Abstract
Purpose
The aim of the study was to determine which diagnostic modality [Computerized Tomography (CT), Magnetic Resonance Imaging (MRI), or ultrasound (US)] is more precise in terms of sensitivity and specificity in diagnosing inguinal hernia and sub-type of inguinal hernia (direct or indirect).
Methods
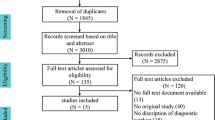
This systematic review was reported according to Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA), and a search for relevant articles was undertaken in PubMed, Embase, and the Cochrane Library. Inclusion criteria were original studies that preoperatively diagnosed patients suspected of inguinal hernia by either CT, MRI, or US and compared diagnostic findings with operative findings or definitive follow-up. The main outcomes were the diagnostic certainty of inguinal hernia and type of hernia by sensitivity and specificity. All eligible studies were searched in the Retraction Watch database to ensure that all included studies were suitable for inclusion.
Results
Bubble charts depicting the size of each patient cohort and percentual range for both sensitivity and specificity showed that US was better than CT and MRI in diagnosing inguinal hernia. Bubble charts for US and CT depicted high values within the studies that reported sensitivity and specificity in diagnosing type of hernia.
Conclusions
We found that US had the highest sensitivity and specificity. However, it must be taken into consideration that performance is highly dependent on the operator’s level of expertise. Based on this systematic review, ultrasound may be the preferred imaging modality when physical examination is inconclusive, given that local expertise in performing US examination for hernia disease is adequate.





Similar content being viewed by others
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
Kingsnorth A (2004) Treating inguinal hernias. BMJ 328(7431):59–60. https://doi.org/10.1136/bmj.328.7431.59
Oberg S, Andresen K, Rosenberg J (2017) Etiology of inguinal hernias: a comprehensive review. Front Surg 4:52. https://doi.org/10.3389/fsurg.2017.00052
Stavros AT, Rapp C (2010) Dynamic ultrasound of hernias of the groin and anterior abdominal wall. Ultrasound Q 26(3):135–169. https://doi.org/10.1097/RUQ.0b013e3181f0b23f
Rosenberg J, Bisgaard T, Kehlet H, Wara P, Asmussen T, Juul P, Strand L, Andersen FH, Bay-Nielsen M, Database DH (2011) Danish Hernia Database recommendations for the management of inguinal and femoral hernia in adults. Dan Med Bull 58(2):C4243
The HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22(1):1–165. https://doi.org/10.1007/s10029-017-1668-x
Brierly RD, Hale PC, Bishop NL (1999) Is herniography an effective and safe investigation? J R Coll Surg Edinb 44(6):374–377
Ng TT, Hamlin JA, Kahn AM (2009) Herniography: analysis of its role and limitations. Hernia 13(1):7–11. https://doi.org/10.1007/s10029-008-0423-8
Gullmo A (1989) Herniography. World J Surg 13(5):560–568. https://doi.org/10.1007/bf01658871
Robinson A, Light D, Kasim A, Nice C (2013) A systematic review and meta-analysis of the role of radiology in the diagnosis of occult inguinal hernia. Surg Endosc 27(1):11–18. https://doi.org/10.1007/s00464-012-2412-3
Ekberg O (1983) Complications after herniography in adults. AJR Am J Roentgenol 140(3):491–495. https://doi.org/10.2214/ajr.140.3.491
Ducharme JC, Guttman FM, Poljicak M (1980) Hematoma of bowel and cellulitis of the abdominal wall complicating herniography. J Pediatr Surg 15(3):318–319. https://doi.org/10.1016/s0022-3468(80)80146-1
Haastrup E, Andresen K, Rosenberg J (2017) Low reoperation rates in young males after sutured repair of indirect inguinal hernia: arguments for a tailored approach. Am J Surg 214(5):844–848. https://doi.org/10.1016/j.amjsurg.2017.02.015
Miller J, Cho J, Michael MJ, Saouaf R, Towfigh S (2014) Role of imaging in the diagnosis of occult hernias. JAMA Surg 149(10):1077–1080. https://doi.org/10.1001/jamasurg.2014.484
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Greenhalgh T, Peacock R (2005) Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ 331(7524):1064–1065. https://doi.org/10.1136/bmj.38636.593461.68
Didier E, Guaspare-Cartron C (2018) The new watchdogs' vision of science: a roundtable with Ivan Oransky (Retraction Watch) and Brandon Stell (PubPeer). Soc Stud Sci 48(1):165–167. https://doi.org/10.1177/0306312718756202
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM, Group Q (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155(8):529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
Deitch EA, Soncrant MC (1981) Ultrasonic diagnosis of surgical disease of the inguinal–femoral region. Surg Gynecol Obstet 152(3):319–322
Alabraba E, Psarelli E, Meakin K, Quinn M, Leung M, Hartley M, Howes N (2014) The role of ultrasound in the management of patients with occult groin hernias. Int J Surg 12(9):918–922. https://doi.org/10.1016/j.ijsu.2014.07.266
Alam A, Nice C, Uberoi R (2005) The accuracy of ultrasound in the diagnosis of clinically occult groin hernias in adults. Eur Radiol 15(12):2457–2461. https://doi.org/10.1007/s00330-005-2825-7
Bradley M, Morgan J, Pentlow B, Roe A (2006) The positive predictive value of diagnostic ultrasound for occult herniae. Ann R Coll Surg Engl 88(2):165–167. https://doi.org/10.1308/003588406X95110
Cummings J, Edwards H (2013) Local investigation of outcomes based on ultrasound examinations for suspected inguinal hernia performed by sonographers and radiologists. Ultrasound 21(1):12–15. https://doi.org/10.1258/ult.2012.012035
Kamei N, Otsubo T, Koizumi S, Morimoto T, Nakajima Y (2019) Prone "computed tomography hernia study" for the diagnosis of inguinal hernia. Surg Today 49(11):936–941. https://doi.org/10.1007/s00595-019-01837-2
Miyaki A, Yamaguchi K, Kishibe S, Ida A, Miyauchi T, Naritaka Y (2017) Diagnosis of inguinal hernia by prone- vs. supine-position computed tomography. Hernia 21(5):705–713. https://doi.org/10.1007/s10029-017-1640-9
Niebuhr H, Konig A, Pawlak M, Sailer M, Kockerling F, Reinpold W (2017) Groin hernia diagnostics: dynamic inguinal ultrasound (DIUS). Langenbecks Arch Surg 402(7):1039–1045. https://doi.org/10.1007/s00423-017-1604-7
Diao X, Chen Y, Qiu Z, Pang Y, Zhan J, Chen L (2014) Diagnostic value of an automated breast volume scanner for abdominal hernias. J Ultrasound Med 33(1):39–46. https://doi.org/10.7863/ultra.33.1.39
Garvey JF (2012) Computed tomography scan diagnosis of occult groin hernia. Hernia 16(3):307–314. https://doi.org/10.1007/s10029-011-0899-5
Djuric-Stefanovic A, Saranovic D, Ivanovic A, Masulovic D, Zuvela M, Bjelovic M, Pesko P (2008) The accuracy of ultrasonography in classification of groin hernias according to the criteria of the unified classification system. Hernia 12(4):395–400. https://doi.org/10.1007/s10029-008-0352-6
Robinson P, Hensor E, Lansdown MJ, Ambrose NS, Chapman AH (2006) Inguinofemoral hernia: accuracy of sonography in patients with indeterminate clinical features. AJR Am J Roentgenol 187(5):1168–1178. https://doi.org/10.2214/AJR.05.1251
Kraft BM, Kolb H, Kuckuk B, Haaga S, Leibl BJ, Kraft K, Bittner R (2003) Diagnosis and classification of inguinal hernias. Surg Endosc 17(12):2021–2024. https://doi.org/10.1007/s00464-002-9283-y
Bradley M, Morgan D, Pentlow B, Roe A (2003) The groin hernia—an ultrasound diagnosis? Ann R Coll Surg Engl 85(3):178–180. https://doi.org/10.1308/003588403321661334
Zhang GQ, Sugiyama M, Hagi H, Urata T, Shimamori N, Atomi Y (2001) Groin hernias in adults: value of color Doppler sonography in their classification. J Clin Ultrasound 29(8):429–434. https://doi.org/10.1002/jcu.10000
van den Berg JC, de Valois JC, Go PM, Rosenbusch G (1999) Detection of groin hernia with physical examination, ultrasound, and MRI compared with laparoscopic findings. Invest Radiol 34(12):739–743. https://doi.org/10.1097/00004424-199912000-00002
Korenkov M, Paul A, Troidl H (1999) Color duplex sonography: diagnostic tool in the differentiation of inguinal hernias. J Ultrasound Med 18(8):565–568. https://doi.org/10.7863/jum.1999.18.8.565
Renzulli P, Frei E, Schafer M, Werlen S, Wegmuller H, Krahenbuhl L (1997) Preoperative Nyhus classification of inguinal hernias and type-related individual hernia repair. A case for diagnostic laparoscopy. Surg Laparosc Endosc 7(5):373–377
van den Berg JC, de Valois JC, Go PM, Rosenbusch G (1997) Dynamic magnetic resonance imaging in the diagnosis of groin hernia. Investig Radiol 32(10):644–647. https://doi.org/10.1097/00004424-199710000-00010
Hojer AM, Rygaard H, Jess P (1997) CT in the diagnosis of abdominal wall hernias: a preliminary study. Eur Radiol 7(9):1416–1418. https://doi.org/10.1007/s003300050309
Palumbo V, Tomasello G, Bruno A, Damiano G, Spinelli G, Sinagra E, Cocchiara G, Buscemi S, Sammartano A, Bonafade E, Ficarella S, Luca S, Carlo G, Blasi M, Sorrentino F, Aiello C, Fazzotta S, Giuseppe B, Ignazio A, Monte L (2014) The value of diagnostic ultrasound for detecting occult inguinal hernia in patients with groin pain. Acta Med Mediterr 30(2):493–496
Miller J, Tregarthen A, Saouaf R, Towfigh S (2018) Radiologic reporting and interpretation of occult inguinal hernia. J Am Coll Surg 227(5):489–495. https://doi.org/10.1016/j.jamcollsurg.2018.08.003
Maisenbacher T, Kratzer W, Formentini A, Schmidberger J, Kaltenbach T, Henne-Bruns D, Graeter T, Hillenbrand A (2018) Value of ultrasonography in the diagnosis of inguinal hernia—a retrospective study. Ultraschall Med 39(6):690–696. https://doi.org/10.1055/a-0637-1526
Vasileff WK, Nekhline M, Kolowich PA, Talpos GB, Eyler WR, van Holsbeeck M (2017) Inguinal hernia in athletes: role of dynamic ultrasound. Sports Health 9(5):414–421. https://doi.org/10.1177/1941738117717009
Lee RK, Griffith JF, Ng WH (2015) High accuracy of ultrasound in diagnosing the presence and type of groin hernia. J Clin Ultrasound 43(9):538–547. https://doi.org/10.1002/jcu.22271
Kim B, Robinson P, Modi H, Gupta H, Horgan K, Achuthan R (2015) Evaluation of the usage and influence of groin ultrasound in primary and secondary healthcare settings. Hernia 19(3):367–371. https://doi.org/10.1007/s10029-014-1212-1
Grant T, Neuschler E, Hartz W 3rd (2011) Groin pain in women: use of sonography to detect occult hernias. J Ultrasound Med 30(12):1701–1707. https://doi.org/10.7863/jum.2011.30.12.1701
Light D, Ratnasingham K, Banerjee A, Cadwallader R, Uzzaman MM, Gopinath B (2011) The role of ultrasound scan in the diagnosis of occult inguinal hernias. Int J Surg 9(2):169–172. https://doi.org/10.1016/j.ijsu.2010.10.014
Cherian PT, Parnell AP (2008) The diagnosis and classification of inguinal and femoral hernia on multisection spiral CT. Clin Radiol 63(2):184–192. https://doi.org/10.1016/j.crad.2007.07.018
Suzuki S, Furui S, Okinaga K, Sakamoto T, Murata J, Furukawa A, Ohnaka Y (2007) Differentiation of femoral versus inguinal hernia: CT findings. AJR Am J Roentgenol 189(2):W78–W83. https://doi.org/10.2214/AJR.07.2085
Hasbahceci M, Erol C (2015) Usefulness of computed tomography for differentiation of primary inguinal hernia. Gazi Med J 26(4):170–173. https://doi.org/10.12996/gmj.2015.50
Barnett ML, Boddupalli D, Nundy S, Bates DW (2019) Comparative accuracy of diagnosis by collective intelligence of multiple physicians vs individual physicians. JAMA Netw Open 2(3):e190096. https://doi.org/10.1001/jamanetworkopen.2019.0096
Funding
This review received no external funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the idea and design of the study. EP performed the literature search. DZ and EP conducted eligibility screening and EP drafted the manuscript. DZ, KA, and JR critically revised the work. All authors read and gave final approval of the manuscript to be published and agreed to be accountable for the content of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflicts of interest.
Ethics approval
Not applicable.
Informed consent
Consent to participate: not applicable. Consent for publication: not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Piga, E., Zetner, D., Andresen, K. et al. Imaging modalities for inguinal hernia diagnosis: a systematic review. Hernia 24, 917–926 (2020). https://doi.org/10.1007/s10029-020-02189-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-020-02189-4