Abstract
Objective
Palatal rugae are frequently used in the evaluation of tooth movement after treatment in orthodontics and as a stable region in superimposition. It is important to note that the impression method and material used to record the rugae region affect the accuracy of the impression. The aim of this study is to compare the accuracy of palatal rugae, in three-dimensional (3D) by employing both conventional and digital impression methods.
Materials and methods
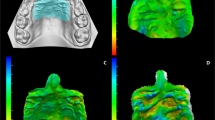
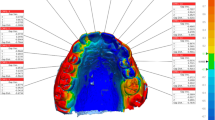
In this study, 22 patients (12 females, 10 males) mean age of 13.5 ± 1.7 years old were selected with complete permanent dentition. Three different impressions were taken from the maxillae of the patients: conventional impression using silicone rubber impression material, conventional impression using alginate impression material, and optical impression using an intraoral scanner. The impressions’ digital data were analyzed by the GOM Inspect (Version 2018, Braunschweig, Germany), a 3D analysis software. The Root Mean Square (RMS) values of the total ruga region were evaluated in this software. The data were statistically analyzed using the Jamovi program. The Kruskal–Wallis test and Mann–Whitney U test were performed due to the non-normal distribution of the data.
Results
There is no statistically significant difference between the comparison points of the right and left rugae’s medial and lateral points and total rugae regions’ RMS values. Although there was no statistically significant difference, the total RMS values of alginate and digital scan measurements showed closer results than the RMS values of silicone and digital scan measurements.
Conclusion
The study found that there was no statistically significant difference in the total RMS values of the ruga region between traditional and digital impression methods.
Clinical relevance
The treatment period in orthodontics is long. Different impression materials and methods can be used for diagnostic, mid-treatment, and final impressions. For superimpositions and treatment and post-treatment palatal ruga evaluations, traditional and digital impression methods are clinically acceptable and can be used as alternatives to each other.




Similar content being viewed by others
Data availability
The full anonymized dataset of the study was opened and available from the corresponding author when it is required.
References
Thomas CJ, Kotze TJ, Van der Merwe CA (1987) An improved statistical method for the racial classification of man by means of palatal rugae. Arch Oral Biol 32(4):315–317. https://doi.org/10.1016/0003-9969(87)90028-8
Jain A, Chowdhary R (2014) Palatal rugae and their role in forensic odontology. J Investig Clin Dent 5:171–178. https://doi.org/10.1111/j.2041-1626.2013.00150.x
Patil MS, Patil SB, Acharya AB (2008) Palatine rugae and their significance in clinical dentistry: a review of the literature. J Am Dent Assoc 139(11):1471–8. https://doi.org/10.14219/jada.archive.2008.0072
Thomas CJ, Van Wyk CW (1988) The palatal rugae in an identification. J Forensic Odontostomatol 6(1):21–27
Bansode SC, Kulkarni MM (2009) Importance of palatal rugae in individual identification. J Forensic Dent Sci 1:77–81. https://doi.org/10.4103/0974-2948.60378
Almeida MA, Phillips C, Kula K et al (1995) Stability of the palatal rugae as landmarks for analysis of dental casts. Angle Orthod 65(1):43–48. https://doi.org/10.1043/0003-3219(1995)065%3c0043:SOTPRA%3e2.0.CO;2
Abdel Aziz HM, Sabet NE (2001) Palatal rugae area: a landmark for analysis of pre-and post-orthodontically treated adult Egyptian patients. EMHJ-East Mediterr Health J 7(1–2):60–66
Abdi AH, Nouri M (2017) Registration of serial maxillary models via the weighted rugae superimposition method. Orthod Craniofac Res 20(2):79–84. https://doi.org/10.1111/ocr.12142
Garib D, Miranda F, Yatabe MS et al (2019) Superimposition of maxillary digital models using the palatal rugae: does ageing affect the reliability? Orthod Craniofac Res 22(3):183–193. https://doi.org/10.1111/ocr.12309
Zhao J, Du S, Liu Y et al (2022) Evaluation of the stability of the palatal rugae using the three-dimensional superimposition technique following orthodontic treatment. J Dent 119:104055. https://doi.org/10.1016/j.jdent.2022.104055
Hourfar J, Kanavakis G, Bister D et al (2015) Three dimensional anatomical exploration of the anterior hard palate at the level of the third ruga for the placement of mini-implants–a cone-beam CT study. Eur J Orthod 37(6):589–595. https://doi.org/10.1093/ejo/cju093
Nucera R, Costa S, Bellocchio AM et al (2022) Evaluation of palatal bone depth, cortical bone, and mucosa thickness for optimal orthodontic miniscrew placement performed according to the third palatal ruga clinical reference. Eur J Orthod 44(5):530–536. https://doi.org/10.1093/ejo/cjac007
Hourfar J, Bister D, Kanavakis G et al (2017) Influence of interradicular and palatal placement of orthodontic mini-implants on the success (survival) rate. Head Face Med 13:1–6. https://doi.org/10.1186/s13005-017-0147-z
Çağlar İ, Yeşil Duymuş Z, Ateş SM (2015) Diş hekimliğinde kullanılan ölçü sistemlerinde güncel yaklaşımlar: dijital ölçü. Atatürk Diş Hek Fak Derg 10: 135–40 https://doi.org/10.17567/dfd.96167
Shah S, Sundaram G, Bartlett D et al (2004) The use of a 3D laser scanner using superimpositional software to assess the accuracy of impression techniques. J Dent 32:653–658. https://doi.org/10.1016/j.jdent.2004.07.005
Chen SY, Liang WM, Chen FN (2004) Factors affecting the accuracy of elastometric impression materials. J Dent 32(8):603–609. https://doi.org/10.1016/j.jdent.2004.04.002
Faria ACL, Rodrigues RCS, Macedo AP et al (2008) Accuracy of stone casts obtained by different impression materials. Braz Oral Res 22:293–298. https://doi.org/10.1590/S1806-83242008000400002
Fatema S, Quader SMS, Shamsuzzaman M et al (2013) A comparative study on accuracy and reproducibility of alginate and addition reaction silicone as an ımpression materials. Update Dent Coll J 3(2):28–33
Howell KJ, McGlumphy EA, Drago C, Knapik G (2013) Comparison of the accuracy of Biomet 3i Encode Robocast Technology and conventional implant impression techniques. Int J Oral Maxillofac Implants 28:228–240. https://doi.org/10.11607/jomi.2546
Palone M, Bellavia M, Floris M, Rombolà A, Cremonini F, Albertini P, Lombardo L (2024) Evaluation of effects of brackets and orthodontic wires on intraoral scans: a prospective in-vivo study. Orthod Craniofac Res 27(1):44–54. https://doi.org/10.1111/ocr.12682
International Organization for Standardization (1994) ISO 5725– 1. Accuracy (trueness and precision) of measurement methods and results - Part 1: General principles and defnitions Geneva: International Organization for Standardization. www.iso.org/obp/ui/#iso:std:iso: 5725:-1:ed-1:v1:en
Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analyses using G* Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41(4):1149–60
Emara A, Sharma N, Halbeisen FS, Msallem B, Thieringer FM (2020) Comparative evaluation of digitization of diagnostic dental cast (plaster) models using different scanning technologies. Dent J 8(3):79
https://www.3shape.com/tr/scanners/trios-3. Accessed 20 January 2024.
Taneva ED, Johnson A, Viana G et al (2015) 3D evaluation of palatal rugae for human identification using digital study models. J Forensic Dent Sci 7(3):244. https://doi.org/10.4103/0975-1475.172451
Choi JW, Ahn JJ, Son K, Huh JB (2019) Three-dimensional evaluation on accuracy of conventional and milled gypsum models and 3D printed photopolymer models. Materials 12(21):3499. https://doi.org/10.3390/ma12213499
Dahlberg G (1940) Statistical methods for medical and biological students. Br Med J 2:358–359
Ender A, Attin T, Mehl A (2016) In vivo precision of conventional and digital methods of obtaining complete-arch dental impressions. J Prosthet Dent 115(3):313–320. https://doi.org/10.1016/j.prosdent.2015.09.011
Ender A, Zimmermann M, Attin T, Mehl A (2016) In vivo precision of conventional and digital methods for obtaining quadrant dental impressions. Clin Oral Invest 20:1495–1504
Nedelcu R, Olsson P, Nyström I, Rydén J, Thor A (2018) Accuracy and precision of 3 intraoral scanners and accuracy of conventional impressions: a novel in vivo analysis method. J Dent 69:110–118. https://doi.org/10.1016/j.jdent.2017.12.006
Quaas S, Rudolph H, Luthardt RG (2007) Direct mechanical data acquisition of dental impressions for the manufacturing of CAD/CAM restorations. J Dent 35:903–908. https://doi.org/10.1016/j.jdent.2007.08.008
da Costa JB, Pelogia F, Hagedorn B, Ferracane JL (2010) Evaluation of different methods of optical impression making on the marginal gap of onlays created with CEREC 3D. Oper Dent 35:324–329. https://doi.org/10.2341/09-178-L
Seelbach P, Brueckel C, Wöstmann B (2013) Accuracy of digital and conventional impression techniques and workflow. Clin Oral Investig 17:1759–1764
Shetty D, Juneja A, Jain A et al (2013) Assessment of palatal rugae pattern and their reproducibility for application in forensic analysis. J Forensic Dent Sci 5(2):106. https://doi.org/10.4103/0975-1475.119775
Hoggan BR, Sadowsky C (2001) The use of palatal rugae for the assessment of anteroposterior tooth movements. Am J Orthod Dentofac Orthop 119(5):482–488. https://doi.org/10.1067/mod.2001.113001
Muthusubramanian M, Limson KS, Julian R (2005) Analysis of rugae in burn victims and cadavers to simulate rugae identification in cases of incineration and decomposition. J Forensic Odontostomatol 23:26–29
Schirmer UR, Wiltshire WA (1997) Manual and computer-aided space analysis: a comparative study. Am J Orthod Dentofacial Orthop 112(6):676–680. https://doi.org/10.1016/S0889-5406(97)70234-8
Groth C, Graham JW, Redmond WR (2014) Three-dimensional printing technology. J Clin Orthod 48(8):475–85
Tomita Y, Uechi J, Konno M (2018) Accuracy of digital models generated by conventional impression/plaster-model methods and intraoral scanning. Dent Mater J 37(4):628–633. https://doi.org/10.4012/dmj.2017-208
Author information
Authors and Affiliations
Contributions
Concept – Ş.G., K.G.T., G.S.D.; Design – Ş.G., K.G.T, G.S.D.; Supervision – S.G; Materials – Ş.G., K.G.T.; Data Collection and/or Processing – Ş.G., K.G.T,; Analysis and/or Interpretation – K.G.T, G.S.D.; Literature Review – Ş.G., K.G.T.; Writing – Ş.G., K.G.T.; Critical Review – K.G.T., Ş.G., G.S.D.,S.G.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The ethical approvals were taken from the University of Health Science Scientific Research Ethics Committee.
Consent to participate
Informed consent was obtained from the parents and/or legal guardians of individuals younger than 18 years of age for participation in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gökmen, Ş., Topsakal, K.G., Duran, G.S. et al. Clinical comparative study on the accuracy of palatal rugae in models obtained by different impression materials and intraoral scanning. Clin Oral Invest 28, 153 (2024). https://doi.org/10.1007/s00784-024-05556-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-024-05556-y