Abstract
Purpose
To compare a minimally invasive preperitoneal (MIP) single-layer mesh repair with the standard Lichtenstein hernia repair (LHR) for inguinal hernia in terms of operative characteristics, recovery, complications, recurrence and chronic pain.
Method
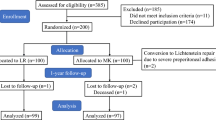
Two hundred and twenty male patients diagnosed with primary inguinal hernia were randomized to either MIP or LHR methods. MIP repair consisted of a single-layer polypropylene mesh developed by our group placed preperitoneally using the Kugel technique. Patients were followed for a minimum of 2 years. Chronic pain was assessed by Sheffield’s pain score.
Results
One hundred and one patients in MIP group and 105 patients in LHR group were included in the analysis. Most patients were diagnosed with indirect hernia (n = 79 for MIP, n = 81 for LHR). Surgery was slightly but significantly shorter for MIP (38.2 ± 7.4 vs. 40.3 ± 6.6, p = 0.031). Early complications such as cord edema, hematoma, scrotal edema, and wound infection were infrequent in both groups. Recurrence was detected in three patients in MIP and one patient in LHR. Chronic pain score was similar with both methods within the first year, but significantly lower for MIP at 24 months (0.66 ± 0.06 vs. 0.87 ± 0.07, p = 0.03).
Conclusion
MIP single-layer mesh repair is as effective and safe as LHR, with the additional benefits of minimally invasive nature, less chronic pain at 2 years and low polypropylene load when compared with the original Kugel patch.




Similar content being viewed by others
References
Rutkow IM (2003) Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am 83:1045–1051 (v–vi)
Amid PK, Shulman AG, Lichtenstein IL (1995) The Lichtenstein open “tension-free” mesh repair of inguinal hernias. Surg Today 25:619–625
Lichtenstein IL (1987) Herniorrhaphy. A personal experience with 6,321 cases. Am J Surg 153:553–559
Bay-Nielsen M, Nilsson E, Nordin P, Kehlet H, Swedish Hernia Data Base the Danish Hernia Data Base (2004) Chronic pain after open mesh and sutured repair of indirect inguinal hernia in young males. Br J Surg 91:1372–1376
Franneby U, Sandblom G, Nordin P, Nyren O, Gunnarsson U (2006) Risk factors for long-term pain after hernia surgery. Ann Surg 244:212–219
Poobalan AS, Bruce J, King PM, Chambers WA, Krukowski ZH, Smith WC (2001) Chronic pain and quality of life following open inguinal hernia repair. Br J Surg 88:1122–1126
Douek M, Smith G, Oshowo A, Stoker DL, Wellwood JM (2003) Prospective randomised controlled trial of laparoscopic versus open inguinal hernia mesh repair: five year follow up. BMJ 326:1012–1013
Grant AM, Scott NW, O’Dwyer PJ, MRC Laparoscopic Groin Hernia Trial Group (2004) Five-year follow-up of a randomized trial to assess pain and numbness after laparoscopic or open repair of groin hernia. Br J Surg 91:1570–1574
McCormack K, Scott NW, Go PM, Ross S, Grant AM, EU Hernia Trialists Collaboration (2003) Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev (1):CD001785
Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R Jr, Dunlop D, Gibbs J, Reda D, Henderson W, Veterans Affairs Cooperative Studies Program 456 Investigators (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350:1819–1827
Kugel RD (1999) Minimally invasive, nonlaparoscopic, preperitoneal, and sutureless, inguinal herniorrhaphy. Am J Surg 178:298–302
Amid PK (2004) Lichtenstein tension-free hernioplasty: its inception, evolution, and principles. Hernia 8(1):1–7
Muldoon RL, Marchant K, Johnson DD, Yoder GG, Read RC, Hauer-Jensen M (2004) Lichtenstein vs anterior preperitoneal prosthetic mesh placement in open inguinal hernia repair: a prospective, randomized trial. Hernia 8:98–103
Rutkow IM, Robbins AW (1998) Classification systems and groin hernias. Surg Clin North Am 78:1117–1127 (viii)
Szopinski J, Dabrowiecki S, Pierscinski S, Jackowski M, Jaworski M, Szuflet Z (2012) Desarda versus Lichtenstein technique for primary inguinal hernia treatment: 3-year results of a randomized clinical trial. World J Surg 36:984–992
Nienhuijs S, Staal E, Keemers-Gels M, Rosman C, Strobbe L (2007) Pain after open preperitoneal repair versus Lichtenstein repair: a randomized trial. World J Surg 31:1751–1759
Berrevoet F, Maes L, Reyntjens K, Rogiers X, Troisi R, de Hemptinne B (2010) Transinguinal preperitoneal memory ring patch versus Lichtenstein repair for unilateral inguinal hernias. Langenbecks Arch Surg 395:557–562
Pelissier EP (2006) Inguinal hernia: preperitoneal placement of a memory-ring patch by anterior approach. Preliminary experience. Hernia 10:248–252
Willaert W, De Bacquer D, Rogiers X, Troisi R, Berrevoet F (2012) Open Preperitoneal Techniques versus Lichtenstein Repair for elective Inguinal Hernias. Cochrane Database Syst Rev 7:CD008034
Li J, Ji Z, Cheng T (2012) Comparison of open preperitoneal and Lichtenstein repair for inguinal hernia repair: a meta-analysis of randomized controlled trials. Am J Surg 204:769–778
Bischoff JM, Aasvang EK, Kehlet H, Werner MU (2012) Does nerve identification during open inguinal herniorrhaphy reduce the risk of nerve damage and persistent pain? Hernia 16:573–577
Simons MP, Aufenacker T, Bay-Nielsen M (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13(4):343–403
Yazdankhah Kenary A1, Afshin SN, Ahmadi Amoli H, Yagoobi Notash A, Borjian A, Yagoobi Notash A Jr, Shafaattalab S, Shafiee G (2013) Randomized clinical trial comparing lightweight mesh with heavyweight mesh for primary inguinal hernia repair. Hernia 17(4):471–477. doi:10.1007/s10029-012-1009
Abbas AE, Abd Ellatif ME, Noaman N, Negm A, El-Morsy G, Amin M, Moatamed A (2012) Patient-perspective quality of life after laparoscopic and open hernia repair: a controlled randomized trial. Surg Endosc 26:2465–2470. doi:10.1007/s00464-012-2212-9
Sadowski B, Rodriguez J, Symmonds R, Roberts J, Song J, Rajab MH, Cummings C, Hodges B, Scott and White Outcomes and Effectiveness Registry Group (2011) Comparison of polypropylene versus polyester mesh in the Lichtenstein hernia repair with respect to chronic pain and discomfort. Hernia 15:643–654
Hakeem A, Shanmugam V (2011) Inguinodynia following Lichtenstein tension-free hernia repair: a review. World J Gastroenterol 17:1791–1796
van der Pool AE, Harlaar JJ, den Hoed PT, Weidema WF, van Veen RN (2010) Long-term follow-up evaluation of chronic pain after endoscopic total extraperitoneal repair of primary and recurrent inguinal hernia. Surg Endosc 24:1707–1711
Kumar S, Wilson RG, Nixon SJ, Macintyre IM (2002) Chronic pain after laparoscopic and open mesh repair of groin hernia. Br J Surg 89:1476–1479
Bay-Nielsen M, Perkins FM, Kehlet H, Danish Hernia Database (2001) Pain and functional impairment 1 year after inguinal herniorrhaphy: a Nationwide Questionnaire Study. Ann Surg 233:1–7
Ceriani V, Faleschini E, Bignami P et al (2005) Kugel hernia repair: open “mini-invasive” technique. Personal experience on 260 patients. Hernia 9:344–347
Schroder DM, Lloyd LR, Boccaccio JE et al (2004) Inguinal hernia recurrence following preperitoneal Kugel patch repair. Am Surg 70:132–136
Baroody M, Bansal B, Maish G (2004) The open preperitoneal approach to recurrent inguinal hernias in high-risk patients. Hernia 8:373–375
Fenoglio ME, Bermas HR, Haun WE et al (2005) Inguinal hernia repair: results using an open preperitoneal approach. Hernia 9:160–161
Reddy KM, Humphreys W, Chew A et al (2005) Inguinal hernia repair with the Kugel patch. ANZ J Surg 75:43–47
Wright D, Paterson C, Scott N et al (2002) Five-year follow-up of patients undergoing laparoscopic or open groin hernia repair: a randomized controlled trial. Ann Surg 235:333–337
Heikknen T, Bringman S, Ohtonen P et al (2004) Five-year outcome of laparoscopic and Lichtenstein hernioplasties. Surg Endosc 18:518–522
Butters M, Redecke J, Koninger J (2007) Long-term results of a randomized clinical trial of Shouldice, Lichtenstein and transabdominal preperitoneal hernia repairs. Br J Surg 94:562–565
Hallen M, Bergenfelz A, Westerdahl J (2008) Laparoscopic extraperitoneal inguinal hernia repair versus open mesh repair: long-term follow-up of a randomized controlled trial. Surgery 143:313–317
Eklund A, Rudberg C, Leijonmarck CE et al (2007) Recurrent inguinal hernia: randomized multicenter trial comparing laparoscopic and Lichtenstein repair. Surg Endosc 21:634–640
Acknowledgments
Thanks to surgical nurses Mrs. Meryem Eren and Mrs. Necla Karademir for their valuable contributions in making mesh.
Conflict of interest
The authors declare that there are no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arslan, K., Erenoglu, B., Turan, E. et al. Minimally invasive preperitoneal single-layer mesh repair versus standard Lichtenstein hernia repair for inguinal hernia: a prospective randomized trial. Hernia 19, 373–381 (2015). https://doi.org/10.1007/s10029-014-1306-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-014-1306-9