazidime (42.9%) and cefepime (28.6%) was alarming. Our finding was similar to that of Hautala et al.27 that demonstrated the frequency of drug-resistant Gram-negative bacteria to cephalosporins varied from 75.0% for cefazolin to 84.2% for cefuroxime. Our result also agreed marginally with the results of recent studies conducted in Ethiopia28,29,30,31,32. Such high levels of drug resistance by Gram-negative bacteria to cephalosporin could be attributed that they have been used in many settings for empirical treatment mainly due to their broad-spectrum activity and low toxicity. More importantly, however, Gram-negative bacteria are the main producers of enzymes (ESBLs) that inactivate drugs with beta-lactam functional groups such as cephalosporins. The observation of a high drug-resistant profile of Gram-negative bacteria to cephalosporines was suggestive of the fact that 50.0% E. coli, 55.0% K. pneumoniae, 42% of A. baumannii, and 28.6% P. aeruginosa isolates in the present study were ESBL producers. Why E. coli was comparatively less resistant to cephalosporins in the present work given that the bacterium was the second most producer of ESBL in the current study was obscure. Similarly, less resistance rate of E. coli to cephalosporins was reported from Nepal33. Therefore, with caution, our study demonstrated that similar to penicillins, new cephalosporins (2nd–4th generations) synthesized with an expansion of their activities against Gram-negative rods as the goal is declining. Gram-negative bacteria isolates were highly sensitive to carbapenem with a resistance level of 6.5% to meropenem vs 5.2% to imipenem. A lower resistance rate of Gram-negative bacteria to carbapenem (1.7%) to both meropenem and imipenem than our study has been reported in a study conducted in Ethiopia by Beyene et al.28. However, higher resistance rates of Gram-negative bacteria to carbapenem than our study have been reported in related studies conducted in Ethiopia29,31,32. Despite the poor drug-controlling system in Ethiopia coupled with the absence of drug stewardship, the resistance of Gram-negative bacteria to carbapenem is generally low. The high sensitivity of Gram-negative bacteria to carbapenems could be attributed to the fact that carbapenems are highly controlled antibiotics (they are not readily available over the counter) in Ethiopia. Furthermore, carbapenems are β-lactam drugs that are structurally different from penicillins and cephalosporins that are not easily inactivated by most β-lactamases. Yet the prevalence of drug resistance to the carbapenems in our study is frightening in a country where alternative antibiotics are scarce. Moreover, the emergence and spread of carbapenem-resistant bacteria are more problematic in developing countries due to the lack of laboratory capacity for their diagnosis.
The analysis of the drug resistance profile of the most commonly isolated Gram-negative bacteria per drug category demonstrated variable results. The resistance rate of K. pneumoniae, the commonest Gram-negative bacterium in our study was 9.0% to meropenem and 4.5% to imipenem. Our result agreed with the results of studies conducted in Ethiopia31, and China34. The occurrence of resistant isolates of K. pneumoniae to aminoglycoside in the present work was variable being 72.7% for gentamycin and 32.0% for tobramycin. Similar results were reported from Ethiopia by many studies15,28,30,32. Yet a seventy percent resistance rate of the pathogen to tobramycin reported by Beyene et al.28 was extremely high compared to our result. The incidence of resistant isolates of the pathogen to quinolones in our study was 13.6% for levofloxacin and 41.0% for ciprofloxacin which is lower than compared resistance rates that extend from 40.0% to 69.0%15,28,30,32. Among drugs of β-lactam/β-lactamase inhibitor combinations, piperacillin/tazobactam was better active against K. pneumoniae with a resistance rate of 26.6% than amoxicillin/ clavulanic acid with a resistance level of 52.0%. A notable difference was not observed between our result and the results reported by studies conducted in Ethiopia28,29.
The resistance rate of E. coli to carbapenem in our study was 7.1%; (0.0% to imipenem vs 7.1% to meropenem). Our finding was similar to reports from China34, USA35, and Europe36,37. A resistance rate of 28.8% to both gentamycin and tobramycin of the pathogen in our study was comparable with 5–25% from Europe36,37. A 50% resistance of E. coli to both levofloxacin and ciprofloxacin in this study correlated with quinolone resistance of E. coli in the USA (41.8%) and EU countries (11 to 52%)38. The pathogen was susceptible to β-lactam/β-lactamase inhibitor combinations, piperacillin/tazobactam with a resistance rate of 14.3%, and amoxicillin/ clavulanic acid with a resistance rate of 21.4%.
Over 70% of A. baumannii was resistant to 15 drugs of which 100% of the isolates were resistant to eight drugs. Furthermore, 14.3% of the pathogen was resistant to carbapenems, the most active drugs to Gram-negative bacteria in our study demonstrating that Acenitobacter species were the most carbapenem-resistant next to P. aeruginosa. It has been shown that > 50% of isolates of A. baumannii were resistant to carbapenems, quinolones, and aminoglycosides in Europe38.
Pseudomonas aeruginosa in our study was also 100% resistant to 12 drugs and the resistance rate of the bacterium was 28.0% to meropenem and 14.3% to imipenem. The resistance rate of the bacterium to aminoglycosides is 14.3% to both gentamycin and tobramycin, quinolones (0% to ciprofloxacin vs 28.6% to levofloxacin), and cefepime (28.6%) are relatively low. In Europe, P. aeruginosa with high resistance rates to aminoglycosides, ceftazidime, quinolones, piperacillin-tazobactam, and carbapenems have been reported39.
The higher drug resistance of the non-fermentative Gram-negative bacteria compared to the enterobacteria noted in our study is not amazing. Non-fermentative Gram-negative bacteria are recognized to be naturally resistant to the most important classes of antibiotics. Higher intrinsic resistance in these bacteria has been associated with their lower cellular permeability and higher efflux activities39. It has been noted that the drug resistance rate against Gram-negative bacteria was higher for meropenem than imipenem, ciprofloxacin than levofloxacin, gentamycin than tobramycin and amoxicillin/clavulanic acid than piperacillin-tazobactam. The pattern of drug resistance noted in our work was associated with the pattern of antibiotic use in Ethiopia. Generally, meropenem, ciprofloxacin, gentamycin and amoxicillin/clavulanic acid are the most commonly prescribed antibiotics in Ethiopia. Higher resistance rates of these drugs than drugs in the same drug category supported the notion that extensive use of antibiotics is a key driving force for the development of drug resistance40.
The frequency of drug resistance in Gram-positive cocci differed from 0.0% for vancomycin and daptomycin to 70.1% for clindamycin. Their drug resistance rate to the commonly prescribed antibiotics was high and corresponded with the findings of related studies in the country15,18. The high antibiotic resistance reported against these drugs in this study may be due to easy accessibility over the counter to most antibiotics and a high selection pressure due to the extensive use of these antibiotics. However, Gram-positive bacteria showed 100% susceptibility to vancomycin and daptomycin, although reduced susceptibility to glycopeptides (vancomycin) in S. aureus has emerged during the last decades. All Gram-positive bacterial isolates were also 100% susceptible to daptomycin despite the development of resistance to this lipopeptide antibiotic reported by Chong et al.41. All isolates of Gram-positive bacteria in our study were also 100% susceptible to linezolid except S. epidermidis with a resistance rate of 5.9% and S. intermedius with a resistance rate of 20%. About 1–5% linezolid-resistant coagulase-negative staphylococci have been reported to oxazolidinone by Decousser et al.42. Enterococcus faecalis was extremely resistant to erythromycin (83.3%), minocycline (83.3%), quinupristin (100%) tetracycline (83.3%) nevertheless all strains of the bacterium were 100 susceptible to vancomycin, daptomycin, and linezolid. Glycopeptide resistance in enterococci is a serious problem in the USA. It has been reported that by 2007, > 80% of E. faecium isolates in USA hospitals were resistant to vancomycin42,43.
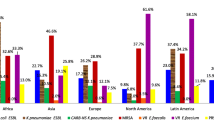
The phenotypic data generated in the current study showed that 32.9% of Gram-negative bacteria were ESBL producers. The prevalence of ESBL production noted in the present study did not substantially deviate from earlier studies conducted within and outside Ethiopia31,44,45,46. Nevertheless, the higher prevalence rate of ESBL production than the prevalence of the current study was reported within Ethiopia and abroad29,30,44,45,46. K. pneumoniae (55.0%), E. coli (50.0%), and A. baumannii (42.9%) were the commonest ESBL producers in the present study. E. coli with a frequency of 83.13% and K. pneumoniae with a frequency of 78.84% are reported as the two major ESBL producers in Mexico46. Similarly, E. coli with a frequency of 70.9% and Klebsiella spp. with a magnitude of 59.4% are recorded as the commonest ESBL produces in Nepal33.
The rapid increase and spread of multidrug-resistant bacteria are major threats to public health all over the world. The problem is more significant in Enterobacteriaceae because of their omnipresence in the environment and the relative ease of gaining plasmids containing genes that encode for ESBLs and other resistance genes that confer resistance to many other classes of antibiotics47. The magnitude of MDR bacteria in this study was 41.6% which is lower than almost two-fold prevalence rates reported by, Moges et al. (85.8%)30 Beyene et a, (94.5%)28, Alebel et al. (81.1%)32 nevertheless comparable with prevalence rate demonstrated from studies conducted in Ethiopia by Abdeta et al. 45.2%29 Perez48, Bitew et al. (41.2%)49, Biset et al. 56.7%44. In the current study, 85% of A. baumannii, 77.3% of K. pneumoniae, (28.6%), of E. coli, and (28.6%) of P. aeruginosa were multidrug-resistance strains. About 32 multidrug-resistant bacteria out of a total of 79 Gram-negative bacteria were high. As a developing country, increased use of drugs over the counter, incomplete courses of therapy, and prolonged therapy for recurrent bacterial diseases are commonly practiced in Ethiopia. These practices could be cited as possible factors for the high prevalence of MDR Gram-negative bacterial species noted in the current study.
The overall prevalence of MDR Gram-positive bacteria in our study was 59.7%. About 66.7% of S. aureus, 66.7% of E. faecalis, 66.7% of S. warneri, and 52.9% of S. epidermidis were MDR. The overall prevalence of MDR Gram-positive bacteria in our study was higher than those reported by Asres et al. (53.3%)50, and Azene et al. (52.7%)51 but lower than those reported by Godebo et al. (66%)52 and Alam et al. (69.0%)12. The possible explanation for such irregularities in the prevalence of MDR bacteria might be the difference in study settings where previous studies solely included inpatients where higher MDR strains are expected. S. aureus was the most predominant MDR bacterium in almost all of these studies.
Limitations of the study
The drug resistance reported in this study is primarily phenotypic. To this end determination of drug resistance genes by molecular methods is the aim of our future studies.
Conclusion
The prevalence of bloodstream infection was 18.5%. Yet most bacterial species isolated in the study were serious life-threatening bloodborne pathogens. Multidrug resistance in blood-borne pathogens and ESBL production in Gram-negative bacteria were high. Although carbapenem resistance prevalence was low, the recognized resistance to the drugs in our study is alarming since alternative drugs and laboratory capacity for their detection are hardly available. All these situations call for the establishment of strong infection control strategies, a drug regulatory system, and established antibiotic stewardship in healthcare settings.
Data availability
The dataset generated and/or analyzed during the current study is available from the corresponding author upon reasonable request.
References
Mehdinejad, A., Khosravi, A. D. & Morvaridi, A. Study of prevalence and antimicrobial susceptibility pattern of bacteria isolated from blood culture. J. Biol. Sci. 9, 249–253 (2009).
Garg, A., Anupurha, S., Garg, J., Goyal, R. K. & Sen, M. R. Bacteriological profile and antimicrobial resistance of blood culture isolates from a university hospital. J. Indian Acad. Clin. Med. 8, 139–143 (2007).
James, A. K. et al. Prevalence and antimicrobial susceptibilities of bacteria isolated from blood cultures of hospitalized patients in the United States in 2002. Ann. Clin. Microbiol. Antimicrob. 3, 7 (2004).
Rudd, K. E. et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the Global Burden of Disease Study. Lancet 395, 200–211 (2020).
Shaikh, S., Fatima, J., Shakil, S., Rizvi, S. M. D. & Kamal, M. A. Prevalence of multidrug-resistant and extended-spectrum beta-lactamase-producing Pseudomonas aeruginosa in a tertiary care hospital. Saudi J. Biol. Sci. 22, 62–64 (2015).
Negvekar, V., Sawant, S. & Amey, S. Prevalence of multidrug-resistant Gram-negative bacteria cases at admission in a multispecialty hospital. J. Glob. Antimicrob. Resist. 9, 457–461 (2020).
World Health Organization. Antimicrobial Resistance: Global Report on Surveillance 2014 (WHO, 2014).
Ayukekbong, J. A., Ntemgwa, M. & Atabe, A. N. The threat of antimicrobial resistance in developing countries: Causes and control strategies. Antimicrob. Resist. Infect. Control 6, 47 (2017).
Piddock, L. J. Reflecting on the final report of the O’Neill review on antimicrobial resistance. Lancet Infect. Dis. 16, 767–768 (2016).
Diekema, D. J. et al. Epidemiology and outcome of nosocomial and community-onset bloodstream infection. J. Clin. Microbiol. 41, 3655–3660 (2003).
Gigliotti, C. et al. Escherichia coli and Staphylococcus aureus: bad news and good news from the European Antimicrobial Resistance Surveillance Network (EARS-Net, formerly EARSS), 2002 to 2009. Euro-surveillance 16, 19819. https://doi.org/10.2807/ese.16.11.19819-en (2011).
Alam, M. S., Pillai, P. K., Kapur, P. & Pillai, K. K. Resistant patterns of bacteria isolated from bloodstream infections at a university hospital in Delhi. J. Pharm. Bio-Allied. Sci. 3, 525–530 (2011).
Byarugaba, D. K. A view on antimicrobial resistance in developing countries and responsible risk factors. Int. J. Antimicrob. Agents. 24, 105–110 (2004).
Le Doare, K., Bielicki, J., Heath, P. T. & Sharland, M. Systematic review of antibiotic resistance rates among Gram-negative bacteria in children with sepsis in resource-limited countries. J. Pediatric. Infect. Dis. Soc. 4, 11–20 (2015).
Tsegaye, E. A. et al. Bacterial and fungal profile, drug resistance pattern and associated factors of isolates recovered from blood samples of patients referred to Ethiopian Public Health Institute: A cross-sectional study l. BMC Infect. Dis. 21, 1201 (2021).
Arega, B., Woldeamanue, Y., Adane, K., Sheriff, A. A. & Asrat, D. Microbial spectrum and drug-resistance profile of isolates causing bloodstream infections in febrile cancer patients at a referral hospital in Addis Ababa Ethiopia. Infect. Drug Res. 11, 1511–1519 (2018).
Sharma, M., Goel, N., Chaudhary, U., Aggarwal, R. & Arora, D. R. Bacteremia in children. Indian J. Pediatric. 69, 1029–1032 (2002).
Arora, U. & Devi, P. Bacterial profile of bloodstream infections and antibiotic resistance pattern of isolates. J.K. Sci. 9, 186–190 (2007).
Moyo, S., Aboud, S., Kasubi, M. & Maselle, S. Y. Bacteria isolated from bloodstream infections at a tertiary hospital in Dares Salaam, Tanzania-antimicrobial resistance of isolates. S. Afr. Med. J. 100, 835–838 (2010).
Shrestha, S., Amatya, R. & Shrestha, R. Frequency of blood culture isolates and their antibiogram in a teaching hospital. J. Nepal Med. Assoc. 52, 692–697 (2014).
Khan, M. A., Mohamed, A. M., Faiz, A. & Ahmad, J. Enterobacterial infection in Saudi Arabia: First record of Klebsiella pneumoniae with triple carbapenemase genes resistance. J. Infect. Dev. Ctries. 13, 34–41 (2019).
Weinstein, P. M. et al. The clinical significance of positive blood cultures in the 1990s: A prospective comprehensive evaluation of the microbiology, epidemiology, and outcome of bacteremia and fungemia in adults. Clin. Infect. Dis. 24, 584–602. https://doi.org/10.1093/clind/24.4.584 (1997).
Jain, A., Agarwal, A., Verma, R. K., Awasthi, S. & Singh, K. P. Intravenous device associated bloodstream staphylococcal infection in pediatric patients. Indian J. Med. Res. 134, 193–199 (2011).
Mehta, M., Dutta, P. & Gupta, V. Antimicrobial susceptibility pattern of blood isolates from a teaching hospital in north India. Jpn. J. Infect. Dis. 58, 174–176 (2005).
Kasanga, M. et al. antimicrobial susceptibility patterns of bacteria that commonly cause bacteremia at a tertiary hospital in Zambia. Future Microbiol. 15, 1735–1745 (2020).
Ahmed, D. et al. Bacterial etiology of bloodstream infections and antimicrobial resistance in Dhaka, Bangladesh, 2005–2014 Antimicrob. Resist. Infect. Contr. 6, 2. https://doi.org/10.1186/s13756-016-0162-z (2017).
Hautala, T. et al. Blood culture Gram stain and clinical categorization based empirical antimicrobial therapy of bloodstream infection. Intern. J. Antimicrob. Agents. 25, 329–333 (2005).
Beyene, D., Bitew, A., Fantew, S., Mihret, A. & Evans, M. Multidrug-resistant profile and prevalence of extended-spectrum β-lactamase and carbapenemase production in fermentative Gram-negative bacilli recovered from patients and specimens referred to National Reference Laboratory, Addis Ababa, Ethiopia. PLoS ONE 14(9), e0222911 (2019).
Abdeta, A. et al. Phenotypic characterization of carbapenem non-susceptible gram-negative bacilli isolated from clinical specimens. PLoS ONE 16(12), e0256556 (2021).
Moges, F. et al. Multidrug resistance and extended-spectrum beta-lactamase-producing Gram-negative bacteria from three Referral Hospitals of Amhara region, Ethiopia. Ann. Clin. Microbiol. Antimicrob. 20(1), 1–2. https://doi.org/10.1186/s12941-020-00409-4PMID33402178 (2021).
Gashaw, M. et al. Emergence of high drug-resistant bacterial isolates from patients with healthcare-associated infections at Jimma University medical center: A cross-sectional study. Antimicrob. Resist. Infect. Control 7, 1–8. https://doi.org/10.1186/s13756-018-0431-0 (2018).
Alebel, M., Mekonnen, F. & Mulu, W. Extended-spectrum β-lactamase and carbapenemase producing gram-negative bacilli infections among patients in intensive care units of Felegehiwot Referral Hospital: A prospective cross-sectional study. Infect. Drug Resist. 14, 391 (2021).
Lamichhane, B. Antibiotic resistance patterns of Gram-negative isolates in a tertiary care hospital of Nepal. Asian J. Pharm. Clin. Res. 7, 30–33 (2014).
Xu, A. et al. National epidemiology of carbapenem-resistant and extensively drug-resistant Gram-negative bacteria isolated from blood samples in China in 2013. Clin. Microbiol. Infect. https://doi.org/10.1016/j.cmi.2015.09.015 (2016).
Guh, A. Y. et al. Epidemiology of carbapenem-resistant Enterobacteriaceae in 7 US communities, 2012–2013. JAMA 314, 1479–1487 (2015).
WHO Regional Office for Europe. Central Asian and Eastern European Surveillance of antimicrobial resistance. Ann Rep 2014.
EARS-Net: European Centre for Disease Prevention and Control (ECDC), Antimicrobial resistance interactive database (Internet). Stockholm (Sweden): ECDC (cited 2015 Oct 22).
European Centre for Disease Prevention and Control (ECDC). Annual epidemiological report 2014. Antimicrobial resistance and healthcare-associated infections. 2015.
Moubareck, C. A., Halat, D. H., Akkawi, C. H., Sarkis Peters, C. & Celiloglu, D. K. Role of outer membrane permeability, efflux mechanism, and carbapenemases in carbapenem non-susceptible Pseudomonas aeruginosa from Dubai hospitals: Results of the first cross-sectional survey. Int. J. Infect. Dis. 84, 143–150 (2019).
Shallcross, L. J. & Davies, D. S. Antibiotic overuse: A key driver of antimicrobial resistance. Br. J. Gen. Pract. 64, 604–605 (2014).
Chong, Y. P. et al. Clinical and microbiologic analysis of the risk factors for mortality in patients with heterogeneous vancomycin-intermediate Staphylococcus aureus bacteremia. Antimicrob. Agents. Chemother. 59, 3541–3547 (2015).
Decousser, J. W. et al. Microbs Study Group. Susceptibility trends including the emergence of linezolid resistance among coagulase-negative staphylococci and methicillin-resistant Staphylococcus aureus from invasive infections. Int. J. Antimicrob. Agents 46, 622–630 (2015).
O’Driscoll, T. & Crank, C. W. Vancomycin-resistant enterococcal infections: Epidemiology, clinical manifestations, and optimal management. Infection Drug Res. 8, 217–230 (2015).
Biset, S., Moges, F., Endalamaw, D. & Eshetie, S. Multi-drug resistant and extended-spectrum β-lactamases producing bacterial uropathogens among pregnant women in Northwest Ethiopia. Ann. Clin. Microbiol. Antimicrob. 19, 25 (2020).
Ogbolu, D. O., Daini, O. A., Ogunledun, A., Alli, A. U. & Webber, M. A. High levels of multidrug resistance in clinical isolates of gram-negative pathogens from Nigeria. Int. J. Antimicrob. Agents. 37, 62–66 (2011).
Ghimire, A., Acharya, B. & Tuladhar, R. Extended Spectrum β-Lactamase (ESBL) producing multidrug-resistant gram-negative bacteria from various clinical specimens of patients visiting a Tertiary Care Hospital. Tribhuvan Univ. J. Microbiol. 4, 1–8 (2018).
Uc-Cachón, A. H., Gracida-Osorno, C., Luna-Chi, I. G., Jiménez-Guillermo, J. G. & Molina-Salinas, G. M. High prevalence of antimicrobial resistance among gram-negative isolated bacilli in intensive care units at a tertiary-care hospital in Yucatán Mexico. Medicina (Kaunas) 55, 588 (2019).
Perez, F. & Van Duin, D. Carbapenem-resistant Enterobacteriaceae: A menace to our most vulnerable patients. Clevel. Clin. J. Med. 80, 225–233 (2013).
Bitew, A. & Tsige, E. High prevalence of multidrug-resistant and extended-spectrum β-lactamase-producing enterobacteriaceae: A cross-sectional study at arsho advanced medical laboratory, Addis Ababa, Ethiopia. J. Trop. Med. 30, 2020 (2020).
Asres, G. S., Legese, M. H. & Woldeargay, G. M. Prevalence of multidrug-resistant bacteria in postoperative wound infections at tikur anbessa specialized hospital, Addis Ababa, Ethiopia. Arch. Med. 9(4), 12. https://doi.org/10.21767/1989-5216.1000233 (2017).
Azene, M. K. & Beyene, B. A. Bacteriology and antibiogram of pathogens from wound infections at Dessie Laboratory, North-east Ethiopia. Tanzan J. Health Res. 13, 68–77 (2011).
Godebo, G., Kibru, G. & Tassew, H. Multidrug-resistant bacterial isolates in infected wounds at Jimma University specialized hospital, Ethiopia. Ann. Clin. Microbiol. Antimicrob. 12, 17. https://doi.org/10.1186/1476-0711-12-17 (2013).
Acknowledgements
We thank Arsho Advance Medical Laboratories for providing us with laboratory space and facilities for free. The nurses working for the Arsho are acknowledged for their assistance in blood sample collection. We would like to extend our thanks to the laboratory technician for assisting us in culture media and reagent preparation. We are also in debt to patients for their participation in the study.
Funding
The work was not funded by a government or non-government organization.
Author information
Authors and Affiliations
Contributions
A.B., played a substantial contribution to the conception, study design, revision, and critical reviewing of the article. A.A. contributed to the drafting, acquisition of data analysis, and interpretation of data. A.A. also contributed to the processes of drafting, revision, and critical review. All authors unanimously agreed to submit the article to this journal. Gave final approval to the version to be published. Agree to be accountable for all aspects of work. Not applicable as we did not collect images, records, and videos of our patients.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bitew, A., Adane, A. & Abdeta, A. Bacteriological spectrum, extended-spectrum β-lactamase production and antimicrobial resistance pattern among patients with bloodstream infection in Addis Ababa. Sci Rep 13, 2071 (2023). https://doi.org/10.1038/s41598-023-29337-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-29337-x
- Springer Nature Limited