Abstract
Purpose Ingrowth of fibroblasts in a polypropylene mesh may cause contraction and a later recurrence. We assessed mesh contraction in intraabdominal and retromuscular implantation after incisional hernia repair.
Methods
A cohort of patients within an RCT on laparoscopic (LHR) versus open hernia repair (OHR) had their mesh borders marked with metal clips. X-ray was performed on postoperative day 1 and after 1 year. Total length, width, and dislocation were measured. A tacker fixated large-pore polypropylene mesh was used in LHR, and a retromuscular small-pore heavy-weight mesh was sutured to the midline in OHR. Patient’s pain was assessed before surgery and after 1 year.
Results
For analysis 37/47 patients remained: 20 LHR and 17 OHR. Hernia defect area was median 41 cm2 in LHR and 25 cm2 in OHR (p < 0.140). Implanted mesh size was 300 cm2 for LHR and 240 cm2 for OHR (p < 0.341). After 1 year the mesh area decreased by 4.4% and 0.5% in LHR and OHR, respectively (p < 0.063). Longitudinal distance decreased by 2.8% in LHR and by 2.6% in OHR (p < 0.269). Transverse distance decreased by 1.6% in LHR but increased by 3.1% in OHR (p < 0.005). Dislocation was seen in four LHR and one OHR. Two recurrent and one port-site hernia were diagnosed after LHR. Measurements between observers were identical in 58% and consensus was made in the remainder. Pain was not correlated to mesh area change.
Conclusions
Mesh contraction after 1 year is not a clinical issue for an intraperitoneal large-pore mesh or a retromuscular small-pore mesh. It is not correlated to postoperative pain.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
The use of mesh in incisional hernia repair reduces recurrent hernia formation [1]. Success depends on the ingrowth of the mesh to the abdominal wall, as well as adequate fixation. Mesh size and overlap of the hernia defect are also important factors. Recurrences occur outside the mesh area or if the mesh is displaced from its intended place.
Early meshes were manufactured with thicker fibers and small pores. However, tissue responses to these early meshes could generate a fibrous plate, encapsulating the mesh and causing symptoms for the patient. A stiff abdominal wall and a foreign body sensation have been described with such early meshes. Animal studies have shown that the fibroblast ingrowth of the mesh can cause 20–25% contraction of the mesh size [2,3,4,5,6] and that a small-pore (<0.8 mm) mesh is more prone to contraction than larger pore meshes [7]. However, few studies have verified these findings in humans.
The meshes are stronger than the abdominal wall tissues [8]. Thus, dislocation as a result of contraction or insufficient fixation can expose the abdominal wall defect and cause a recurrence. Increasing the mesh size for a larger overlap to compensate for contraction has been recommended [2].
Severe complications (e.g., chronic infection) have often been the indication for mesh explantation [9], which may give a biased view of the problem of contraction. An enhanced immunological response to the mesh material might also induce contraction, as described in in vitro work by Schachtrupp et al. [10].
The location of the implanted mesh may also play a role; retromuscular, extraperitoneal and intraperitoneal locations may induce different responses and behaviors of meshes. A retromuscular-placed mesh has muscle on one side and fibrous sheet on the other side, thus forming an envelope. This gives little space for mesh dislocation or folding, as well as a good environment for ingrowth that is further facilitated by the elevated intraabdominal pressure.
The extraperitoneal space between muscle and peritoneum provides similar conditions for ingrowth of the mesh, but with potentially more space for mesh folding, due to less support from the peritoneum compared to the fascia. The intraperitoneal location is less favorable. The peritoneal surface is glossy and unfavorable for mesh ingrowth. The peritoneum is loosely attached to the underlying rectus sheet or to the muscles in the area below the umbilicus and at the falciform ligament, making the mesh more susceptible to dislocation.
Fixation of the mesh in the abdominal cavity is a prerequisite for success. It is especially problematic in areas having only peritoneal coverage behind the muscles, where fixation techniques may fail. Fixation is a technical challenge in all locations of the abdominal cavity, with potential for long-lasting pain, or mesh dislocations with an associated risk of recurrence [11].
This study aims to assess mesh size changes and dislocation in the intraabdominal and retromuscular positions in incisional hernia repair in a clinical context, and to review the literature on in vivo clinical studies in humans.
Methods
The patients included in the study are a subgroup of the PROLOVE trial [12, 13] treated at a single center. The PROLOVE trial is a randomized controlled multicenter trial comparing laparoscopic hernia repair (LHR) to open hernia repair (OHR) for midline incisional hernias with a width of less than 10 cm. The primary endpoint was postoperative pain at 3 weeks after surgery. Highly standardized procedures were used, with a standard heavy-weight mesh (ProLite™, Atrium) in the open repair and a large-pore coated mesh (Proceed™, Ethicon Surgery) intra-abdominally placed with laparoscopic technique.
Metal clip markers were placed at the cephalic, caudal, and lateral borders of the mesh in the OHR patients. Laparoscopically implanted meshes were fixed with metal tackers with a double-crown technique (one row of tackers at the rim of the mesh with an intention of 15 mm spacing, and a second row around the unclosed hernia defect). No other fixation method was used. The hernia defect borders were also marked with clips, similar to the OHR mesh directions to facilitate detection of mesh dislocation. In the open repair group, the mesh was placed in the retromuscular space, only sutured to the midline of the closed posterior aponeuroses of the rectus abdominis muscles, without any lateral fixation. All implanted meshes aimed to overlap the hernia defect by at least 5 cm in all directions. Within 2 days, a digital X-ray examination of the abdomen was taken in the supine position, according to the protocol, with a standardized stainless steel washer as a circular marker with a 25 mm diameter and 10 mm central hole for calibration placed on the skin of the abdomen, on the former hernia location. Marker placement and patient position at X-ray was checked for accuracy by comparing marker size to the width of the body of lumbar vertebra 5, or the distance between the sacro-iliacal fissures.
The patients were re-examined after 1 year, when a second abdominal X-ray examination was performed with identical instructions. All images were reviewed in the Sectra Workstation IDS7 image system (Sectra AB, Sweden). The software was calibrated with the markers in the image. Distance and possible dislocation of the mesh markers were assessed and noted in the protocol. The longitudinal and transverse distances between designated mesh markers were recorded independently by an experienced radiologist and two surgeons. When a difference was encountered, the placement of the measuring points was compared and discussed for agreement between observers. The implanted mesh area was calculated as a rectangle (length × width). Dislocation was defined as clearly changed in relation to other markers and anatomic landmarks. Distances were reported as a percentage of the initial measurement. A recurrence seen on X-ray or at clinical examination was noted.
In the PROLOVE trial design, pain was assessed before surgery, daily during 4 weeks or until free of pain, and at the 1-year follow-up. A 100 mm visual analog scale (VAS) was used, with 0 representing “no pain” and 100 “worst pain imaginable”.
Review of the literature
A literature search was performed using PubMed, Web of Science, Google Scholar, and reference lists. The search strategy focused on human in vivo trials and included the keywords “humans AND trial AND hernia AND mesh AND (shrink* OR contract*)”. Publications published before 2000 were excluded, as well as animal studies and case reports on explanted meshes. The last search was performed in September 2016.
Information was retrieved on type of study, hernia and mesh size after implantation, type of fixation, and mesh position. Long-term follow-up included: time for follow-up, how the mesh size was assessed, change in mesh dimensions and area, mesh dislocation, and recurrence. Mesh size was assessed immediately after implantation and at long-time follow-up. If information on mesh area was missing, an estimate from linear scales was used for calculation, assuming equal changes in vertical and transverse directions. Individual mesh area size change was calculated in percent points for a weighted average of studies on both intraperitoneal onlay mesh IPOM and sublay mesh positions. The current study was included in the calculations.
Statistics
All patients in the current RCT were analyzed as intention to treat. Statistical analyses were performed using IBM SPSS Statistics v22 software. Student t tests were used to analyze continuous variables, Mann–Whitney U tests for non-normal distributed variables, and Pearson χ 2 or Fisher exact tests for categorical variables. The correlation is Pearson’s r.
Results
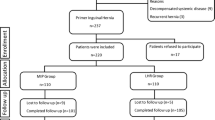
Fifty-two patients were initially included in the study, of which 15 were excluded, giving a total of 37 patients for analysis. The reasons for exclusion were nine lost/incomplete X-ray examinations, two patients with inadequate images not including all markers, two deceased patients, and two lost to follow-up (stroke and undiagnosed abuse).
Twenty patients received LHR and 17 OHR. There were 11 women in each group (p < 0.549). The mean age of the LHR group was 62, standard deviation (SD) 15 years and mean age was 62, SD 10 years for the OHR group (p < 0.968). The body mass index (BMI) was 28.2, SD 3.9 kg/m2, in the LHR and 29.1, SD 4.6 kg/m2, in the OHR group (p < 0.499).
Hernia defects and mesh sizes at implantation and at 1-year follow-up are shown in Table 1. At 1-year follow-up the longitudinal distance between markers decreased by 2.8%, SD 5.2, in the LHR and 2.6%, SD 6.9, in the OHR groups (p < 0.278). The transverse distance decreased by 1.6%, SD 5.4, in the LHR group but increased by 3.1%, SD 4.0, in the OHR group (p < 0.002). Mesh area decreased by 4.4%, SD 6.6, in the LHR group (p < 0.008) but increased by 0.5%, SD 8.9, in the OHR group (p < 0.826). Examples of the measurements on radiographs of both surgical procedures are shown in Figs. 1 and 2.
Abdominal supine examination after open incisional hernia repair. Mesh is placed in the retromuscular plane of the rectus abdominis muscles. Metal clips mark the longitudinal and transverse edges of the mesh and the hernia defect. The marker has a 10-mm hole and a 25 mm diameter. a Postoperative 1 day. b Postoperative 1 year
Dislocation of the mesh markers was noted in four (21%) LHR patients, of whom two had a recurrence. One (6%) OHR patient had a dislocation but no recurrence. No difference was noted in dislocation rate between the groups (p < 0.342). In the LHR group two upper midline recurrent hernias occurred, and one port-site hernia was diagnosed. The mesh area changes of the two recurrent hernias were −13 and −7%.
Pain assessed before and 1 year after surgery is presented in Table 2. There are no differences between LHR and OHR regarding pain and mesh area change. No correlations were found between pain assessments and mesh area change.
Review of the literature
The literature search returned 114 publications. After reviewing the abstracts, six publications remained: three randomized clinical trials [3, 6, 14], one retrospective study [15] and two publications [14, 16] on imaging and measuring implanted meshes in humans (Table 3). Mesh contraction in the IPOM position was addressed in three publications and in the sublay position in one. Two publications on inguinal hernia repairs were identified: one with a mesh in the anterior/interstitial position (Lichtenstein repair) and one with a mesh in the posterior extraperitoneal position (TAPP).
All publications included different meshes with particular textures, porosities, and weights. Three were made of polypropylene [3, 5, 6], one of expanded polytetrafluoroethylene (ePTFE) [15], one of polyvinylidene difluoride (PVDF) [17], and one was a composite mesh of polypropylene and PVDF [14]. IPOMs were fixed using transfascial non-resorbable sutures in combination with permanent [3, 15] or resorbable [14] tackers. The randomized trial on mesh fixation with resorbable versus permanent tackers included 18 patients in each group [3]. In the retrospective study, 17 of 40 patients received non-resorbable tackers.
The size of the meshes was assessed radiologically with either conventional abdominal X-ray examination, computer-assisted tomography (CT), or magnetic resonance imaging (MRI). Preoperative radio-opaque treatment or metal clips on the borders made the mesh position visible on examinations. All except the retrospective study examined the mesh size within 1 week of mesh implantation and at follow-up (3–18 months).
Mesh size change was reported as percent of the size at the first examination. The area of the meshes in the IPOM position varied between −2.5 and −14%, resulting in an overall mean area change of −6.4%, SD 6.4 (decrease), corresponding to a linear change of −3.3%. The area of meshes in the retromuscular position varied between a 12 and 16% increase (mainly due to a transverse increase) resulting in an overall mean area size change of +10%, SD 6.1 (increase), corresponding to a linear change of +5% (Table 4).
Discussion
We assessed the long-term behavior of meshes in the IPOM and retromuscular position. At 1-year follow-up the IPOM meshes had decreased marginally in size for both directions, in contrast to the retromuscular meshes that marginally decreased in the longitudinal, but surprisingly increased in the transverse direction. Alterations in both groups were marginal. The IPOM and retromuscular meshes are not directly comparable, as they are designed with properties specific for their intended position in the abdominal wall. Provided adequate mesh placement, we found that contraction alone cannot account for recurrence.
The difference in length and width of the mesh in this study was around 3% in the laparoscopic position, equal to 0.3 cm per 10 cm. Beldi et al. [3] performed an RCT on laparoscopic hernia repair with a light-weight coated polypropylene mesh, comparing tackers versus combined tackers and transfixation, where mesh shrinkage in relation to pain was studied. Radiological examination after 6 months was compared to immediate postoperative examinations. In their tack fixation group, Beldi et al. found a horizontal size difference of −3.1% and vertical size difference of −2.8%, which is in line with our results. Area size was estimated using a special software tool and resulted in a −2.5% difference (indicating a −1.3% linear change, from Beldi et al., Fig. 3c) in the tack group, a clinically insignificant difference. No mesh displacements were found.
We found no correlation between mesh area change and pain. Postoperative pain has been regarded as a consequence of surgical injury to nerves, fixing techniques, or potential mesh contraction. Permanent transfascial sutures have been associated with chronic pain in 1–11% [3, 11]. Severe pain occurs when sutures include nerves or cause tension at the fixation points in the abdominal wall. However, one cohort trial and one RCT on pain after LHR comparing sutures to tackers did not show any difference between fixation techniques [18, 19]. It is difficult to separate the amount of pain caused by tension or contraction versus fixation in LHR since fixation of the mesh is mandatory. The intention of using resorbable fixation devices in LHR is that pain caused by fixation is to disappear over time, while biointegration will keep the mesh in place.
This study was not designed to detect differences in recurrences. All meshes were to cover the hernia defect and the total incision by at least 5 cm in all directions. We consider the two recurrences that occurred within 12 months in the LHR group as technical failures. Another patient experienced a new port-site hernia, an inherent risk with the laparoscopic technique.
The horizontal width of the mesh increased in the OHR group. It may be an advantage for the OHR-operated patients that the hernia defects were closed, thereby increasing the relative overlap. The “readapted” hernia borders at the midline in OHR stretch the abdominal wall structures caused by the tension of the closing suture. During the postoperative period an adjustment might take place until equilibrium of tension forces is attained in tissue. This may explain the horizontal extension of the mesh in the sublay position after 1 year, even if the mesh properties (heavy-weight with small pores) suggest otherwise. In an RCT, Langer et al. [5] compared a light-weight small-pore mesh to a heavy-weight middle-size pore mesh (both polypropylene) in the sublay position. A small mesh contraction of 8% was found, all in the heavy-weight mesh group. All remaining meshes displayed a horizontal increase in size (but not vertical), in contrast to our study.
Using radio-opaque markers and X-ray examination has weaknesses. The accuracy of the measuring method has not been validated. A protocol for the imaging procedure was pursued, attempting to replicate the setup of the images. Placing the marker on the former midline hernia turned out to be difficult due to the wound dressing in the initial image. An improved, standardized placement of the marker, e.g., at the umbilicus, or at a point triangulated from anatomic landmarks such as the iliac spines and the symphysis, could have optimized the imaging further. The distance between the skin and the position of the mesh is the subcutaneous fat and the muscular wall, usually a few centimeters. There is about 1 m distance between the marker and the X-ray tube, making the projection error between the 25 mm marker and the mesh about 0.25 mm per 1 cm distance (rule of proportions, regula de tribus). No record of BMI at follow-up was recorded, as a major weight change could change the relation between the observed measure of the markers and of the mesh. CT would probably have returned easier measurement points and facilitated complementary data collection, but could hardly justify the increased radiation exposure of the patient.
To our knowledge no standard polypropylene meshes today are visible on a routine X-ray examination without special treatment, which in turn may alter the immunological response and degree of collagen deposition. The use of metal clips can only help in identifying the borders of the mesh. One commercially available polyvinylidene difluoride (PVDF) mesh has added superparamagnetic nanoparticles of ferrofluids to make it visible in MRI exams [17]. This property of a mesh could facilitate studies of mesh contraction, wrinkling, folding or displacement over time.
Successful integration of the mesh requires a flat mesh that adheres to the abdominal wall [16]. This can easily be achieved in the retromuscular position, where the mesh will be kept in place in an envelope of fascia or peritoneum. The intraabdominal wall pressure will also help by giving the mesh good support for ideal ingrowth and to keep the mesh in place. Fixation of the mesh can be reduced and probably even abandoned in the retromuscular space due to the pressure properties. This is a huge advantage in reducing pain compared to the extensive fixation of the mesh needed in the intraabdominal position using IPOM techniques [12].
The majority of studies report on mesh “contraction” in the IPOM position. However, it is unclear whether this is a result of a true contraction due to fibrosis from a host response, or because of partial detachment of the mesh due to poor local conditions for mesh ingrowth and the physiological activity of the abdominal wall resulting in small “wrinkling” of the mesh, which seems to increase the risk for observed “contraction” and makes in vivo mesh measuring prone to errors [17]. When placing a flat mesh using laparoscopic technique, some “planned” wrinkles occur to fit the dome-shaped cavity. The intraabdominal pressure is often lowered during the operation when the mesh is implanted, in an attempt to reduce wrinkles. This would only marginally reduce the problem since the surgeon would still need a proper view for mesh placement. At desufflation even more wrinkles may appear, making perfect ingrowth hard to attain.
The abdominal cavity exhibits a huge variation in conditions for mesh attachment and ingrowth. The abdominal cavity has a well-attached peritoneal coverage over the posterior rectal fascia, excluding the area of the fatty falciform ligament and from the midline below the umbilicus. Peritoneum is more loosely attached to the lateral muscles and very loosely attached below the arcuate line. As a result, the conditions for mesh integration vary widely in different locations. Surgical techniques used for preparation before placing the mesh at laparoscopy vary and are seldom described in details in studies. Most surgeons would advocate covering the mesh with the peritoneum whenever possible. Transfixation sutures through the abdominal wall of the mesh can cause severe pain, at least initially, as well as nerve entrapment [3, 20].
Ingrowth of the mesh, i.e., fibroblast migration and collagen synthesis enclosing the mesh fibers, fixing it to the supporting tissue, is dependent on time and on physical properties of the mesh. Several studies have reported on an active phase with intensive immunological activity lasting 1–4 weeks [5]. After 3–6 months the activity subsides and returns to normal activity, and after 6 months maturation of the scar tissue has been seen [4, 21]. A heavy-weight mesh induces stronger and more long-lasting tissue response with active inflammatory processes even after 1 year [22], but even after 5 years were the processes active in explanted heavy-weight meshes [23]. However, these explants may not be representative as it contained complications of inguinal hernia meshes—recurrence (62%), infection (25%), and chronic pain (13%)—explanted after median 20 (range 4–180) months. The authors concluded that for heavy-weight meshes the biocompatibility increased over time, and that complications were extremely rare 5 years after implantation, the majority occurring within 3 years. With diminishing immunological activity and maturation of the collagen scar, further mesh contraction seems unlikely [24].
There is no standard approach for how to report on mesh contraction. In some reports the linear scale is used and in others a quadratic scale (i.e., the area). A 10% decrease in the linear scale corresponds to a 19% decrease in the quadratic scale (and 20–36%). From a clinical perspective, an area size reduction of 10% would correspond to a linear decrease in about 5–7 mm from the center of a 10-cm mesh. Meticulous placement of a mesh of adequate size will be important. The recommendation of at least a 5-cm overlap of the mesh in the IPOM position [11] might be insufficient to compensate for inadequate placement and fixation. Tacker fixation is recommended to be put in aponeurotic tissue. Transfascial permanent fixation may be more reliable, but has its shortcomings in causing possible chronic pain by nerve entrapment or tension.
In conclusion, long-term mesh size changes are minimal in both retromuscular and IPOM position and should not be regarded as a clinical problem. Pain seems not to be correlated to mesh area change. Adequate mesh overlap, positioning, peritoneal contact, and fixation are all important for the prevention of recurrences, particularly in laparoscopic intraperitoneal mesh placement.
References
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240(4):578–583 (discussion 583–575)
Amid PK (1997) Classification of biomaterials and their related complications in abdominal wall hernia surgery. Hernia 1(1):15–21
Beldi G, Wagner M, Bruegger LE, Kurmann A, Candinas D (2011) Mesh shrinkage and pain in laparoscopic ventral hernia repair: a randomized clinical trial comparing suture versus tack mesh fixation. Surg Endosc 25(3):749–755. doi:10.1007/s00464-010-1246-0
Klinge U, Klosterhalfen B, Muller M, Ottinger AP, Schumpelick V (1998) Shrinking of polypropylene mesh in vivo: an experimental study in dogs. Eur J Surg 164(12):965–969
Langer C, Forster H, Konietschke F, Raab BW, Schaper A, Brunner E, Becker H (2010) [Mesh shrinkage in hernia surgery: data from a prospective randomized double-blinded clinical study.] (Netzschrumpfung in der Hernienchirurgie: Ergebnisse einer klinischen, prospektiv-randomisierten Doppelblindstudie.). Chirurg. doi:10.1007/s00104-009-1853-2
Silvestre AC, de Mathia GB, Fagundes DJ, Medeiros LR, Rosa MI (2011) Shrinkage evaluation of heavyweight and lightweight polypropylene meshes in inguinal hernia repair: a randomized controlled trial. Hernia 15(6):629–634. doi:10.1007/s10029-011-0853-6
Klinge U, Klosterhalfen B, Birkenhauer V, Junge K, Conze J, Schumpelick V (2002) Impact of polymer pore size on the interface scar formation in a rat model. J Surg Res 103(2):208–214. doi:10.1006/jsre.2002.6358
Cobb WS, Kercher KW, Heniford BT (2005) The argument for lightweight polypropylene mesh in hernia repair. Surg Innov 12(1):63–69
Coda A, Bendavid R, Botto-Micca F, Bossotti M, Bona A (2003) Structural alterations of prosthetic meshes in humans. Hernia 7(1):29–34. doi:10.1007/s10029-002-0089-6
Schachtrupp A, Klinge U, Junge K, Rosch R, Bhardwaj RS, Schumpelick V (2003) Individual inflammatory response of human blood monocytes to mesh biomaterials. Br J Surg 90(1):114–120. doi:10.1002/bjs.4023
LeBlanc KA (2007) Laparoscopic incisional hernia repair: are transfascial sutures necessary? A review of the literature. Surg Endosc 21(4):508–513. doi:10.1007/s00464-006-9032-8
Rogmark P, Petersson U, Bringman S, Eklund A, Ezra E, Sevonius D, Smedberg S, Osterberg J, Montgomery A (2013) Short-term outcomes for open and laparoscopic midline incisional hernia repair: a randomized multicenter controlled trial: the PRoLOVE (prospective randomized trial on open versus laparoscopic operation of ventral eventrations) trial. Ann Surg 258(1):37–45. doi:10.1097/SLA.0b013e31828fe1b2
Rogmark P, Petersson U, Bringman S, Ezra E, Osterberg J, Montgomery A (2016) Quality of life and surgical outcome 1 year after open and laparoscopic incisional hernia repair: PROLOVE: a randomized controlled trial. Ann Surg 263(2):244–250. doi:10.1097/SLA.0000000000001305
Kohler G, Pallwein-Prettner L, Koch OO, Luketina RR, Lechner M, Emmanuel K (2015) Magnetic resonance-visible meshes for laparoscopic ventral hernia repair. JSLS 19(1):e2014 00175. doi:10.4293/JSLS.2014.00175
Schoenmaeckers EJ, van der Valk SB, van den Hout HW, Raymakers JF, Rakic S (2009) Computed tomographic measurements of mesh shrinkage after laparoscopic ventral incisional hernia repair with an expanded polytetrafluoroethylene mesh. Surg Endosc 23(7):1620–1623. doi:10.1007/s00464-009-0500-9
Klinge U, Klosterhalfen B (2012) Modified classification of surgical meshes for hernia repair based on the analyses of 1,000 explanted meshes. Hernia 16(3):251–258. doi:10.1007/s10029-012-0913-6
Ciritsis A, Hansen NL, Barabasch A, Kuehnert N, Otto J, Conze J, Klinge U, Kuhl CK, Kraemer NA (2014) Time-dependent changes of magnetic resonance imaging-visible mesh implants in patients. Invest Radiol 49(7):439–444. doi:10.1097/rli.0000000000000051
Bansal VK, Misra MC, Babu D, Singhal P, Rao K, Sagar R, Kumar S, Rajeshwari S, Rewari V (2012) Comparison of long-term outcome and quality of life after laparoscopic repair of incisional and ventral hernias with suture fixation with and without tacks: a prospective, randomized, controlled study. Surg Endosc 26(12):3476–3485. doi:10.1007/s00464-012-2390-5
Nguyen SQ, Divino CM, Buch KE, Schnur J, Weber KJ, Katz LB, Reiner MA, Aldoroty RA, Herron DM (2008) Postoperative pain after laparoscopic ventral hernia repair: a prospective comparison of sutures versus tacks. JSLS 12(2):113–116
Heniford BT, Park A, Ramshaw BJ, Voeller G (2003) Laparoscopic repair of ventral hernias: nine years’ experience with 850 consecutive hernias. Ann Surg 238(3):391–399. doi:10.1097/01.sla.0000086662.49499.ab (discussion 399–400)
Harrell AG, Novitsky YW, Cristiano JA, Gersin KS, Norton HJ, Kercher KW, Heniford BT (2007) Prospective histologic evaluation of intra-abdominal prosthetics four months after implantation in a rabbit model. Surg Endosc. doi:10.1007/s00464-006-9147-y
Novitsky YW, Cristiano JA, Harrell AG, Newcomb W, Norton JH, Kercher KW, Heniford BT (2008) Immunohistochemical analysis of host reaction to heavyweight-, reduced-weight-, and expanded polytetrafluoroethylene (ePTFE)-based meshes after short- and long-term intraabdominal implantations. Surg Endosc 22(4):1070–1076. doi:10.1007/s00464-007-9737-3
Klosterhalfen B, Junge K, Hermanns B, Klinge U (2002) Influence of implantation interval on the long-term biocompatibility of surgical mesh. Br J Surg 89(8):1043–1048. doi:10.1046/j.1365-2168.2002.02149.x
Gonzalez R, Fugate K, McClusky D 3rd, Ritter EM, Lederman A, Dillehay D, Smith CD, Ramshaw BJ (2005) Relationship between tissue ingrowth and mesh contraction. World J Surg 29(8):1038–1043. doi:10.1007/s00268-005-7786-0
Acknowledgements
Sources of unrestricted funding: Lund University, Region Skåne Research & Development Funds, Ethicon, Johnson & Johnson Medical Ltd, The Einar and Inga Nilsson Foundation, The Anna Lisa and Sven-Eric Lundgren Foundation, The Crafoord Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
PR declares no conflict of interest. OE declares no conflict of interest. AM declares no conflict of interest.
Funding
The funders have not taken part in the design, conduction, and evaluation of this trial.
Ethical approval
The trial protocol, part of the PROLOVE trial [11], was approved by the Regional Ethic Review Board in Lund, Sweden (H4710/2004) and the Regional Committee on Radiation Protection (RK 2005:5). The PROLOVE trial was registered at http://www.ClinicalTrials.gov (NCT00472537).
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
All participants signed informed consents when recruited.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Rogmark, P., Ekberg, O. & Montgomery, A. Long-term retromuscular and intraperitoneal mesh size changes within a randomized controlled trial on incisional hernia repair, including a review of the literature. Hernia 21, 687–696 (2017). https://doi.org/10.1007/s10029-017-1624-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-017-1624-9