Abstract
Current guidelines recommend treating rheumatoid arthritis (RA) patients to reach low disease activity or remission, however, most biologic-naive RA patients fail to reach treatment targets on their first biologic therapy. Approximately 90% of biologic-naive RA patients receive a tumor necrosis factor alpha inhibitor (anti-TNF) as their first biologic treatment, even though several alternative mechanism of action (MOA) therapies are approved as first-line options. After 3 months of therapy, patients may remain on anti-TNF therapy even if they fail to achieve the treatment target, mainly due to formulary structures. This means patients have to endure a second and even a third ineffective anti-TNF—called anti-TNF cycling—before changing MOA. This significantly delays patients from reaching their treatment targets. All anti-TNF drugs target the same molecular and inflammatory pathways; thus, it is not surprising that most patients who are primary non-responders to their initial anti-TNF therapy fail to achieve their treatment targets when cycled through alternative anti-TNFs. This suggests that primary non-responders should be switched to an alternative MOA therapy rather than enduring anti-TNF cycling. Avoiding anti-TNF cycling would prevent disease progression and improve quality of life for RA patients who are primary non-responders to anti-TNFs. The development of a personalized medicine approach to identify primary non-responders to anti-TNFs prior to treatment would allow significantly more patients to reach their treatment target by treating them with alternative MOA therapies as first-line therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction: treatment target goals and the definition of response
Rheumatoid arthritis (RA) is a complex, chronic, autoimmune disease that leads to inappropriate inflammation and systemic tissue damage. RA can progress from painful inflammation of the joints to joint stiffness, joint destruction, loss of function, and, eventually, to permanent irreversible disability [1]. As RA progresses, it negatively affects the ability of patients to work and perform activities of daily living and household chores, leading to decreased quality and length of life [2]. The objective of treatment is to slow or even halt disease progression and improve the quality of life for RA patients.
The RA population is very heterogeneous and the development of disease symptoms depends on a variety of genetic (susceptibility genes, epigenetic modifications) and environmental factors (smoking, obesity, changes to the microbiome of the mouth and gut). Together, these factors elicit immune responses, leading to inappropriate and robust immune cell proliferation, differentiation, and autoantibody production, which stimulate and maintain the inflammatory cascade in the synovium [1]. This can occur through multiple molecular pathways that involve signaling through pro-inflammatory cytokines such as tumor necrosis factor alpha (TNF-α) and interleukin-6 (IL-6) [1]. The variety of molecular inflammatory pathways activated in RA patients may determine each individual’s response to treatment, as recently approved therapies for RA treatment are molecularly targeted. The advent of personalized [3] or precision [4] medicine (PM) for RA will make it possible to determine if an individual will respond to a specific targeted treatment, improving a clinician’s ability to “treat-to-target” [5, 6], which is the primary goal of RA therapy. Treat-to-target is the foundation of the American College of Rheumatology (ACR) [7] and the European League Against Rheumatism (EULAR) [8], and their current guidelines for RA treatment define the target as achieving either remission or, if remission is not possible, achieving low disease activity (LDA). Remission is an extremely high bar for therapy targets and is achieved by only a very small proportion of RA patients. In the DREAM registry, 6% of patients achieved remission as defined by ACR and EULAR criteria, whereas 27% achieved Disease Activity Score (DAS28) < 2.6 which is a less stringent measure of remission as it allows for some residual disease activity [9]. Table 1 compares the specific cut-offs in the different disease activity scales for LDA and remission and summarizes these for the ACR and EULAR guidelines. Although it is achieved by only a small proportion of patients, there are substantiated structural and functional benefits to achieving remission compared to LDA [12], including delaying disease progression and improving quality of life. However, LDA remains the most realistic and achievable target for the majority of RA patients.
To follow the treat-to-target recommendations, it is necessary for a rheumatologist to measure the DAS, specify the DAS target to be met, and decide on a period of time to define the response to treatment for each patient. Therefore, standardizing the measurement of disease activity has been key to determining the efficacy of RA drugs and for clinicians to evaluate and follow the effect of treatment on their patients. The most commonly used measures in clinical care (Table 1) are the Clinical Disease Activity Index (CDAI) and DAS28 [7, 8]. For drug development, the ACR20, ACR50, and ACR70 were established as response criteria. The ACR number refers to the percentage of improvement in a standard set of measures (Table 2) [14]. ACR20 is the most widely used measure of response in RA clinical trials and accepted by the Food and Drug Administration (FDA) as the efficacy bar for drug approval [10], despite not being routinely used in the clinic.
Current treatment guidelines [7, 8] for RA (Fig. 1) recommend beginning treatment with a conventional synthetic (cs) disease modifying anti-rheumatic disease (DMARD) monotherapy such as hydroxychloroquine, leflunomide, methotrexate, or sulfasalazine. Methotrexate is the initial DMARD recommended for treating patients with early RA, defined as a disease duration of < 6 months [7]. Patients with early RA or RA flares may be given low-dose glucocorticoids (prednisone or equivalent ≤ 10 mg/day) for short periods (< 3 months) of time along with the csDMARD. If the goal of treatment is not met, the guidelines recommend switching to combination therapy with two or three csDMARDS or targeted therapies (anti-TNFs, non-TNF biologics, or non-biologic Janus kinase (JAK) inhibitors) with methotrexate, if possible [7, 8].
Following these recommendations, Smolen et al. [1] reported that approximately 25% of patients reached remission on initial DMARD monotherapy with methotrexate or glucocorticoids within 6 months and roughly another 25% achieve LDA. Similar results have been reported using either combination csDMARDS and glucocorticoids or anti-TNF therapy plus methotrexate [16]. In a non-inferiority trial for patients with sub-optimal response to methotrexate, likelihood of continuation of therapy after 1 year of follow-up for triple therapy was shown to be significantly more durable than for methotrexate-etanercept [17]. These results illustrate that not all patients require biologic therapy to achieve treatment targets; however, for those failing to reach LDA on csDMARDs and combination therapies, their disease activities were moderate to high. Those who were initiating a biologic therapy in recent pivotal [15, 18,19,20] and real-world [21] trials had a median DAS28 of 5.4 at baseline. To achieve a meaningful response compatible with ACR and EULAR targets, the required decrease in DAS28 would be > 2.2 to reach LDA (DAS < 3.2).
A recent observational study of insurance plan and Medicare data found that anti-TNF drugs were the first-line treatment in 96% of patients who fail methotrexate therapy [22]. In pivotal trials, between 25 and 42% of anti-TNF-treated patients achieved ACR50 (Table 3) [47]. Drug trials typically enroll patients with moderate to severe disease activity and report the percentage of subjects who achieved ACR20, ACR50, or ACR70. In terms of achieving clinically meaningful change in disease activity, it is unlikely that an ACR20 response would be sufficient. Rather, patients realistically need to achieve at least an ACR50 to reach DAS scores compatible with remission, and close to ACR50 to reach LDA. ACR50 is therefore a better indicator of meaningful clinical progress and response than ACR20 and is more relevant to achieving treatment targets [48,49,50]. Patients who do not reach their treatment targets [50] are forced to cycle through multiple anti-TNF drugs while their disease has time to progress. A recent study compares the consistency of Boolean, CDAI, and SDAI regarding their stringency, power, and face value in assessing patients reaching remission. It finds that these three measures are roughly comparable when assessing remission, with Boolean being the most stringent and requiring the largest sample size for statistical power. However, CDAI is the most practical and preferred choice in clinical practice [51].
The goal of this paper is to review current use of anti-TNF drugs and their impact on clinically meaningful responses, discuss alignment with ACR’s treat to target guidelines for RA, and propose a future alternative approach that allows more patients to reach their treatment targets using a PM approach.
Anti-TNF and alternative approved targeted therapies
In the late 1990s, anti-TNF therapies revolutionized RA treatment because significant numbers of patients achieved LDA for the first time. The first anti-TNF biologic to be tested in RA patients was infliximab (Remicade®, Janssen Biotech Inc., Horsham, PA) [11, 52]. Infliximab is a chimeric mouse-human monoclonal antibody that binds to soluble and membrane-bound TNF-α and blocks TNF-α signaling. With infliximab therapy, inflammation was reduced through downregulation of pro-inflammatory cytokines, which resulted in decreased joint destruction [13] and fewer leukocytes in joints [53]. Overall, anti-TNF therapies have been shown to slow the progression of RA [2]. Maini et al. [11] combined infliximab with methotrexate and showed a response to this combination therapy in patients who did not respond well, or at all, to methotrexate monotherapy. This led to the approval of other anti-TNF drugs and small molecules with different molecular structures (Table 4). Other anti-TNF drugs currently available are etanercept (Enbrel®, Amgen, Thousand Oaks, CA) [54], adalimumab (Humira®, Abbott Laboratories, North Chicago, IL) [55], golimumab (Simponi®, Janssen Biotech Inc., Horsham, PA) [56], and certolizumab (Cimzia®, UCB, Inc., Smyrna, GA) [2, 36]. All of these anti-TNF drugs have molecular structures that target and neutralize the same pro-inflammatory cascade. For example, etanercept is an immunoglobulin G (IgG) fusion protein that consists of the extracellular portion of the human TNF receptor 2 (TNFR2) and the Fc portion and binds to TNF-α as a decoy receptor. Adalimumab and golimumab are human monoclonal antibodies that, like infliximab, bind to TNF-α, preventing downstream inflammatory response. Certolizumab is a Fab fragment of an anti-TNF-α monoclonal antibody that binds to soluble and membrane-bound TNF-α. While anti-TNF drugs are highly effective for some (Table 3), the majority of patients do not respond adequately to such therapies and switch to alternative approved targeted therapies (AATTs) to try to achieve their treatment targets.
AATTs are therapies that target specific molecules, other than TNF-α and its receptor, that are involved in the inflammatory cascade. AATTs inhibit pro-inflammatory cytokines such as interleukin-6 (IL-6), interleukin-1 (IL-1), or inhibit specific enzymes such as JAKs. Examples that target IL-6 are tocilizumab (Actemra®, Genentech, Inc., South San Francisco, CA) and sarilumab (Kevzara®, Sanofi-Aventis, Bridgewater, NJ). Abatacept (Orencia®, Bristol-Myers Squibb, Princeton, NJ) [57] inhibits T cell activation, tofacitinib (Xeljanz®, Pfizer, Inc., New York, NY) and baricitinib (Olumiant®, Eli Lilly and Company, Indianapolis, IN) target different JAK family members.
ACR responses to anti-TNF therapies
The ACR20, ACR50, and ACR70 responses of patients with RA treated with anti-TNF drugs were reviewed by Chung et al. [49], and Scott [58] and are summarized in Table 3. Taken together, these data indicate ACR50 is an attainable target for patients with RA and can be maintained for at least 3 years [59]. Unfortunately, only 25–42% of patients reach the treatment target of ACR50 (Table 3). This agrees with the percentage of patients estimated to obtain ACR20, 50 and 70 responses to these drugs at week 24 of treatment: ACR20, 13–46%; ACR50, 11–38%; ACR70, 8–20% [48] (Table 3).
Time to reach adequate response
According to EULAR recommendations [8], the time period to determine a clinical response to treatment is 3 months, after which significant clinical improvement should be measurable (i.e., achieving LDA). Lack of response to treatment at 3 months indicates a low probability of achieving a clinical response after 1 year of the same treatment [25]. Therefore, the 3-month response rate is used as a surrogate marker of long-term outcome [16, 50]. This coincides with both ACR and EULAR guidelines, which recommend evaluating response to treatment at 3 months [7, 8] and to continue treatment for patients who respond to that therapy.
Switching bDMARD due to inefficacy: within and across mechanistic category
A thorough classification of patient populations that do not respond to anti-TNF therapy is important for a better understanding of the disease mechanism and is critical for finding the most efficient therapies for such individuals. Patients who do not respond to anti-TNFs (non-responders) can be classified into two groups of patients: those who are primary non-responders and those who initially respond but then exhibit secondary loss of response. Primary non-responders may or may not show some initial response, but never reach their treatment target with anti-TNFs. If these patients do not respond to one anti-TNF therapy, they are not likely to respond to other anti-TNFs. This is probably because the chronic inflammation caused by their disease is not sufficiently driven by TNF-α-dependent biological processes. In contrast, loss of response occurs in people who respond initially to treatment, but the response diminishes over time and is often due to the development of neutralizing or anti-drug antibodies [1]. After a loss of response to one anti-TNF, switching to another anti-TNF may recover progress to the treatment target in secondary loss of response patients [60]. However, only a small number of primary non-responsive patients who switch to a second anti-TNF achieve a significant clinical response, and the clinical benefit for patients who cycle to a third anti-TNF is negligible [60]. Therefore, there is a clear unmet need for a PM approach to predict response to anti-TNF therapies before treatment initiation so that predicted primary non-responders can be offered AATTs.
New directions for treatment of RA
Currently, there is no way to determine which RA patients will respond to a targeted treatment. In clinical practice, it is common for non-responding patients to cycle among several anti-TNFs prior to switching to a drug with a different mechanism of action (MOA) [61]. There is a clear unmet need for a PM approach to predict response to anti-TNF therapies before treatment initiation to avoid harming patients, especially those who respond partially or not at all to therapy and continue to try various treatments while their disease progresses [4]. Meeting this need would require defining biomarker signals that predict a patient’s response to therapy, so that medical treatment can be customized to each individual patient. This PM approach is currently in use in oncology [4], where the therapies are prescribed to patients with specific genetic markers. There are also a few positive examples of PM approaches in RA where a number of different biomarkers are being utilized or have been explored. These include biomarkers for seropositivity [62], genetic risk loci such as HLA-DBR1, and the group of alleles referred to as shared epitope. In total, genetic approaches to identify biomarkers of response have been taken to address anti-TNF [63] and tocilizumab [64, 65] interventions. Many have attempted to utilize gene expression data to identify biomarkers of biologic therapeutic response [66], but these have been limited in the main by modest sample size. In addition, the production of antibodies against biological agents, such as those to anti-TNFs, have been associated with loss of patient response to treatment [67]. Although disease-gene associations that may potentially lead to a greater understanding of RA have been established, there is yet a lack of a predictive classifier with meaningful clinical utility that can predict treatment response.
To adapt this approach to RA, an individual patient’s molecular signature of gene expression would be predictive of their response to a particular treatment [4]. Such a test to determine if a patient will respond to a particular therapy is currently under development [3].
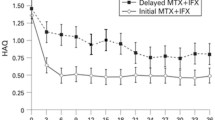
Predicting a patient’s response to anti-TNF drugs is important because roughly 90% of patients with RA receive anti-TNF therapy as the first-line biological DMARD (bDMARD). Detecting patients who will not respond to anti-TNF therapy (primary non-responders) would allow more rapid achievement of treatment targets than current practice because clinicians can treat predicted primary non-responders with an AATT that they are more likely to respond to rather than cycling through the same ineffective MOA. As can be seen in Fig. 2, patients who cycle through anti-TNFs, rather than switching to another MOA, switch classes again much earlier than non-cyclers on AATTs, almost certainly for inefficacy. The data summarized in Table 5 shows that the response rate is higher when switching mechanism of action vs switching within the anti-TNF class.
The cost of anti-TNF cycling
For non-responders, prolonged anti-TNF treatment is costly and unnecessary and may be associated with potentially harmful side effects such as infusion or injection site reactions, infections, tuberculosis, malignancy, lupus-like syndromes, demyelinating syndromes, and/or the appearance of blocking auto-antibodies [1, 3, 26]. Hence, long-term treatment is not recommended for patients who do not respond to therapy [6]. Yet, it is common practice for primary non-responders to anti-TNF drugs to receive multiple anti-TNFs for prolonged periods, often years [61].
A randomized clinical trial compared the efficacy of a non-anti-TNF biologic with a second anti-TNF drug for patients who failed to meet their treatment targets on anti-TNFs [68]. After 24 weeks of treatment, patients who had previously responded insufficiently to an anti-TNF reported a better response on a non-anti-TNF therapy compared to a second anti-TNF (70% vs 52%, achieving a good or moderate EULAR response; 45% vs 28%, achieving low disease activity; 27% vs. 19%, achieving remission) [68]. However, when comparing only those subjects achieving EULAR good responses, the differences were more striking. At both 12 and 24 weeks of treatment, the proportion of EULAR good responders on the non-anti-TNF alternative was almost double than that on a second anti-TNF (after 24 weeks 39% on non-anti-TNF alternatives vs 21% on a second anti-TNF and after 12 weeks 28% on non-anti-TNF alternatives vs 13% on a second anti-TNF). This clinical trial, like others comparing second-line therapy options, could not include a true placebo arm. As a result, the reported response rate is likely an over-estimation of the actual response rate. Other studies [23, 24, 25] reported switching from an anti-TNF medication to the anti-CD20 therapy, rituximab (Rituxan), was associated with better clinical outcomes than switching to another anti-TNF therapy. Furthermore, switching to a treatment with AATT is more effective than cycling to another anti-TNF in patients with an inadequate response to the initial anti-TNF drug [27, 61]. Together, these data demonstrate that switching to AATT therapy after anti-TNF treatment failure improves clinical outcomes for patients with RA [26, 60, 68] and is more efficient in terms of healthcare costs and medication compliance [61] than TNF-cycling. This is supported by ACR and EULAR guidelines, which recommend AATTs as an option to an anti-TNF as a first-line therapy, or as a second-line therapy after one anti-TNF has been tried, instead of switching to a second anti-TNF [61].
Summary and conclusions
ACR50 is a definition of meaningful clinical response in RA sufficient for most patients with moderate to severe disease activity to reach treatment targets. The time to assess whether a patient is responding adequately to a therapy is 3 months. In the pivotal trials that supported anti-TNF therapy approval, 58–73% of patients failed to reach ACR50 (Table 3). Approximately 90% of biologic-naive RA patients with moderate to severe disease activity still receive such therapies as first-line biologic therapy [3].
Cycling patients through multiple anti-TNFs does not appear to significantly improve their clinical response rate and exposes them to disease progression and costly and ineffective treatments with potentially harmful side effects. By switching anti-TNF primary non-responders to an AATT as their first-line therapy, the likelihood of a meaningful response increases (Table 5). A PM test is required to achieve this goal and would allow rheumatologists to start treatment for biologic-naive RA patients with medications more likely to produce a positive clinical response the first time. When this goal is achieved, it will usher in an era of PM for autoimmune diseases such as RA, leading to a significant increase in the number of patients achieving their treatment target on their first targeted therapy. The ultimate goal, however, remains to find a PM test that predicts for all approved therapeutic options and not just for anti-TNFs.
References
Smolen JS, Aletaha D, Barton A, Burmester GR, Emery P, Firestein GS, Kavanaugh A, McInnes IB, Solomon DH, Strand V, Yamamoto K (2018) Rheumatoid arthritis. Nat Rev Dis Primers 4:18001. https://doi.org/10.1038/nrdp.2018.1
Monaco C, Nanchahal J, Taylor P, Feldmann M (2015) Anti-TNF therapy: past, present and future. Int Immunol 27(1):55–62
Johnson K, Weinblatt M (2018) Precision medicine in complex disease: Use of the PrismRA test to stratify patients for response to anti-TNF therapy in rheumatoid arthritis. Precision Medicine. https://www.thejournalofprecisionmedicine.com/wp-content/uploads/2018/11/Johnson-online.pdf.Accessed May 2019
Karsdal MA, Bay-Jensen AC, Henriksen K, Christiansen C, Genant HK, Chamberlain C, Platt A (2014) Rheumatoid arthritis: a case for personalized health care? Arthritis Care Res 66(9):1273–1280
Cardiel MH (2013) Treat to target strategy in rheumatoid arthritis: real benefits. Reumatol Clin 9(2):101–105
Mian AN, Ibrahim F, Scott DL, Galloway J, group Ts (2016) Optimal responses in disease activity scores to treatment in rheumatoid arthritis: Is a DAS28 reduction of >1.2 sufficient? Arthritis Res Ther 18(1):142
Singh JA, Saag KG, Bridges SL Jr, Akl EA, Bannuru RR, Sullivan MC, Vaysbrot E, McNaughton C, Osani M, Shmerling RH, Curtis JR, Furst DE, Parks D, Kavanaugh A, O'Dell J, King C, Leong A, Matteson EL, Schousboe JT, Drevlow B, Ginsberg S, Grober J, St.Clair EW, Tindall E, Miller AS, McAlindon T (2016) 2015 American College of Rheumatology Guideline for the treatment of rheumatoid arthritis. Arthritis Rheum 68(1):1–26
Smolen JS, Landewe R, Breedveld FC, Buch M, Burmester G, Dougados M et al (2014) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 update. Ann Rheum Dis 73(3):492–509
de Punder YM, Fransen J, Kievit W, Houtman PM, Visser H, van de Laar MA et al (2012) The prevalence of clinical remission in RA patients treated with anti-TNF: results from the Dutch Rheumatoid Arthritis Monitoring (DREAM) registry. Rheumatology (Oxford) 51(9):1610–1617
FDA (2013) FDA guidance for industry rheumatoid arthiritis: developing drug products for treatment
Maini RN, Breedveld FC, Kalden JR, Smolen JS, Davis D, Macfarlane JD et al (1998) Therapeutic efficacy of multiple intravenous infusions of anti-tumor necrosis factor alpha monoclonal antibody combined with low-dose weekly methotrexate in rheumatoid arthritis. Arthritis Rheum 41(9):1552–1563
Radner H, Smolen JS, Aletaha D (2014) Remission in rheumatoid arthritis: benefit over low disease activity in patient-reported outcomes and costs. Arthritis Res Ther 16(1):R56
Lipsky PE, van der Heijde DM, St Clair EW, Furst DE, Breedveld FC, Kalden JR, Smolen JS, Weisman M, Emery P, Feldmann M, Harriman GR, Maini RN, Anti-Tumor Necrosis Factor Trial in Rheumatoid Arthritis with Concomitant Therapy Study Group (2000) Infliximab and methotrexate in the treatment of rheumatoid arthritis. Anti-tumor necrosis factor trial in rheumatoid arthritis with concomitant therapy study group. N Engl J Med 343(22):1594–1602
Felson DT, LaValley MP (2014) The ACR20 and defining a threshold for response in rheumatic diseases: too much of a good thing. Arthritis Res Ther 16(1):101
Fleischmann R, Kremer J, Cush J, Schulze-Koops H, Connell CA, Bradley JD, Gruben D, Wallenstein GV, Zwillich SH, Kanik KS, ORAL Solo Investigators (2012) Placebo-controlled trial of tofacitinib monotherapy in rheumatoid arthritis. N Engl J Med 367(6):495–507
Smolen JS, Breedveld FC, Burmester GR, Bykerk V, Dougados M, Emery P, Kvien TK, Navarro-Compán MV, Oliver S, Schoels M, Scholte-Voshaar M, Stamm T, Stoffer M, Takeuchi T, Aletaha D, Andreu JL, Aringer M, Bergman M, Betteridge N, Bijlsma H, Burkhardt H, Cardiel M, Combe B, Durez P, Fonseca JE, Gibofsky A, Gomez-Reino JJ, Graninger W, Hannonen P, Haraoui B, Kouloumas M, Landewe R, Martin-Mola E, Nash P, Ostergaard M, Östör A, Richards P, Sokka-Isler T, Thorne C, Tzioufas AG, van Vollenhoven R, de Wit M, van der Heijde D (2016) Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international task force. Ann Rheum Dis 75(1):3–15
Peper SM, Lew R, Mikuls T, Brophy M, Rybin D, Wu H, O'Dell J (2017) Rheumatoid arthritis treatment after methotrexate: the durability of triple therapy versus etanercept. Arthritis Care Res 69(10):1467–1472
Keystone EC, Kavanaugh AF, Sharp JT, Tannenbaum H, Hua Y, Teoh LS et al (2004) Radiographic, clinical, and functional outcomes of treatment with adalimumab (a human anti-tumor necrosis factor monoclonal antibody) in patients with active rheumatoid arthritis receiving concomitant methotrexate therapy: a randomized, placebo-controlled, 52-week trial. Arthritis Rheum 50(5):1400–1411
van Vollenhoven RF, Fleischmann R, Cohen S, Lee EB, Garcia Meijide JA, Wagner S et al (2012) Tofacitinib or adalimumab versus placebo in rheumatoid arthritis. N Engl J Med 367(6):508–519
Genovese MC, Kremer J, Zamani O, Ludivico C, Krogulec M, Xie L, Beattie SD, Koch AE, Cardillo TE, Rooney TP, Macias WL, de Bono S, Schlichting DE, Smolen JS (2016) Baricitinib in patients with refractory rheumatoid arthritis. N Engl J Med 374(13):1243–1252
Pappas DA, Kremer JM, Reed G, Greenberg JD, Curtis JR (2014) Design characteristics of the CORRONA CERTAIN study: a comparative effectiveness study of biologic agents for rheumatoid arthritis patients. BMC Musculoskelet Disord 15:113
Jin Y, Desai RJ, Liu J, Choi NK, Kim SC (2017) Factors associated with initial or subsequent choice of biologic disease-modifying antirheumatic drugs for treatment of rheumatoid arthritis. Arthritis Res Ther 19(1):159
Gomez-Reino JJ, Maneiro JR, Ruiz J, Rosello R, Sanmarti R, Romero AB et al (2012) Comparative effectiveness of switching to alternative tumour necrosis factor (TNF) antagonists versus switching to rituximab in patients with rheumatoid arthritis who failed previous TNF antagonists: the MIRAR study. Ann Rheum Dis 71(11):1861–1864
Soliman MM, Hyrich KL, Lunt M, Watson KD, Symmons DP, Ashcroft DM, British Society for Rheumatology Biologics Register (2012) Rituximab or a second anti-tumor necrosis factor therapy for rheumatoid arthritis patients who have failed their first anti-tumor necrosis factor therapy? Comparative analysis from the British Society for Rheumatology biologics register. Arthritis Care Res 64(8):1108–1115
van der Heijde D, Keystone EC, Curtis JR, Landewe RB, Schiff MH, Khanna D et al (2012) Timing and magnitude of initial change in disease activity score 28 predicts the likelihood of achieving low disease activity at 1 year in rheumatoid arthritis patients treated with certolizumab pegol: a post-hoc analysis of the RAPID 1 trial. J Rheumatol 39(7):1326–1333
Emery P, Gottenberg JE, Rubbert-Roth A, Sarzi-Puttini P, Choquette D, Taboada VM et al (2015) Rituximab versus an alternative TNF inhibitor in patients with rheumatoid arthritis who failed to respond to a single previous TNF inhibitor: SWITCH-RA, a global, observational, comparative effectiveness study. Ann Rheum Dis 74(6):979–984
Kim HL, Lee MY, Park SY, Park SK, Byun JH, Kwon S, Lee EK (2014) Comparative effectiveness of cycling of tumor necrosis factor-alpha (TNF-alpha) inhibitors versus switching to non-TNF biologics in rheumatoid arthritis patients with inadequate response to TNF-alpha inhibitor using a Bayesian approach. Arch Pharm Res 37(5):662–670
Gomez-Reino JJ, Maneiro JR, Ruiz J, Rosello R, Sanmarti R, Romero AB, Group MS (2012) Comparative effectiveness of switching to alternative tumour necrosis factor (TNF) antagonists versus switching to rituximab in patients with rheumatoid arthritis who failed previous TNF antagonists: the MIRAR Study. Ann Rheum Dis 71(11):1861–1864. https://doi.org/10.1136/annrheumdis-2012-201324
Kim HL, Lee MY, Park SY, Park SK, Byun JH, Kwon S, Lee EK (2014) Comparative effectiveness of cycling of tumor necrosis factor-alpha (TNFalpha) inhibitors versus switching to non-TNF biologics in rheumatoid arthritis patients with inadequate response to TNF-alpha inhibitor using a Bayesian approach. Arch Pharm Res 37(5):662–670. https://doi.org/10.1007/s12272-014-0337-1
Inoue E, Yamanaka H, Hara M, Tomatsu T, Kamatani N (2007) Comparison of Disease Activity Score (DAS)28- erythrocyte sedimentation rate and DAS28- C-reactive protein threshold values. Ann Rheum Dis 66(3):407–409. https://doi.org/10.1136/ard.2006.054205
Fleischmann RM, van der Heijde D, Gardiner PV, Szumski A, Marshall L, Bananis E (2017) DAS28-CRP and DAS28-ESR cut-offs for high disease activity in rheumatoid arthritis are not interchangeable. RMD Open 3(1):e000382. https://doi.org/10.1136/rmdopen-2016-000382
Singh JA, Noorbaloochi S, Singh G (2010) Golimumab for rheumatoid arthritis: a systematic review. J Rheumatol 37(6):1096–1104. https://doi.org/10.3899/jrheum.091466
Emery P, Fleischmann RM, Moreland LW, Hsia EC, Strusberg I, Durez P, Nash P, Amante EJ, Churchill M, Park W, Pons-Estel BA, Doyle MK, Visvanathan S, Xu W, Rahman MU (2009) Golimumab, a human anti-tumor necrosis factor alpha monoclonal antibody, injected subcutaneously every four weeks in methotrexate-naive patients with active rheumatoid arthritis: twenty-four-week results of a phase III, multicenter, randomized, double-blind, placebo-controlled study of golimumab before methotrexate as first-line therapy for early-onset rheumatoid arthritis. Arthritis Rheum 60(8):2272–2283. https://doi.org/10.1002/art.24638
Smolen JS, Kay J, Doyle MK, Landewe R, Matteson EL, Wollenhaupt J, Gaylis N, Murphy FT, Neal JS, Zhou Y, Visvanathan S, Hsia EC, Rahman MU, investigators G-As (2009) Golimumab in patients with active rheumatoid arthritis after treatment with tumour necrosis factor alpha inhibitors (GOAFTER study): a multicentre, randomised, double-blind, placebo-controlled, phase III trial. Lancet 374(9685):210–221. https://doi.org/10.1016/S0140-6736(09)60506-7
Keystone EC, Genovese MC, Klareskog L, Hsia EC, Hall ST, Miranda PC, Pazdur J, Bae SC, Palmer W, Zrubek J, Wiekowski M, Visvanathan S, Wu Z, Rahman MU, Study G-F (2009) Golimumab, a human antibody to tumour necrosis factor {alpha} given by monthly subcutaneous injections, in active rheumatoid arthritis despite methotrexate therapy: the GO-FORWARD Study. Ann Rheum Dis 68(6):789–796. https://doi.org/10.1136/ard.2008.099010
Certolizumab (2016) Certolizumab Package Insert
Moreland LW, Alten R, Van den Bosch F, Appelboom T, Leon M, Emery P, Cohen S, Luggen M, Shergy W, Nuamah I, Becker JC (2002) Costimulatory blockade in patients with rheumatoid arthritis: a pilot, dose-finding, double-blind, placebo-controlled clinical trial evaluating CTLA-4Ig and LEA29Y eighty-five days after the first infusion. Arthritis Rheum 46(6):1470–1479. https://doi.org/10.1002/art.10294
Genovese MC, Becker JC, Schiff M, Luggen M, Sherrer Y, Kremer J, Birbara C, Box J, Natarajan K, Nuamah I, Li T, Aranda R, Hagerty DT, Dougados M (2005) Abatacept for rheumatoid arthritis refractory to tumor necrosis factor alpha inhibition. N Engl J Med 353(11):1114–1123. https://doi.org/10.1056/NEJMoa050524
Kremer JM, Genant HK, Moreland LW, Russell AS, Emery P, Abud-Mendoza C, Szechinski J, Li T, Ge Z, Becker JC, Westhovens R (2006) Effects of abatacept in patients with methotrexate-resistant active rheumatoid arthritis: a randomized trial. Ann Intern Med 144(12):865–876
Tocilizumab (2010) Tocilizumab Package Insert.
Singh JA, Beg S, Lopez-Olivo MA (2011) Tocilizumab for rheumatoid arthritis: a Cochrane systematic review. J Rheumatol 38(1):10–20. https://doi.org/10.3899/jrheum.100717
Maini RN, Taylor PC, Szechinski J, Pavelka K, Broll J, Balint G, Emery P, Raemen F, Petersen J, Smolen J, Thomson D, Kishimoto T, Group CS (2006) Double-blind randomized controlled clinical trial of the interleukin-6 receptor antagonist, tocilizumab, in European patients with rheumatoid arthritis who had an incomplete response to methotrexate. Arthritis Rheum 54(9):2817–2829. https://doi.org/10.1002/art.22033
Emery P, Keystone E, Tony HP, Cantagrel A, van Vollenhoven R, Sanchez A, Alecock E, Lee J, Kremer J (2008) IL-6 receptor inhibition with tocilizumab improves treatment outcomes in patients with rheumatoid arthritis refractory to anti-tumour necrosis factor biologicals: results from a 24-week multicentre randomised placebo-controlled trial. Ann Rheum Dis 67(11):1516–1523. https://doi.org/10.1136/ard.2008.092932
Smolen JS, Beaulieu A, Rubbert-Roth A, Ramos-Remus C, Rovensky J, Alecock E, Woodworth T, Alten R, Investigators O (2008) Effect of interleukin-6 receptor inhibition with tocilizumab in patients with rheumatoid arthritis (OPTION study): a double-blind, placebo-controlled, randomised trial. Lancet 371(9617):987–997. https://doi.org/10.1016/S0140-6736(08)60453-5
Tofacitinib (2018) Tofacitinib Package Insert.
Dhillon S (2017) Tofacitinib: A Review in Rheumatoid Arthritis. Drugs 77(18):1987–2001. https://doi.org/10.1007/s40265-017-0835-9
Curtis JR, Zhang J, Xie F, Beukelman T, Chen L, Fernandes J, Ginsberg S, Spettell C, Yun H, Saag KG, Schiff M (2014) Use of oral and subcutaneous methotrexate in rheumatoid arthritis patients in the United States. Arthritis Care Res 66(11):1604–1611
Lacroix BD, Karlsson MO, Friberg LE (2014) Simultaneous exposure-response modeling of ACR20, ACR50, and ACR70 improvement scores in rheumatoid arthritis patients treated with certolizumab pegol. CPT Pharmacometrics Syst Pharmacol 3:e143
Chung CP, Thompson JL, Koch GG, Amara I, Strand V, Pincus T (2006) Are American College of Rheumatology 50% response criteria superior to 20% criteria in distinguishing active aggressive treatment in rheumatoid arthritis clinical trials reported since 1997? A meta-analysis of discriminant capacities. Ann Rheum Dis 65(12):1602–1607
Fagnani F, Pham T, Claudepierre P, Berenbaum F, De Chalus T, Saadoun C et al (2016) Modeling of the clinical and economic impact of a risk-sharing agreement supporting a treat-to-target strategy in the management of patients with rheumatoid arthritis in France. J Med Econ 19(8):812–821
Mack ME, Hsia E, Aletaha D (2017) Comparative assessment of the different American College of Rheumatology/European League against rheumatism remission definitions for rheumatoid arthritis for their use as clinical trial end points. Arthritis Rheum 69(3):518–528
Infliximab (1998) Infliximab Package Insert
Taylor PC, Peters AM, Paleolog E, Chapman PT, Elliott MJ, McCloskey R, Feldmann M, Maini RN (2000) Reduction of chemokine levels and leukocyte traffic to joints by tumor necrosis factor alpha blockade in patients with rheumatoid arthritis. Arthritis Rheum 43(1):38–47
Enbrel (2011) Enbrel for subcutaneous injection: Etanercept package insert
Adalimumab (2002) Adalimumab Package Insert
Golimumab (2009) Golimumab Package insert
Abatacept (2013) Abatacept Package Insert
Scott DL (2012) Biologics-based therapy for the treatment of rheumatoid arthritis. Clin Pharmacol Ther 91(1):30–43
Kremer JM, Russell AS, Emery P, Abud-Mendoza C, Szechinski J, Westhovens R, Li T, Zhou X, Becker JC, Aranda R, Peterfy C, Genant HK (2011) Long-term safety, efficacy and inhibition of radiographic progression with abatacept treatment in patients with rheumatoid arthritis and an inadequate response to methotrexate: 3-year results from the AIM trial. Ann Rheum Dis 70(10):1826–1830
Wei W, Knapp K, Wang L, Chen CI, Craig GL, Ferguson K, Schwartzman S (2017) Treatment persistence and clinical outcomes of tumor necrosis factor inhibitor cycling or switching to a new mechanism of action therapy: real-world observational study of rheumatoid arthritis patients in the United States with prior tumor necrosis factor inhibitor therapy. Adv Ther 34(8):1936–1952
Chastek B, Chen CI, Proudfoot C, Shinde S, Kuznik A, Wei W (2017) Treatment persistence and healthcare costs among patients with rheumatoid arthritis changing biologics in the USA. Adv Ther 34(11):2422–2435
Isaacs JD, Cohen SB, Emery P, Tak PP, Wang J, Lei G, Williams S, Lal P, Read SJ (2013) Effect of baseline rheumatoid factor and anticitrullinated peptide antibody serotype on rituximab clinical response: a meta-analysis. Ann Rheum Dis 72(3):329–336
Verweij CL (2011) Pharmacogenetics: anti-TNF therapy in RA--towards personalized medicine? Nat Rev Rheumatol 7(3):136–138
Wang J, Platt A, Upmanyu R, Germer S, Lei G, Rabe C, Benayed R, Kenwright A, Hemmings A, Martin M, Harari O (2013) IL-6 pathway-driven investigation of response to IL-6 receptor inhibition in rheumatoid arthritis. BMJ Open 3(8):e003199
Wang J, Thingholm LB, Skieceviciene J, Rausch P, Kummen M, Hov JR et al (2016) Genome-wide association analysis identifies variation in vitamin D receptor and other host factors influencing the gut microbiota. Nat Genet 48(11):1396–1406
Smith SL, Plant D, Eyre S, Barton A (2013) The potential use of expression profiling: implications for predicting treatment response in rheumatoid arthritis. Ann Rheum Dis 72(7):1118–1124
Atzeni F, Talotta R, Salaffi F, Cassinotti A, Varisco V, Battellino M, Ardizzone S, Pace F, Sarzi-Puttini P (2013) Immunogenicity and autoimmunity during anti-TNF therapy. Autoimmun Rev 12(7):703–708
Gottenberg JE, Brocq O, Perdriger A, Lassoued S, Berthelot JM, Wendling D, Euller-Ziegler L, Soubrier M, Richez C, Fautrel B, Constantin AL, Mariette X, Morel J, Gilson M, Cormier G, Salmon JH, Rist S, Lioté F, Marotte H, Bonnet C, Marcelli C, Sellam J, Meyer O, Solau-Gervais E, Guis S, Ziza JM, Zarnitsky C, Chary-Valckenaere I, Vittecoq O, Saraux A, Pers YM, Gayraud M, Bolla G, Claudepierre P, Ardizzone M, Dernis E, Breban MA, Fain O, Balblanc JC, Aberkane O, Vazel M, Back C, Candon S, Chatenoud L, Perrodeau E, Sibilia J, Ravaud P (2016) Non-TNF-targeted biologic vs a second anti-TNF drug to treat rheumatoid arthritis in patients with insufficient response to a first anti-TNF drug: a randomized clinical trial. JAMA. 316(11):1172–1180
Acknowledgments
Professional medical writing was provided by Andrea Gwosdow, Ph.D. of Gwosdow Associates Science Consultants, LLC and was funded by Scipher Medicine Corporation.
Funding
This research received no specific grant funding from any agency.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This is a review article for which ethical approval was not required.
Conflict of interest
All authors are full-time employees of Scipher Medicine Corporation.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Johnson, K.J., Sanchez, H.N. & Schoenbrunner, N. Defining response to TNF-inhibitors in rheumatoid arthritis: the negative impact of anti-TNF cycling and the need for a personalized medicine approach to identify primary non-responders. Clin Rheumatol 38, 2967–2976 (2019). https://doi.org/10.1007/s10067-019-04684-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-019-04684-1