Abstract
Purpose
Inguinal hernias are mainly diagnosed clinically, but imaging can aid in equivocal cases or for treatment planning. The purpose of this study was to evaluate the diagnostic performance of CT with Valsalva maneuver for the diagnosis and characterization of inguinal hernias.
Methods
This single-center retrospective study reviewed all consecutive Valsalva-CT studies between 2018 and 2019. A composite clinical reference standard including surgery was used. Three blinded, independent readers (readers 1–3) reviewed the CT images and scored the presence and type of inguinal hernia. A fourth reader measured hernia size. Interreader agreement was quantified with Krippendorff’s α coefficients. Sensitivity, specificity, and accuracy of Valsalva-CT for the detection of inguinal hernias was computed for each reader.
Results
The final study population included 351 patients (99 women) with median age 52.2 years (interquartile range (IQR), 47.2, 68.9). A total of 381 inguinal hernias were present in 221 patients. Sensitivity, specificity, and accuracy were 85.8%, 98.1%, and 91.5% for reader 1, 72.7%, 92.5%, and 81.8% for reader 2, and 68.2%, 96.3%, and 81.1% for reader 3. Hernia neck size was significantly larger in cases correctly detected by all three readers (19.0 mm, IQR 13, 25), compared to those missed by all readers (7.0 mm, IQR, 5, 9; p < 0.001). Interreader agreement was substantial (α = 0.723) for the diagnosis of hernia and moderate (α = 0.522) for the type of hernia.
Conclusion
Valsalva-CT shows very high specificity and high accuracy for the diagnosis of inguinal hernia. Sensitivity is only moderate which is associated with missed smaller hernias.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernias are the most common form of hernias where a defect of the abdominal wall leads to protrusion of the parietal peritoneum with or without abdominal contents at the level of the groin [1]. The lifetime risk of developing inguinal hernia is estimated to be 27–43% in men and 3–6% in women with increasing incidence at advanced age and with higher body mass index [1,2,3]. Inguinal hernias can be complicated by incarceration or strangulation [4]. Surgical repair is the treatment of choice for symptomatic disease.
According to current guidelines, clinical assessment remains the mainstay for diagnosing inguinal hernia, and imaging is seldom warranted [5, 6]. Nonetheless, imaging can assist in diagnosing clinically occult cases and for surgical planning [7, 8]. Furthermore, differentiating hernia types and confirming bilateral hernias through clinical examination is challenging, but important for planning treatment [9, 10].
Ultrasound (US) with dynamic maneuvers (e.g., Valsalva maneuver) is most often used for the assessment of inguinal hernia [11,12,13]. Valsalva maneuver increases hernia conspicuity as the hernia sac protrudes more under increased abdominal pressure. Drawbacks of US are its operator-dependence and limitations related to patient size. Moreover, interpretation of US images for treatment planning purposes can be challenging for the surgeon [14, 15].
Magnetic resonance imaging (MRI) is less examiner-dependent and images are easier to interpret for non-radiologists given the possibility of multiplanar views [16]. However, MRI has some contraindications (claustrophobia, non-compatible devices) and may not be readily available at every institution.
The literature about the accuracy of computed tomography (CT) imaging for the diagnosis of inguinal hernia is scarce. One study evaluated CT under Valsalva maneuver (Valsalva-CT) for the diagnosis of abdominal wall hernias [17]. However, only five inguinal hernias were included and there was no reference standard to verify findings. Others investigated the diagnostic performance of CT in prone positioning for the diagnosis of inguinal hernias and found higher accuracy of prone compared to supine CT (98.1 vs. 72.8%) [18, 19]. However, prone positioning may not be feasible for all patients and may mask the presence of other concurrent abdominal wall hernias.
We are routinely using a dedicated protocol consisting of a non-contrast CT of the abdomen/pelvis in supine position acquired during a Valsalva maneuver in patients with suspected inguinal hernia to screen for additional unsuspected occult hernias and other abdominal wall hernias as these could influence treatment planning. The primary objective of this study was to evaluate the diagnostic performance of Valsalva-CT for the diagnosis and characterization of inguinal hernias. Secondary objectives were to assess interreader agreement and to investigate influencing factors on the diagnostic performance of the modality.
Materials and methods
The institutional review board and local ethics committee approved this retrospective study (BASEC-Nr: 2021-02464). Patients were included if they had signed a written general informed consent form for the anonymized use of their data for research.
Patient population
The departmental radiology information system (RIS) was searched for all consecutive patients who had undergone a Valsalva-CT for the evaluation of abdominal wall hernias between January 2018 and December 2019. Exclusion criteria were: no signed general informed consent for research-related use of anonymized patient data, duplicates (only the initial CT was included if the same patient had more than one CT within the study period), CT images missing or degraded by image artifacts, CT performed for the evaluation of other hernia types (i.e., Bochdalek hernia), early postoperative CT, no adequate reference standard, and inconclusive surgical report (e.g., if there was no clear description of the hernia type) (Fig. 1). Demographic and clinical data were retrieved from the electronic medical records.
Reference standard
All patients were assessed clinically by abdominal surgeons from our institution. Inguinal hernias were either diagnosed clinically by physical exam or a high suspicion was raised based on clinical findings. The indication for Valsalva-CT was to screen for the presence of abdominal wall hernias. A composite clinical reference standard was used. In those patients who had undergone surgery, the intraoperative findings were used as a reference standard. In the others, a combination of clinical examination findings according to current guidelines [5, 20], another imaging modality (either US or MRI), and clinical follow-up of at least 2 years was used as a reference standard. Abdominal surgeons from our hospital performed all surgical hernia repairs. Procedures included laparoscopic or open techniques. Details about intraoperative findings including the type of hernia (direct, indirect, combined) were retrieved from the surgical reports.
CT imaging
All patients were scanned on a dual-source or single-source CT scanner (SOMATOM Force, SOMATOM Definition Edge, Siemens Healthineers, Forchheim, Germany). Protocol details are outlined in Supplemental Table 1. All patients received one non-contrast CT of the abdomen and pelvis in supine position and images were acquired during a maximum Valsalva maneuver. Additional images without Valsalva maneuver are not obtained in our clinical practice due to lack of added benefit [17] and considerations related to radiation exposure. Prior to obtaining the CT scan, all patients were instructed thoroughly by the CT technologists on how to perform the Valsalva maneuver correctly and were allowed to practice under guided supervision. For the time of the image acquisition, the patients were asked to bear down as much as they could, “push out their belly”, and hold their breath for as long as they could (Supplemental Figure 1). No oral or rectal contrast was given.
Image analysis
Three board-certified radiologists with 5 (reader 1, D.S.), 8 (reader 2, A.H.), and 4 (reader 3, M.K.) years of experience in abdominal radiology reviewed the images. Reader 1 and reader 2 were radiologists with subspecialization in abdominal imaging. The readers, who were blinded to the reference standard, independently reviewed the CT images and scored for each patient and each side of the groin whether there was an inguinal hernia or not. Any fascial defect or interruption of the abdominal wall in the groin region with or without bulging fat or protrusion of intraabdominal structures was defined as a hernia. If a hernia was scored as present, readers were asked to define the type (indirect, direct, or combined). Indirect hernias originate posterolateral and superior to the course of the inferior epigastric vessels while direct hernias originate anteromedial and inferior to the course of these vessels [5, 21]. Combined hernias were defined as the occurrence of a direct and indirect hernia on the same side of the groin.
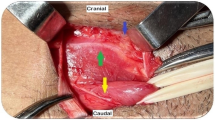
A fourth, unblinded reader (reader 4, S.G.) with 5 years of experience in abdominal imaging measured the hernia size using the electronic caliper tool in the PACS and recorded the hernia contents. Measurements included the size of the hernia neck and the maximum diameter of the hernia sac (Fig. 2).
Statistical analysis
The statistical analysis was performed using R statistical software (version 4.0.2.; R Core Team, R Foundation for Statistical Computing, Vienna, Austria) and SPSS (version 26.0, IBM Corp, Armonk, NY). Clinical data and readout results were evaluated using descriptive statistics. Continuous variables are presented as either mean ± standard deviation or median (interquartile range) and categorical variables as numbers with percentages.
Diagnostic performance (sensitivity, specificity, accuracy) of Valsalva-CT for the detection of inguinal hernias was computed for each reader and for each side of the groin separately as well as for both sides together. For each test characteristic, the 95% confidence interval (CI) was determined by using the standard normal approximation of the binomial distribution table. Performance in classification of hernia type (direct, indirect, or combined) was assessed through calculation of accuracy and balanced accuracy for each reader. Interreader agreement was quantified with Krippendorff’s α coefficients (0.0–0.20 = poor agreement, 0.21–0.40 = fair agreement, 0.41–0.60 = moderate agreement, 0.61–0.80 = substantial agreement, and 0.81–1.00 = almost perfect agreement) [22] and by computing the percentage agreement. Normal distribution of data was tested with the Kolmogorov–Smirnov test. Comparisons between groups were analyzed with the Mann Whitney U test. Two-tailed p-values below 0.05 were considered to infer statistical significance.
Results
Patient population and reference standard
The initial search in the RIS yielded 711 eligible CT scans. Following exclusions were made: no signed general informed consent for research-related use of anonymized patient data (n = 99), duplicates (n = 41), CT images missing or degraded by image artifacts (n = 3), CT performed for the evaluation of other hernia types (n = 34), early postoperative CT (n = 95), no adequate reference standard (n = 70), and inconclusive surgical report (n = 18). After applying exclusion criteria, the final study population included 351 patients (Fig. 1).
A total of 381 inguinal hernias (right side n = 185, left side n = 196) were present in 221 patients (221/351, 63.0%). One hundred thirty patients (130/351, 37%) had no inguinal hernia. Seventy-nine patients (79/351, 22.5%) had a history of prior inguinal hernia repair. Median time in months between CT and surgery (in those patients were operated) was 2 months (1, 4). Main patient and hernia characteristics are outlined in Table 1.
Diagnostic performance of Valsalva-CT for diagnosis of inguinal hernia
Sensitivity of Valsalva-CT for the diagnosis of inguinal hernia was 85.5% for reader 1, 72.7% for reader 2, and 68.2% for reader 3. Specificity was 98.1% for reader 1, 92.5% for reader 2, and 96.3% for reader 3. Accuracy was 91.5% for reader 1, and 81.8% for reader 2, and 81.1% for reader 3. The detailed overall and side-specific results are outlined in Table 2.
Results for the diagnostic performance of Valsalva-CT for detection of bowel- or bladder-containing hernias and for cases with prior inguinal hernia repair are outlined in Supplemental Text 1.
Diagnostic performance of Valsalva-CT for the type of inguinal hernia
The accuracy and balanced accuracy of Valsalva-CT for the classification of hernia type is outlined in Table 3. More details are reported in Supplemental Text 1. Figure 3 shows two examples of combined type inguinal hernias.
Two examples of combined inguinal hernias. Top row A, B shows axial CT images a few slices apart at the level of the groin in a patient with bilateral combined inguinal hernias. The indirect component (arrows in A) arises lateral to the inferior epigastric vessels (arrowhead in A) while the direct component (arrows in B) arises medial to the inferior epigastric vessels (arrowheads in B). This case was correctly classified by all three readers. Bottom row C, D shows axial CT images a few slices apart at the level of the groin in a patient with a right-sided combined inguinal hernia. The larger, indirect component (arrow in C) is seen lateral to the inferior epigastric vessels (arrowhead in C), but there is also a small direct component (arrow in D). This case was misclassified as indirect inguinal hernia by all three readers
Hernia size
The median size of the hernia neck was 19.0 mm (13.0, 25.0) for hernias that were detected by all three readers compared with 10.0 mm (8.0, 15.5) for hernias detected by only two readers. The median size of the hernia neck for cases missed by two readers was 9 mm (6.0, 10.0) compared with 7 mm (5.0, 9.0) for cases missed by all three readers. There were significant differences in neck size between cases which were correctly detected by all readers and those missed by all readers (7.0 mm [5, 9] vs. 19.0 mm [13, 24], p < 0.001) as well as for those cases detected by two readers compared with those missed by two readers [10.0 mm (8.0, 15.5) vs. 9.0 mm (6.0, 10.0), p < 0.001].
The median size of the hernia sac was 47.0 mm (35.0, 62.0 mm) for hernias that were detected by all three readers compared with 32.0 mm (20.0, 50.0 mm) for hernias detected by only two readers. The median size of the hernia sac for cases missed by two readers was 27.0 mm (17.3, 39.8) compared with 15.0 mm (12.0, 20.0) for cases missed by all three readers. There were significant differences in hernia sac size between cases which were correctly detected by all readers and those missed by all [47.0 mm (35.0, 62.0) vs. 15.0 mm (12.0, 20.0), p = 0.004], but not for those cases detected by two readers compared with those missed by two readers [32.0 mm (20.0, 50.0) vs. 27.0 mm (17.3, 39.8), p = 0.054].
The false negative rate in hernias with a neck size of < 10 mm was 33.0% (37/112), 56.3% (63/112), and 66.9% (75/112) for reader 1, reader 2, and reader 3, respectively. The false negative rate in hernias with a neck size of ≥10 mm was 6.0% (16/269), 14.9% (40/269), and 17.1% (46/269) for reader 1, reader 2, and reader 3, respectively. Details about hernia size of combined hernias are shown in Table 1.
Interreader agreement of Valsalva-CT for diagnosis and type of inguinal hernia
Interreader agreement for the presence of inguinal hernia between all three readers was substantial (both sides: α = 0.723, right side: α = 0.721, left side: α = 0.731) with percentage of agreement ranging from 78.8% to 85.5%. Interreader agreement was also substantial when only analyzing hernias containing more than fat (i.e., bowel, bladder) (α = 0.752) with percentage of agreement between readers ranging from 96.2%—99.0%. Interreader agreement for the type of inguinal hernia between all three readers was moderate (α = 0.522) with a percentage of agreement of 64.6%. Detailed results of interreader agreement between single readers for different subcategories are outlined in Supplemental Table 2.
Discussion
In this study we evaluated the diagnostic performance and interreader agreement of Valsalva-CT for the detection and characterization of inguinal hernias. This study showed substantial interreader agreement (α = 0.723), high specificity (92.5–98.1%) and accuracy (81.1–91.5%) of Valsalva-CT. In contrast, sensitivity was only moderate, ranging from 68.2% to 85.8%, which was associated with missed smaller hernias.
A few studies have investigated the role of CT for the diagnosis of inguinal hernia [8, 16,17,18,19, 23,24,25]. However, those studies either included a small number of patients [17, 23], did not investigate the Valsalva maneuver [16, 18, 19], did not have a dedicated read-out of CT images [16], did not clearly describe their reference standard [17], or focused on differentiation between types of groin hernias [24, 25]. In a systematic review, Piga et al. [12] analyzed the existing literature on the diagnostic performance of different imaging modalities for the diagnosis of inguinal hernia. Sensitivity and specificity of CT ranged from 57 to 100% and 83 to 100%, respectively. Only one study was included where Valsalva maneuver was performed in a subset of 8 patients [26].
Jaffe et al. [17] examined CT with and without Valsalva maneuver for identifying abdominal wall hernias and found increased conspicuity of hernias with Valsalva maneuver. Notably, most cases involved abdominal wall hernias other than inguinal hernias. Furthermore, the reference standard is not clear and diagnostic performance metrics were not reported in a consistent manner. We included all surgically proven inguinal hernias, regardless of size, even those incidentally diagnosed during surgery for other hernias. Hence, our cohort also included patients with small inguinal hernias. The threshold for calling a hernia in subtle cases may vary among individual readers, which could account for the lower and more inconsistent sensitivity rates observed. This hypothesis is supported by the observation that the size of the hernia neck and sac were notably smaller in cases overlooked by all three readers, relative to those identified by all three readers.
In our study, the two radiologists who were more experienced and subspecialized in abdominal imaging had a higher accurary than the reader with experience but without subspecialization. These findings are in line with a previous study from Miller et al. [8] where a dedicated second reading of hernia scans by a radiologist led to a significant increase in accuracy compared to the baseline radiology reports (accuracy increased from 35 to 79%). Other studies have shown an increase in perceived report quality and decrease in interpretive discrepancies with subspecialized reporting [27, 28]. Subspecialized reporting can yield significant clinical advantages, particularly in instances involving small and clinically occult hernias.
Accuracy for hernia type characterization was only moderate (66.5%–84.3%). Direct and indirect inguinal hernias were classified more accurately than combined hernias. While 80% of combined hernias were recognized as a hernia, only 24% were accurately identified as a combined type. Combined hernias tend to have one component that is more pronounced than the other, potentially leading to a lower degree of accuracy in their classification [8]. Kamei et al. [18] reported correct classification in 95.8%, but with possible selection bias as only surgery was used as a reference standard and hernia size was not reported. Their data also suggests a higher misclassification rate for combined hernias. Clinically, the type of inguinal hernia may not be as important for treatment planning as the detection of any hernia or the accurate identification of hernia contents, as this may inform treatment urgency, surgical approach, and complexity [29,30,31,32]. In our study, the detection rate of inguinal hernias containing bowel or bladder was high, ranging from 94.3 to 95.2%. Only three cases (2.9%) were overlooked by all three readers.
The recurrence rates following inguinal hernia repair can be as high as 15%, and their diagnosis through clinical examination alone can prove challenging owing to scarring and fibrosis [32, 33]. Detection rates for inguinal hernias were similar between surgery-naïve patients and those with history of inguinal hernia repair in our cohort, indicating that Valsalva-CT can be used as a diagnostic tool in patients with suspected recurrent hernia.
Our study has several limitations. First, it is a single-center retrospective study with data from a tertiary referral center and hence our findings may not be representative of other clinical practices and results should be validated in a prospective multi-center setting. We tried to minimize this bias by including all patients in a consecutive manner. Nevertheless, our study includes to date the largest cohort investigating supine CT with Valsalva maneuver for the detection of inguinal hernias. Second, surgery was performed by different surgeons from our hospital and varying surgical techniques may have introduced heterogeneity. However, as opposed to reoperation rates and outcome, which are established surgeon quality metrics, intraoperative confirmation of an inguinal hernia is less likely to be affected by surgeon-level variation [34]. Furthermore, we used a composite clinical reference standard which entails the risk of over- or underestimation of the diagnostic test accuracy, can introduce verification bias, and affects the translation of our findings into a broader clinical setting. However, in the absence of a perfect reference standard we defined our reference standard based on current clinical practice guidelines for the diagnosis of inguinal hernia [5, 20]. The hernia size and European Hernia Society (EHS) groin hernia classification [5] was not consistently reported in the operative reports. Therefore, we were not able to correlate imaging-based hernia size with objective measurements from surgery in this retrospective study. Last, given the retrospective nature of the study, we were not able to compare the diagnostic accuracy of CT with other imaging modalities like US or MRI.
In conclusion, CT with Valsalva maneuver has a very high specificity and high accuracy for the diagnosis of inguinal hernia and the detection rate for inguinal hernias containing bowel or bladder is high. However, sensitivity is only moderate and affected by hernia size, as very small hernias are more frequently missed.
Data availability
All data supporting the findings of this study are available within the paper and its supplementary material.
Abbreviations
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- IQR:
-
Interquartile range
- MRI:
-
Magnetic resonance imaging
- RIS:
-
Radiology information system
- US:
-
Ultrasound
- Valsalva-CT:
-
Computed tomography with Valsalva maneuver
References
Kingsnorth A, LeBlanc K (2003) Hernias: inguinal and incisional. Lancet 362:1561–1571. https://doi.org/10.1016/s0140-6736(03)14746-0
Rosemar A, Angerås U, Rosengren A (2008) Body mass index and groin hernia: a 34-year follow-up study in Swedish men. Ann Surg 247:1064–1068. https://doi.org/10.1097/SLA.0b013e31816b4399
Jensen KK, Henriksen NA, Jorgensen LN (2017) Inguinal hernia epidemiology. In: Hope WW, Cobb WS, Adrales GL (eds) Textbook of hernia. Springer, Cham, pp 23–27
Murphy KP, O’Connor OJ, Maher MM (2014) Adult abdominal hernias. Am J Roentgenol 202:W506–W511. https://doi.org/10.2214/AJR.13.12071
(2018) International guidelines for groin hernia management. Hernia; 22:1–165. https://doi.org/10.1007/s10029-017-1668-x.
Moreno-Egea A, Girela E, Canteras M, Martinez D, Aguayo JL (2000) Accuracy of clinical diagnosis of inguinal and femoral hernia and its usefulness for indicating laparoscopic surgery. Hernia 4:23–27. https://doi.org/10.1007/BF01230587
Plumb AA, Rajeswaran G, Abbasi MA, Masci L, Warren O, Wilson J (2022) Contemporary imaging of inguinal hernia and pain. Br J Radiol 95:20220163. https://doi.org/10.1259/bjr.20220163
Miller J, Tregarthen A, Saouaf R, Towfigh S (2018) Radiologic reporting and interpretation of occult inguinal hernia. J Am Coll Surg 227:489–495. https://doi.org/10.1016/j.jamcollsurg.2018.08.003
Ralphs DN, Brain AJ, Grundy DJ, Hobsley M (1980) How accurately can direct and indirect inguinal hernias be distinguished? Br Med J 280:1039–1040. https://doi.org/10.1136/bmj.280.6220.1039
Tromp WG, van den Heuvel B, Dwars BJ (2014) A new accurate method of physical examination for differentiation of inguinal hernia types. Surg Endosc 28:1460–1464. https://doi.org/10.1007/s00464-013-3359-8
Kwee RM, Kwee TC (2018) Ultrasonography in diagnosing clinically occult groin hernia: systematic review and meta-analysis. Eur Radiol 28:4550–4560. https://doi.org/10.1007/s00330-018-5489-9
Piga E, Zetner D, Andresen K, Rosenberg J (2020) Imaging modalities for inguinal hernia diagnosis: a systematic review. Hernia 24:917–926. https://doi.org/10.1007/s10029-020-02189-4
Stavros AT, Rapp C (2010) Dynamic ultrasound of hernias of the groin and anterior abdominal wall. Ultrasound Q 26:135–169. https://doi.org/10.1097/RUQ.0b013e3181f0b23f
Olmo JCM, Garc¨ªa-Vallejo L, Gestal JN, Coello PC, Antona FB, Trincado MT, Gonz¨¢lez JS, et al (2015) The usefulness of magnetic resonance imaging in the preoperative study and postoperative control in the laparoscopic treatment of the incisional hernia. Surg Sci 6(8):7. https://doi.org/10.4236/ss.2015.68055.
Claus CMP, Cavalieiri M, Malcher F, Trippia C, Eiras-Araujo AL, Pauli E, Cavazzola LT (2022) DECOMP report: answers surgeons expect from an abdominal wall imaging exam. Rev Col Bras Cir 49:e20223172. https://doi.org/10.1590/0100-6991e-20223172en.
Miller J, Cho J, Michael MJ, Saouaf R, Towfigh S (2014) Role of imaging in the diagnosis of occult hernias. JAMA Surg 149:1077–1080. https://doi.org/10.1001/jamasurg.2014.484
Jaffe TA, O’Connell MJ, Harris JP, Paulson EK, DeLong DM (2005) MDCT of abdominal wall hernias: is there a role for Valsalva’s maneuver? Am J Roentgenol 184:847–851. https://doi.org/10.2214/ajr.184.3.01840847
Kamei N, Otsubo T, Koizumi S, Morimoto T, Nakajima Y (2019) Prone “computed tomography hernia study” for the diagnosis of inguinal hernia. Surg Today 49:936–941. https://doi.org/10.1007/s00595-019-01837-2
Miyaki A, Yamaguchi K, Kishibe S, Ida A, Miyauchi T, Naritaka Y (2017) Diagnosis of inguinal hernia by prone- vs. supine-position computed tomography. Hernia 21:705–713. https://doi.org/10.1007/s10029-017-1640-9
LeBlanc KE, LeBlanc LL, LeBlanc KA (2013) Inguinal hernias: diagnosis and management. Am Fam Phys 87:844–848
Burkhardt JH, Arshanskiy Y, Munson JL, Scholz FJ (2011) Diagnosis of inguinal region hernias with axial CT: the lateral crescent sign and other key findings. Radiographics 31:E1–E12. https://doi.org/10.1148/rg.312105129
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Cherian PT, Parnell AP (2008) The diagnosis and classification of inguinal and femoral hernia on multisection spiral CT. Clin Radiol 63:184–192. https://doi.org/10.1016/j.crad.2007.07.018
Kitami M, Takase K, Tsuboi M, Rikimaru Y, Hakamatsuka T, Yamada T, Takahashi S (2009) Differentiation of femoral and inguinal hernias on the basis of anteroposterior relationship to the inguinal ligament on multidimensional computed tomography. J Comput Assist Tomogr 33:678–681. https://doi.org/10.1097/RCT.0b013e3181977a0a
Suzuki S, Furui S, Okinaga K, Sakamoto T, Murata J, Furukawa A, Ohnaka Y (2007) Differentiation of femoral versus inguinal hernia: CT findings. AJR Am J Roentgenol 189:W78-83. https://doi.org/10.2214/ajr.07.2085
Højer AM, Rygaard H, Jess P (1997) CT in the diagnosis of abdominal wall hernias: a preliminary study. Eur Radiol 7:1416–1418. https://doi.org/10.1007/s003300050309
Lindgren EA, Patel MD, Wu Q, Melikian J, Hara AK (2014) The clinical impact of subspecialized radiologist reinterpretation of abdominal imaging studies, with analysis of the types and relative frequency of interpretation discrepancies. Abdom Imaging 39:1119–1126. https://doi.org/10.1007/s00261-014-0140-y
Zabel A, Leschka S, Fischer T, Wildermuth S, Dietrich T (2021) Effects of changing the reporting system from decentralized/modality-based to centralized/subspecialized radiology on radiologists, radiologic technicians and referring physicians of a multi-center radiology network. J Belg Soc Radiol 105:45. https://doi.org/10.5334/jbsr.2483
Garagliano JM, Jaramillo JD, Kopecky KE, Knowlton LM (2020) Amyand hernia: considerations for operative approach and surgical repair. Trauma Surg Acute Care Open 5:e000466. https://doi.org/10.1136/tsaco-2020-000466
Branchu B, Renard Y, Larre S, Leon P (2018) Diagnosis and treatment of inguinal hernia of the bladder: a systematic review of the past 10 years. Turk J Urol 44:384–388. https://doi.org/10.5152/tud.2018.46417
Köckerling F, Simons MP (2018) Current concepts of inguinal hernia repair. Visc Med 34:145–150. https://doi.org/10.1159/000487278
Simons MP, Smietanski M, Bonjer HJ, Bittner R, Miserez M, Aufenacker TJ, Fitzgibbons RJ et al (2018) International guidelines for groin hernia management. Hernia 22:1–165. https://doi.org/10.1007/s10029-017-1668-x
Gopal SV, Warrier A (2013) Recurrence after groin hernia repair-revisited. Int J Surg 11:374–377. https://doi.org/10.1016/j.ijsu.2013.03.012
Aquina CT, Fleming FJ, Becerra AZ, Xu Z, Hensley BJ, Noyes K, Monson JRT et al (2017) Explaining variation in ventral and inguinal hernia repair outcomes: a population-based analysis. Surgery 162:628–639. https://doi.org/10.1016/j.surg.2017.03.013
Funding
Open access funding provided by University of Zurich. This study was funded by Universität Zürich, Filling the Gap, Soleen Ghafoor.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Soleen Ghafoor, Andrin Tognella, Thomas Sartoretti, Hatem Alkadhi, Daniel Stocker, Andreas M. Hötker, Malwina Kaniewska, and André Euler. The first draft of the manuscript was written by Soleen Ghafoor and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Soleen Ghafoor is supported by a grant from the University of Zurich (“Filling the Gap”). Other than that, all authors declare that they have no financial or non-financial conflicts of interest to declare.
Ethical approval
The Institutional Review Board and Local Ethics Committee approved this retrospective study. Only patients who gave written general informed consents were included. This study, which included human participants, was carried out in accordance with the Helsinki Declaration of 1964 and its subsequent amendments.
Human and animal rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Informed Consent
Only patients who had given written general informed consent for research-related use of their anonymized data were included. Given the retrospective nature of the study, the need for additional written informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10029_2023_2830_MOESM2_ESM.tif
Supplementary file2 Supplemental Fig. 1: Top row shows axial (A) and sagittal (B) image of Valsalva-CT in a 61-year-old male patient. Bottom row shows axial (C) and sagittal (D) images from a CT abdomen study of the same patient without Valsalva maneuver that was done for other reasons one year prior. Note the outward bowing of the abdominal wall (arrows in A and B) due to increased abdominal pressure indicating a successful Valsalva maneuver. (TIF 4480 KB)
10029_2023_2830_MOESM3_ESM.tif
Supplementary file3 Supplemental Fig. 2 : A: 46-year-old male patient with previous bilateral inguinal hernia repair and surgically proven recurrent direct hernia on the right with subtle bulging of the bladder (arrow in A). Note the thin linear structure in the right groin region (arrowhead in A) representing hernia mesh from prior surgery. This subtle recurrent hernia was missed by all three readers. B: 76-year-old male patient with abdominal wall weakness and surgically proven bilateral femoral hernias and combined inguinal hernias. Note small bowel loops protruding into the wide-necked bilateral hernias. All three readers rated this case as negative for inguinal hernia and interpreted images as femoral hernias. C: 68-year-old male patient with history of radical prostatectomy presenting with a large incisional hernia in the lower midline abdominal wall and concurrent direct inguinal hernias (arrows in C) with protruding bowel loops. All three readers read this case as negative for inguinal hernia, probably due to the presence of the large incisional hernia involving the origin of the direct inguinal hernias at the Hesselbach triangle. (TIF 1322 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ghafoor, S., Tognella, A., Stocker, D. et al. Diagnostic performance of CT with Valsalva maneuver for the diagnosis and characterization of inguinal hernias. Hernia 27, 1253–1261 (2023). https://doi.org/10.1007/s10029-023-02830-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-023-02830-y